Abstract
Aim of database
Danish Breast Cancer Cooperative Group (DBCG), with an associated database, was introduced as a nationwide multidisciplinary group in 1977 with the ultimate aim to improve the prognosis in breast cancer. Since then, the database has registered women diagnosed with primary invasive nonmetastatic breast cancer. The data reported from the departments to the database included details of the characteristics of the primary tumor, of surgery, radiotherapy, and systemic therapies, and of follow-up reported on specific forms from the departments in question.
Descriptive data
From 1977 through 2014, ~110,000 patients are registered in the nationwide, clinical database. The completeness has gradually improved to more than 95%. DBCG has continuously prepared evidence-based guidelines on diagnosis and treatment of breast cancer and conducted quality control studies to ascertain the degree of adherence to the guidelines in the different departments.
Conclusion
Utilizing data from the DBCG database, a long array of high-quality DBCG studies of various designs and scope, nationwide or in international collaboration, have contributed to the current updating of the guidelines, and have been an instrumental resource in the improvement of management and prognosis of breast cancer in Denmark. Thus, since the establishment of DBCG, the prognosis in breast cancer has continuously improved with a decrease in 5-year mortality from ~37% to 15%.
Keywords: breast cancer, database, guidelines, quality control, research
Introduction
The Danish Breast Cancer Cooperative Group (DBCG) was established as a nationwide multidisciplinary organization in 1977 on the initiative from the Danish Surgical Society. According to the statutes,1 the organization comprises all the departments in Denmark responsible for diagnosis, treatment, follow-up, and research in breast cancer and includes a central database.
The ultimate aim of the organization was to offer similar nationwide diagnostic and therapeutic procedures to all patients with primary breast cancer and to improve the prognosis.2
Study population
From 1977 through 2014, ~110,000 women with early unilateral nonmetastastic invasive breast cancer have been entered into the database.
The completeness of the database has gradually improved from ~80% early on to ~95% since the mid-nineties according to comparison with the Danish Cancer Registry3 and, since its establishment in 1999, the National Pathology Registry.4
In the case of bilateral cancer, a detailed registration is restricted to the most advanced tumor. Men with breast cancer and women with a second primary breast cancer are not registered.
The DBCG database is linked to the Civil Registration System5 to obtain vital status and to the National Pathology Registry to monitor the completeness of the reporting to DBCG. In addition, there are occasional linkages to the Danish Cancer Registry to monitor the presence of other malignant diseases and second primaries and to the Danish National Patient Registry to monitor comorbidity and late adverse events.
Main variables and follow-up
Data reported from the departments to the database include data concerning diagnostic procedures, surgery, radiation therapy, and systemic therapy, as well as clinical follow-up for up to 10 years, as specified in Table 1. A more detailed description of the data is presented in the DBCG home page.1
Table 1.
Main variables reported to the DBCG database
| Main groups | Variables |
|---|---|
| Patient characteristics | Age, menopausal status, comorbidity |
| Reasons not to enter standard treatment program for primary breast cancer | Distant metastases, previous malignant disease (except cancer cutis/cancer colli uteri in situ), bilateral breast cancer, technically inoperable or not operated according to guidelines, patient preference |
| Tumor characteristics | Histological diagnosis, tumor size, number of examined nodes, number of positive nodes, grade, ER status, HER-2 status |
| Surgery | Type of preoperative biopsy, sentinel node biopsy, axillary dissection, lumpectomy +/− oncoplastic surgery, mastectomy +/− reconstruction |
| Adjuvant therapy | Radiotherapy, chemotherapy, endocrine therapy, anti-HER-2 therapy |
| Follow-up | Vital status, recurrence, contralateral breast cancer, other malignant disease |
Abbreviations: DBCG, Danish Breast Cancer Cooperative Group; ER, estrogen receptor; HER-2, human epidermal growth factor receptor 2.
