Abstract
Aim of the database
The steering committee of the Danish Hysterectomy and Hysteroscopy Database (DHHD) has defined the objective of the database: the aim is firstly to reduce complications, readmissions, reoperations; secondly to specify the need for hospitalization after hysterectomy; thirdly to secure quality assessment of hysterectomy and hysteroscopy by setting standards and national guidelines; and finally to intensify the monitoring of laparoscopic surgery and explore long-term side effects after hysterectomy.
Study population
We include all women in Denmark who have had elective benign uterine surgery since 2003. The surgery includes hysterectomy and operative hysteroscopy. In the latter, we include resection of the endometrium and submucosal leiomyomas and ablations of the endometrium.
Main variables
Detailed information about the hysterectomy and hysteroscopy operation techniques, cooperations, and indications is registered directly in the National Patient Register (NPR), as well as relevant lifestyle factors and confounders. It is mandatory to register information about complications and readmissions in the NPR. Data included in DHHD are directly extracted from the NPR.
Descriptive data
Annually approximately 4,300 hysterectomies and 3,200 operative hysteroscopies are performed in Denmark. Since the establishment of the database in 2003, 50,000 hysterectomies have been registered. DHHD’s nationwide cooperation and research have led to national guidelines and regimes. Annual national meetings and nationwide workshops have been organized.
Conclusion
The use of vaginal and laparoscopic hysterectomy methods has increased during the past decade and the overall complication rate and hospital stay have declined. The regional variation in operation methods has also decreased.
Keywords: epidemiology, laparoscopy, gynecology, complication, clinical quality register
Introduction
Each year in Denmark, 4,500 women undergo elective hysterectomy performed on benign indications, corresponding to a 10% lifetime risk for all Danish women.1 The procedure is most commonly performed due to abnormal menstrual bleeding, leiomyomas, descensus of the uterus, or abdominal pain.1
In 2002, a nationwide analysis of hospitalization, morbidity, and readmissions after elective benign hysterectomy was performed in Denmark. The results disclosed a surprisingly high rate of 18% for perioperative complications.2 This provided the impetus to establish the Danish Hysterectomy Database in 2003. The initial report from the database confirmed a high complication rate in 2004, with 8% bleeding complications, 4% infections, and 2% injuries on bladder, ureter, or intestine. Readmission occurred after 7% of the hysterectomies, and in 5% of the cases, reoperations were performed within 30 days after surgery.3
In 2011, the Danish Hysterectomy Database merged with the clinical database for hysteroscopies to form the Danish Hysterectomy and Hysteroscopy Database (DHHD). Each year in Denmark, 3,200 women undergo an elective operative hysteroscopy as a minimal invasive alternative to hysterectomy. Hysteroscopy has fewer complications than hysterectomy as shown in the hysteroscopy database.4 However, these methods are less efficient compared to hysterectomy as approximately 25% need a reoperation within the following 5 years.
A reduction of complications and need for reoperations following hysterectomy and hysteroscopy would not only improve the quality of life for the patients but also have a great influence on the national public health economy.5,6
Aim of the database
The objective of DHHD is firstly to reduce the complications, readmissions, and reoperations; secondly to specify the need for hospitalization; thirdly to secure quality assessment of hysterectomy and hysteroscopy by setting standards and national guidelines (benchmarking). Specified goals were set in 2003 and revised in 2013 (Table 1). In 2015, DHHD defined supplementary future aims of the database based on a national clinical guideline from the National Board of Health. The recommendations are to intensify the monitoring of the implementation of laparoscopic surgery and explore long-term side effects after hysterectomy. This currently covers descensus, urinary incontinence, vaginal cuff dehiscence, bowel obstruction, and herniation. Additionally, DHHD wishes to contribute to the implementation of updated, optimized, fast-track regimes through evidence-based national guidelines. DHHD annually hosts nationwide meetings for benchmarking, knowledge sharing, and rapid implementation of guidelines and necessary changes.
Table 1.
