Abstract
Introduction
To evaluate retrospectively the diagnostic accuracy of MR arthrography, compared with arthroscopy, in research of the glenoid labrum tear in patients with a first episode of traumatic anterior shoulder instability (TUBS).
Material and methods
We retrospectively reviewed the MR arthrography shoulder images of 118 patients with a first episode of TUBS, between June 2014 and May 2016.
Results
The overall accuracy of MR arthrography compared with arthroscopy of the glenoid labrum lesions was 94%, sensitivity 93%, and specificity 96%. The sensitivity of MR arthrography for Perthes lesion was 71.4%, and for ALPSA lesion, it was 91%. Slap lesion occurred in 11 out of 77 cases (9.3% of 118 cases). The Hill-Sachs lesion occurred in 48 out of 118 cases (40.7%), while the Hill-Sachs reverse lesion in 4 cases (3.4%).
Conclusions
The MR arthrography is accurate in detecting labral injuries. However, other studies are needed to assess the less frequent tear, as Perthes lesion. The presence of the Hill-Sachs lesion could provide useful information about the level of the shoulder instability.
Keywords: MR arthrography, Glenoid labrum tears, Traumatic anterior shoulder instability
1. Introduction
The Traumatic Anterior Shoulder Instability (TUBS) is the most frequent cause of glenoid labrum tears, which can be associated to the glenoid bone lesions. The glenoid labrum lesions of TUBS are a common problem and often occur in young subjects who practice sport activity.1, 2, 3
The correct diagnosis of the glenoid labrum lesions is useful to improve the multi-disciplinary approach and the outcomes of the patient during everyday life but above all during sports, where such lesions are present with highest risk of recurrence.4
The purpose of our study was to retrospectively evaluate the diagnostic accuracy of the MR arthrography, compared with arthroscopy, in the glenoid labrum lesions in patients with a first episode of TUBS.
2. Material and methods
Informed consent was obtained from research subjects. One hundred and eighteen patients (92 males and 26 females, range 16–66) with at least a single episode of TUBS over 12 months, with or without bone involvement were retrospectively evaluated. All patients were contacted after 12 months of the MR arthrography to evaluate the course. The images were obtained from the database of our hospital between June 2014 and May 2016. All images were acquired with MR magnetic field 1.5 T “Faced” Array coil (Philips, Best, Netherlands), matrix of 224 × 256 and foveal of 16–18 cm; for each patient were performed four standardized sequences: spin echo (SE) T1-weighted (W) fat-sat in axial, coronal, and sagittal section a weighted proton density (DP) fat-sat in coronal section.5
A few minutes before the examination, the patient was placed on a bed in a supine position. The affected shoulder was kept in slight abduction and slight external rotation and disinfected with Iodopovidone; with an anterior manual approach and without utilization of the radiological guidance (fluoroscopy) or ultrasound, a needle (20–23 Gauge) was introduced into the articulation for the gadolinium chelates injection (Dotarem; Guerbet, Roissy, France) (10 ml; dilution: 0.25 ml of 0.1 M paramagnetic contrast diluted in 100 ml of saline).6 In 2 cases, the paramagnetic contrast agent introduced is found to be outside the joint cavity that has resulted in the repetition of the procedure.
The MR examination was carried out about five minutes after the intra-articular injection of the contrast medium. The patient was positioned in a supine position with his arm along the body in a neutral position; a coil type “Flax-M” inserted in the shoulder was used.
Two radiologists, with at least 5 and 15 years of experience in musculoskeletal radiology, retrospectively analyzed the MR arthroscopy images; the results were compared with arthroscopy (diagnostic or therapeutic), which is currently the diagnostic goal, carried out at the orthopedic service of our center.
Operators have analyzed the following parameters:
Glenoid labrum anterior-inferior tear was classified into:
-
-
Bankart lesion, defined as complete avulsion of the labrum from the glenoid associated with fibrocartilage and periosteal tear (Fig. 1).
-
-
“Bony Bankart” lesion, when anterior inferior glenoid bone loss was present.
Fig. 1.