Data are reported to the database from the departments of pathology, surgery, and oncology according to a number of forms prepared for the departments in question. Queries are sent to the departments if reporting is missing according to the guidelines indicated on the forms, or if the database receives forms from one discipline (for instance, pathology), but not from the corresponding discipline (for instance, surgery or oncology). In 2006, the National Clinical Quality Database for Breast Cancer was established, headed by a group with representation from DBCG, the Registry Support Center of Clinical Quality and Health Informatics East and the Registry Support Center of Epidemiology and Biostatistics North, and each of the five Danish regions. Based on the data reported to DBCG complemented by data from the Danish Pathology Registry and the Danish National Patient Registry, the group annually reports the quality of a number of indicators (Table 2) used to monitor the quality of diagnosis and management of breast cancer, nationwide and between the hospitals. This is reported monthly directly to the hospitals and published yearly in a comprehensive report (in Danish: Kvalitetsindikatorrapport for Brystkræft).1 The most recent report is for the year 2014 and concludes that the treatment of breast cancer in Denmark meets the quality objectives but insufficient reporting of data on systemic treatment remains an important issue.
Table 2.
Quality indicators in DBCG, 2014
| Indicator, proportion of | Observed value (%) | Reference value (%) |
|---|---|---|
| Surgical intervention for malignant disease | 79 | ≥67 |
| Patients with axillary lymph node status determined with the SN technique | 97 | >95 |
| Patients with ten or more nodes excised in axillary dissection | 96 | >95 |
| Patients with complete reporting of data | 92 | >95 |
| High-risk patients allocated to adjuvant treatment according to the guidelines | 89 | –a |
| Patients completing the follow-up program according to the guidelines | 82 | >95 |
| Patients with local recurrence within 5 years following lumpectomy | 1.6 | <7 |
| Patients with reoperation due to surgical complications | 3 | –b |
| Patients without late SN positivity | 96c | –d |
| Patients receiving radiotherapy according to the guidelines | 97 | >95 |
Notes:
Because allocation depends upon patient preference and practice of information;
no international consensus;
preoperative frozen microscopy on SN is negative but later microscopy is positive;
no prior specification of standard.
Abbreviations: DBCG, Danish Breast Cancer Cooperative Group; SN, sentinel node.
Research
Throughout the years, the reported data have been used to assess the quality of potential prognostic and predictive factors and surgical and oncological procedures to ensure similar quality on a nationwide basis.
Through numerous national and international studies, DBCG has contributed to an improvement of the evidence-based guidelines for diagnostic aspects and treatment. The results achieved by DBCG have been published in 430 peer-reviewed papers,1 and the data have contributed to several theses and to the meta-analyses conducted by Early Breast Cancer Triallists’ Collaborative Group.6,7
In the following section, we present some examples of how DBCG studies, based on data reported to the database, have contributed to the refinement of the treatment of breast cancer.
Surgery
DBCG has been deeply engaged in the change in treatment strategy from mastectomy to breast-conserving surgery (BCS). Thus in 2008, DBCG published a randomized study which demonstrated similar outcomes in terms of local and distant recurrences and survival with BCS compared with mastectomy.2 Since then, the standard surgical treatment for breast cancer has gradually become BCS, which is now offered to ~70% of patients with primary breast cancer.
When BCS was introduced in the 1990s, at least 1 cm margin was recommended. Gradually, this has been reduced and since the 2009 St Gallen Consensus Conference, the Danish guidelines defined “no tumor on ink” as sufficient for invasive cancer and 2 mm free margin in case of ductal carcinoma in situ. Afterward, a study of ~12,000 patients registered in the database showed that the 2009 recommendations were well-supported by Danish data.8
Standard procedure for assessment of spread of the disease to the axillary lymph nodes was, until ~15 years ago, axillary lymph node dissection, and according to DBCG data an optimal node staging required at least ten nodes to be examined.9
According to international evidence, the sentinel node technique was introduced in Denmark on the initiative by DBCG. Requirements were set up by DBCG as concerns volume and quantity, and the individual departments were certified only after formal approval by DBCG monitors.10 The introduction of the sentinel node technique implies that a decreasing proportion of breast cancer patients are exposed to axillary dissection, which is omitted in the case of negative nodal status. Hereby the risk of late adverse effects in terms of pain, sensations, reduced mobility, and lymphedema is reduced.