Danish Hysterectomy and Hysteroscopy Database: quality indicators, goals, and 10-year results
| Year | 2004 | 2005 | 2006 | 2010 | 2011–2012b | 2012–2013 | 2013–2014 | Goal 2003 | Goal 2013 |
|---|---|---|---|---|---|---|---|---|---|
| Hysterectomy per year (n) | 4,588 | 4,578 | 4,451 | 4,270 | 4,509 | 4,287 | 4,309 | – | – |
| Total complications – old indicator definition (%) | 19 | 17 | 18 | 18 | – | – | – | 6 | – |
| Total complications – new indicator definition (%)a | – | – | – | – | 16 | 15 | 14 | – | <12 |
| Readmissions (%) | 7 | 5 | 5 | 6 | – | – | – | 4 | – |
| Reoperations (%) | 5 | 4 | 4 | 5 | 4 | 4 | 3 | 3 | <2 |
| Length of hospital stay (days) | 2 | 2 | 2 | 2 | 1 | – | – | 2 | – |
| Major complications (%) | – | – | – | – | 8 | 7 | 7 | – | <5 |
| Postoperative bleeding complications (%) | – | – | – | – | 6 | 6 | 4 | – | <3 |
Notes:
The indicators were revised in 2011–2012, excluding pain and voiding problems as complications unless these symptoms are part of the indication for readmission and/or surgery.
From 2003 to 2011, the annual report followed the calendar year; from 2012, the period June 1–May 31. Data for 2007–2009 were excluded from the table, since both the overall complication rates and the frequencies of reoperations, readmissions, and length of hospital stay were stable during this period. The bold values represent observational data.
Study population
DHHD includes all women undergoing an elective hysterectomy performed on benign diagnoses in any hospital in Denmark, and all women undergoing an operative hysteroscopy, including resection of the endometrium or submucosal leiomyomas, and ablation of the endometrium. Benign indications include cervical dysplasia, endometrial hyperplasia without atypical cells, and exclude all malignancies. All information about diagnoses and operations is recorded in the National Patient Register (NPR), which is an administrative register covering all hospital procedures in Denmark.7 In the future, DHHD will include other alternatives to hysterectomy as well. Annually approximately 4,300 hysterectomies are registered in the DHHD in addition to approximately 3,200 hysteroscopic resections of the endometrium, submucosal leiomyomas, or ablations of the endometrium. Since the establishment of the database in 2003, detailed information of approximately 50,000 hysterectomies has been registered.8
Main variables
DHHD has defined supplementary codes for the NPR registration to cover not only the mandatory procedure and indication but also a range of relevant lifestyle factors and confounders. There has been a slight change in this registration over the past 10 years as the scientific focus of interest changes.
For each patient undergoing hysterectomy, we currently register indication, menopause status, comorbidity, smoking, alcohol usage, height, weight, method of hysterectomy, cooperations, specified techniques of how the uterus is removed and how suspension of the vaginal cuff is handled, uterus weight, intraoperative bleeding, duration of surgery, perioperative complications, and use of antibiotics, antithrombotics, and tranexamic acid. The surgeon marks all this information in a chart, and a secretary subsequently registers all the codes directly in NPR.
We have defined a list of national quality indicators with specified goals for hysterectomies presented in an extensive report each year under the Danish Clinical Registries (RKKP, homepage http://www.rkkp.dk/) – incidence of hysterectomy, operation method (eg, abdominal, vaginal, laparoscopic, and robotic) total versus subtotal hysterectomy, use of antibiotics and antithrombotics, length of hospital stay, perioperative complications within the first 30 days, readmissions, reoperations, and mortality.8 For each quality indicator, there is a specified set of NPR codes to be extracted directly from the NPR. Some of the complications are registered from 0 to 30 days, others only at readmissions, and finally the long-term complications up to 5 years postoperatively. The quality indicators and correlated goals concerning hysterectomy are listed in Table 1. Each department conducts a local validation of the registration every year.
Follow-up
Since 1977, all treatments performed at any Danish hospital have been registered in NPR and since 1995 all outpatients contacts. All data are individualized using a unique civil registration number assigned to all residents in Denmark by the Civil Registration System. Therefore, it is mandatory to register every readmission, reoperation, or other complications in NPR, so losses to follow-up are minimal. However, minor complications treated by general practitioners are not included, and thus minor complications might be underestimated. On the contrary, not all the diagnoses in the NPR are actually relevant as complications to hysterectomy. Thus, the major complication rate has been overestimated. This has been corrected during the validation process. Therefore, the follow-up indicators are to be interpreted carefully.8 Currently, the follow-up period is 5 years for both hysterectomies and hysteroscopies. It is possible to merge DHHD with other health or administrative registers for research purposes or quality monitoring.
