The purpose of this study was to examine changes in Medicaid-funded one-to-one behavioral support use in school as children age and to determine whether these changes differed for children with various psychiatric disorders.
Schools are the most common setting for behavioral health services for children and adolescents (Child Trends, 2013; Farmer, Burns, Phillips, Angola, & Costello, 2003; Freudenberg & Rules, 2007). School-based services also can be very effective, by reducing disciplinary referrals and out-of-school suspensions (Flay, Allred, & Ordway, 2001; Kang-Yi, Mandell, & Hadley, 2013; the Children's Aid Society, 2001); decreasing academic failure and school dropout (Wyman et al., 2010); and improving learning behavior, grade promotion, and grades (Conduct Problems Prevention Research Group, 2002; Flay et al., 2001; Ailing et al., 1999; Jennings, Pearson, & Harris, 2000; Kang-Yi, Mandell, & Hadley, 2013; Kollam, Rebook, IA logo, & Mayer,1994; Kerns et al., 2011; Nelson, Martello, & Marchand-Martella, 2002; Walter et al., 2011; Wyman et al., 2010).
While more adolescents with psychiatric disorders receive behavioral health services in school than in any other setting (Costello, He, Sampson, Kessler, & Merikangas, 2014), they are undertreated relative to younger children with psychiatric disorders (Green, McLaughlin, Alegria, et al., 2013; Kataoka, Zhang, & Wells, 2002; Leaf et al., 1996; Merikangas, 2011). A recent national survey reports that only one third of adolescents with psychiatric disorders receive behavioral health treatment (Merikangas et al., 2011). Perhaps because they do not receive more appropriate care, adolescents are more likely than younger children to use more restrictive and expensive forms of care. For example, children aged 13-17 years with autism are 80% more likely than children aged 5-12 years with autism to be admitted to inpatient psychiatric hospitals (Mandell et al., 2012) and be placed in long-term and restrictive care (Cidav, Marcus, & Mandell, 2014). A recent national study of children diagnosed with psychiatric disorders found that more than 50% of children who had inpatient hospitalization and emergency department visits for psychiatric disorders in 2006 and 2011 were between 15 and 17 years old (Tori, Encino's, Bedrail, McCormick, & Simpson, 2015). Psychiatric hospitalizations among adolescents with psychiatric disorders cost $3.9 billion annually (Weiss et al., 2015). Connecting adolescents with appropriate community-based services is a critical component of preventing psychiatric hospitalization (Fontanella, 2008).
Increasing access to school-based behavioral health services for adolescents could be a critical component of improving their outcomes and reducing the use of more costly, restrictive care. Most studies of school-based behavioral health services have examined the experiences of elementary school-aged children, with only a few that have examined the experiences of high school students (Durlak et al., 2011). One systematic review identified only five studies of adolescents’ use of school-based behavioral health care (Farahmand, Grant, Polo, & Duffy, 2011).
In the present study, we specifically examine Medicaid-reimbursed school-based behavioral health care for adolescents. Medicaid has become an increasingly important source of funding for this type of service, especially in under-resourced areas (Mandell et al., 2008). The reasons are several-fold. First, the Individuals with Disabilities Education Improvement Act explicitly bans the use of federal education funds for mental health treatment of children in special education programs, meaning that local education agencies must turn elsewhere to obtain funding for mental health care for their students. Second, Medicaid, which serves more than 1 in 4 children in the United States, has historically embraced the task of providing medical care to children in special education. For example, amendments in 1986 clarified that Medicaid funds can be used to pay for services that are listed in a child's individualized education plan. Most states leverage the Early and Periodic Screening Diagnosis and Treatment (EPSDT) program to pay for this care, even if it falls outside of their state Medicaid plans (Noel & Shreve, 2006; Parrish et al., 2004; Rodman et al., 1999; Semansky, Koyanagi, & Vandivort-Warren, 2003). The proportion of children Medicaid serves and the breadth of coverage will only expand under the Affordable Care Act.
Despite the importance of Medicaid as a funder of school-based behavioral health services, little information on Medicaid-funded school-based behavioral health service use among adolescents is available. Most published studies examine medication use among children with psychiatric disorders (e.g., Kamble, Chen, Johnson, Bhatara, & Aparasu, 2015; Rettew, et al., 2015; Visser et al., 2015), acute psychiatric treatment use such as psychiatric hospitalization (e.g., Fantanella et al., 2015), and Medicaid expenditures (e.g., Cidav, Lawer, Marcus, & Mandell, 2013). Even less research has examined school-based behavioral health service use by disorder. Behavioral health care needs and use may vary considerably by psychiatric disorder (Merikangas et al., 2011).
Examining how school-based behavioral health service use and associated spending change as children age will draw attention to potential gaps in or loss of coverage, and identify important potential points of intervention to increase continuity of care, improve access, and ultimately improve outcomes for children and adolescents with psychiatric disorders. Our study paid particular attention to Medicaid-funded one-to-one behavior support service in school, which is provided to children if their ability to function in school is significantly impaired as a result of their primary diagnosis (Kang-Yi et al., 2013). Although one-to-one behavioral support in school is an important resource for children with psychiatric disorders with limited school functioning, whether children continue to receive one-to-one behavioral support services in school as they age and if one-to-one behavioral support service use differs by psychiatric disorder are unknown. Our study also examined out-of-school behavioral health service use to identify if children use other routine care such as outpatient psychiatric treatment and other behavioral health services as they age and if the pattern of in-school and out-of-school service use by age differs by psychiatric disorder. Our examination of these trends will allow for greater specificity in targeting groups that are particularly vulnerable to loss of care.