Radiotherapy
Prior to 1977, treatment of primary breast cancer in the vast majority of cases consisted of mastectomy followed by radiotherapy. When the DBCG 77 program was introduced, the staging procedure was improved, and radiotherapy following mastectomy was restricted to patients with positive axillary nodes or a primary tumor exceeding 5 cm or deep invasion. In the following program (DBCG 82), DBCG tested the hypothesis of lack of effect by radiotherapy when administered in addition to systemic therapy. However, two large national studies demonstrated a significant reduction in the rate of local recurrence and improved survival.11
Due to lack of evidence, international practice differs as concerns radiation to the parasternal nodes as part of locoregional radiation. However, a recent very large Danish study demonstrated that additional radiation to the parasternal nodes was associated with a significant gain in terms of breast cancer mortality and overall survival.12
For some years, DBCG has conducted trials to evaluate the morbidity following reduction of the irradiated breast volume after breast conserving surgery and following hypofractionation (less numbers of fractions with higher dose per fraction) in patients eligible for irradiation of the residual breast only. Furthermore, DBCG recently launched a trial to evaluate morbidity associated with hypofractionation in patients eligible for locoregional radiation, with international participation.1
Systemic therapy
The postoperative (adjuvant) systemic therapy has been significantly developed since DBCG’s first program (DBCG 77) confirmed the hypothesis that this treatment strategy was associated with an improvement of the prognosis.
Since then, DBCG has launched a number of treatment programs, some of them as part of prospective studies or as result of retrospective analyses utilizing the data in the database. Due to the unselected patient materials and data collection, and the national quality assurance according to the guidelines, DBCG has been an attractive collaborator in several large international studies.13
The benefit of the systemic therapies has been steadily increasing and with the present treatment strategies, which in the individual patients may include one or more of the three treatment modalities; chemotherapy, endocrine therapy, and biological therapy, ~50% of the expected deaths can be avoided among the patients receiving the respective therapies.
Since the first DBCG treatment programs were introduced, the selection of the patients for systemic therapy has been according to classical prognostic factors, from the late eighties complemented with a predictive factor for endocrine therapy (estrogen receptor status) and from 2007 for biological therapy (human epidermal growth factor receptor 2 [HER2]-status). And more recently, by combining a number of factors, data from large cohorts of patients entering different DBCG programs have been utilized to better identify patients eligible for systemic therapy.14,15
The proportion of patients offered adjuvant systemic therapy has been increasing since the late seventies from ~50% to close to 90%. Obviously, with the present treatment strategies a large proportion of the patients are overtreated and DBCG is, like many other groups, heavily involved in the search for valid genomic assays to better identify the patients who are estimated to benefit from a specific treatment.
Improvement of the prognosis
When DBCG was established in 1977, the prognosis in breast cancer differed according to region of the country. Since then, the prognosis has improved and without regional differences. As appears from Figure 1, ~37% of patients diagnosed with breast cancer in the late seventies died within 5 years, but this figure has steadily dropped to ~15%. This can be ascribed among other factors to better quality of the surgical treatment, to earlier diagnosis, but especially to improved efficacy of the systemic treatment.16 More detailed analysis of the development of the survival in breast cancer including analysis of the age-adjusted relative survival since 1995 has recently been published.17 As appears from Figure 2, the relative survival improves in all the three categories of patients. Indeed, the 5-year survival in patients with node-negative disease is very similar to the survival in the background population.
Figure 1.
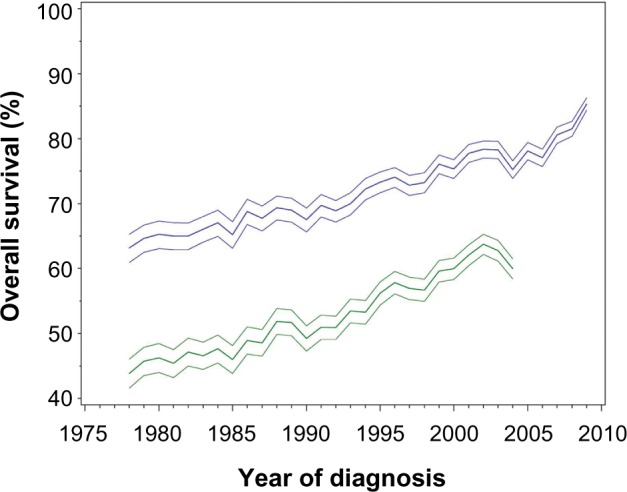
Overall survival ± 95% confidence intervals, 5 (upper curve) and 10 (lower curve) years after time of first diagnosis of invasive breast cancer in Denmark, 1978–2009 (N=94.579).