Examples of research
DHHD is a dynamic database where the information gathered is based on scientific hypothesis. It generates relevant research projects and results that can be directly implemented nationwide. The variables and indicators defined by DHHD are all undergoing adjustments, according to the evolution of new procedures or new clinical problems.
Achievement of primary goals
Nationwide change from abdominal to minimal invasive hysterectomy
Due to annual benchmarking meetings, there has been an overall nationwide increase in the use of vaginal and laparoscopic methods (Figure 1) and a decline in the overall complication rate during the past years (Table 1). The level of competence for physicians training to become specialists was changed in 2013 based on DHHD data. A large part of these specialized laparoscopic operations is now being performed in teams partly performed by consultants.
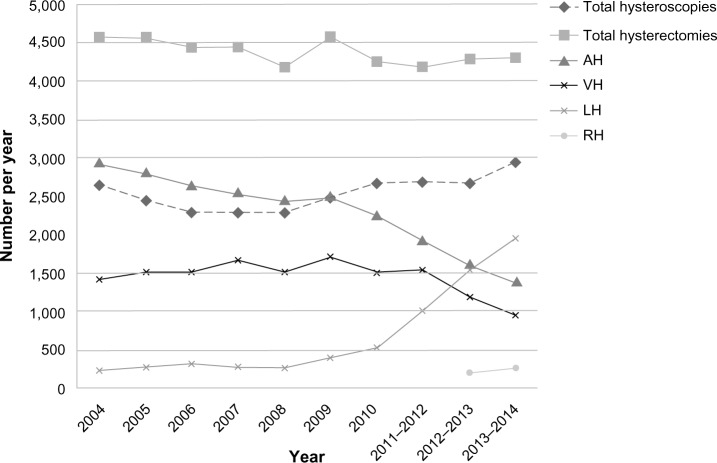
Figure 1.
Rates of hysteroscopy and hysterectomy performed on benign diagnosis from 2004 to 2014.
Abbreviations: AH, abdominal hysterectomy; VH, vaginal hysterectomy; LH, laparoscopic hysterectomy; RH, robot-assisted hysterectomy.
Decline in regional variation
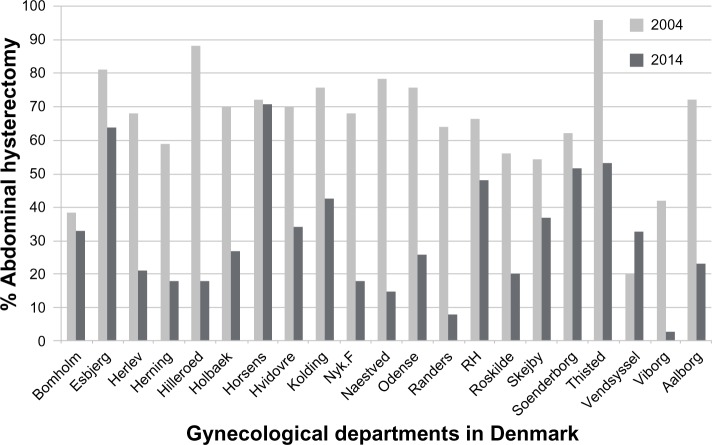
There has been a reduction in the regional variation in choice of hysterectomy methods. In 2004, hysterectomies were performed in 31 public gynecological departments with a variation of 0% to 70% minimal invasive procedures (Figure 2) comprising 31% vaginal and 5% laparoscopic hysterectomies. In 2014, the overall number of departments performing hysterectomies was reduced to 22 public gynecological departments and five large private hospitals, the minimal invasive hysterectomy now ranging from 25% to 100%, comprising 22% vaginal and 51% laparoscopic methods (Figure 2).
Figure 2.
Regional reduction in abdominal hysterectomy from 2004 to 2014 at 21 public gynecological departments performing hysterectomies during the 10-year period.
Notes: In 2004, there were 31 public hospitals and an unknown number of private hospitals performing hysterectomies. Ten of the public departments were closed or merged before 2014 and therefore not shown. None of the private hospitals was registering hysterectomies in 2004. On a national level, there were 75% abdominal hysterectomies. In 2014, there were 21 public hospitals and 5 private hospitals performing hysterectomies. On a national level, there were 27% abdominal hysterectomies.
Abbreviations: Nyk.F, Nykoebning Falster; RH, Rigshospitalet.