Methods
Study Sample
The study included 24,271 children who were between 5-17 years old, and used Medicaid-funded behavioral health services in Philadelphia between October 1, 2008 and September 30, 2009. The University of Pennsylvania's Institutional Review Board and the Institutional Review Board of the City of Philadelphia Department of Public Health approved this protocol.
Variables
Psychiatric disorders were categorized as autism, conduct disorder/oppositional defiant disorder (conduct disorder/ODD), attention deficit hyperactivity disorder (ADHD), and other psychiatric disorders. The diagnoses were identified using the International Classification of Diseases (9th ed., ICD-9). Children with primary diagnosis of 299.xx were identified as having autism. Children with the primary diagnosis of 312.xx or 313.xx were identified as having conduct disorder/ODD. Children with the primary diagnosis of 314.xx were identified as having ADHD. Other psychiatric disorders included affective mood disorder, substance abuse, schizophrenia, and other psychiatric diagnoses. Consistent with previous studies of this dataset (Kang-Yi, Locke, Marcus, Mandell, & Hadley, 2015), among children with more than one diagnosis, only one diagnosis was assigned. If any autism diagnosis was present in the claims, children were categorized as having autism, regardless of other diagnoses. Similarly, if no autism diagnosis was present but a diagnosis of ADHD was present, the child was categorized as having ADHD, regardless of the presence of other diagnoses. Conduct disorder/ODD took precedence over the remaining diagnoses. Children were categorized as “other psychiatric disorders” if autism, ADHD, or conduct disorder/ODD were not present (Kang-Yi et al., 2015). Less than 5% of the sample had more than one diagnosis. The diagnosis of anxiety and depression are very unreliable in community settings (Garland et al., 2001). In our sample, children with these disorders comprised only 22.3% of the “other psychiatric disorders” group. We therefore combined them with other psychiatric disorders.
Behavioral health service use was divided into two categories: Medicaid funded 1) in-school one-to-one behavioral support, and 2) out-of-school behavioral health services (such as outpatient treatment and out-of-school Behavioral Health Rehabilitation Services (BHRS) provided in Pennsylvania for children with psychiatric disabilities). BHRS comprises wraparound services designed to provide therapeutic intervention to children who are aged 3-21 years with serious emotional disturbance, social, or behavioral problems and need more intense behavioral services other than outpatient treatment (City of Philadelphia Department of Behavioral Health and Intellectual Disability Services, 2006). Our study examined community-based behavioral health care; therefore, our definition of out-of-school services did not include acute services such as crisis center visits, inpatient hospitalization, or residential treatment. Based on the available school data, as of school year 2008-2009, Medicaid-funded behavioral health services were provided in 270 schools. One-to-one behavioral support was most common across schools. Average school enrollment was 634; 51% of students were males, 66% were African Americans and 79% were on the free and reduced lunch program. Age was categorized into two groups: Elementary school age (5-11 years old), and middle school and high school age (12-17 years old) to identify behavioral health service use by psychosocial development stage using the child development milestones. While the Centers for Disease Control and Prevention (CDC, 2015) defines developmental milestones into three stages including middle school and high school ages as separate stages, our study combined these two groups due to the small number of high school-aged children using one-to-one in-school behavioral support. Annual mean Medicaid expenditures for in-school one-to-one behavioral support service use and out-of-school behavioral health service use per child were calculated for each age group by psychiatric disorder. Other demographic variables included sex (male vs. female) and race/ethnicity (African American, White, Hispanic, and Other).
Analysis
Chi-square tests were used to examine differences in demographic characteristics by psychiatric disorder. Unadjusted behavioral health service use and annual mean Medicaid expenditures were calculated by age, psychiatric disorder and service type among users. Logistic regression was used to examine the association of children's in-school one-to-one behavioral support use and out-of-school behavioral health service use (dependent variables) with age for each psychiatric disorder, adjusting for race/ethnicity and sex. An additional logistic regression model included all subjects across psychiatric disorders and examined the interaction between age and diagnosis. This latter model tests the extent to which the magnitude of the relationship between age and service use differs by diagnosis. Using parallel techniques, generalized linear models with a gamma distribution and log link function were conducted to compare similar differences in expenditures for in-school one-to-one behavioral support and out-of-school behavioral health service use.
Results
Table 1 presents demographic characteristics of the study sample by psychiatric disorder. The age distribution significantly differed by psychiatric disorder (p < 0.05). About two thirds of children with autism and ADHD were between the ages of 5-11; about a third of children with conduct disorder/ODD and other psychiatric disorders were between the ages of 5-11. Sex and race/ethnicity distributions also significantly differed by psychiatric disorder. The proportion of females was the highest for the other psychiatric disorders group (51.5%), followed by conduct/ODD (33.4%), ADHD (28.0%) and autism (15.6%, significant difference at p < 0.001). The proportion of African American children was the highest among children with conduct/ODD (74.8%) and the proportion of Hispanic children was highest in the ADHD group (38.7%, significant difference at p < 0.001).
Table 1.
