Abstract
Objective
Although distress during treatment procedures and longer-term treatment-related anxiety are among the most common cancer-related stressors for children and their families, they are not invariant. This study examined whether individual differences in temperament and personality play a role in how children respond to treatment procedures. Attention control, a facet of the effortful control dimension of temperament, and the personality attribute ego-resilience were hypothesized to predict lower levels of distress during procedures. Moreover, ego-resilience and distress during procedures were hypothesized to account for indirect associations between attention control and longer-term treatment-related anxiety. Child gender was examined as a potential moderator of these relationships.
Method
Participants were 147 children undergoing treatment for pediatric cancer and their parents. At baseline, parents reported on children’s effortful control and ego-resilience. Multiple raters assessed children’s distress during multiple cancer-related procedures. Treatment-related anxiety was measured 3 months and 9 months after the last assessed treatment procedure.
Results
Attention control was linked to ego-resilience and lower levels of distress, and these variables, in turn, accounted for indirect associations between attention control and treatment-related anxiety. Associations involving ego-resilience were stronger for boys than girls.
Conclusion
Attention control plays an important role in children’s immediate and longer-term responses to cancer-related medical procedures. Medical staff should consider individual differences in child temperament and personality when considering the nature and extent of support to provide to pediatric cancer patients and their families.
Keywords: Pediatric Cancer, Procedure Anxiety, Distress, Temperament
Children undergoing treatment for cancer face numerous challenges. Invasive cancer treatment procedures and the distress that often accompanies such treatments are among the most common cancer-related stressors for children.1 Children often find the stress, nausea, and fatigue associated with treatment to be more distressing than the disease itself.2 Further, there is evidence that the psychological effects of cancer treatments may persist over time.3 Yet, there are substantial individual differences in how children respond to treatment procedures.4,5 Little is known, however, about the role of temperament in children’s treatment-related distress or how individual differences in temperament and personality might be related to longer-term treatment-related anxiety. This study focused on understanding how children’s temperament and personality may account for individual differences in distress during cancer treatment procedures and longer-term anxiety about these treatment procedures.
Temperament and Longer-Term Treatment-Related Anxiety
Temperament is the enduring part of an individual’s character that is influenced by heredity, biological factors, experience, and maturation.6 The capacity for self-regulation is one aspect of temperament that facilitates adaptive responses to treatment for pediatric cancer, and self-regulatory capacity is closely aligned with the dimension of temperament called effortful control. Effortful control is multi-faceted; specific facets are the capacity to shift one’s attention, thoughtful planning, detecting one’s own errors, and inhibiting a dominant response in favor of a more adaptive subdominant response.6 Effortful control is linked to adaptive attributes during childhood, including empathy and social competence,7 and might play an important role in children’s responses to cancer treatments.
However, not all facets of effortful control are necessarily associated with children’s responses to cancer treatments. Two of the primary facets of effortful control are attention control and inhibitory control.6 Attention control includes the capacity to focus and shift attention, and inhibitory control includes the tendency to engage in appropriate behaviors while suppressing inappropriate responses. Moreover, attention control is an aspect of the set-shifting component of children’s executive function, and inhibitory control is an aspect of the response inhibition component.8 Lower levels of attention control are associated with anxiety and other childhood internalizing problems,9 whereas lower levels of inhibitory control tend to be more closely associated with aggression and externalizing problems.10 Therefore, the capacity to focus and shift attention may be more strongly associated with children’s ongoing anxiety about cancer treatment procedures than inhibitory control.
Mediators Linking Temperament to Longer-Term Treatment-Related Anxiety
Two possible pathways may explain how lower levels of attention control could lead to longer-term treatment-related anxiety. The first path involves the personality attribute of ego-resilience, the extent to which a person can “bounce back” following stressful experiences.11 The ability to focus and shift attention might facilitate children’s capacity for resilience following stressors which, in turn, might mitigate their longer-term anxiety related to treatment. Supporting this perspective, ego-resilience has been found to mediate associations between effortful control and several aspects of children’s adaptation, including fewer internalizing problems.12 In addition, in a prior investigation we found that ego-resilience mediated the association between overall effortful control and children’s cancer-related quality of life, including aspects of treatment-related anxiety.13
The second path involves children’s distress during treatment procedures. Children with lower levels of attention control may have difficulty shifting attention away from the stressful aspects of treatment procedures and may, therefore, experience and express more distress during procedures. Experience distress during procedures could, in turn, lead to longer-term treatment-related anxiety. Prior research has found that lower levels of overall effortful control are associated with using fewer adaptive coping behaviors such as humor and deep breathing during invasive medical procedures.14 However, relationships among specific facets of effortful control, children’s distress during cancer treatments, and longer-term treatment-related anxiety have not been explored.