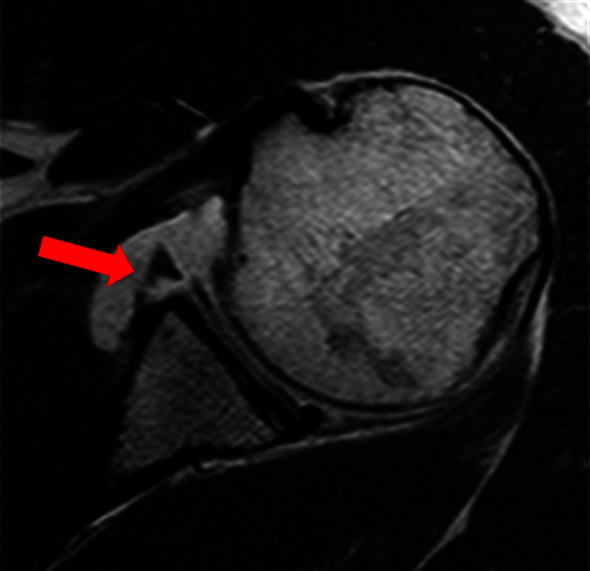
A 26-year-old male patient with shoulder anterior instability type TUBS. MR arthrography of the right shoulder, axial section, sequence spin echo T1 W. Bankart lesion (arrow) characterized by complete avulsion of the labrum from the glenoid labrum anterior inferior associated with periosteal detachment.
Main variants of the Bankart lesion are:
-
-
Perthes lesion: glenoid labrum detachment with an intact periosteum (Fig. 2).
-
-
ALPSA lesion (anterior labrum periosteal sleeve avulsion): scarring of the anterior inferior glenoid labrum with periosteum not interrupted.
-
-
GLAD (glenolabrum articular disruption) lesion: anterior-inferior lesion of the glenoid labrum associated with cartilage erosion.
-
-
Presence/absence of Hill-Sachs lesion (posterolateral humeral head compression fracture) and Hill-Sachs reverse lesion (impaction fracture of antero-medial aspect of humeral head following posterior dislocation).
-
-
SLAP lesion (superior labrum anterior to posterior), with or without involvement of the long head biceps tendon.
Fig. 2.
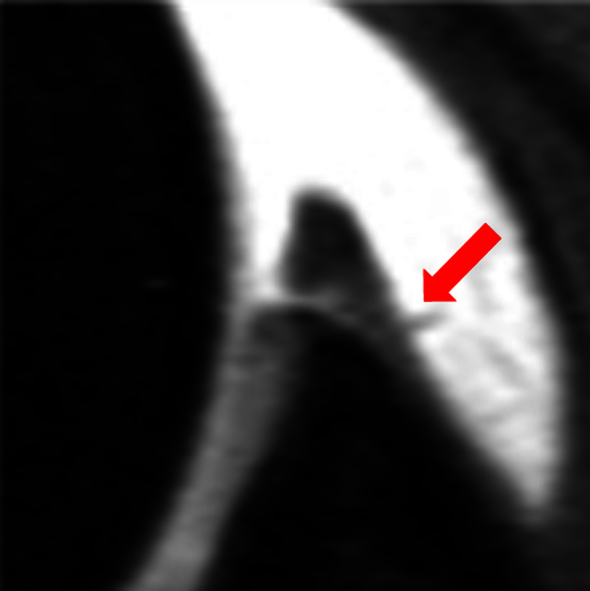
A 31-year-old male patient with anterior instability type TUBS. MR arthrography of the right shoulder, axial section, sequence spin echo T1 W with fat suppression. Perthes lesion (arrow) characterized by glenoid labrum detachment with an intact periosteum.
2.1. Statistical analysis
The parameters were age and sex of the patient; glenoid labrum anterior-inferior lesions (Bankart/Bony Bankart and variants, as Perthes and ALPSA lesions); GLAD lesions; Hill-Sachs lesion; SLAP lesions; and posterior labrum lesions.