Demographic Characteristics by Psychiatric Disorder
| Characteristics | Autism ( N = 941) | Conduct disorder/ODD (N = 5,118) | ADHD (N = 9,669) | Other psychiatric disorders (N = 8,543) | Total (N = 24, 271) |
|---|---|---|---|---|---|
| % | |||||
| Age** | |||||
| 5-11 years | 69.7 | 37.5 | 66.6 | 35.7 | 49.7 |
| 12-17 years | 30.3 | 62.5 | 33.4 | 64.3 | 50.3 |
| Race/Ethnicity*** | |||||
| African American | 46.1 | 74.8 | 49.1 | 59.7 | 58.1 |
| White | 30.0 | 7.3 | 9.5 | 12.9 | 11.0 |
| Hispanic | 13.6 | 16.2 | 38.7 | 24.7 | 28.1 |
| Other | 10.3 | 1.8 | 2.7 | 2.7 | 2.8 |
| Sex*** | |||||
| Male | 84.4 | 66.6 | 72.0 | 48.5 | 63.1 |
| Female | 15.6 | 33.4 | 28.0 | 51.5 | 36.9 |
Note.
p < .01
p < .001; significant difference by psychiatric disorder
Use of In-School One-to-One Behavioral Support
Overall, 6.8% (n = 1,643) of the children received one-to-one behavioral support, while 95.8% (n = 23,251) received other out-of-school behavioral health services. For all psychiatric disorders, middle and high school-aged children were less likely to use one-to-one behavioral support than elementary school-aged children did, and the degree of the service use gap by age significantly differed by psychiatric disorder (p < 0.001 when comparing 12-17 year olds to 5-11 year olds by psychiatric disorder). Among children with autism, middle- and high-school aged children were 48% less likely than elementary school-aged children to use one-to-one behavioral support (p < 0.001). For children with conduct disorder/ODD, middle and high school-aged children were 80% less likely than elementary school-aged children to use one-to-one behavioral support (p < 0.001). For children with ADHD, middle and high school-aged children were 60% less likely than elementary school-aged children to use one-to-one behavioral support (p < 0.001 for both results). For children with other psychiatric disorders, middle school and high school-aged children were 68% less likely than elementary school-aged children to use one-to-one behavioral support (p < 0.001).
Out-of-School Behavioral Health Service Use
The distribution of out-of-school behavioral health service use significantly differed by age group and by psychiatric disorder. Middle and high school-aged children with autism, conduct/ODD and other psychiatric disorders were less likely to use out-of-school behavioral health services than elementary school-aged children did. Middle school and high school-aged children with autism were 75% less likely than elementary school-aged children with autism to use out-of-school services (p < 0.001). Middle school and high school-aged children with conduct disorder/ODD were 17% less likely than elementary school-aged children with conduct disorder/ODD to use out-of-school services (p < 0.05). Middle school and high school-aged children with other psychiatric disorders were 35% less likely than elementary school-aged children with other psychiatric disorders to use out-of-school services (p < 0.01).
Medicaid Expenditures for In-School One-to-One Behavioral support
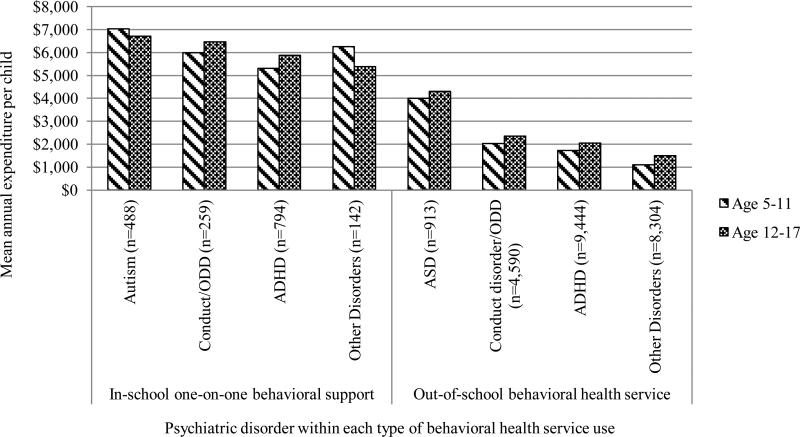
Figure 1 and Table 2 present Medicaid expenditures for one-to-one behavioral support by age group and by psychiatric disorder. As shown in Figure 1, the annual mean Medicaid expenditures for one-to-one behavioral support per child ranged from $5,311 (for elementary school-aged children with ADHD) to $7,021 (for elementary school- aged children with autism). By diagnosis group, the mean expenditure per child was the highest for children with autism. After controlling for gender and race/ethnicity, the expenditures among service users for one-to-one behavioral support were not significantly different by age group for children for all diagnosis groups (Table 2).
Figure 1.
Annual mean Medicaid expenditures by age, psychiatric disorder and service type among service users. ODD: Oppositional defiant disorder, ADHD: Attention deficit hyperactivity disorder
Table 2.