Gender Differences
The magnitude of associations among attention control, ego-resilience, distress, and treatment-related anxiety may differ depending on child gender. Girls tend to have substantially higher levels of overall effortful control than boys, although the effect size for gender differences in attention control is small.15 Despite higher levels of effortful control, girls do not necessarily show better adjustment to cancer treatments and tend to express higher levels of distress during treatment procedures.16 The pattern of gender differences across the constructs of interest suggests that examining gender differences in the magnitude of associations between constructs could prove fruitful, although it is not entirely clear whether the magnitude of associations would be stronger among boys relative to girls. However, in a recent study of at-risk youth, temperament was more strongly associated with ego-resilience among boys than among girls.17 Therefore, there is initial evidence to suggest that some of the pathways may be stronger among boys.
Present Study
This longitudinal study, which examined individual differences in temperament, personality, and treatment responses as predictors of longer-term treatment-related anxiety in a sample of children undergoing treatment for pediatric cancer, had three goals. The first goal was to examine direct associations between the two facets of effortful control and children’s distress during treatments and longer-term treatment-related anxiety. We hypothesized that higher baseline levels of attention control would be associated with more ego-resilience, lower levels of distress during cancer-related procedures, and lower levels of longer-term treatment-related anxiety. The second goal focused on indirect pathways linking facets of effortful control and treatment-related anxiety. Specifically, we expected that ego-resilience and lower distress during treatment procedures would mediate the association between attention control and treatment-related anxiety at follow-ups conducted three and nine months after the last assessed treatment procedure. The third goal was to explore whether the magnitude of the above associations differed by gender. As there is little prior research to guide specific hypotheses, we did not propose specific relationships regarding the strength of associations for boys relative to girls.
METHOD
Overview
The present study is part of a larger longitudinal parent study that collected data from 2009 to 2015 at two large children’s hospitals in the United States. The study protocol was reviewed and approved by the hospitals’ Institutional Review Boards (IRB) and the university affiliated with one of the hospitals. The parent study’s primary aim was to identify factors that mitigate the psychosocial impact of cancer-related treatment procedures on families of pediatric cancer patients. There were four phases of data collection: (1) baseline assessment – adult primary caregivers (“parents”) completed questionnaires about themselves and their children at study entry; (2) treatment assessments – data were collected at up to three sequential children’s treatment-related procedures (port starts, bone marrow aspirations, or lumbar punctures); ratings of child distress and cooperation during procedures were made by parents, nurses, children, and independent observers of the treatment procedures; (3) first follow-up assessment – approximately three months after the last treatment assessment, parents completed a set of questionnaires about themselves and their children; (4) second follow-up assessment – approximately 9 months after the last treatment assessment, parents completed a second set of questionnaires about themselves and their children.
Recruitment Procedures
Families were eligible if (a) the child was between 3 and 12 years old; (b) the child had been diagnosed with cancer at least 1 month but no more 18 months before study entry and was receiving port starts, lumbar punctures, and/or bone marrow aspirations as part of treatment; and (c) parent and child were able to speak and the parent could read English well enough to provide consent and complete the questionnaires. Following HIPAA guidelines, clinical staff identified eligible children and initially approached families about their interest in the study. Research staff met with interested parents and obtained informed consent, and when appropriate, verbal assent from children. Parents and children were compensated with gift cards for assessments. Approximately 87% of parents and children approached agreed to participate. Parents who completed the baseline assessment were included in the present analyses.
Participants
The current study sample consisted of 147 parents (85% female; average age=34.00; SD=6.95) of children (60% male; average age=6.5; SD=3.14) with pediatric cancer. Seventy-four percent of parents (72% of children) identified as White. Other demographic information is presented in Table 1. The majority of children were diagnosed with Acute Lymphoblastic Leukemia (79.6%), followed by Wilm’s Tumors (4.8%), Non-Hodgkin’s Lymphoma (3.4%), other lymphomas (2.8%), astrocytoma (2%), and other cancers (e.g., Ewing’s sarcoma, osteosarcoma; 7.4%). At study entry, all children had started cancer treatment (mean time in treatment=3.49 months, SD=3.22; median=2.43).
Table 1.
Parent and Child Demographics (N=147 families)
| Parents (n=147) | Children (n=147) | |
|---|---|---|
| Age: Mean (SD) | 33.97 (6.95) | 6.5 (3.14) |
| Gender (%) Female Male |
125 (85%) 22 (15%) |
59 (40%) 88 (60%) |
| Ethnicity (%) White African American Bi-racial Hispanic/Latino American Indian/Alaskan Other |
109 (74.7%) 26 (17.8%) 0 8 (5.5%) 2 (1.4%) 1 (0.7%) |
106 (72.1%) 27 (18.4%) 7 (4.8%) 6 (4.1%) 0 1 (0.7%) |
| Household income <$20,000 $20,000-$59,999 $60,000-$100,000 >$100,000 |
30.1% 31.4% 28.0% 10.5% |
|
| Employment status Unemployed Part-time Full-time |
52.4% 16.1% 31.5% |
|
| Education Less than high school diploma High school diploma Some college College degree or higher |
13.6% 21.1% 38.8% 26.5% |
At the first follow-up assessment, average total amount of time children had been in treatment (i.e., prior treatment plus treatment during study) was 9.92 months (SD=4.13); average time from study entry was 6.45 months (SD=2.45; range=3.65-19.98). At the second follow-up assessment, average total amount of time in treatment was 16.60 months (SD=4.00); average time from study entry was 13.21 months (SD=2.40; range=9.43-21.62).
