Abstract
Non bacterial thrombotic endocarditis presenting as a stroke is a rare presentation as a result of an underlying occult ovarian clear cell adenocarcinoma. Embolic events secondary to non bacterial thrombotic endocarditis are potentially a life-threatening condition if not diagnosed and treated promptly. High clinical suspicion for an underlying neoplasm is one of the key elements to be considered in the management of non bacterial thrombotic endocarditis. Systemic anticoagulation will treat as well as prevent further thromboembolic events.
Keywords: non bacterial thrombotic endocarditis, ovarian clear cell carcinoma, stroke, fever of unknown origin
Introduction
The term non bacterial thrombotic endocarditis refers to a spectrum of lesions ranging from microscopic aggregates of platelets to large vegetations on formerly normal heart valves in the absence of a bacterial infection.1 This has been found to be often associated with connective tissue disorders, hypercoagulable states or advanced malignancy such as lung and ovarian adenocarcinomas.1,2 We report a rare case of a 60-year-old female presenting with left-sided weakness as a consequence of non bacterial thrombotic endocarditis in a previously undiagnosed ovarian malignancy. Three cases have been revealed so far in the literature showing the association of embolic events in non bacterial thrombotic endocarditis on a previously diagnosed ovarian clear cell carcinoma, but a first presentation as stroke in a previously healthy individual has never been reported in the literature.
Case report
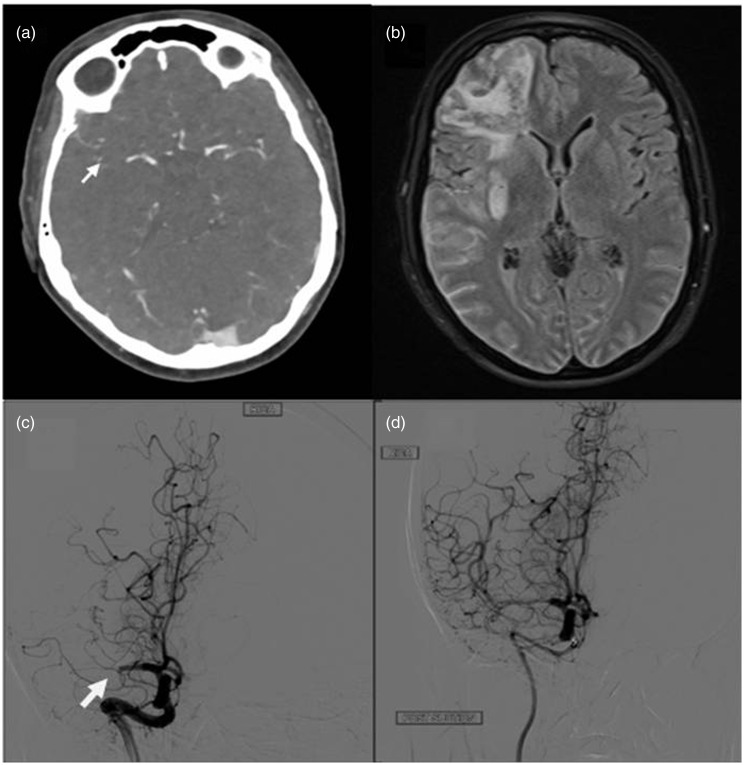
A 60-year-old female who was previously healthy with no risk factors for stroke presented with sudden onset left-sided weakness and dysphasia. National Institutes of Health Stroke Scale score on admission was 20. Brain computer tomography did not reveal any established infarct, however a computer tomography cranial angiogram showed evidence of thrombus in the proximal right middle cerebral artery (Figure 1(a)). She was treated with thrombolysis and endovascular mechanical clot removal (Figure 1(c) and (d)) with a successful outcome of recovering to a National Institutes of Health Stroke Scale score of 2 within 24 hours.
Figure 1.
(a) Abrupt cut off (white arrow) at the mid section of the right middle cerebral artery (computer tomography cranial angiogram). (b) Right frontal parenchymal haemorrhage with surrounding oedema and multiple small infarcts in the right middle cerebral artery territory (magnetic resonance imaging head). (c) Occlusion of the right middle cerebral artery prior to suctioning of the clot during endovascular mechanical thrombectomy. (d) Post suctioning of the clot demonstrating the patency of the middle cerebral artery.