Medicaid Funded In-School One-to-One Behavioral Support and Associated Medicaid Expenditures
| In-school one-to-one behavioral support service | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism (n=488) | Conduct disorder/ODD (n=259) | ADHD (n=794) | Other psychiatric disorder (n=142) | Type III overall interaction effect test |
|||||||||
| Age | N | Row % | OR | N | Row % | OR | N | Row % | OR | N | Row % | OR | P-value |
| 12-17 years old | 116 | 18.0 | 0.516*** | 68 | 37.6 | 0.202*** | 142 | 13.8 | 0.398*** | 52 | 30.7 | 0.324*** | <.001 |
| 5-11 years old | 372 | 14.6 | Reference | 191 | 50.0 | Reference | 652 | 6.9 | Reference | 90 | 28.5 | Reference | NA |
| Medicaid expenditures for in-school one-to-one behavioral support service | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Mean expenditures |
Standard Deviation |
Mean estimate |
Mean expenditures |
Standard Deviation |
Mean estimate |
Mean expenditures |
Standard Deviation |
Mean estimate |
Mean expenditures |
Standard Deviation |
Mean estimate |
P-value |
| 12-17 years old | $6,704 | 6448.95 | 0.942 | $6,468 | 3744.03 | 1.095 | $5,875 | 3914.21 | 1.109 | $5,390 | 4154.32 | 0.857 | 0.224 |
| 5-11 years old | $7,021 | 6689.93 | Reference | $5,985 | 3493.74 | Reference | $5,311 | 3509.12 | Reference | $6,262 | 3812.14 | Reference | NA |
Note. ODD: Oppositional defiant disorder, ADHD: Attention deficit hyperactivity disorder. OR: Odds ratio.
p < 0.001. Separate logistic and log linear model (using a gamma distribution) were run within each diagnosis group to predict service use and expenditures, respectively. The models control for sex and race/ethnicity. Omnibus regression models were produced including all subjects to examine the interaction between age and diagnosis. Mean estimates present exponentiated beta coefficients.
Medicaid Expenditures for Out-of-School Behavioral Health Service Use
As shown in Table 3 and Figure 1, the annual mean expenditures for out-of-school behavioral health service use per child ranged from $1,095 (for elementary school-aged children with ADHD) to $4,309 (for middle and high school-aged children with other psychiatric disorders). The expenditures among users of out-of-school services for middle and high school-aged children with conduct disorder/ODD were 18% higher than the expenditures for elementary school-aged children with conduct disorder/ODD (p < 0.001). The expenditures for middle school and high school-aged children with ADHD were 17% higher than the expenditures for elementary school-aged children with ADHD (p < 0.001). The expenditures for middle and high school-aged children with other psychiatric disorders were 35% higher than the expenditures for elementary school-aged children with other psychiatric disorders (p < 0.001). The within-psychiatric group differences in the expenditures between middle and high school- aged group and elementary school-aged group were significantly different by psychiatric disorder (p < 0.001).
Table 3.
Medicaid-Funded Out-Of-School Behavioral Health Service Use and Associated Medicaid Expenditures
| Out-of-school behavioral health service use | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Autism (n=913) | Conduct disorder/ODD (n=4,590) | ADHD (n=9,444) | Other psychiatric disorder (n=8,304) | Type III overall interaction effect test |
|||||||||
| Age | N | Row % | OR | N | Row % | OR | N | Row % | OR | N | Row % | OR | P-value |
| 12-17 years old | 267 | 26.3 | 0.254*** | 2852 | 27.2 | 0.825* | 3152 | 45.9 | 0.951 | 5323 | 2.3 | 0.654** | 0.007 |
| 5-11 years old | 646 | 14.9 | Reference | 1738 | 54.0 | Reference | 6292 | 25.6 | Reference | 2981 | 5.5 | Reference | NA |
| Medicaid expenditures for out-of-school behavioral health services | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | Mean expenditures |
Standard Deviation |
Mean estimate |
Mean expenditures |
Standard Deviation |
Mean estimate |
Mean expenditures |
Standard Deviation |
Mean estimate |
Mean expenditures |
Standard Deviation |
Mean estimate 95% CI |
P-value |
| 12-17 years old | $2,349 | 4612.51 | 1.057 | $2,039 | 4094.76 | 1.184*** | $1,497 | 3369.48 | 1.168*** | $4,309 | 6383.98 | 1.351*** | <.001 |
| 5-11 years old | $2,020 | 2803.59 | Reference | $1,722 | 2931.76 | Reference | $1,095 | 1951.13 | Reference | $3,990 | 4900.88 | Reference | NA |
Note. ODD: Oppositional defiant disorder, ADHD: Attention deficit hyperactivity disorder. OR: Odds ratio.
p < 0.05
p < 0.01
p < 0.001. Separate logistic and log linear model (using a gamma distribution) were run within each diagnosis group to predict service use and expenditures, respectively. The models control for sex and race/ethnicity. Omnibus regression models were produced including all subjects to examine the interaction between age and diagnosis. Mean estimates present exponentiated beta coefficients.
Discussion and Conclusion
Our study compared the use of in-school one-to-one behavioral support and out-of-school behavioral health care among Medicaid-enrolled children of different ages and with different psychiatric disorders. We found that 90% of children who received behavioral health care in Philadelphia through Medicaid between 2008 and 2009 used out-of-school behavioral health services, while only 6.8% of them used one-to-one behavioral supports in school. Almost all children who received in-school services received out-of-school services regardless of age and psychiatric disorder, although the volume of service use differed by age and psychiatric disorder.
We found that for each psychiatric disorder, older children were much less likely than younger children to use in-school one-to-one support. Of the middle school and high school-aged children, those with conduct disorder/ODD had the highest use (37.6%) followed by other psychiatric disorders (30.7%). Of the elementary school-aged children, those with conduct disorder/ODD had the highest use (59.0%). Although the descriptive statistics showed higher proportions of middle school and high school-aged children with autism, ADHD and other psychiatric disorders compared to the proportions of elementary school-aged children using in-school one-to-one support, when age and race/ethnicity controlled, the significant lower use among older children was found. Older children may receive other types of school-based services that are not paid for through Medicaid such as accommodations, tutoring, counseling, or testing provided by a school counselor or psychologists. One-to-one behavioral support may be less effective in meeting older children's behavioral needs. Adolescents’ satisfaction with in-school services and stigma against children with psychiatric disorders might be other factors in the reduced use of one-to-one behavioral support. Stigma has been identified as a barrier to behavioral health service use among adolescents (Goplan et al., 2010). The reduced use of one-to-one behavioral support as children age may indicate less need for this service.