Baseline Assessment
At the initial assessment, parents provided information about their own and their child’s demographics and their child’s clinical history. Parents also completed the measures of their child’s temperament and personality described below.
Facets of effortful control
Attention control and inhibitory control were assessed using age-appropriate temperament scales developed by Rothbart and colleagues (c.f., 18). Specifically, the Child Behavior Questionnaire18 was used for children ages 3-6; the Temperament in Middle Childhood Questionnaire Version 319 for children ages 7-9, and the Early Adolescent Temperament Questionnaire Revised20 for ages 10-12. The questionnaires have multiple subscales, and attention control and inhibitory control are operationalized as the average score on each of the relevant subscales. The subscales each contain 5-10 items with a 5-point scale (from 1=“almost always untrue of your child” to 5=“almost always true of your child”) regarding children’s behavior over the past six months. In this study, coefficient alphas (α) for attention control were: .73 (ages 3-6), .95 (ages 7-9), and .63 (ages 10-12). Coefficient alphas (α) for inhibitory control were: .79 (ages 3-6), .72 (ages 7-9), and .52 (ages 10-12). The coefficient alphas were generally consistent with Rothbart’s reports, although the reliability of the inhibitory control scale was considerably lower in the oldest age group compared to these reports.20 This low internal reliability may have been due in part to small number of items (5) on this scale.
Based on prior work,4 we had concerns about being able to enroll sufficient numbers of children to conduct meaningful analyses with sufficient power within the different age groups. We consulted with scale authors about the strategy of combining scores from the three scales into one age-standardized overall distribution, and they supported this strategy (S. Putnam, personal communication, July 15, 2013). As expected, there were not sufficient numbers of children in each age group; thus, we followed this strategy of using single age-standardized distributions of each subscale score.
Ego-resilience
Parents rated their child’s level of ego-resilience using an 11-item measure developed by Eisenberg and colleagues.12 Items were rated on a 5-point Likert-type scale (from 1=“almost always untrue of your child” to 5=“almost always true of your child”). The scale has good internal consistency and has consistently been associated with measures of effortful control.12 Across the three age groups, coefficient alphas ranged from .66 to .71.
Covariates
The following measures from the baseline assessment were included as potential covariates in the analyses because prior research suggests they may be associated with psychosocial outcomes in pediatric cancer patients and survivors.21-23
Total time in treatment (i.e., prior treatment plus in-study treatment) at the time of the 3-month follow-up was used to create a “time in treatment” variable.
Household income and parent education were moderately correlated (r=. 44, p<.001). Each variable was standardized and then averaged to create a relative SES index.
Parent trait anxiety and depression were assessed at baseline. Trait anxiety was assessed with the 20-item trait subscale of the State-Trait Anxiety Inventory STAI 24 (α=.91). Depression was measured with the 20-item Center for Epidemiologic Studies—Depression Scale 25 (α=.90). These measures were standardized and averaged to create a single index of parent neuroticism. In addition, we included child age as a potential covariate and child gender as a moderator.
Treatment Assessment
Child distress
Children’s procedure-related distress was rated after each procedure using the FACES scale.26 Parents, nurses, children themselves, and independent observers provided ratings (from 1=“no distress at all” to 6=“the worst distress”). Parents, medical staff, and children who were awake independently provided distress ratings immediately after a procedure was completed. At one of the two hospitals, children who received general anesthesia rated their distress when they regained consciousness. Observers viewed video-recordings of the procedures before making their rating. All raters were blind to ratings from other sources. Inter-rater correlations among parents, nurses, children, and observers across the three procedures were all significant (p< .001). Coefficient alphas were used to estimate (1) inter-rater agreement within each procedure and (2) intra-rater agreement across procedures. Within a procedure, alphas ranged from .85 (first procedure) to .89 (second procedure); across procedures, alphas ranged from .67 (nurses) to .83 (children).
To create a single distress factor score for use in subsequent analyses, a confirmatory factor analysis (CFA) was conducted in Mplus 7.2.27 The best fitting model (χ2=47.787, p<.05; RMSEA=.06; CFI=.98) included a higher-order distress latent construct that was comprised of four informant constructs for child, parent, medical staff, and observer. Each informant construct was comprised of three indicators (one for each time point), and residuals for indicators within the same time point (e.g., parent at time 2 with observer at time 2) were allowed to correlate. Due to the relatively small sample size and modest statistical power, we extracted the distress latent construct factor score and used this factor score as a manifest variable (rather than a latent construct) in analyses presented below.
