Abstract
Major depressive disorder (MDD) is a prevalent and frequently comorbid psychiatric disorder. This study evaluates the development of depressive symptoms, MDD diagnosis, and suicidal ideation in a high-risk sample (N=524) diagnosed with conduct disorder (CD) and substance use disorder (SUD) symptoms as youth and re-assessed approximately 6.5 years later. Dual trajectory classes of both alcohol and other drug use (AOD) and antisocial behavior (ASB), previously identified using latent class growth analyses (LCGA), were used to predict depression outcomes. The Dual Chronic, Increasing AOD/Persistent ASB, and Decreasing Drugs/Persistent ASB classes had higher past-week depression scores, more past-year MDD symptoms, and were more likely to have past-year MDD than the Resolved class. The Dual Chronic and Decreasing Drugs/Persistent ASB classes also had more past-year MDD symptoms than the Persistent AOD/Adolescent ASB class. Youth at highest risk for developing or maintaining depression in adulthood had the common characteristic of persistent antisocial behavior. This suggests young adulthood depression is associated more with persistent antisocial behavior than with persistent substance use in comorbid youth. As such, interventions targeting high-risk youth, particularly those with persistent antisocial behavior, are needed to help reduce the risk of severe psychosocial consequences (including risk for suicide) in adulthood.
Keywords: Trajectories, Longitudinal, At-risk, Suicidal ideation, Conduct disorder
1. Introduction
Major depressive disorder (MDD) is one of the most common mental disorders. The past-year prevalence of MDD during adolescence and early adulthood reaches 12.4% (Kessler and Walters, 1998), and the lifetime prevalence in the U.S. general population is 16.6% (Kessler et al., 2005). MDD is associated with severe psychosocial consequences including role impairment, poor quality of life, and risk for suicide (Lewinsohn et al., 1998; Kessler et al., 2003) Because of these negative outcomes, depression has been a major focus of mental health prevention and intervention efforts, particularly in youth (Lewinsohn et al., 1995; Reinherz et al., 2000). Risk factors associated with higher levels of depressive symptoms in adolescence and early adulthood include low socioeconomic status (Melchior et al., 2013), delinquency or conduct problems (Kandel and Davies, 1982; Lewinsohn et al., 1994; Angold et al., 1999), cigarette smoking (Brook et al., 2004), and other substance use (Cook et al., 2007).
In U.S. epidemiological studies, MDD is associated with both alcohol use disorders (AUDs) and other substance use disorders (SUDs), as well as with conduct disorder (CD) and antisocial personality disorder (Regier et al., 1990; Kessler et al., 1996; Holdcraft et al., 1998; Wolff and Ollendick, 2006). Associations between SUDs and mood disorders are greater for dependence than abuse and are stronger in females than males (Conway et al., 2006). Longitudinal studies have demonstrated both unidirectional and reciprocal effects between SUDs and the development of MDD (Schuckit, 1983; Giaconia et al., 2001). Clinical studies indicate individuals with comorbid MDD and SUDs have poorer treatment outcomes (Schmitz et al., 2001; Kirchner et al., 2002; Cornelius et al., 2005).
Studies also demonstrate associations between depressive symptoms and antisocial behavior. For example, Bor and colleagues found adults with adolescent onset and life course persistent antisocial behavior exhibited elevated rates of depressive symptoms (Bor et al., 2010). Burke and colleagues reported that CD influenced later MDD through psychosocial impairment (Burke et al., 2005). In addition, some studies demonstrate that adolescent conduct problems tend to precede adult depression (Zoccolillo, 1992; Hofstra et al., 2002), and adults with histories of both CD and MDD have worse outcomes and poorer prognoses (Marmorstein and Iacono, 2003).
A few longitudinal studies have demonstrated prospective effects of adolescent antisocial behavior on later depression. The age of onset for antisocial behaviors usually precedes the age of onset for depression (Biederman et al., 1995; Nock et al., 2006) and data from the National Comorbidity Survey Replication study found that CD preceded depression in 72% of cases (Nock et al., 2006). These findings are consistent with a “failure model” hypothesis, which suggests depression results from the social and educational failures that often follow early onset antisocial behavior (Capaldi and Stoolmiller, 1999).
SUDs and antisocial behavior are often chronic conditions (Giaconia et al., 2001; Marmorstein and Iacono, 2003), and each have been shown to increase depression (Giaconia et al., 2001; Hofstra et al., 2002; Cornelius et al., 2005; Cook et al., 2007; Bor et al., 2010). The comorbidity of SUDs and antisocial behavior is well-documented, but few studies have investigated their combined influence on the emergence of depression. Wymbs et al. (2014) assessed early adolescent substance use as a risk factor for developing conduct disorder and depressive symptoms in a community sample of middle school students. Results indicated substance use predicted conduct disorder symptoms, but failed to predict depressive symptoms in last adolescence. Additional research is needed to understand how these comorbid disorders jointly influence the development of depression and affect psychosocial outcomes to improve our prognostic abilities and allow for better prevention and treatment of those at risk.