As shown in the number of children using the services in Tables 2 and 3, among children with other psychiatric diagnoses, the use of one-to-one behavioral support decreased more than did out-of-school service use as they aged. Other psychiatric disorders included children with affective mood disorder, substance abuse, schizophrenia, and other psychiatric diagnoses. Many of these psychiatric disorders develop during adolescence and the low use of one-to-one behavioral support among adolescents with these diagnoses is consistent with previous findings (Merikangas et al., 2011). School-based behavioral health care models may not be appropriate for older children with these disorders.
Although the number of children using school-based one-to-one behavioral support decreased with age, expenditures for this service did not show a significant difference. The finding suggests that once children are enrolled in the one-to-one behavioral support, children receive similar level of care regardless of their age. While the use of out-of-school behavioral health services is significantly lower for older children than elementary school-aged children for all psychiatric disorders groups but ADHD (after controlling for age and sex), the annual mean Medicaid expenditures for older children are significantly higher than those for elementary school-aged children. The higher expenditures may indicate greater need among older children.
Overall, adolescents compared to elementary school-aged children used significantly less in-school one-to-one support and out-of-school behavioral services. The reasons may vary. Although our study did not examine use of behavioral health treatment in other settings such as psychotropic medication use and pediatric care due to the limited data, older children with psychiatric disorders may seek out other types of behavioral health services because of perceived stigma attached to using school-based services (Corrigan, Kerr, & Knudsen, 2005; Gulliver, Griffiths, & Christensen, 2010; Mellor, 2014). Adolescents with other psychiatric disorders such as affective mood disorder and substance abuse may use more psychotropic medication than other types of behavioral services. The adolescents who do not use in-school or out-of-school routine behavioral health services may use more restrictive and acute care such as psychiatric hospitalization, psychiatric residential treatment or psychiatric medications, which we did not examine in this study. It also is possible that changing priorities such as focusing more on readiness for postsecondary education and job training in high school compared with middle schools and elementary schools may affect schools and families (Carter & Wehby, 2003; Hendricks & Wehman, 2009) to pay less attention to the need for behavioral health services among adolescents with psychiatric disorders.
Whether or not the one-to-one behavioral support is meeting the level of need for older children have is questionable. Medicaid expenditures for one-to-one behavioral health service is considerably higher than the expenditures for other routine care such as outpatient treatment. Our study finds the gap in the expenditures between two services per child to be more than double (except the expenditures for other psychiatric disorder group) and this might be the reason why 90% of children receive out-of-school services through Medicaid. Nonetheless, the proportion of children Medicaid serves will increase under the Affordable Care Act and school-based service use is likely to increase. Efforts to increase routine behavioral health care in school should be made by tailoring and expanding other types of school-based services to meet the specific needs of adolescents going through unique developmental transitions that exacerbate psychiatric symptoms. Expanding behavioral health services designed to provide age-appropriate care is essential. Treatment models that combine transition care for adolescents such as teaching communication and social skills for independent community living and employment might attract more adolescents to use school-based services. Offering school-based behavioral health services in the specialty mental health setting should be further emphasized. Cross-system collaboration between youth-serving systems to increase appropriate school-based services and the service use based on a cohesive policy that aligns care coordination and innovative funding strategies should be developed to effectively serve adolescents with psychiatric disorders (Salum et al., 2012).
Limitations
Our study had several limitations. The cross-sectional design of this study limits understanding of what changes in service use might occur across ages. Future longitudinal studies may explain when the drop in service use occurs in the older ages. The analysis of behavioral health service use is based on behavioral health Medicaid claims data and does not take into account psychiatric medication use, which may be more prevalent among adolescents. Due to the data available, we did not have severity measures nor access to behavioral health services funded through other sources such as the education system, private insurance and out of pocket expenses. Thus, the differences in behavioral health service use and associated expenditures by age group reflect only the Medicaid-funded services. Additionally, our study focused on routine psychiatric care. Analysis of acute and restrictive behavioral health service use such as inpatient psychiatric hospitalization, residential treatment and crisis response center visit could provide more comprehensive understanding of differences in behavioral health service use by age group. Although we did not examine these behavioral health services, our findings show that adolescents with psychiatric disorders were not receiving routine psychiatric care. Future research extending our study to examining behavioral health care for adolescents in other settings will lead policy makers and practitioners to identify effective service delivery of routine behavioral health care for adolescents with psychiatric disorders. Our study focused primarily on service use for disruptive behavior disorders based on the evidence that the more common psychiatric disorders among children served by public specialty mental health system is disruptive behavioral disorders (Garland et al., 2001). Although internalizing behavioral disorders were included in our analyses under the other psychiatric disorders category, we did not conduct in-depth analyses regarding the relationship between internalizing behavioral disorders and school-based behavioral health service use. Future research that examines the relationship between internalizing disorders and use of in-school one-to-one behavioral support and associated behavioral health care expenditures is important to further identify strategies to provide appropriate school-based care to older children with these internalizing behavioral disorders. Finally, the geographic generalizability of the findings should be limited to the areas with similar demographics of children and adolescents and behavioral health services.