Follow-Up Assessments
Treatment-related anxiety
At the 3-month and 9-month follow-up assessments, parents completed age-appropriate versions of the PedsQL™ Cancer Module for their child. Subscales of the Cancer Module have demonstrated good construct validity and high coefficient alphas. The module assesses several cancer treatment-related quality of life dimensions, including the procedure anxiety and treatment anxiety subscales that were the focus of the present study.23 The procedure anxiety subscale contains three items assessing fears and anxiety about various parts of a procedure (i.e., injections, IVs, and blood tests). The treatment anxiety subscale contains three items assessing general fears and anxiety about doctor visits and going to the hospital. Parents used a 5-point Likert-type scale (from 0=“never” to 5=“almost always”) to respond to items. Total subscale scores are converted to a 0-100 scale with higher scores indicating fewer problems (i.e., better quality of life). As the procedure anxiety and treatment anxiety subscale scores were highly correlated in the present study (r=.60, p<.001 at 3-month follow-up and r=.64, p<.001 at 9-month follow-up), the subscale scores were averaged to create indexes of “treatment-related anxiety” for the 3-month and 9-month follow-ups, respectively.
Data Preparation and Analysis Plan
Values for sporadic missing data (<1% of all items) were imputed using substitution of sample mean. Data were inspected for outliers; none were identified. To create equivalent scores on age-appropriate scales, attention control, inhibitory control, ego-resilience, and the two treatment-related anxiety scores were standardized within each of the three age groups and combined to create a single distribution of scores for each variable.
Missing data within the sample of 147 were estimated using full information maximum likelihood (FIML) procedures in Mplus. FIML procedures include all cases for analysis with available statistical information utilized to estimate parameters. These estimates are unbiased when data are missing at random. There were no differences on variables collected at the baseline assessment when comparing parents who completed each follow-up assessment with those who did not complete each follow-up assessment, suggesting that data were missing at random. Overall model fit was examined with multiple fit indices including Chi-square, ratio of Chi-Square to degrees of freedom, RMSEA, and CFI. Individual direct paths and indirect paths connecting the two facets of effortful control to treatment-related anxiety were also tested for statistical significance.
As we were interested in examining whether the model of associations between the two facets of effortful control, ego-resilience, distress, and treatment-related anxiety differed for boys and girls, we examined group invariance in the overall path model. An unconstrained model where focal path coefficients were allowed to vary across male and female subgroups was compared with a model where these path coefficients were constrained to be equal. The chi-square difference test was used to compare the chi-square and degrees of freedom for the two models (unconstrained vs. constrained) to determine whether constraining the focal path coefficients affected model fit.
RESULTS
Descriptive Statistics and Bivariate Correlations
Table 2 presents means, standard deviations, and ranges for study variables. Table 3 presents bivariate correlations among these variables. Older children were less distressed during treatment procedures, and higher levels of parent neuroticism were associated with lower levels of ego-resilience and greater treatment-related anxiety at 3-month and 9-month follow-ups. None of the other potential covariates were associated with the hypothesized mediators or with treatment-related anxiety at either follow-up. Therefore, only child age and parent neuroticism were included as covariates in the path analyses described below.
Table 2.
Descriptive Statistics
| N | M | SD | Range | |
|---|---|---|---|---|
| Parent Neuroticism (Baseline Assessment) | 147 | 0 | 0.91 | −1.70 to 2.96 |
| Attention Control (Baseline Assessment) | 147 | 0 | 0.99 | −2.87 to 2.60 |
| Inhibitory Control (Baseline Assessment) | 147 | 0 | 0.99 | −2.45 to 2.13 |
| Ego-Resilience (Baseline Assessment) | 147 | 0 | 0.99 | −2.36 to 2.20 |
| Distress (Treatment Assessments) | 123 | 0 | 0.43 | −.58 to 1.06 |
| Total Time in Treatment at 3-Month Follow-Up | 128 | 9.92 | 4.13 | 5.06 to 24.02 |
| Treatment-related Anxiety at 3-Month Follow-Up | 125 | 65.57 | 24.63 | 4.17 to 100 |
| Treatment-related Anxiety at 9-Month Follow-Up | 107 | 72.47 | 24.19 | 0 to 100 |
Table 3.
Bivariate Correlations
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Child Age | ||||||||||
| 2. Child Gender | −.11 | |||||||||
| 3. Time in Treatment | .03 | .08 | ||||||||
| 4. Family SES | .06 | .08 | −.09 | |||||||
| 5. Parent Neuroticism | .03 | −.08 | .08 | −.18* | ||||||
| 6. Attention Control | −.00 | .16 | −.09 | .19* | −.19* | |||||
| 7. Inhibitory Control | .02 | .08 | −.09 | .26** | −.23** | .58** | ||||
| 8. Ego-Resilience | −.04 | .08 | .05 | .08 | −.36** | .41** | .35** | |||
| 9. Distress | −.51** | .10 | .05 | −.04 | −.05 | −.19* | −.12 | .00 | ||
| 10. Treatment-Related Anxiety (3 Months) | −.01 | .03 | .09 | −.06 | −.21* | .03 | −.03 | .27** | −.23* | |
| 11. Treatment-Related Anxiety (9 Months) | .09 | .08 | .16 | .20* | −.25* | .12 | .11 | .19* | −.19 | .57** |
p<.05;
p<.01.
SES=Socioeconomic Status.