Result of MR arthrography, compared with arthroscopy, about overall diagnostic accuracy, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV).7 Statistical analysis was performed using SPSS Statistics “19.0.0.1 FixPack” (IBM, United States) using the “Chi square Pearson” test.
3. Result
Overall, the glenoid labrum tears occurred in 77 out of 118 cases (65.2%). Among the 41 remaining cases, 11 out of 41 cases showed a Hill-Sachs isolated lesion (26.8%); the remaining 30 out of 41 cases were considered true negative (TN) (73.2%, 25.4% of the total).
By comparing the MR arthrography results with arthroscopy, the following were obtained: 77 cases of glenoid labrum tears (65.2%), 71 true positives (TP), 1 false positive (FP) and 5 false negatives (FN); of these, a false positive case concerns a SLAP lesion type II, the 5 false-negative cases concern 2 Perthes lesions, 1 ALPSA lesion, and 2 posterior glenoid labrum lesions (Table 1).
Table 1.
Difference between MR arthrography and arthroscopy result.
| MR arthrography | Arthroscopy | % MR arthrography | |
|---|---|---|---|
| Bankart lesion | 36 | 36 | 100 |
| Variant of BL | 16 | 19 | 84.2 |
| GLAD lesion | 2 | 2 | 100 |
| AI dislocation | 1 | 1 | 100 |
| Posterior-inferior lesion | 5 | 7 | 71.4 |
| Slap lesion | 17 | 18 | 89.4 |
BL: Bankart lesion; AI: anterior inferior.
The anterior-inferior glenoid labrum lesions occurred in 55 out of 77 cases (71%, 46.6% of 118). The most results are evaluated in Table 2.
Table 2.
Principal results of anterior-inferior Glenoid Labrum Injury evaluated with MR arthrography. percentage (%).
| Glenoid labrum injury classification (total of 55 lesions) | |||
|---|---|---|---|
| Bankart lesions | 36 (65.4) | No Bony Bankart | 22 (61) |
| Bony Bankart | 14 (39) | ||
| Variants of Bankart lesion | 16 (29) | ALPSA lesion | 11 (20) |
| Perthes lesion | 5 (5) | ||
| GLAD lesion | 2 (3.6) | ||
| Anterior inferior dislocation | 1 (1.8) | ||
The SLAP lesion occurred in 17 out of 77 cases (22% excluding 1 FP case); of these, 13 SLAP lesions were type II (16.8%), 4 type III (5.2%), and 0 type IV.
Type II SLAP lesion was associated in one case with a Bankart lesion (9%), in 2 cases with Bony Bankart lesions (18%), and in 2 cases with ALPSA lesion (18%); no case of SLAP lesions was associated with Perthes lesion.
The posterior glenoid labrum lesions occurred in 5 out of 77 cases (6.5%, excluding the two cases evaluated as FN).
The Hill-Sachs lesion occurred in 48 out of 118 cases (41%), while the Hill-Sachs reverse lesion in 4 out of 118 cases (3.4%).
The Hill-Sachs lesion was present in 11 cases not associated with glenoid labrum lesion, (9.3% of 118 cases), in 13 cases associated with Bankart lesion without bone involvement (59% out of 22 total), in 9 out of 14 cases with Bony Bankart lesion (64.2%), in 2 out of 5 cases with Perthes lesion (40%), in 8 out of 11 cases with ALPSA lesion (72.7%), in 100% of the GLAD lesion, and in 100% of the medial dislocation of the glenoid labrum, in 2 out of 11 cases of Slap Lesion (18.1%), and finally, in 1 out of 5 cases in posterior glenoid labrum tear (20%).
The Hill-Sachs reverse lesion occurred in 2 out of 5 cases in combination with posterior labrum tear (40%) and in 2 out of 36 cases in association with a Bankart lesion (5.5%).
The overall accuracy of MR arthrography for glenoid labrum tears was 94%, the overall sensitivity 93%, the overall specificity 96%, and the overall PPV and NPV respectively 98% and 86%.
The sensitivity for the Bankart lesion with or without bone involvement was 100%.
The sensitivity of the MR arthrography for the Perthes lesion was 71.4%, and for the ALPSA lesion, it was 91%.