Conclusion
This study is one of the first to investigate differences in Medicaid-funded one-to-one behavioral support and out-of-school behavioral service use, and expenditures for children with psychiatric disorders across age groups. The findings indicated that differences in service use exist across age groups, with significantly fewer adolescents with psychiatric disorders using both in-school and out-of-school behavioral health services, than younger children. These findings point to the need for systemic interventions designed to improve behavioral health service utilization for adolescents with psychiatric disorders both in and out of schools. The period of adolescence is an especially critical stage in which all youth are susceptible to emotional and behavioral dysregulation; these developmental changes may be exacerbated in adolescents with psychiatric disorders who already present with significant emotional and behavioral challenges. As such, adolescents with psychiatric disorders likely have an increased need for behavioral health services in order to maintain emotional and behavioral stability during a developmental time of increased emotional instability as well as to successfully prepare them for the transition into adulthood. This study points to the need for interventions to ameliorate the disparity in service use for adolescents with psychiatric disorders in order to improve their immediate and longer-term outcomes.
Acknowledgments
Funding: This study was partially funded by the City of Philadelphia Department of Behavioral Health and Intellectual Disability Services. The preparation of this article also was supported in part by NIMH K01MH100199, the Autism Science Foundation (Grant # 13-ECA-01L) and FARFund Early Career Award (Locke).
Footnotes
Compliance with Ethical Standards:
The Medicaid claims data were shared through the Memorandum of Understanding between the City of Philadelphia Department of Behavioral Health and Intellectual Disability Services and the University of Pennsylvania.
The University of Pennsylvania's Institutional Review Board and the Institutional Review Board of the City of Philadelphia Department of Public Health approved this study protocol.
Conflict of Interest: Drs. Kang-Yi, Locke, Pellecchia, Marcus, Hadley, and Mandell declare that they have no conflict of interest.
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Contributor Information
Christina D. Kang-Yi, University of Pennsylvania Center for Mental Health Policy and Services Research, 3535 Market Street, 3rd Floor, Philadelphia, PA 19104, USA.
Jill Locke, Speech and Hearing Sciences, University of Washington, University of Washington Autism Center, Box 357920, Seattle, WA 98195, USA, Phone: 206-616-6703, jjlocke@uw.edu.
Melanie Pellecchia, University of Pennsylvania Center for Mental Health Policy and Services Research, 3535 Market Street, 3rd Floor, Philadelphia, PA 19104, USA, Phone: 215-746-1950, pmelanie@upenn.edu.
Steve C. Marcus, University of Pennsylvania School of Social Policy and Practice, 3701 Locust Walk, Caster Building Room C16, Philadelphia, PA 19104, Phone: 215-573-7941, marcuss@upenn.edu.
Trevor Hadley, University of Pennsylvania Center for Mental Health Policy and Services Research, 3535 Market Street, 3rd Floor, Philadelphia, PA 19104, USA, Phone: 215-746-1765, thadley@upenn.edu.
David S. Mansell, University of Pennsylvania Center for Mental Health Policy and Services Research, The Children's Hospital of Philadelphia Center for Autism Research, 3535 Market Street, 3rd floor, Philadelphia, PA 19104, Phone: 215-573-7494, mandelld@upenn.edu.
References
- Ailing NS, Werthamer LW, Kellman SG, Brown CH, Wang S, Lin Y. Proximal impact of two first-grade preventive interventions on the early risk behaviors for later substance abuse, depression and antisocial behavior. American Journal of Community Psychology. 1999;27:599–641. doi: 10.1023/A:1022137920532. [DOI] [PubMed] [Google Scholar]
- Carter EW, Wehby JH. Job performance of transition-age youth with emotional and behavioral disorders. Exceptional Children. 2003;69:449–465. [Google Scholar]
- The Centers for Disease Control and Prevention [September 2, 2015];Child Development. 2015 Aug; http://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/adolescence2.html.
- Child Trends [January 10, 2013];Adolescent health highlight: Access to mental health care. Publication # 2013-2. http://www.childtrends.org/wp-content/uploads/2013/04/Child_Trends-2013_01_01_AHH_MHAccessl.pdf.
- Cidav Z, Lawer L, Marcus SC, Mandell DS. Age-related variation in health service use and associated expenditures among children with autism. Journal of Autism and Developmental Disorders. 2013;43:924–931. doi: 10.1007/s10803-012-1637-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cidav Z, Marcus SC, Mandell DS. Home- and community-based waivers for children with autism: Effects on service use and costs. Intellectual and Developmental Disabilities. 2014;52(4):239–248. doi: 10.1352/1934-9556-52.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- City of Philadelphia Department of Behavioral Health and Intellectual Disability Services [January 15, 2015];Utilizing management guide: Community behavioral health. 2006 http://dbhids.us/assets/Forms--Documents/CBH/UMFULLrev0110.pdf.