Both attention control and inhibitory control were significantly correlated with children’s ego-resilience. Higher attention control (but not inhibitory control) was correlated with less child distress during procedures (p<.05). Attention control was not significantly correlated with treatment-related anxiety at the 3-month and 9-month follow-ups. Ego-resilience and distress were not correlated with each other. However, ego-resilience was correlated with lower levels of treatment-related anxiety (p<.01), and distress was correlated with higher levels of treatment-related anxiety (p<.05) at 3-month follow-up. Ego-resilience was also correlated with lower levels of treatment-related anxiety at the 9-month follow-up (p<.05).
Path Models
An initial path model explored whether attention control and inhibitory control each independently contributed to ego-resilience, distress, and treatment-related anxiety. Inhibitory control did not predict these constructs in the initial model. Therefore, inhibitory control was not included in subsequent models.
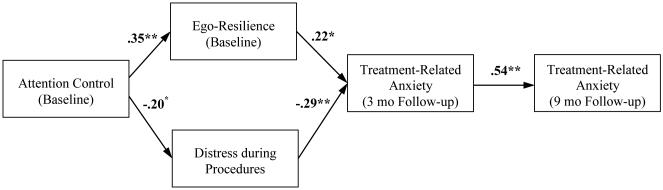
The model presented in Figure 1 allowed us to examine the hypotheses that attention control would directly predict both ego-resilience and lower distress and that ego-resilience and lower distress would both directly predict treatment-related anxiety at 3-month follow up. Moreover, the model allowed us to examine indirect paths from attention control to treatment-related anxiety at 3-month follow-up. The model also included a direct path from treatment-related anxiety at 3-month follow-up to treatment-related anxiety at 9-month follow-up. The model also included paths from the covariates (i.e., child age and parent neuroticism) to ego-resilience, distress, and treatment-related anxiety. In the interest of clarity, paths including covariates are not shown in the figure.
Figure 1.
Path Model Linking Attention Control to Treatment-Related Anxiety.
Note. Standardized path coefficients are presented in the figure. Controls for child age and parent neuroticism.
* p < .05. ** p < .01
The indices showed good fit for the model shown in Figure 1, χ2 (5)=6.34, p>.05, RMSEA=.04, and CFI=.99. All of the standardized parameter estimates for the direct paths shown in Figure 1 were statistically significant. We evaluated the statistical significance of the focal indirect pathways with the Model Indirect command in Mplus that uses the Delta method to test the statistical significance of indirect effects.28 The indirect path from attention control to treatment-related anxiety via ego-resilience was statistically significant, z=2.23, p<.05. The indirect path from attention control to treatment-related anxiety via distress was also statistically significant, z=2.00, p<.05. In addition, the indirect paths from ego-resilience and distress to treatment-related anxiety at 9-month follow-up via treatment-related anxiety at 3-month follow-up were statistically significant (z=2.35, p<.05 for ego-resilience and z=−2.81, p<.05 for distress).
When we reran the model shown in Figure 1 restricting the analysis to children with Acute Lymphoblastic Lymphoma (ALL; n = 117), model fit continued to be good χ2 (5)=6.38, p>.05, RMSEA=.05, and CFI=.99. Moreover, all pathways shown in Figure 1 continued to be statistically significant, with the exception of a marginally significant path from ego resilience to treatment-related anxiety at 3-month follow-up (p = .05). The indirect path from distress to treatment-related anxiety at 9-month follow-up via treatment-related anxiety at 3-month follow-up was statistically significant, and all other indirect paths were marginally significant (all ps < .08).
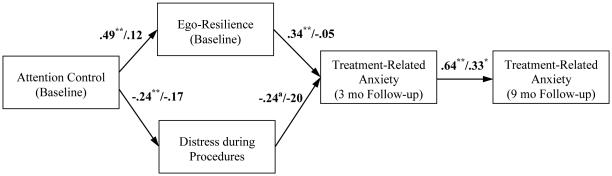
Child Gender as a Moderator
In order to explore child gender as a moderator, subgroup models comparing boys and girls were evaluated. These models included the same focal and covariate paths as the initial model linking attention control to treatment-related anxiety. In the unconstrained multi-group model, three of the five direct paths were statistically significant among boys but not among girls (see Figure 2). Furthermore, among boys, predictors in the model explained 28.1% of the variance in treatment-related anxiety at 3-month follow-up and 47.5% of the variance in treatment-related anxiety at 9-month follow-up. In contrast, among girls, predictors in the model explained 4.6% and 11.6% of the variance in treatment-related anxiety at 3-month and 9-month follow-ups, respectively.
Figure 2.
Unconstrained Path Models Linking Attention Control to Treatment-Related Anxiety.