There is no statistically significant correlation between the distribution of the lesions type Slap and labrum anterior inferior (p > 0.05).
The statistical value on the association between the presence of the Hill-Sachs lesion and the development of the anterior-inferior glenoid labrum tear, using the Chi-square test of Pearson, was statistically significant (p < 0.05).
Not make themselves known complications during and in the procedure. Age and sex were not statistically significant (p > 0.05).
4. Discussion
The MR arthrography is a diagnostic technique with a high sensitivity (93%) and specificity (96%) in the evaluation of lesions of the glenoid labrum tear after a single episode of TUBS.
According to the recent literature, the MR arthrography has a sensitivity of 88–96% and a specificity of 91–98%, which is often linked to the experience of the operator.8, 9, 10, 11
Since, as confirmed in the literature, most of the shoulder dislocations are anterior-inferior (95%), glenoid labrum lesions following episodes of post-traumatic dislocations often refer to the anterior-inferior labrum tear.12, 13 Among the glenoid labral tears, those of the anterior-inferior glenoid margin have also the largest number of recurrent dislocation.13, 14, 15
In our study, the main injury after TUBS is represented by the Bankart lesion (65.4%) (Fig. 1), with or without bone involvement; however, the Bony Bankart lesion was often present (38%); these results are in accordance with the literature, which reports an incidence of at least 40% of all the antero-inferior glenoid labrum injuries.14
In our study, the association of the Bankart lesion with the Hill-Sachs lesion is very frequent, both in the presence of Bankart lesions without bone loss (59%) and in the presence of Bony Bankart lesion (64.2%).
The Hill-Sachs lesion was not only simple markers of previous anterior-inferior shoulder dislocation; in fact, this could provide useful information about the level of stability of the shoulder before the trauma responsible for dislocation: more deep was the Hill-Sachs lesion, more higher was the joint stability before the trauma. It is not obvious, however, that in the presence of the Hill-Sachs lesion, a glenoid labrum tear is often associated; in fact, the Hill-Sachs lesion is developed in the absence of the glenoid labrum tear in 9.3% of the cases.
The Hill-Sachs reverse lesion is a rare type of lesion, often tied to a posterior dislocation of the shoulder. The dynamics is the opposite of the more common Hill-Sachs lesion, and is often associated with the posterior glenoid labrum tear (40% in our study), while more rarely (5.5%) is associated with Bankart lesions. These cases probably reflect a gleno-humeral multidirectional dislocation that occurred during traumatic episode.13, 14
The inferior labro capsular distance can be easily and quickly measured and used as an effective clinical screening method for multidirectional instability of the shoulder.16
In the recent years, a more detailed classification of the labrum lesions has been developed, and several variants of these have been described. However, although for some injuries, as the Bankart lesion, the diagnostic criteria and treatment are well standardized, it is not always possible to classify easily with the MR arthrography all the abnormal glenoid labrum.8
The Perthes lesion, for example (Fig. 2), known since 1905 to be a variant of Bankart lesion, often can not be diagnosed in the classical axial MR acquisitions, and sometimes, may be unnoticed into the arthroscopy; Waldt et al. emphasized that the Perthes lesion is particularly difficult to estimate, representing an accuracy of 50% for MR arthrography, especially where there are fibrotic phenomena that prevent infiltration of intra-articular contrast medium.17
In such a case, the accuracy of MR arthrography could be improved by placing the patient's arm in ABER (Abduction and extra-rotation of the arm) position during acquisition of the images.18, 19
Even a recent study by Li et al. confirms that the accuracy in the diagnosis of the Perthes lesion with MR arthrography is modest, amounting to 57%.20
In our case, the incidence of Perthes injuries was 9%, more higher than in the publications of Waldt and Li, who present a similar number of case. However, the Perthes lesion among all was the one that presented the lowest sensitivity (71%), as the theories supported by many authors.8, 17, 20
In our experience, ALPSA lesion, results of a previous Perthes lesion, has not been very frequent (20%), as reported in recent studies.20, 21
Even for the search of this type of glenoid labrum lesions, some authors recommend the additional acquisitions, such as the ADIR (adduction and internal rotation of the arm) position.5, 22
Virtual MR arthroscopy of the shoulder joint has been described in a few reports using 3D gradient echo sequences after intra-articular injection of dilute gadolinium.23 The technique can act as a useful adjunct tool to MR arthrography in the assessment of labral tears, by providing helpful visual information similar to arthroscopy.23
Our study is limited because it is retrospective and the variant of Bankart has been infrequent.