Trajectory analyses of longitudinal data increasingly have been used to examine substance use and antisocial behavior over time (Di Giunta et al., 2010; Ensor et al., 2010; Marti et al., 2010; Van Ryzin and Dishion, 2012). In addition, there are a few longitudinal studies using this methodology that have examined the effect of substance use and/or antisocial behavior on the development of depressive symptoms. For example, a study using trajectory analyses of an inpatient adult psychiatric sample found more severe depression trajectories were associated with female sex, trauma exposure, prior psychiatric hospitalization, and a primary MDD diagnosis, while a less severe depression trajectory was associated with AUDs/SUDs (Clapp et al., 2013). Wiesner et al. (2005) examined developmental trajectories in a sample of young adult offenders and found that even after controlling for antisocial propensity, parental criminality, demographic factors and baseline levels of each outcome, young adults who were chronic high-level offenders had higher levels of depressive symptoms compared with young adults in three other trajectory groups: very rare, decreasing low-level, and decreasing high-level offenders. Measelle et al. (2006) studied the temporal relationship between antisocial behavior and depression in adolescent girls using a developmental trajectory model and found that initial level of antisocial behavior predicted increases in depressive symptoms. Stice et al. (2004) evaluated data from 496 adolescent girls to test the temporal relationship between substance abuse and depression and reported that substance abuse symptoms predicted onset of depression. Using the same sample of adolescent girls, Marti et al. (2010) found problematic substance use and abuse trajectory groups showed elevations in depressive symptoms relative to non-problematic groups. The majority of these studies, to date, have only focused on the individual understanding of substance use or antisocial behavior on depression.
In a prior study from our laboratory, we used bivariate trajectory analyses to evaluate prospective data from a sample of high-risk youth who had both CD and SUD symptoms in adolescence (Trim et al., 2015). Using this novel person-centered analytic approach, we identified longitudinal patterns of conjoint substance use and antisocial behavior from adolescence into young adulthood. Five distinct subgroups were identified based on the combination of alcohol and other drug (AOD) use and antisocial behavior (ASB) trajectories: Dual Chronic, Increasing AOD/Persistent ASB, Persistent AOD/Adolescent ASB, Decreasing Drugs/Persistent ASB, and Resolved. The current study extends this work and evaluates depressive symptoms and diagnoses in these five subgroups to determine the combined influence of substance use and antisocial behavior on the development of depression in early adulthood. As a secondary outcome, we also examined suicidal ideation in those participants with a MDD diagnosis in early adulthood.
2. Methods
2.1. Participants
This study used a sample of youth 13–19 years of age and who were originally recruited for studies on familial transmission and genetic linkage of SUDs and CD (Derringer et al., 2015; Trim et al., 2015). The participants were recruited from three sites between 1993 and 2007: substance use treatment programs in Denver, Colorado (n=352); the Colorado criminal justice system (n=202); and treatment programs/alternative schools for behaviorally troubled youth in San Diego, California (n=245). (All participants N=799) met inclusion criteria for having at least one CD symptom and one non-tobacco alcohol or other drug symptom at the baseline assessment. Participants who completed a follow-up interview and were at least 19 years old at follow-up (n=536) were included in our prior study of bivariate trajectories (Trim et al., 2015). Depression measures were missing from 12 participants either at baseline or the early adult follow-up assessment. Thus, the current study includes 524 participants (66% of the initial sample) with a mean age of 16.1 (SD=1.2) years at baseline and a mean age of 22.6 (SD=2.0) years at follow-up approximately 6.5 years later. Attrition analyses revealed this subsample did not differ significantly from the initial sample on MDD severity (p=.28) or past-year MDD diagnosis (p=.41) at baseline, nor was there any evidence of bias due to attrition in any baseline demographic variables.
2.2. Measures
2.2.1. Baseline depression
At baseline each participant completed the Diagnostic Interview Schedule for Children (DISC), a highly structured computerized interview designed for assessment of DSM-IV diagnoses by non-clinicians (Shaffer et al., 1993). In this study baseline DISC responses were used to assess the total count of past-year MDD symptoms and DSM-IV diagnosis of past-year MDD, which were used to examine potential baseline differences between trajectory classes and as covariates in the main analyses.
2.2.2. Follow-up depression
At follow-up each participant completed the Center for Epidemiologic Studies Depression Scale (CES-D), a 20-item self-report measure of depressive symptoms during the past week (Radloff, 1977). The CES-D had high internal consistency in this sample (Cronbach’s α=.88). Participants also completed the Diagnostic Interview Schedule for DSM-IV (DIS-IV), a structured and computerized diagnostic interview designed for non-clinicians (Helzer et al., 1987). In this study DIS-IV responses were used to measure the total count of past-year MDD symptoms and past-year DSM-IV diagnosis of MDD. An additional item administered to participants with past-year MDD (“Did you think about committing suicide?”) was also used to examine past-year suicidal ideation.