As a part of stroke work-up brain magnetic resonance imaging (MRI) was performed. Interestingly magnetic resonance imaging showed multiple infarcts with haemorrhages in the right middle cerebral artery territory and bilateral cerebellar hemisphere raising a possibility of an embolic source (Figure 1(b)). While reviewing the history, it became obvious that the patient had not been well for the previous four weeks prior to admission. She had a low grade pyrexia and mildly raised inflammatory markers with associated anaemia and thrombocytopenia. All the above symptoms and image findings raised the possibility of infective endocarditis.
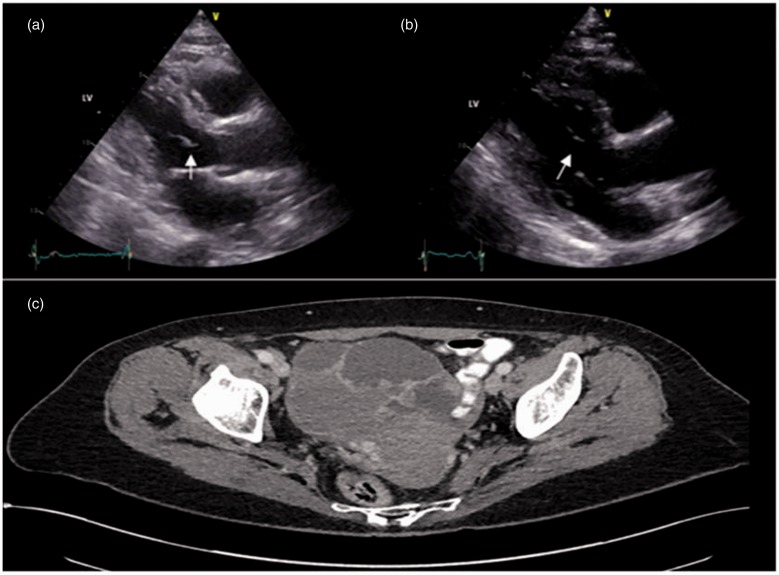
An urgent echocardiogram established a mobile mass in the anterior mitral valve leaflet indicative of a vegetation which was further proven on transoesophageal echocardiography. It was a large mobile mass measuring about 11 × 4 mm and prolapsing in to the left ventricular outflow tract with mild aortic regurgitation (Figure 2(a)). She was then treated for infective endocarditis with intravenous antibiotics. Despite therapy she continued to have an intermittent fever with persistent raised inflammatory markers. However serial blood cultures and serology remained sterile. Further studies including virology, vasculitic screen (together with thrombophilia screen) and serology for atypical organisms were negative.
Figure 2.
(a) Vegetation (white arrow) in the Anterior mitral valve leaflet prolapsing in to the left ventricular outflow tract prior to treatment. (b) Reduced size of the thrombotic vegetation (white arrow) three months after anticoagulation. (c) computer tomography pelvis showing the right ovarian multicystic complex tumour.
Hence a computer tomography of thorax, abdomen and pelvis was performed to identify an infective focus. Interestingly an underlying large pelvic mass suggestive of a right-sided ovarian tumour (9 × 9 cm) was found without any evidence of metastasis (Figure 2(c)). Imaging also revealed pulmonary, splenic and renal embolic events with evidence of infarcts. Multi systemic embolisation with poor clinical response to antibiotics raised a suspicion of non bacterial thrombotic endocarditis. Therefore low molecular weight heparin was commenced. She underwent hysterectomy with bilateral salpingo-oophorectomy and omentectomy followed by adjuvant chemotherapy. A high grade ovarian clear cell carcinoma was confirmed on histology.
Serial repeat transthoracic and transoesophgeal echocardiography was performed to assess the size of the vegetation as a response to anticoagulation and a promising result was demonstrated (Figure 2(b)).
Discussion
Stroke can be rarely the first presentation in an underlying clear cell ovarian tumour as a manifestation from non bacterial thrombotic endocarditis. A hypercoagulable state is commonly seen in mucin producing adenocarcinomas but very rarely found in ovarian clear cell carcinoma.3 Only very few cases reported so far show an association between non bacterial thrombotic endocarditis and ovarian clear cell carcinoma.