5. Conclusions
The glenoid labrum lesion after TUBS is very frequent and the MR arthrography is very accurate in detecting labral injuries. Many authors agree that the MR arthrography is the non-invasive diagnostic goal in the glenoid labrum lesions. However, other studies are needed to assess the less frequent tear, as Perthes lesion. The presence of the Hill-Sachs lesion could provide useful information about the level of the shoulder instability.
Conflicts of interest
The authors have none to declare.
Contributor Information
Luca Saba, Email: lukas_red@hotmail.it.
Massimo De Filippo, Email: luca.saba@chb.unicancer.fr.
References
- 1.Thomas S.C., Matsen F.A. An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability. J Bone Jt Surg Am. 1989;71(4):506–513. [PubMed] [Google Scholar]
- 2.Woerteler K., Waldt S. MRI imaging in sports-related glenohumeral instability. Eur Radiol. 2006;16:2622–2636. doi: 10.1007/s00330-006-0258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Applegate G.R., Hewitt M., Snyder S.J., Watson E., Kwak S., Resnick D. Chronic labral tears: value of magnetic resonance arthrography in evaluating the glenoid labrum and labral-bicipital complex. Arthroscopy. 2004;20:959–963. doi: 10.1016/j.arthro.2004.08.017. [DOI] [PubMed] [Google Scholar]
- 4.Palmer W.E., Brown J.H., Rosenthal D.I. Labral-ligamentous complex of the shoulder: evaluation with MR arthrography. Radiology. 1994;190:645–651. doi: 10.1148/radiology.190.3.8115604. [DOI] [PubMed] [Google Scholar]
- 5.Steinbach L.S. MRI of shoulder instability. Eur J Radiol. 2008;68:57–71. doi: 10.1016/j.ejrad.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 6.Faletti C., De Filippo M., Giudice G., Larciprete M., Seccia A., Regis G. Fibro-cartilaginous lesions of the glenoid labrum in shoulder instability: a proposed classification using sagittal-oblique arthro-MRI. Radiol Med. 2002;104(1–2):68–74. [PubMed] [Google Scholar]
- 7.Bossuyt P., Reitsma J.B., Bruns D.E. Towards complete and accurate reporting of studies on diagnostic accuracy: the STARD initiative. Fam Pract. 2004;21(February (1)):4–10. doi: 10.1093/fampra/cmh103. [DOI] [PubMed] [Google Scholar]
- 8.Waldt S., Burkart A., Imhoff A.B., Bruegel M., Rummeny E.J., Woertler K. Anterior shoulder instability: accuracy of MR arthrography in the classification of anteroinferior labroligamentous injuries. Radiology. 2005;237(2):578–583. doi: 10.1148/radiol.2372041429. [DOI] [PubMed] [Google Scholar]
- 9.Chandnani V.P., Yeager T.D., Bencardino Christensen K. Glenoid labral tears: prospective evaluation with MR imaging, MR arthrography, and CT arthrography. Am J Roentgenol. 1993;161:1229–1235. doi: 10.2214/ajr.161.6.8249731. [DOI] [PubMed] [Google Scholar]
- 10.Palmer W.E., Caslowitz P.L. Anterior shoulder instability: diagnostic criteria determined from prospective analysis of 121 MR arthrograms. Radiology. 1995;197:819–825. doi: 10.1148/radiology.197.3.7480762. [DOI] [PubMed] [Google Scholar]
- 11.Roger B., Skaf A., Hooper A.W., Lektrakul N., Yeh L., Resnick D. Imaging findings in the dominant shoulder of throwing athletes: comparison of radiography, arthrography, CT arthrography, and MR arthrography with arthroscopic correlation. Am J Roentgenol. 1999;172:1371–1380. doi: 10.2214/ajr.172.5.10227520. [DOI] [PubMed] [Google Scholar]