2.2.3. AOD and ASB trajectory classes
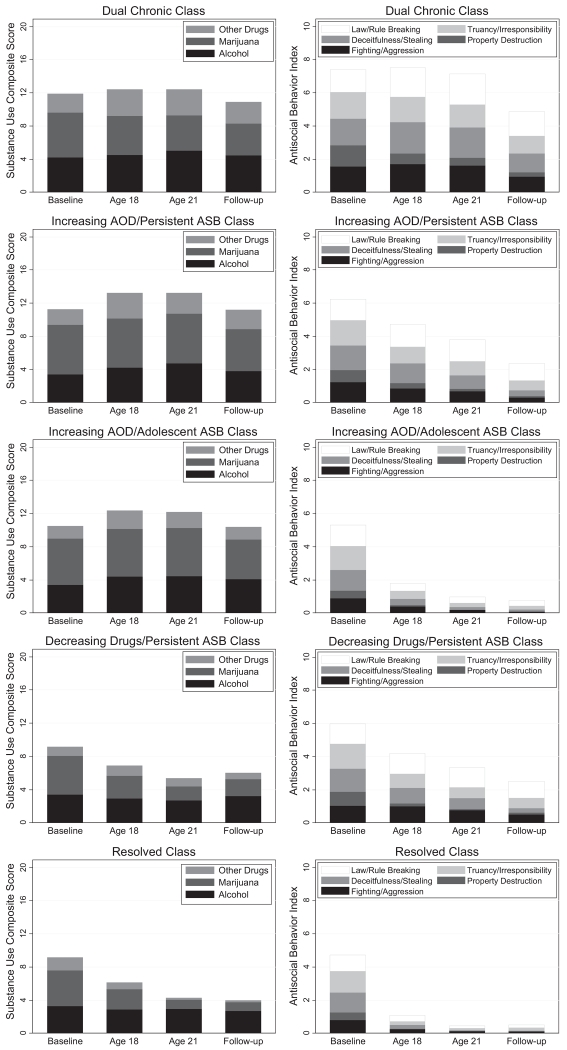
Participants reported substance use on the Composite International Diagnostic Interview Substance Abuse Module (CIDI-SAM), a structured diagnostic interview (Crowley et al., 2001) administered at baseline and follow-up. Past-year frequency scores for alcohol, marijuana and other drug use (ranging from 0 “Never” to 7 “Daily”) were summed to create a composite AOD index (Range of 0–21). On the DISC (baseline) and the DIS-IV (follow-up) participants reported on five behavioral domains of ASB: law/rule-breaking, truancy and irresponsibility, stealing/deceitfulness, property destruction, and fighting/aggression. Past-year scores for each domain, ranging from 0 (None) to 2 (2 or more behaviors), were summed to create the composite ASB index (Range of 0–10). In addition to baseline and follow-up AOD and ASB scores, participants age 22 or older at follow-up reported on AOD symptoms and ASB behaviors for age 18 and age 21 (87% of the sample was at least 21 at follow-up). Using all available measures of AOD and ASB, our prior work identified five bivariate longitudinal trajectory classes using LCGA. Details on this analytic process can be found in our previous study (Trim et al., 2015); the 5-class solution was chosen based on recommended guidelines of model selection (BIC=16710, entropy=.822, LMR-LRT p<.05, BLRT p<.001, posterior probabilities from .84 to .96.). The five classes defined by disparate patterns of AOD and ASB over time (see Fig. 1) are:
Class 1: Dual chronic (9.5%): defined by the highest baseline AOD, no significant change in AOD over time, high baseline ASB, and a significant non-linear change in ASB that peaked in early adulthood and declined thereafter.
Class 2: Increasing AOD/Persistent ASB (18.1%): defined by slightly lower baseline AOD than Class 1, a significant increase in AOD over time, relatively high baseline ASB, and a non-significant decline in ASB over time.
Class 3: Persistent AOD/Adolescent ASB (29.0%): defined by consistently high levels of AOD, no significant change in AOD over time, and a rapid decline in ASB from high baseline levels, suggestive of adolescent-limited pattern of ASB for this group.
Class 4: Decreasing drugs/Persistent ASB (11.8%): defined by the second highest rates of baseline AOD, a significant decrease in AOD over time (attributable largely to reductions in marijuana use), the highest levels of ASB at baseline, with a modest decline in ASB that remained relatively high over time (second only to Class 1).
Class 5: Resolved (31.5%): defined by high rates of initial AOD, early decline in AOD that stabilized at low levels, the lowest baseline ASB, and a rapid decline of ASB by age 18 suggestive of adolescent-limited ASB (similar to Class 3).
Fig. 1.
Alcohol and other drug use (AOD) and antisocial behavior (ASB) indices across time for each trajectory class.
2.3. Statistical analyses
Chi-square tests and analysis of variance (ANOVA) were used in preliminary analyses to examine associations between baseline depression measures, sex, and the five trajectory classes previously identified in LCGA (Nagin, 1999). Paired-sample t-test and McNemar’s test were used to examine change in depression measures from baseline to follow-up. Sex differences on depression measures at follow-up were also examined using chi-square tests and ANOVA. Additional covariates tested in univariate analyses included baseline depression, ethnicity, and years of education.
The primary analyses examined associations between trajectory class and depression outcomes at follow-up, including past-week CES-D score, past-year MDD severity (symptom count), and past-year MDD diagnosis. All analyses controlled for sex and MDD severity at baseline. We used analysis of covariance (ANCOVA) to model CES-D score and past-year MDD severity and logistic regression to model past-year MDD diagnosis. After testing statistical significance of the overall trajectory class variable, follow-up analyses compared individual trajectory classes, beginning with the Resolved class as the referent and examining all pairwise comparisons. As a secondary analysis, we used chi-square analysis to examine the association between trajectory class and suicidal ideation for the subsample of participants who had past-year MDD diagnosis at follow-up. The rationale for this subsample analysis was both theoretical (suicidal ideation has a low base-rate in non-depressed samples) and practical (only participants who endorsed MDD screeners on the DIS completed items related to suicide). All analyses were conducted in Stata 13.0 (StataCorp., 2013).