Note. Standardized path coefficients for boys (first coefficient) and girls (second coefficient) are presented in the figure. Controls for child age and parent neuroticism.
a p<.07. * p < .05. ** p < .01
To directly examine gender as a moderator of the model shown in Figure 2, we compared the constrained model (which assumes no moderating influence of child gender) to an unconstrained model (which assumes differences across the moderating variable). The former (constrained) model had poorer model fit relative to the unconstrained model (Δχ²=15.06, Δdf=5, p<.05). This suggests that child gender impacts the overall fit of this model. To follow up, we evaluated child gender as a moderator of the five individual paths shown in Figure 2 by comparing separate models that constrained a single path (e.g., attention control to ego-resilience) to an unconstrained model. Constrained models had significantly poorer model fit relative to the unconstrained model when constraining the individual paths from attention control to ego-resilience and from ego-resilience to treatment-related anxiety at 3-month follow-up (Δχ²=4.80, Δdf=1, p<.05 and Δχ²=4.98, Δdf=5, p<.05 for these two paths, respectively). These tests provide evidence that the two paths involving ego-resilience were significantly stronger for boys than for girls. In line with this finding, in the unconstrained model, the indirect pathway from attention control to treatment-related anxiety at 3-month follow-up via ego-resilience was statistically significant among boys (z=2.91, p.01) but not among girls (z=−.27, p>.05).
DISCUSSION
Pediatric cancer patients differ in their immediate and longer-term responses to the invasive and stressful treatment procedures they must receive. The present study’s first goal was to examine the hypotheses that higher levels of attention control would be associated with higher levels of ego-resilience, less distress during procedures, and lower levels of longer-term treatment-related anxiety. The hypotheses were partially supported; higher attention control was associated with higher ego-resilience and less distress during treatment procedures, but not longer-term treatment-related anxiety. Inhibitory control was only related to ego-resilience. Thus, it appears that only attention control plays a unique role in children’s responses to treatment procedures.
Although this finding primarily speaks to the role of individual differences in children’s responses to cancer treatments, it may also inform strategies to reduce children’s distress during these treatments. For example, using distraction techniques such as imagery or deep breathing to direct the child’s attention away from potentially distressing stimuli is viewed as a key component of cognitive-behavioral approaches to managing procedure-related pain and fears.29 There is also promising evidence about the benefits of mindfulness interventions, which also focus attention while discouraging avoidance of emotions, in non-cancer child populations.30 Our findings support the value of continuing to evaluate the efficacy of such techniques. However, our findings also show that that children with lower levels of attention control are more prone to experiencing distress during procedures. Thus, these vulnerable children may require extra support to benefit from these distraction techniques. Given that parents’ neuroticism is related to children’s treatment-related anxiety, it is also important to consider how to support vulnerable parents in promoting children’s distraction and their broader adjustment to cancer treatment.
To address the study’s second goal, we tested a path model in which ego-resilience and child distress separately mediated the path from attention control to longer-term treatment-related anxiety. The results confirm the validity of this conceptualization of how temperament can affect longer-term treatment-related anxiety among pediatric cancer patients. It seems that lower levels of attention control can undermine both children’s ability to “bounce back” from general life stressors as well as their emotional responses during specific treatment procedures. The support for these dual pathways is especially noteworthy because ego-resilience and distress during treatment procedures were not correlated, suggesting they are two independent pathways leading from difficulty managing attention to longer-term anxiety about treatment. From a clinical perspective, multiple pathways of influence increase the potential benefit and impact of an intervention. Rather than increasing ego-resilience or reducing distress alone, our findings show that improving attention control can have a beneficial impact on ego-resilience and distress. Multiple pathways of influence also suggests that even if one pathway is not impacted, increasing a child’s attention control can still have the intended effect of reducing longer-term treatment-related anxiety.
In the third goal, we explored the moderating effects of child gender on the magnitude of these associations. The results suggest that gender does have a moderating role. Specifically, the indirect pathway from attention control to treatment-related anxiety via ego-resilience was supported for boys, but this pathway was non-significant among girls. There are not many studies of gender differences in associations between temperament and personality, but these findings are consistent with work by Eisenberg et al17 showing stronger associations between aspects of temperament and personality among at-risk boys relative to girls. There were no mean-level differences between boys and girls on the constructs at the baseline assessment, suggesting that differences in the results cannot be explained by initial gender differences. Thus, for boys, the ability to manage and redirect attention is an especially crucial element of their capacity to respond adaptively to the stress of cancer treatments. It further suggests that distraction may be especially effective with male pediatric cancer patients and that perhaps earlier intervention that targets their ability to effectively respond to new situations may be an especially effective approach to preventing their treatment-related anxiety.
Limitations and Future Directions
Although the findings also provide new insights into the associations between attention control, ego-resilience, distress during treatment procedures, and longer-term treatment-related anxiety, they should be interpreted in light of several limitations. First, parents provided the reports of children’s effortful control, ego-resilience, and treatment-related anxiety, therefore raising the possibility that the magnitude of associations was due to common method variance. However, the distress factor score based on multiple informants—child, observer, nurse, and parent—was also associated with attention control and treatment-related anxiety, suggesting that, despite parents being the only reporting source for most constructs, their reports generally correspond to other informants’ reports. Nonetheless, the findings might have been strengthened had other informants, such as teachers or the older children, provided reports of effortful control and ego-resilience. Older children could also provide reports of their longer-term treatment-related anxiety.
A second limitation involves our power to detect effects in the exploratory gender moderation analyses. Sample size in this study was larger than most other prospective longitudinal studies on children in active treatment for cancer. However, in an absolute sense, our sample was not large. Even though there was adequate power to detect the strong indirect pathway from attention control to treatment-related anxiety via ego-resilience for boys, the other indirect pathway from attention to control to treatment-related anxiety via distress was non-significant when analyzed separately for boys and girls. The modest sample size warrants caution when interpreting the findings, especially those from the exploratory analyses of moderation.