During the past 5 years, several departments have arranged annual workshops to spread knowledge nationwide with live operations, discussion of methods, and how to avoid and handle laparoscopic complications. In spring 2015, Denmark hosted the first Nordic Congress on gynecological endoscopy and minimal invasive gynecological surgery, and a Nordic society was initiated.
Quality assessment and postoperative complications
Readmissions, reoperations, and duration of hospital stay all improved during the past 10 years. However, implementing fast-track hysterectomies with short hospital stay of just 1–2 days might increase the need for readmissions or outpatient clinic contacts. The total complication rate after hysterectomy seemed unchanged despite other favorable changes (Table 1). However, after a thorough validation process of the registration in NPR and redefinition of some of the indicators, the total complication rate has been declining in the past 3 years as expected.
Hysteroscopic methods
Regarding hysteroscopy, in 2002, the overall complication rate was 4.8% and the need for further treatment within 5 years was 20%. Today, the complication rate is 2%–4%, and the need for further treatment is 21% after endometrial resection. Thus, this method does not seem to change the efficacy over time and it does not seem to reduce the rates of hysterectomy during the past 10 years (Figure 1).
National guidelines
DHHD’s nationwide cooperation and research have led to the following national guidelines – All women undergoing a hysterectomy on benign indications are recommended to be included in fast-track regimes, the vaginal or laparoscopic methods should be preferred, especially in overweight women,1,9 and prophylactic treatment with antibiotics and antithrombotics should be used.10 Furthermore, routine tests for potential transfusions have proved unnecessary.11
Other studies
We have investigated socioeconomic influence on the choice of hysterectomy method, the relation between surgeon’s experience and the risk of complications, and chronic pain after hysterectomy.12,13
Current projects
Currently, a randomized controlled trial is being conducted to investigate whether prophylactic use of an antifibrinolytic drug, tranexamic acid, could reduce bleeding complications. Suspension methods of the vaginal cuff are registered to investigate the risk of pelvic organ prolapse after hysterectomy.14,15 A long-term follow-up on the suspension and development of pelvic organ prolapse is being established. Finally, complications after the different methods of hysterectomy are currently being analyzed, and a large register study (including data from the NPR, DHHD, and the birth register) has been set up to investigate the long-term risk of hernias, bowel obstruction, ureter injuries, fistulas, and vaginal cuff dehiscence after hysterectomy.
Administrative issues and funding
DHHD has been established on national funding for Danish clinical databases, approved as one of the national clinically high-quality databases by the Danish National Board of Health since 2009, and deeply rooted in the Danish Society of Obstetrics and Gynecology.
Since 2013–2014, the Danish Clinical Registries (RKKP) and Registry Support Centre of Clinical Quality and Health Informatics (East) have constituted the infrastructure of DHHD to ensure a continued improvement in the utilization of the national clinical databases. Since 2012, statistical support to the database has been provided by Registry Support Centre of Epidemiology and Biostatistics (North).
Conclusion
DHHD is a nationwide clinical database with ambitious national goals for reduction of complications for hysterectomy. DHHD aims to explore and monitor the long-term efficacy of several alternatives to hysterectomy and to continue to increase the knowledge about short- and long-term risks for benign hysterectomy and hysteroscopy. This will improve the daily clinical decision-making process and ultimately benefit the women undergoing these procedures.
Acknowledgments
We thank the remaining members of the steering committee of DHHD – Lisa Maria Bang, Jan Blaakær, Eva Dreisler, Margit Dueholm, Helga Gimbel, Annemette Jørgensen, Jan Schultz Larsen, Øjvind Lidegaard, Charlotte Møller, Mads Nielsen-Breining, Bent Ottesen, Lars Schouenborg, and Henrik Halvor Springborg. We also thank Sofia Kyndesen and Pia Frøslev, Registry Support Centre of Clinical Quality and Health Informatics (East), for providing qualified support for our database.