3. Results
3.1. Depression at baseline
At baseline the mean past-year MDD severity was 1.2 (SD=2.23) symptoms with the majority of participants (72%, n=378) endorsing no symptoms, and 12% of the sample (n=63) meeting criteria for past-year MDD diagnosis. There was a significant sex difference in baseline MDD severity, F(1, 522)=28.79, p<.001), with women having more MDD symptoms (M=2.03, SD=2.67) than men (M=0.87, SD=1.97). Women also were significantly more likely to have a baseline past-year MDD diagnosis than men (22.5% of women and 8.3% of men), χ2 (1)=19.30, p<.001. As shown in Table 1, there was a significant association between sex and trajectory class, χ2(4)=58.85, p<.001, with men more likely to be in the Dual Chronic (z=4.11, p<.001), Increasing AOD/Persistent ASB (z=5.12, p<.001), or Persistent AOD/Adolescent ASB class (z=5.15, p<.001) than the Resolved class. Analyses of depression outcomes included sex as a covariate to control for potential confounding effects. There were no significant differences across the five trajectory classes on past-year MDD severity, F(4, 519)=.35, p=.84, or past-year MDD diagnosis, χ2(4)=.67, p=.96, at baseline (see Table 1).
Table 1.
Descriptive statistics of depression outcomes and covariates for the full sample (N=524) and with in each trajectory class.
| Full sample | Latent trajectory groups | |||||
|---|---|---|---|---|---|---|
|
|
||||||
|
(n=50) dual
chronic |
(n=95)increasing AOD/
persistent ASB |
(n=152) persistent AOD/
adolescent ASB |
(n=62) decreasing drugs/
persistent ASB |
(n=165)
resolved |
||
| Baseline variables | ||||||
| Recruitment source | ||||||
| Alternative school or community |
33.0% | 33.0% | 34.7% | 32.2% | 35.5% | 33.9% |
| Treatment facilities | 43.9% | 43.9% | 43.2% | 45.1% | 50.0% | 37.6% |
| Juvenile justice | 23.1% | 23.1% | 22.1% | 22.4% | 14.5% | 25.5% |
| Sex (proportion male) | 73.7% | 92.0% | 88.4% | 82.9% | 62.9% | 55.2 |
| Race (proportion white) | 51% | 52% | 56% | 59% | 44% | 44% |
| MDD symptom count: M (SD) | 1.2 (2.2) | 1.2 (2.4) | 1.0 (2.2) | 1.2 (2.1) | 1.3 (2.3) | 1.3 (2.3) |
| Past-year MDD diagnosis | 12.0% | 12.0% | 10.5% | 11.8% | 12.9% | 12.7 |
|
Follow-up depression
outcomes |
||||||
| CES-D score: M (SD) | 12.3 (9.8) | 16.9 (12.1) | 13.3 (11.2) | 11.3 (8.8) | 13.9 (10.4) | 10.7 (8.3) |
| MDD symptom count: M (SD) | 0.93 (2.3) | 1.5 (3.0) | 1.0 (2.5) | 0.7 (1.9) | 1.7 (3.0) | 0.7 (1.7) |
| MDD diagnosis | 8.9% | 16.0% | 10.5% | 6.6% | 19.4% | 4.2 |
| Suicidal ideation | 17% | 50% | 10% | 0% | 25% | 0% |
3.2. Depression at follow-up
As shown in Table 1, the mean past-week CES-D score at follow-up was 12.3 (SD=9.84), which is within the range of mild depressive symptoms. Mean past-year MDD severity was 0.93 (SD=2.26) symptoms, with most of the sample (73%, n=386) endorsing no symptoms during the past year and 9% of the sample (n=47) meeting DSM-IV criteria for past-year MDD diagnosis at follow-up. Sex was a significant predictor of depression at follow-up, for past-week CES-D score, F(1, 522)=4.42, p<0.05), past-year MDD severity, F(1, 522)=12.39, p<.001), and past-year MDD diagnosis, χ2 (1)=8.96, p<.01. Women had higher CES-D scores (M=13.83, SD=11.9) than men (M=11.79, SD=9.27), had more past-year MDD symptoms (M=1.51, SD=2.78) than men (M=0.73, SD=2.00), and were more likely to have a past-year MDD diagnosis (15.2%) than men (6.7%). Sex differences in suicidal ideation at follow-up were not statistically significant. Baseline depression severity also predicted past-week CES-D score, F(1, 522)=11.89, p<.001), past-year MDD severity, F(1,522)=24.16, p<.001), and past-year MDD diagnosis, χ 2 (1)=3.96, p<.05), but not past-year suicidal ideation. Ethnicity and years of education did not significantly predict depression at follow-up.