Figure 2.
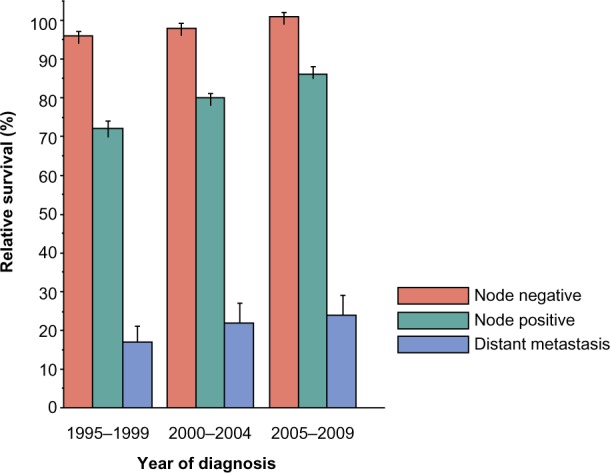
Age-adjusted 5-year relative survival according to stage in patients diagnosed with invasive breast cancer in Denmark during three consecutive time periods.
Administrative issues and funding
The successful implementation of quality control studies and the national and international scientific studies and the continuous revision of the guidelines according to new evidence can be ascribed to the multidisciplinary organization including all the departments responsible for diagnosis, treatment, follow-up, and research in breast cancer.
The budget of the central secretariat includes expenses for the operation of the database and salaries for the staff to manage the technical maintenance and development of the database, to manage the collaboration and communication between the departments and the different committees, to monitor the quality of the data reported to the database, and to edit revisions of the guidelines. Presently, the staff includes one statistician, one data manager, one secretary, and a halftime physician. Expenses to manage the research studies have been covered through external funding.
Until 1982, DBCG was financed from private sources; The Danish Health and Medicines Authority and the Finsen Institute. Thereafter, the DBCG was supported from the counties with a charge of ~1,100 Danish Krone (DKK) per newly registered patient equivalent to an annual budget in 2007 of ~4.4 million DKK. Since 2007, with the establishment of the Danish Regions, the financing has been from the regions, with a budget reduction of ~50%. Part of this reduction has been compensated for by staff reduction through reorganization from reporting of data to DBCG on paper to online electronic reporting of data to the database. However, it has been necessary via private funding to finance the optimization of the data in the database, which is a prerequisite to use the data for research.
Conclusion
The DBCG database provides data to a vast array of both clinical and epidemiological studies. The quality of the data is consecutively assessed by the clinical quality indicators, and studies utilizing the data have contributed substantially to the evidence-based guidelines on diagnosis and treatment of breast cancer prepared by DBCG. Furthermore, DBCG has through quality control studies continuously ascertained the degree of adherence to the guidelines in Denmark. Since the establishment of DBCG, the prognosis in breast cancer has continuously improved with a decrease in 5-year mortality from ~37% to 15%.