- Conduct Problems Prevention Research Group Evaluation of the first 3 years of the Fast Track Prevention Trial with children at high risk for adolescent conduct problems. Journal of Abnormal Child Psychology. 2002;30:19–35. doi: 10.1023/a:1014274914287. [DOI] [PubMed] [Google Scholar]
- Corrigan P, Kerr A, Knudsen L. The stigma of mental illness and methods for change. Applied & Preventive Psychology. 2005;11:179–190. [Google Scholar]
- Costello EJ, He J, Sampson NA, Kessler RC, Merikangas KR. Services for adolescents with psychiatric disorders: 12-month data from the national comorbidity Survey-Adolescent. Psychiatric Services. 2014;65(3):359–366. doi: 10.1176/appi.ps.201100518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durlak JA, Weissberg RP, Dymnicki AB, Taylor RD, Schellinger KB. The impact of enhancing students’ social and emotional learning: A meta-analysis of school-based universal interventions. Child Development. 2011;82(1):405–432. doi: 10.1111/j.1467-8624.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- Farahmand FK, Grant KE, Polo AJ, Duffy SN. School-based mental health and behavioral programs of low-income, urban youth: A systematic and meta-analytic review. Clinical Psychology: Science and Practice. 2011;18(4):372–390. [Google Scholar]
- Farmer EM, Burns BJ, Phillips SD, Angola A, Costello EJ. Pathways into and through mental health services for children and adolescents. Psychiatric Services. 2003;54(1):60–66. doi: 10.1176/appi.ps.54.1.60. [DOI] [PubMed] [Google Scholar]
- Flay BR, Allred CG, Ordway N. Effects of the Positive Action Program on achievement and discipline: two matched control comparisons. Prevention Science. 2001;2:71–89. doi: 10.1023/a:1011591613728. [DOI] [PubMed] [Google Scholar]
- Fontanella CA. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. American Journal of Orthopsychiatry. 2008;78(2):187–198. doi: 10.1037/a0012557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freudenberg N, Ruglism J. Reframing school dropout as a public health issue. [January 4, 2015];Preventing Chronic Disease. 4(4) http://www.cdc.gov/pcd/issues/2007/oct/07_0063.htm. [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Aarons GA, Saltzman MD, Kruse MI. Correlates of adolescents’ satisfaction with mental health services. Mental Health Services Research. 2000;2(3):127–139. doi: 10.1023/a:1010137725958. [DOI] [PubMed] [Google Scholar]
- Garland AF, Hough RL, McCabe KM, Yeh M, Wood PA, Aarons GA. Prevalence of psychiatric disorders with youths across five sectors of care. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(4):409–418. doi: 10.1097/00004583-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Goplan G, Goldstein L, Klingenstein K, Sicher C, Blake C, McKay MM. Engaging families into child mental health treatment: Update and special considerations. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2010;19(3):182–196. [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Alegria M, Costello EJ, Gruber MJ, Hoagwood K, Leaf PJ, et al. School mental health resources and adolescent mental health service use. Journal of American Academy of Child and Adolescent Psychiatry. 2013;52(5):501–510. doi: 10.1016/j.jaac.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators of mental health help-seeking in young people: A systematic review. BioMed Central Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks DR, Wehman P. Transition from school to adulthood for youth with autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2009;24:77–88. [Google Scholar]
- Jennings J, Pearson G, Harris M. Implementing and maintaining school-based mental health services in a large, urban school district. Journal of School Health. 2000;70(5):201–206. doi: 10.1111/j.1746-1561.2000.tb06473.x. [DOI] [PubMed] [Google Scholar]
- Kamble P, Chen H, Johnson ML, Bhatara V, Aparasu RR. Concurrent use of stimulants and second-generation antipsychotics among children with ADHD enrolled in Medicaid. Psychiatric Services. 2015;66(4):404–410. doi: 10.1176/appi.ps.201300391. [DOI] [PubMed] [Google Scholar]
- Kang-Yi CD, Locke J, Marcus SC, Mandell DS, Hadley T. A Comparison of School-Based Behavioral Health Service Use and Associated Expenditures for Children with Autism with those of Children with Other Disorders. Psychiatric Services. 2015 doi: 10.1176/appi.ps.201400505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang-Yi CD, Mandell DS, Hadley T. School-based mental health program evaluation: Children's school outcomes and acute mental health service use. Journal of School Health. 2013;83:463–472. doi: 10.1111/josh.12053. [DOI] [PubMed] [Google Scholar]
- Kataoka SH, Zhang L, Wells KB. Unmet need for mental health care among U.S. children: variation by ethnicity and insurance status. American Journal of Psychiatry. 2002;159:1548–1555. doi: 10.1176/appi.ajp.159.9.1548. [DOI] [PubMed] [Google Scholar]
- Kerns SE, Pullmann MD, Walker SC, Lyon AR, Cosgrove TJ, Burns EJ. Adolescent use of school-based health centers and high school dropout. Archives of Pediatrics & Adolescent Medicine. 2011;165(7):617–623. doi: 10.1001/archpediatrics.2011.10. [DOI] [PubMed] [Google Scholar]
- Kollam S, Rebook G, IA logo N, Mayer L. The course and malleability of aggressive behavior from early first grade into middle school: results of a developmental epidemiologically based preventive trial. Journal of Child Psychology and Psychiatry. 1994;35:259–281. doi: 10.1111/j.1469-7610.1994.tb01161.x. [DOI] [PubMed] [Google Scholar]