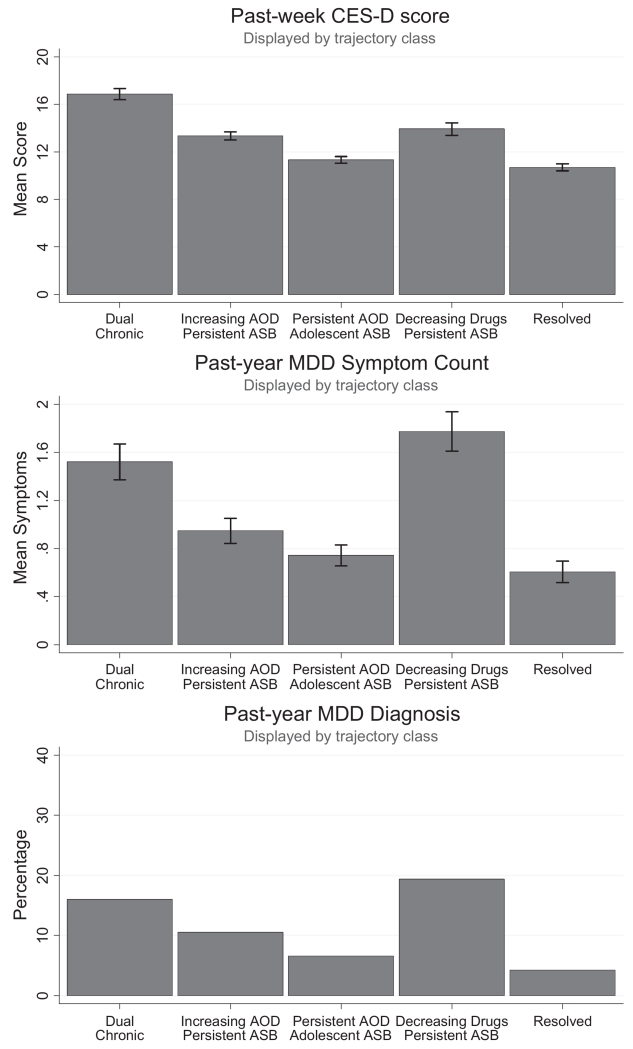
3.3. Associations between trajectory class and depression at follow-up
Table 2 displays the results of ANCOVA models used to examine the associations between trajectory classes and depression outcomes at follow-up, controlling for the effects of sex and baseline MDD severity. ANCOVA revealed significant differences between trajectory classes on CES-D score, F(4, 517)=6.21, p<.001, R2=.07. The Dual chronic (t=4.48, p<.001), Increasing AOD/Persistent ASB (t=2.87, p=.004), and Decreasing drugs/Persistent ASB (t=2.39, p=.02) classes all had significantly higher CES-D scores than the Resolved class. Furthermore, the Dual Chronic class had significantly higher CES-D scores than the Increasing AOD/Persistent ASB class (t=2.07, p=.04), the Persistent AOD/Adolescent ASB class (t=3.69, p<.001) and the Decreasing drugs/Persistent ASB class (t=2.03, p=.04). Mean CES-D scores for each of the five trajectory classes (adjusted for sex and baseline MDD severity) are shown in Fig. 2.
Table 2.
Results of ANCOVA and logistic regression models examining associations between trajectory classes and depression outcomes at follow-up, controlling for sex and baseline depression severity.
| ANCOVA |
Logistic regression |
||||
|---|---|---|---|---|---|
| CES-D score | MDD symptom count | MDD diagnosis |
|||
| b | β | b | β | OR | |
| Dual chronic | 7.11*** | 0.21 | 1.19** | 0.21 | 7.05** |
|
Increasing AOD/per-
sistent ASB |
3.67** | 0.14 | 0.64* | 0.14 | 4.28** |
|
Persistent AOD/ado-
lescent ASB |
1.39 | 0.06 | 0.36 | 0.06 | 2.21 |
|
Decreasing drugs/
persistent ASB |
3.40* | 0.11 | 1.22*** | 0.11 | 6.22*** |
| Sex (male) | −2.52* | −0.12 | −0.74** | −0.12 | .37** |
| Baseline MDD severity |
0.56** | 0.12 | 0.18*** | 0.12 | 1.21*** |
Note. The “Resolved” class was treated as the referent group in ANCOVA and logistic regression models. Coefficients for ANCOVA models indicate the difference between each class and the referent, adjusted for covariates.
p<.05;
p<.01;
p<.001
Fig. 2.
Depression outcomes at follow-up for each trajectory class, adjusted for sex and baseline MDD severity.
As shown in Table 2, there also were statistically significant differences between trajectory classes in past-year MDD severity, F (4, 517)=5.27, p<.001, R2=.09. Controlling for the effects of sex and baseline MDD severity, the Dual chronic class (t=3.31, p=.001), Increasing AOD/Persistent ASB class (t=2.22, p=.03), and Decreasing drugs/Persistent ASB class (t=3.77, p<.001) had significantly more past-year MDD symptoms at follow-up than the Resolved class. The Dual Chronic class (t=2.34, p=.02) and Decreasing drugs/Persistent ASB class (t=2.60, p=.01) also had significantly more past-year MDD symptoms than the Persistent AOD/Adolescent ASB class. No other between-group differences were statistically significant. Fig. 2 displays the mean MDD past-year symptom counts for each of the five classes, adjusted for sex and baseline MDD severity.
Logistic regression was used to examine the relationship between trajectory class and past-year MDD diagnosis. As shown in Table 2, trajectory class was significantly associated with past-year MDD, χ2(4)=17.37, p<.01, with the Dual Chronic (OR=7.05, z=3.29, p=.001), Increasing AOD/Persistent ASB (OR=4.28, z=2.34, p=.008), and Decreasing drugs/Persistent ASB classes (OR=6.22, z=3.50, p<.001) having significantly higher rates of MDD than the Resolved class. The Dual chronic class (OR=3.19, z=2.19, p=.03) and Decreasing drugs/Persistent ASB class (OR=2.81, z=2.14, p=.03) also had significantly higher rates of MDD than the Persistent AOD/Adolescent ASB class. Covariate-adjusted rates of past-year MDD diagnosis for each trajectory class are shown in Table 2.