Lastly, it was not possible to recruit families at the time treatment began. Prior work with this population showed that parents were too overwhelmed and distressed at the time of their child’s diagnosis to be recruited to a behavioral (i.e., non-therapeutic) study. Thus, assessment of children’s temperament and personality occurred after treatment began, and their effortful control and ego-resilience may have been influenced by the initial diagnosis and early treatment. Future research could ask parents to report on whether children’s current temperament and personality is in line with their usual, pre-diagnosis temperament and personality. We also did not assess children’s treatment-related anxiety at the beginning of treatment. Had we been able to assess and control for treatment-related anxiety very early in the course of the cancer treatment procedures, we could have conducted a more stringent test of the associations between facets of effortful control, ego-resilience, distress during treatment procedures, and subsequent treatment-related anxiety. Thus, we are only able to speculate about absolute levels and not changes over time in longer-term treatment-related anxiety.
Several important research questions remain. One question is whether distress during specific types of treatment procedures has an especially robust impact on longer-term anxiety. Given our relatively small sample size and the diversity of treatment procedures, we were not able to directly address this question in the current study. A second question concerns gender differences in how temperament and personality are related and how they may affect children’s responses to stressful events. As noted above, the relatively small sample size in the test of moderation allows only speculation about any specific gender differences. However, these initial findings suggest that more research is needed on gender as a moderator of how children with cancer respond to stressful events. Future research should also consider other moderators of adjustment to cancer treatment such as a birth order. Another potential issue is the durability of the effects identified. The period of time covered in this longitudinal study of cancer exceeded one year. However, increasingly large numbers of pediatric cancer patients are surviving ten years or longer after treatment ends. Future research could benefit from investigating longer-term outcomes of effortful control, ego-resilience, and distress during treatment to establish whether associations with anxiety persist during the survivorship phase.
In terms of clinical implications, these findings support the use of evidence-based approaches for treatment-related distress that involve redirecting the child’s attention. However, individual differences in the effectiveness of such interventions have received relatively little attention. An assessment of a child’s self-regulatory skills prior to implementing these techniques may offer information about the child’s likelihood of benefitting from interventions. Assessment tools should be developed to measure specific aspects of attention control and self-regulation that are especially relevant to treatment procedures and anxiety related to medical conditions.
Consideration of a child’s gender and chronological age are likely also relevant factors when implementing interventions. Increasing researchers’ and clinicians’ understanding of individual differences in predictors of anxiety and distress during treatment procedures can enhance efforts to provide effective, personalized approaches that meet children’s and parents’ needs during cancer treatment and reduce immediate and longer-term treatment anxiety.
Acknowledgments
This work is part of a larger investigation of caregivers’ influence on child coping with cancer treatment and was supported by the National Cancer Institute at the National Institutes of Health (NCI#1R01CA138981; PI: L. Penner) and The Herrick Foundation (PI: L. Penner).
Footnotes
The authors have no conflicts of interest.
REFERENCES
- 1.Hildenbrand AK, Clawson KJ, Aderfer MA, et al. Coping with pediatric cancer: strategies employed by children and their parents to manage cancer-related stressors during treatment. J Pediatr Oncol Nurs. 2011;28:344–354. doi: 10.1177/1043454211430823. [DOI] [PubMed] [Google Scholar]
- 2.Hedstrom M, Haglund K, Skolin I, et al. Distressing events for children and adolescents with cancer: child, parent, and nurse perceptions. J Pediatr Oncol Nurs. 2003;20:120–132. doi: 10.1053/jpon.2003.76. [DOI] [PubMed] [Google Scholar]
- 3.Zebrack BJ, Zeltzer LK, Whitton J, et al. Psychological outcomes in long-term survivors of childhood leukemia, Hodgkin's disease, and non-Hodgkin's lymphoma: a report from the Childhood Cancer Survivor Study. Pediatrics. 2002;110:42–52. doi: 10.1542/peds.110.1.42. [DOI] [PubMed] [Google Scholar]
- 4.Harper FWK, Penner LA, Peterson A, et al. Children's positive dispositional attributes, parents' empathic responses, and children's responses to painful pediatric oncology treatment procedures. J Psychosoc Oncol. 2012;30:593–613. doi: 10.1080/07347332.2012.703771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Penner LA, Cline RJW, Albrecht TL, et al. Parents' empathic responses and pain and distress in pediatric patients. Basic Appl Soc Psych. 2008;30:102–113. doi: 10.1080/01973530802208824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rothbart MK. Temperament, development, and personality. Curr Dir in Psychol Sci. 2007;16:207–212. [Google Scholar]