The diagnosis of non bacterial thrombotic endocarditis is considerably more elusive than that of infective endocarditis. Non bacterial thrombotic endocarditis should be highly suspected when no clinical progression is made in a patient who is treated for infective endocarditis.2 There are no pathognomonic signs and symptoms or serum markers that aid the diagnosis of non bacterial thrombotic endocarditis.4 Non bacterial thrombotic endocarditis vegetation is typically small with a broad base, irregular shape and measuring less than 1 cm in diameter. Incidence of valve abscess and rupture is uncommon in non bacterial thrombotic endocarditis unlike in infective endocarditis.5
Histologically vegetations from non bacterial thrombotic endocarditis are made of a combination of fibrins and platelets with minimal inflammatory elements. They have the ability to dislodge easily leading to multi organ systemic infarcts. Cerebral embolisation has been reported as high as 14–91% in the literatures.6 Vegetations in non bacterial thrombotic endocarditis are frequently located on left-sided heart valves, with 64% involving the mitral valve.7 Usually non bacterial thrombotic endocarditis manifests in advanced malignancies, however it has rarely been reported in early stages of cancer such as ovarian cancer due to a high growth rate of the tumour and associated abundant necrosis.8,9 In our patient systemic embolic manifestations developed as a result of non bacterial thrombotic endocarditis while at an early stage of the cancer FIGO 1c (International Federation of Gynaecology and Obstetrics – Gynaecological staging system).
When no obvious infective causes have been found in a clearly evident endocarditis, non bacterial thrombotic endocarditis should be strongly considered.4 In such instances, investigating for an underlying neoplastic disease is of paramount importance as timely intervention on cancer promises successful treatment for both cancer and embolic events. The mainstay of treatment for non bacterial thrombotic endocarditis is anticoagulation. However warfarin is ineffective in this setting, necessitating the treatment with unfractionated, or low-molecular weight heparin.10 It is seldom that surgical intervention for the valve is required unless the patient develops acute cardiac failure.
Acknowledgements
None
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethical approval
Written informed consent for publication was obtained from the patient.
Guarantor
IN.
Contributorship
VK contributed to the manuscript, and gathering of clinical data, as well as relevant imaging information. IN: overall supervision and finalising of manuscript and guarantor for the work presented.
Provenance
Not commissioned; peer-reviewed by Simon Dubrey and Camelia Diaconu.
References
- 1.Kennedy AW, Biscotti CV, Hart WR, Webster KD. Ovarian clear cell adenocarcinoma. Gynecol Oncol 1989; 32: 342–349. [DOI] [PubMed] [Google Scholar]
- 2.Maiti A, Short NJ. A blue finger and hyponatremia leading to a diagnosis of malignancy associated marantic endocarditis. J Gen Intern Med 2016; 31: S484–S484. [Google Scholar]
- 3.Devulapalli S, Pinto N, Gandothra C, Jayam-Trouth A, Kurukumbi M. A rare case of occipital stroke as a consequence of nonbacterial thrombotic endocarditis in ovarian clear cell carcinoma: a case report. Case Rep Neurol 2012; 4: 84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Asopa S, Patel A, Khan OA, Sharma R, Ohri SK. Non-bacterial thrombotic endocarditis. Eur J Cardio-Thorac Surg 2007; 32: 696–701. [DOI] [PubMed] [Google Scholar]
- 5.Otto CM. Nonbacterial thrombotic endocarditis. Valvular heart disease, Philadelphia: W.B. Saunders, 1999, pp. 445–450. [Google Scholar]
- 6.Aryana A, Esterbrooks DJ, Morris PC. Nonbacterial thrombotic endocarditis with recurrent embolic events as manifestation of ovarian neoplasm. J Gen Intern Med 2006; 21: C12–C15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steiner I. Nebakterialni tromboticka endokarditida – studie 171 pripadu [Nonbacterial thrombotic endocarditis – a study of 171 case reports]. Cesk Pathol 1993; 29: 58–60. [PubMed] [Google Scholar]
- 8.Lin YK, Lee JT, Yang FC, Sung YF, Kao HW, Lin CC, et al. Systemic embolic events with nonbacterial thrombotic endocarditis as manifestations of recurrent ovarian clear cell carcinoma. Taiwanese J Obstet Gynecol 2015; 54: 625–628. [DOI] [PubMed] [Google Scholar]
- 9.Tanaka H, Ito M, Yoshida K, Asakura T, Taniguchi H. Nonbacterial thrombotic endocarditis complicated with stage Ia ovarian cancer. Int J Clin Oncol 2009; 14: 369–371. [DOI] [PubMed] [Google Scholar]
- 10.Walsh-McMonagle D, Green D. Low-molecular-weight heparin in the management of Trousseau’s syndrome. Cancer 1997; 80: 649–655. [PubMed] [Google Scholar]