3.4. Suicidal ideation at follow-up in MDD subsample
Among participants with past-year MDD at follow-up (n=47), 17% (n=8) reported suicidal ideation. There was a significant association between trajectory class and suicidal ideation, χ2(4)=10.54, p<.05. None of the participants in the Persistent AOD/Adolescent ASB or Resolved classes with past-year MDD reported suicidal ideation. Compared to these two classes, the prevalence of suicidal ideation was significantly greater in the Dual chronic class (50% of those with past-year MDD), the Increasing AOD/Persistent ASB class (10% of those with past-year MDD), and the Decreasing drugs/Persistent ASB class (25% of those with past-year MDD), although the pairwise differences between these three classes were not statistically significant.
4. Discussion
Depression is one of the most common psychiatric disorders (Kessler and Walters, 1998) and previous research has demonstrated that youth with SUDs (Schuckit, 1983; Giaconia et al., 2001) or with CD (Zoccolillo, 1992; Hofstra et al., 2002; Burke et al., 2005; Bor et al., 2010) are at elevated risk for depression in adulthood. Despite these frequent comorbidities, it is not well understood how the combined, longitudinal course of SUD and CD symptoms in adolescence influence the later development of depression. Findings from this prospective study of high-risk youth utilized bivariate trajectory groups identified in a previous study (Trim et al., 2015) to determine whether persistence of substance use and antisocial behavior was related to young adult depression. Three different measures of depression were assessed to determine the consistency of findings across continuous vs. dichotomous outcomes (MDD symptom count and diagnosis), as well as across timeframes (past-year for MDD and past-week for CES-D). Participants with declining substance use and antisocial behavior (Resolved class) had the least severe depression in young adulthood. Relative to this group, participants with the most severe depression in young adulthood were associated with one of three classes: Dual chronic, Increasing AOD/Persistent ASB, and Decreasing drugs/Persistent ASB, despite having similar rates of depression as the Resolved class at baseline. The common characteristic of these three trajectory classes is the persistence of antisocial behavior, which suggests this has a strong association with young adult depression regardless of the level of concurrent substance use.
Our results suggest that high-risk youth with SUD and CD symptoms are particularly prone to depression when their antisocial behavior persists into adulthood. Consistent with the failure model, which hypothesizes depression results from social and educational failures that follow early onset antisocial behavior (Capaldi and Stoolmiller, 1999), results from our prior study found that the three classes with persistent antisocial behavior had the highest rates of past year job loss, incarceration, relationship problems, and serious illness/injury (Trim et al., 2015). The current study also found that these classes had significantly higher rates of suicidal ideation among those with a MDD diagnosis. Because of the severe psychosocial consequences associated with substance use, antisocial behavior, and depression (including risk for suicide), interventions targeted at high-risk youth, particularly those with persistent antisocial behavior, are warranted. Our findings suggest treatments for high-risk youth that restrict antisocial behavior to adolescence could potentially reduce the incidence of young adult depression in this population.
Interestingly, the participants most likely assigned to the class with consistently high levels of substance use and declining antisocial behavior (Increasing AOD/Adolescent ASB) did not show elevated levels of depression at follow-up compared to those individuals in the referent (Resolved) class, even though the rate of recent substance dependence in the Increasing AOD/Adolescent ASB class was double that of the Resolved class (41% vs 19%) (Trim et al., 2015). We previously found the Increasing AOD/Adolescent ASB class also had the lowest rates of recent incarceration (8%) and relationship problems (27%) and had rates of antisocial personality disorder (14%) similar to those in the Resolved class (Trim et al., 2015). Thus, “maturing out” of adolescent antisocial behavior, but not necessarily substance use, seems to be a protective factor against depression and adverse functional outcomes in adulthood. Even though this subsample of high-risk youth continued to engage in high levels of problematic substance use in adulthood, it appears that avoiding the negative life consequences associated with persistent antisocial behavior buffered against the development of early adulthood depression.
This study has several strengths. This is the first longitudinal study to examine depression outcomes as they relate to concurrent substance use and antisocial behavior over adolescence and early adulthood in a relatively large sample of high-risk youth. Importantly, we controlled for the effects of sex and baseline depression in our analyses and found a consistent pattern of results using different measures of depression (CES-D and DSM-IV MDD criteria). Several study limitations also should be noted. Because this was a study of high-risk, mostly male adolescents, the findings may not generalize to other samples of youth. In addition, the psychiatric assessments relied on self-report and therefore may be influenced by recall and/or reporter bias, and follow-up depression measures were not available for a substantial portion of the original sample, which may have biased the results. Relatedly, suicidal ideation was likely underestimated because it was based on a single item that was administered only to those participants who endorsed past-year MDD symptoms. Despite these limitations, this study found that the persistence of antisocial behavior is associated with elevations in young adult depression in high-risk youth with both SUD and CD symptoms and the findings have important implications for intervening with those at highest risk for severe psychosocial outcomes.
Acknowledgement
This project was supported by National Institute of Drug Abuse Grants R01 DA021692 (PIs: Brown & Wall), R01 DA035804 (PIs: Hopfer, Stallings & Wall), F31 DA030861 (PI: Worley), P60 DA011015 (PI: Hewitt), R01 DA012845 (PI: Hewitt), and R01 DA021913 (PI: Hopfer), and R01 DA015522 (PI: Hopfer).
Footnotes
Contributors
All co-authors contributed significantly to the writing of this manuscript.
Conflict of interest
None.