- Leaf PJ, Alegria M, Cohen P, Goodman SH, Horwitz SM, Hoven CW, Narrow WE, et al. Mental health service use in the community and schools: results from the four-community MECA study. Methods for the epidemiology of child and adolescent mental disorders study. Journal of American Academy of Child and Adolescent Psychiatry. 1996;35:889–897. doi: 10.1097/00004583-199607000-00014. [DOI] [PubMed] [Google Scholar]
- Lyon AR, Ludwig KA, Stoep AV, Gudmundsen G, McCauley E. Patterns and predictors of mental healthcare utilization in schools and other service sectors among adolescents at risk for depression. School Mental Health. 2013;5:155–165. doi: 10.1007/s12310-012-9097-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Machefsky A, Rubin D, Feudtner C, Pati S, Rosenbaum S. Medicaid's role in financing health care for children with behavioral health care needs in the special education system: Implications of the Deficit Reduction Act. Journal of School Health. 2008;78(10):532–538. doi: 10.1111/j.1746-1561.2008.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Xie M, Morales KH, Lawer L, McCarthy M, Marcus SC. The interplay of outpatient services and psychiatric hospitalization among Medicaid-enrolled children with autism spectrum disorders. Archives of Pediatrics & Adolescent Medicine. 2012;166(1):68–73. doi: 10.1001/archpediatrics.2011.714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellor C. School-based interventions targeting stigma of mental illness: Systematic review. Psychiatry Bull. 2014;39:164–171. doi: 10.1192/pb.bp.112.041723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J, Brody D, Fisher PW, Bourdon K, Koretz DS. Prevalence and treatment of mental disorders among US children in the 2001-2004 NHANES. Pediatrics. 2010;125(1):75–81. doi: 10.1542/peds.2008-2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He J, Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescents Supplement (NCS-A). Journal of American Academy of Child and Adolescent Psychiatry. 2011;50(1):32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson JR, Martello RM, Marchand-Martella N. Maximizing student learning: The effects of a comprehensive school-based program for preventing problem behaviors. Journal of Emotional and Behavioral Disorders. 2002;10:136–148. [Google Scholar]
- Noel D, Shreve D. Special ed squeeze: the feds are cutting the Medicaid funds many states rely on to provide health services for disabled students. State Legislatures. 2006;32(10):28–29. [PubMed] [Google Scholar]
- Noel DH, Shreve D. Special ed squeeze: The feds are cutting the Medicaid funds many states rely on to provide health services for disabled students. State Legislatures. 2006;32(10):28–37. [PubMed] [Google Scholar]
- Parrish T, Harr J, Wolman J, Anthony J, Merickel A, Esra P. State special education finance systems, 1999-2000. American Institutes for Research; Palo Alto, Calif: 2004. [Google Scholar]
- Rettew DC, Greenblatt J, Kamon J, Neal D, Harder V, Wasserman R, Berry P, MacLean CD, Hogue N, McMains W. Antipsychotic medication prescribing in children enrolled in Medicaid. Pediatrics. 2015;135(4):658–665. doi: 10.1542/peds.2014-2260. [DOI] [PubMed] [Google Scholar]
- Rodman J, Weill K, Driscoll M, Fenton T, Alpert H, Salem-Schatz S, Palfrey JS. A nationwide survey of financing health-related services for special education students. Journal of School Health. 1999;69(4):133–139. doi: 10.1111/j.1746-1561.1999.tb04169.x. [DOI] [PubMed] [Google Scholar]
- Salum GA, Bortoluzzi A, Silveira PP, Bosa VL, Schuch I, Goldani M, Blaya C, Leistner-Segal S, Manfro GG. Is puberty a trigger for 5HTTLPR polymorphism association with depressive symptoms? Journal of Psychiatric Research. 2012;46:831–833. doi: 10.1016/j.jpsychires.2012.03.018. [DOI] [PubMed] [Google Scholar]
- Semansky R, Koyanagi C, Vandivort-Warren R. Behavioral health screening policies in Medicaid programs nationwide. Psychiatric Services. 2003;54(5):736–739. doi: 10.1176/appi.ps.54.5.736. [DOI] [PubMed] [Google Scholar]
- The Children's Aid Society . Building a Community School. 3rd ed. The Children's Aid Society; New York: 2001. [April 23, 2015]. http://www.rsd.k12.pa.us/Downloads/Development_Chart_for_Booklet.pdf. [Google Scholar]
- Tori CM, Encino's W, Bedrail T, McCormick MC, Simpson LA. Annual report on health care for children and youth in the United States: National estimates of cost, utilization and expenditures for children with mental health conditions. Academic Pediatrics. 2015;15(1):19–35. doi: 10.1016/j.acap.2014.07.007. [DOI] [PubMed] [Google Scholar]
- Visser SN, Kramer D, Snyder AB, Sebian J, McGiboney G, Handler A. Student-perceived school climate is associated with ADHD medication treatment among adolescents in Medicaid. Journal of Attention Disorders. 2015 doi: 10.1177/1087054715569601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter HJ, Gouze K, Cicchetti C, Arend R, Mehta T, Schmidt J, Skavarla M. A pilot demonstration of comprehensive mental health services in inner-city public schools. Journal of School Health. 2011;81(4):185–193. doi: 10.1111/j.1746-1561.2010.00578.x. [DOI] [PubMed] [Google Scholar]
- Weiss CL, Blizzard AM, Vaughan C, Sydnor-Diggs T, Edwards S, Stephan SH. Supporting the transition from inpatient hospitalization to school. Child and Adolescent Psychiatric Clinics of North America. 2015;24:371–383. doi: 10.1016/j.chc.2014.11.009. [DOI] [PubMed] [Google Scholar]
- Wyman PA, Cross W, Brown CH, Yu Q, Tu X, Eberly S. Intervention to strengthen emotional self-regulation in children with emerging mental health problems: Proximal impact on social behavior. Journal of Abnormal Child Psychology. 2010;38(5):707–720. doi: 10.1007/s10802-010-9398-x. [DOI] [PMC free article] [PubMed] [Google Scholar]