Acknowledgments
This paper was funded by the Program for Clinical Research Infrastructure (PROCRIN) established by the Lundbeck Foundation and the Novo Nordisk Foundation and administered by the Danish Regions.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Danish Breast Cancer Cooperative Group [homepage on the Internet] Copenhagen: Statutter [updated 2013 May 23; cited 2016 Jan 30] [Accessed January 31, 2016]. Available from http://www.dbcg.dk/
- 2.Blichert-Toft M, Christiansen P, Mouridsen HT. Danish Breast cancer Cooperative Group-DBCG. History, organization, and status of scientific achievements at 30-year anniversary. Acta Oncol. 2008;47(4):497–505. doi: 10.1080/02841860802068615. [DOI] [PubMed] [Google Scholar]
- 3.Gjerstorff ML. The Danish Cancer Registry. Scand J Public Health. 2011;39:42–45. doi: 10.1177/1403494810393562. [DOI] [PubMed] [Google Scholar]
- 4.Bjerregaard B, Larsen OB. Patology Register. Scand J Public Health. 2011;39:72–74. doi: 10.1177/1403494810393563. [DOI] [PubMed] [Google Scholar]
- 5.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39:22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 6.EBCTCG (Early Breast Cancer Triallists’ Collaborative Group) Effects of chemotherapy and hormonal therapy on local recurrences and on 15-year survival. An overview of randomized trials. Lancet. 2005;365(9472):1687–1717. doi: 10.1016/S0140-6736(05)66544-0. [DOI] [PubMed] [Google Scholar]
- 7.EBCTCG (Early Breast Cancer Triallists’ Collaborative Group) Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and on 15-year survival. An overview of randomized trials. Lancet. 2005;366(9503):2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 8.Bodilsen A, Bjerre K, Offersen BV, et al. Importance of margin width in breast conserving treatment of early breast cancer: a Danish Breast Cancer Cooperative Group study of 11,900 women. J Surg Oncol. 2016 Mar 16; doi: 10.1002/jso.24224. Epub. [DOI] [PubMed] [Google Scholar]
- 9.Axelsson CK, Mouridsen HT, Zedeler K. Axillary dissection of level l and ll lymph nodes is important in breast cancer classification. Eur J Cancer. 1992;28A(8–9):1415–1418. doi: 10.1016/0959-8049(92)90534-9. [DOI] [PubMed] [Google Scholar]
- 10.Friis E, Galatius H, Garne JP. Organized nation-wide implementation of sentinel lymph node biopsy in Denmark. Acta Oncol. 2008;47(4):556–560. doi: 10.1080/02841860802010732. [DOI] [PubMed] [Google Scholar]
- 11.Overgaard M, Christensen JJ. Postoperative radiotherapy in DBCG during 30 years. Techniques, indications and clinical radiobiological experience. Acta Oncol. 2008;47(4):639–653. doi: 10.1080/02841860802078085. [DOI] [PubMed] [Google Scholar]
- 12.Thorsen LBJ, Berg HJ, Brodersen H, et al. Improved survival with internal mammary node irradiation: a prospective study on 3072 patients. Radiother Oncol. 2014;111(Suppl 1):S57. [Google Scholar]
- 13.Møller S, Jensen M-B, Ejlertsen B, et al. The clinical database of the Danish Breast Cancer Cooperative Group (DBCG); its 30-years experience and future promise. Acta Oncol. 2008;47(4):506–524. doi: 10.1080/02841860802059259. [DOI] [PubMed] [Google Scholar]
- 14.Christiansen P, Bjerre K, Ejlertsen B, et al. Mortality rates among early-stage hormone receptor-positive breast cancer patients: a population-based cohort study in Denmark. J Natl Cancer Inst. 2011;102(18):1363–1372. doi: 10.1093/jnci/djr299. [DOI] [PubMed] [Google Scholar]
- 15.Ejlertsen B, Jensen M-B, Mouridsen HT. Excess mortality in postmenopausal high-risk women who only receive adjuvant endocrine therapy for estrogen receptor positive breast cancer. Acta Oncol. 2014;53(2):174–185. doi: 10.3109/0284186X.2013.850738. [DOI] [PubMed] [Google Scholar]
- 16.Mouridsen HT, Bjerre KD, Christiansen P, Jensen M-B, Møller S. Improvement of prognosis in breast cancer in Denmark 1977-2006 based on the nationwide reporting to the DBCG-registry. Acta Oncol. 2008;47(4):525–536. doi: 10.1080/02841860802027009. [DOI] [PubMed] [Google Scholar]
- 17.Christiansen P, Jensen MB. Databasernes Fællessekretariat, editor. DMCG.dk Benchmarking Consortium. Breast Cancer 1995–2012. 2014. [Accessed January 31, 2016]. Chapter 3. Available from: http://dmcg.dk/dmcgdk-benchmarking-consortium/