References
- Angold A, Costello EJ, Erkanli A. Comorbidity. J. Child Psychol. Psychiatry. 1999;40(1):57–87. [PubMed] [Google Scholar]
- Biederman J, Faraone S, Mick E, Lelon E. Psychiatric comorbidity among referred juveniles with major depression: fact or artifact? J. Am Acad. Child. Adolesc. Psychiatry. 1995;34(5):579–590. doi: 10.1097/00004583-199505000-00010. [DOI] [PubMed] [Google Scholar]
- Bor W, McGee TR, Hayatbakhsh R, Dean A, Najman JM. Do antisocial females exhibit poor outcomes in adulthood? An Australian cohort study. Aust NZ J. Psychiatry. 2010;44(7):648–657. doi: 10.3109/00048671003631159. [DOI] [PubMed] [Google Scholar]
- Brook JS, Schuster E, Zhang C. Cigarette smoking and depressive symptoms: a longitudinal study of adolescents and young adults. Psychol. Rep. 2004;95(1):159–166. doi: 10.2466/pr0.95.1.159-166. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. J. Child. Psychol. Psychiatry. 2005;46(11):1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Stoolmiller M. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: III. prediction to young-adult adjustment. Dev. Psychopathol. 1999;11(1):59–84. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Clapp JD, Grubaugh AL, Allen JG, Mahoney J, Oldham JM, Fowler JC, Ellis T, Elhai JD, Frueh BC. Modeling trajectory of depressive symptoms among psychiatric inpatients: a latent growth curve approach. J. Clin. Psychiatry. 2013;74(5):492–499. doi: 10.4088/JCP.12m07842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the national Epidemiologic survey on alcohol and related conditions. J. Clin. Psychiatry. 2006;67(2):247–257. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- Cook JA, Grey DD, Burke-Miller JK, Cohen MH, Vlahov D, Kapadia F, Wilson TE, Cook R, Schwartz RM, Golub ET, Anastos K, Ponath C, Goparaju L, Levine AM. Illicit drug use, depression and their association with highly active antiretroviral therapy in HIV-positive women. Drug Alcohol Depend. 2007;89(1):74–81. doi: 10.1016/j.drugalcdep.2006.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius JR, Clark DB, Bukstein OG, Birmaher B, Salloum IM, Brown SA. Acute phase and five-year follow-up study of fluoxetine in adolescents with major depression and a comorbid substance use disorder: a review. Addict. Behav. 2005;30(9):1824–1833. doi: 10.1016/j.addbeh.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Mikulich SK, Ehlers KM, Whitmore EA, MacDonald MJ. Validity of structured clinical evaluations in adolescents with conduct and substance problems. J. Am Acad. Child. Adolesc. Psychiatry. 2001;40(3):265–273. doi: 10.1097/00004583-200103000-00005. [DOI] [PubMed] [Google Scholar]
- Derringer J, Corley RP, Haberstick BC, Young SE, Demmitt BA, Howrigan DP, Kirkpatrick RM, Iacono WG, McGue M, Keller MC, Brown S, Tapert S, Hopfer CJ, Stallings MC, Crowley TJ, Rhee SH, Krauter K, Hewitt JK, McQueen MB. Genome-wide association study of behavioral disinhibition in a selected adolescent sample. Behav. Genet. 2015 doi: 10.1007/s10519-015-9705-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Giunta L, Pastorelli C, Eisenberg N, Gerbino M, Castellani V, Bombi AS. Developmental trajectories of physical aggression: prediction of overt and covert antisocial behaviors from self- and mothers’ reports. Eur. Child. Adolesc. Psychiatry. 2010;19(12):873–882. doi: 10.1007/s00787-010-0134-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ensor R, Marks A, Jacobs L, Hughes C. Trajectories of antisocial behaviour towards siblings predict antisocial behaviour towards peers. J. Child. Psychol. Psychiatry. 2010;51(11):1208–1216. doi: 10.1111/j.1469-7610.2010.02276.x. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Paradis AD, Hauf AM, Stashwick CK. Major depression and drug disorders in adolescence: general and specific impairments in early adulthood. J. Am Acad. Child Adolesc. Psychiatry. 2001;40(12):1426–1433. doi: 10.1097/00004583-200112000-00013. [DOI] [PubMed] [Google Scholar]
- Helzer JE, Spitznagel EL, McEvoy L. The predictive validity of lay diagnostic interview schedule diagnoses in the general population. A comparison with physician examiners. Arch. Gen. Psychiatry. 1987;44(12):1069–1077. doi: 10.1001/archpsyc.1987.01800240045007. [DOI] [PubMed] [Google Scholar]
- Hofstra MB, van der Ende J, Verhulst FC. Child and adolescent problems predict DSM-IV disorders in adulthood: a 14-year follow-up of a Dutch epidemiological sample. J. Am Acad. Child Adolesc. Psychiatry. 2002;41(2):182–189. doi: 10.1097/00004583-200202000-00012. [DOI] [PubMed] [Google Scholar]
- Holdcraft LC, Iacono WG, McGue MK. Antisocial personality disorder and depression in relation to alcoholism: a community-based sample. J. Stud. Alcohol. 1998;59(2):222–226. doi: 10.15288/jsa.1998.59.222. [DOI] [PubMed] [Google Scholar]
- Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: an empirical study. Arch. Gen. Psychiatry. 1982;39(10):1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS, National Comorbidity Survey, R. The epidemiology of major depressive disorder: results from the national Comorbidity survey replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national Comorbidity survey replication. Arch. Gen. Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Nelson CB, McGonagle KA, Edlund MJ, Frank RG, Leaf PJ. The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. Am. J. Orthopsychiatry. 1996;66(1):17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the national Comorbidity survey. Depress Anxiety. 1998;7(1):3–14. doi: 10.1002/(sici)1520-6394(1998)7:1<3::aid-da2>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Kirchner JE, Curran GM, Thrush CR, Owen RR, Fortney JC, Booth BM. Depressive disorders and alcohol dependence in a community population. Community Ment. Health J. 2002;38(5):361–373. doi: 10.1023/a:1019804311109. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Gotlib IH, Seeley JR. Adolescent psychopathology: IV. specificity of psychosocial risk factors for depression and substance abuse in older adolescents. J. Am Acad. Child Adolesc. Psychiatry. 1995;34(9):1221–1229. doi: 10.1097/00004583-199509000-00021. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. psychosocial risk factors for depression. J. Abnorm. Psychol. 1994;103(2):302–315. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clin. Psychol. Rev. 1998;18(7):765–794. doi: 10.1016/s0272-7358(98)00010-5. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. Major depression and conduct disorder in a twin sample: gender, functioning, and risk for future psychopathology. J. Am Acad. Child Adolesc. Psychiatry. 2003;42(2):225–233. doi: 10.1097/00004583-200302000-00017. [DOI] [PubMed] [Google Scholar]
- Marti CN, Stice E, Springer DW. Substance use and abuse trajectories across adolescence: a latent trajectory analysis of a community-recruited sample of girls. J. Adolesc. 2010;33(3):449–461. doi: 10.1016/j.adolescence.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Measelle JR, Stice E, Hogansen JM. Developmental trajectories of co-occurring depressive, eating, antisocial, and substance abuse problems in female adolescents. J. Abnorm. Psychol. 2006;115(3):524–538. doi: 10.1037/0021-843X.115.3.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melchior M, Chastang JF, Head J, Goldberg M, Zins M, Nabi H, Younes N. Socioeconomic position predicts long-term depression trajectory: a 13-year follow-up of the GAZEL cohort study. Mol. Psychiatry. 2013;18(1):112–121. doi: 10.1038/mp.2011.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: a semiparametric, group-based approach. Psychol. Methods. 1999;4(2):139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the national comorbidity survey replication. Psychol. Med. 2006;36(5):699–710. doi: 10.1017/S0033291706007082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1(3):385–401. [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. results from the Epidemiologic catchment area (ECA) study. JAMA. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- Reinherz HZ, Giaconia RM, Hauf AM, Wasserman MS, Paradis AD. General and specific childhood risk factors for depression and drug disorders by early adulthood. J. Am. Acad. Child Adolesc. Psychiatry. 2000;39(2):223–231. doi: 10.1097/00004583-200002000-00023. [DOI] [PubMed] [Google Scholar]
- Schmitz JM, Averill P, Stotts AL, Moeller FG, Rhoades HM, Grabowski J. Fluoxetine treatment of cocaine-dependent patients with major depressive disorder. Drug Alcohol Depend. 2001;63(3):207–214. doi: 10.1016/s0376-8716(00)00208-8. [DOI] [PubMed] [Google Scholar]
- Schuckit M. Alcoholic patients with secondary depression. Am. J. Psychiatry. 1983;140(6):711–714. doi: 10.1176/ajp.140.6.711. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Schwab-Stone M, Fisher P, Cohen P, Piacentini J, Davies M, Conners CK, Regier D. The diagnostic interview schedule for Children-Revised version (DISC-R): I. preparation, field testing, interrater reliability, and acceptability. J. Am. Acad. Child Adolesc. Psychiatry. 1993;32(3):643–650. doi: 10.1097/00004583-199305000-00023. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- Stice E, Burton EM, Shaw H. Prospective relations between bulimic pathology, depression, and substance abuse: unpacking comorbidity in adolescent girls. J. Consult Clin. Psychol. 2004;72(1):62–71. doi: 10.1037/0022-006X.72.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trim RS, Worley MJ, Wall TL, Hewitt JK, Hopfer CJ, Crowley TJ, Brown SA. Bivariate trajectories of substance use and antisocial behavior from adolescence through young adulthood. Emerg. Adulthood. 2015;3:265–276. doi: 10.1177/2167696815573791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ, Dishion TJ. The impact of a family-centered intervention on the ecology of adolescent antisocial behavior: modeling developmental sequelae and trajectories during adolescence. Dev. Psychopathol. 2012;24(3):1139–1155. doi: 10.1017/S0954579412000582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiesner M, Kim HK, Capaldi DM. Developmental trajectories of offending: validation and prediction to young adult alcohol use, drug use, and depressive symptoms. Dev. Psychopathol. 2005;17(1):251–270. doi: 10.1017/s0954579405050133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JC, Ollendick TH. The comorbidity of conduct problems and depression in childhood and adolescence. Clin. Child Fam. Psychol. Rev. 2006;9(3–4):201–220. doi: 10.1007/s10567-006-0011-3. [DOI] [PubMed] [Google Scholar]
- Wymbs BT, McCarty CA, Mason WA, King KM, Baer JB, Vander Stoep A, McCauley E. Early substance use as a risk factor for developing conduct disorder and depression symptoms. J. Stud. Alcohol Drugs. 2014;75:279–289. [PMC free article] [PubMed] [Google Scholar]
- Zoccolillo M. Co-occurrence of conduct disorder and its adult outcomes with depressive and anxiety disorders: a review. J. Am Acad. Child Adolesc. Psychiatry. 1992;31(3):547–556. doi: 10.1097/00004583-199205000-00024. [DOI] [PubMed] [Google Scholar]