- 7.Eisenberg N, Smith CL, Spinrad TL. Effortful Control: Relations with emotion regulation, adjustment, and socialization in childhood. In: Vohs KD, Baumeister RF, editors. Handbook of Self-Regulation. 2nd The Guilford Press; New York: 2011. pp. 263–283. [Google Scholar]
- 8.Garon N, Bryson SE, Smith IM. Executive function in preschoolers: a review using an integrative framework. Psychol Bull. 2008;134:31–60. doi: 10.1037/0033-2909.134.1.31. [DOI] [PubMed] [Google Scholar]
- 9.Meesters C, Muris P, van Rooijen B. Relations of neuroticism and attentional control with symptoms of anxiety and aggression in non-clinical children. J Psychopathol Behav Assess. 2007;29:149–158. [Google Scholar]
- 10.Muris P, Meesters C, Blijlevens P. Self-reported reactive and regulative temperament in early adolescence: relations to internalizing and externalizing problem behavior and "big three" personality factors. J Adolesc. 2007;30:1035–1049. doi: 10.1016/j.adolescence.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Block JH, Block J. The role of ego-control and ego-resiliency in the organization of behavior. In: Collins WA, editor. The Minnesota Symposia on Child Psychology. Vol. 13. Erlbaum; Hillsdale, NJ: 1980. pp. 39–101. [Google Scholar]
- 12.Eisenberg N, Spinrad TL, Fabes RA, et al. The relations of effortful control and impulsivity to children's resiliency and adjustment. Child Dev. 2004;75:25–46. doi: 10.1111/j.1467-8624.2004.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harper FWK, Goodlett BD, Trentacosta CJ, et al. Temperament, personality, and quality of life in pediatric cancer patients. J Pediatr Psychol. 2014 doi: 10.1093/jpepsy/jst141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salmon K, Pereira JK. Predicting children's response to an invasive medical investigation: the influence of effortful control and parent behavior. J Pediatr Psychol. 2002;27:227–233. doi: 10.1093/jpepsy/27.3.227. [DOI] [PubMed] [Google Scholar]
- 15.Else-Quest NM, Hyde JS, Goldsmith HH, et al. Gender differences in temperament: a meta-analysis. Psychol Bull. 2006;132:33–72. doi: 10.1037/0033-2909.132.1.33. [DOI] [PubMed] [Google Scholar]
- 16.Katz ER, Kellerman J, Siegel SE. Behavioral distress in children with cancer undergoing medical procedures: developmental considerations. J Consult Clin Psychol. 1980;48:356–365. doi: 10.1037//0022-006x.48.3.356. [DOI] [PubMed] [Google Scholar]
- 17.Eisenberg N, Haugen R, Spinrad TL, et al. Relations of temperament to maladjustment and ego resiliency in at-risk children. Soc Dev. 2010;19:577–600. doi: 10.1111/j.1467-9507.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothbart MK, Ahadi SA, Hershey KL, et al. Investigations of temperament at three to seven years: the Children's Behavior Questionnaire. Child Dev. 2001;72:1394–1408. doi: 10.1111/1467-8624.00355. [DOI] [PubMed] [Google Scholar]
- 19.Simonds J, Rothbart MK. The Temperament in Middle Childhood Questionnaire (TMCQ): A computerized self-report measure of temperament for ages 7-10; Poster presented at: Occasional Temperament Conference; Athens, GA: 2004. [Google Scholar]
- 20.Ellis LK, Rothbart MK. Early Adolescent Temperament Questionnaire - Revised Parent Report. University of Oregon; Eugene, OR: 1999. [Google Scholar]
- 21.Patenaude AF, Kupst MJ. Psychosocial functioning in pediatric cancer. J Pedatr Psychol. 2005;30(1):9–27. doi: 10.1093/jpepsy/jsi012. [DOI] [PubMed] [Google Scholar]
- 22.Klassen AF, Anthony SJ, Khan A, et al. Identifying determinants of quality of life of children with cancer and childhood cancer survivors: a systematic review. Support Care Cancer. 2011;19:1275–1287. doi: 10.1007/s00520-011-1193-x. [DOI] [PubMed] [Google Scholar]
- 23.Varni JW, Burwinkle TM, Katz ER. The PedsQL in pediatric cancer pain: a prospective longitudinal analysis of pain and emotional distress. J Dev Behav Pediatr. 2004;25:239–246. doi: 10.1097/00004703-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Spielberger C. State Trait Anxiety Inventory for Adults. Mind Garden; Redwood, CA: 1977. [Google Scholar]
- 25.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 26.Wong DL, Baker CM. Pain in children: comparison of assessment scales. Paediatr Nurs. 1988;14:9–17. [PubMed] [Google Scholar]
- 27.Mplus [Statistical Program]. Version 7.31. Muthen & Muthen; Los Angeles, CA: 2015. [Google Scholar]
- 28.Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological Methodology 1982. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- 29.Powers SW. Empirically supported treatments in pediatric psychology: Procedure related pain. J Pediatr Psychol. 1999;24:131–145. doi: 10.1093/jpepsy/24.2.131. [DOI] [PubMed] [Google Scholar]
- 30.Black DS, Fernando R. Mindfulness training and classroom behavior among lower-income and ethnic minority elementary school children. J Child Fam Stud. 2014;23:1242–1246. doi: 10.1007/s10826-013-9784-4. [DOI] [PMC free article] [PubMed] [Google Scholar]