- 12.Beltran J., Rosenberg Z.S., Chandnani V.P., Cuomo F., Beltran S., Rokito A. Glenohumeral instability: evaluation with MR arthrography. Radiographics. 1997;17:657–673. doi: 10.1148/radiographics.17.3.9153704. [DOI] [PubMed] [Google Scholar]
- 13.Tirman P.F., Stauffer A.E., Crues J.V. Saline magnetic resonance arthrography in the evaluation of glenohumeral instability. Arthroscopy. 1993;9:550–559. doi: 10.1016/s0749-8063(05)80403-7. [DOI] [PubMed] [Google Scholar]
- 14.Jordan R.W., Naeem R., Srinivas K., Shyamalan G. A comparison of magnetic resonance arthrography and arthroscopic findings in the assessment of anterior shoulder dislocations. Skelet Radiol. 2015;44(May (5)):653–657. doi: 10.1007/s00256-014-2080-6. [DOI] [PubMed] [Google Scholar]
- 15.Genovese E., Spanò E., Castagna A. MR-arthrography in superior instability of the shoulder: correlation with arthroscopy. Radiol Med. 2013;118(September (6)):1022–1033. doi: 10.1007/s11547-013-0942-y. [DOI] [PubMed] [Google Scholar]
- 16.Lim C.O., Park K.J., Cho B.K., Kim Y.M., Chun K.A. A new screening method for multidirectional shoulder instability on magnetic resonance arthrography: labro-capsular distance. Skelet Radiol. 2016;45(July (7)):921–927. doi: 10.1007/s00256-016-2364-0. [DOI] [PubMed] [Google Scholar]
- 17.Waldt S., Burkart A., Lange P., Imhoff A.B., Rummeny E.J., Woertler K. Diagnostic performance of MR arthrography in the assessment of superior labral anteroposterior lesions of the shoulder. AJR. 2004;182:1271–1278. doi: 10.2214/ajr.182.5.1821271. [DOI] [PubMed] [Google Scholar]
- 18.Perthes G. Zur therapie der habituellen schulterluxation. Med Zs. 1905;237:481. [Google Scholar]
- 19.Wischer K., Bredella M., Genant H., Stoller D., Bost F., Tirman F. Perthes lesion (a variant of the Bankart lesion): MR imaging and MR arthrographic findings with surgical correlation. AJR. 2002;178:233–237. doi: 10.2214/ajr.178.1.1780233. [DOI] [PubMed] [Google Scholar]
- 20.Li H.F., Liu Y.J., Cheng L.Q. Diagnostic value of MRI and MR arthrography in the detection of injuries of anterior labrum in shoulder. Zhongguo Gu Shang. 2012;25:413–417. [PubMed] [Google Scholar]
- 21.Antonio G.E., Griffith J.F., Yu A.B., Yung P.S., Chan K.M., Ahuja A.T. First-time shoulder dislocation: high prevalence of labral injury and age-related differences revealed by MR arthrography. J Magn Reson Imaging. 2007;26:983–991. doi: 10.1002/jmri.21092. [DOI] [PubMed] [Google Scholar]
- 22.Schaeffeler C., Waldt S., Bauer J.S. MR arthrography including abduction and external rotation images in the assessment of atraumatic multidirectional instability of the shoulder. Eur Radiol. 2014;24(June (6)):1376–1385. doi: 10.1007/s00330-014-3133-x. [DOI] [PubMed] [Google Scholar]
- 23.Song H.T., Huh Y.M., Kim S., Kim S.J., Suh J.S. The usefulness of virtual MR arthroscopy as an adjunct to conventional MR arthrography in detecting anterior labral lesions of the shoulder. AJR Am J Roentgenol. 2009;192:149–155. doi: 10.2214/AJR.07.2312. [DOI] [PubMed] [Google Scholar]