We thank the English-language translator AM Settnes, MA, for revision. This paper was funded by the Program for Clinical Research Infrastructure (PROCRIN) established by the Lundbeck Foundation and the Novo Nordisk Foundation and administered by the Danish Regions.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nielsen SL, Daugbjerg SB, Gimbel H, Settnes A. Use of vaginal hysterectomy in Denmark: rates, indications and patient characteristics. Acta Obstet Gynecol Scand. 2011;90(9):978–984. doi: 10.1111/j.1600-0412.2011.01199.x. [DOI] [PubMed] [Google Scholar]
- 2.Moller C, Kehlet H, Utzon J, Ottesen B. Hysterectomy in Denmark. An analysis of postoperative hospitalisation, morbidity and readmission. Dan Med Bull. 2002;49(4):353–357. [PubMed] [Google Scholar]
- 3.Hansen CT, Moller C, Daugbjerg S, Utzon J, Kehlet H, Ottesen B. Establishment of a national Danish hysterectomy database: preliminary report on the first 13,425 hysterectomies. Acta Obstet Gynecol Scand. 2008;87(5):546–557. doi: 10.1080/00016340802011579. [DOI] [PubMed] [Google Scholar]
- 4.Dansk Hysterektomi og Hysteroskopi Databases, Hyskorapport 2004–2006 [The Danish Hysterectomy and Hysteroscopy Database: Report of Hysteroscopy in Denmark 2004–2006] [Accessed November, 2013]. Available from: http://gynobsguideline.dk/files/HyskobaseAarsrapport%202004%20-%202006.pdf.
- 5.Utzon J, Hansen CC, Andreasen J, Ottesen BS. Dansk Hysterektomi Database set i et sundhedsøkonomisk perspektiv [The Danish Hysterectomy Database seen from a public health-economic perspective] Ugeskr Laeger. 2005;167(34):3170–3174. [PubMed] [Google Scholar]
- 6.Fergusson RJ, Lethaby A, Shepperd S, Farquhar C. Endometrial resection and ablation versus hysterectomy for heavy menstrual bleeding. Cochrane Database Syst Rev. 2013;11:Cd000329. doi: 10.1002/14651858.CD000329.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 8.Dansk Hysterektomi og Hysteroskopi Databases aarsraport 2013 [The Danish Hysterectomy and Hysteroscopy Database yearly report 2013] [Accessed November 30, 2014]. Available from: http://static1.squarespace.com/static/5467abcce4b056d72594db79/t/54b6b1dce4b0567044aa06bb/1421259228340/DHHD_%C3%A5rsrapport_2013_endelig+version.pdf.
- 9.Osler M, Daugbjerg S, Frederiksen BL, Ottesen B. Body mass and risk of complications after hysterectomy on benign indications. Hum Reprod. 2011;26(6):1512–1518. doi: 10.1093/humrep/der060. [DOI] [PubMed] [Google Scholar]
- 10.Hansen CT, Kehlet H, Moeller C, Moerch L, Utzon J, Ottesen B. Timing of heparin prophylaxis and bleeding complications in hysterectomy a nationwide prospective cohort study of 9,949 Danish women. Acta Obstet Gynecol Scand. 2008;87(10):1039–1047. doi: 10.1080/00016340802419384. [DOI] [PubMed] [Google Scholar]
- 11.Thoestesen LM, Rasmussen KL, Lauszus FF, Hansen CT, Titlestad KE, Larsen R. Transfusion rate and prevalence of unexpected red blood cell alloantibodies in women undergoing hysterectomy for benign disease. Acta Obstet Gynecol Scand. 2011;90(6):636–641. doi: 10.1111/j.1600-0412.2011.01117.x. [DOI] [PubMed] [Google Scholar]
- 12.Daugbjerg SB, Ottesen B, Diderichsen F, Frederiksen BL, Osler M. Socioeconomic factors may influence the surgical technique for benign hysterectomy. Dan Med J. 2012;59(6):A4440. [PubMed] [Google Scholar]
- 13.Brandsborg B, Nikolajsen L, Hansen CT, Kehlet H, Jensen TS. Risk factors for chronic pain after hysterectomy: a nationwide questionnaire and database study. Anesthesiology. 2007;106(5):1003–1012. doi: 10.1097/01.anes.0000265161.39932.e8. [DOI] [PubMed] [Google Scholar]
- 14.Lowenstein E, Ottesen B, Gimbel H. Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int Urogynecol J. 2015;26(1):49–55. doi: 10.1007/s00192-014-2413-y. [DOI] [PubMed] [Google Scholar]
- 15.Lykke R, Blaakaer J, Ottesen B, Gimbel H. Pelvic organ prolapse (POP) surgery among Danish women hysterectomized for benign conditions: age at hysterectomy, age at subsequent POP operation, and risk of POP after hysterectomy. Int Urogynecol J. 2015;26(4):527–532. doi: 10.1007/s00192-014-2490-y. [DOI] [PubMed] [Google Scholar]