Abstract
Context:
Knowledge about the specific environmental and practice risks to participants in American intercollegiate football during preseason practices is limited. Identifying risks may mitigate occurrences of exertional heat illness (EHI).
Objective:
To evaluate the associations among preseason practice day, session number, and wet bulb globe temperature (WBGT) and the incidence of EHI.
Design:
Descriptive epidemiology study.
Setting:
Sixty colleges and universities representing 5 geographic regions of the United States.
Patients or Other Participants:
National Collegiate Athletic Association football players.
Main Outcome Measure(s):
Data related to preseason practice day, session number, and WBGT. We measured WBGT every 15 minutes during the practice sessions and used the mean WBGT from each session in the analysis. We recorded the incidence of EHIs and calculated the athlete-exposures (AEs).
Results:
A total of 553 EHI cases and 365 810 AEs were reported for an overall EHI rate of 1.52/1000 AEs (95% confidence interval [CI] = 1.42, 1.68). Approximately 74% (n = 407) of the reported EHI cases were exertional heat cramps (incidence rate = 1.14/1000 AEs; 95% CI = 1.03, 1.25), and about 26% (n = 146) were a combination of exertional heat syncope and heat exhaustion (incidence rate = 0.40/1000 AEs; 95% CI = 0.35, 0.48). The highest rate of EHI occurred during the first 14 days of the preseason period, and the greatest risk was during the first 7 days. The risk of EHI increased substantially when the WBGT was 82.0°F (27.8°C) or greater.
Conclusions:
We found an increased rate of EHI during the first 14 days of practice, especially during the first 7 days. When the WBGT was greater than 82.0°F (27.8°C), the rate of EHI increased. Sports medicine personnel should take all necessary preventive measures to reduce the EHI risk during the first 14 days of practice and when the environmental conditions are greater than 82.0°F (27.8°C) WBGT.
Key Words: environmental conditions, heat injuries, weather monitoring, wet bulb globe temperature
Key Points
The greatest risk of exertional heat illness (EHI) among American collegiate football players occurred during the first 14 days of preseason practice.
The rate of EHI was related to the number of practice sessions held during the preseason period.
The relative risk of EHI was low when wet bulb globe temperature was less than 82.0°F (27.8°C) and increased when it was between 82.0°F and 86.0°F (30.0°C).
Exertional heat illness (EHI) is one of many conditions with which athletic trainers (ATs) must contend when supervising the participation of collegiate student-athletes in preseason football practice sessions. Specifically, 2 EHI categories, exertional heat stroke (EHS) and heat exhaustion (HE), are serious illnesses that can be debilitating and potentially life threatening if appropriate prevention strategies and treatment regimens are not used (Table 1). From 1960 to 2009, 123 cases of heat-related deaths were reported among American football participants in the United States.2 Heat-related deaths increased substantially since 1975: 24 deaths were reported from 1975 to 1994, but over the next 15 years (1995 to 2009), 42 deaths occurred.3 In fact, the 5-year period from 2005 to 2009 included the greatest number of heat-related deaths (n = 18) in high school and collegiate sports for any 5-year period over the previous 35 years.3 From 1988 to 2004, the National Collegiate Athletic Association (NCAA) Injury Surveillance System4 reported 1687 EHI occurrences that resulted in time-loss injuries for athletes during fall (August to October) football practices. Whereas the NCAA data did not specifically identify EHI occurrences as heat cramps, HE, or EHS, they showed that over the 16-year period, an average of 104.3 EHIs per year occurred. This number represents approximately 5.6% of the total preseason practice injuries per year and an EHI injury rate of 0.44 per 1000 athlete-exposures (AEs).4 In a recent retrospective analysis, Grundstein et al5 documented 58 deaths of US football players from 1980 to 2009 that were attributable to hyperthermia. When the dataset included information beginning in 1960, the number increased to 123.
Table 1. .
Definitions of Exertional Heat Illnesses1
| Exertional Heat Illness Type |
Definition |
| Heat cramps | Condition that presents during or after intense exercise as an acute, painful, involuntary muscle contraction |
| Heat syncope | Orthostatic dizziness accompanied by a brief episode of fainting |
| Heat exhaustion | Inability to continue exercise associated with heavy sweating, dehydration, sodium loss, and energy depletion |
| Exertional heat stroke | Elevated core temperature >40°C associated with signs of organ system failure due to hyperthermia |
| Exertional hyponatremia | Serum sodium levels <130 mmol/L (130 mEq/L) |
The EHI occurrences may be attributable to the inability to acclimatize to hot-weather stresses while participating in athletic activities. This illness is not caused by a single factor; rather, it is multifaceted. Heat acclimatization implies that biological functioning has adapted to a more stressful weather condition (eg, increased wet bulb globe temperatures [WBGTs]), allowing an individual to better regulate body temperature during extreme environmental conditions. The acclimatization process is accomplished through repeated exposure to a hot environment so that increases in both core and skin temperatures invoke the sweat response. The effects of heat acclimatization on exercise capability are often substantial, and without acclimatization, the athlete's ability to exercise at maximum level is limited. The heat-acclimatized athlete can often perform sustained athletic activities that were not possible before the acclimatization process.6 The American College of Sports Medicine (ACSM) position stand7 on EHI during training and competition stipulates that heat acclimatization is the best method to protect the athlete against EHS and HE. The position stand relies heavily on WBGT measurements and recommends specific training regimes when WBGTs reach certain levels. Gradual exposure to these conditions and gradual increases in exercise intensity and duration are critical to the athlete's ability to acclimatize during preseason training.
Numerous authors8–11 have indicated that the risk of EHI increases as the WBGT increases during periods of intense exercise. An individual who participates in activities when the WBGT value is high experiences increased physiologic heat gain through both convection and radiation. In addition, the body's ability to compensate for this heat gain is impaired due to high humidity levels, which slow the evaporation process associated with the sweating mechanism.
Investigators10,12–16 have suggested that the acclimatization process can take 8 to 14 days and, in some cases, up to 2 months. The EHI incidence appears to be elevated during this time, as data from the NCAA Surveillance System4 indicated that the first 21 days of preseason practice resulted in the greatest frequency of EHIs for collegiate football players. Similarly, researchers investigating EHIs among 5 NCAA Division I universities in the Southeast during a single season17 observed similar results, noting that EHI was more frequent in August (8.95/1000 AEs) than in September (1.7/1000 AEs) or October (0.00/1000 AEs). However, these findings were limited by the small number of participating institutions and single geographical area. To alleviate these concerns, we studied a national sample that used a digital environmental measuring device to record data throughout the entire practice period, rather than at certain intervals. Therefore, the purpose of our study was to evaluate the associations of practice day, session number, and WBGT and the incidence rates of EHIs for US collegiate athletes participating in football practice during preseason training.
METHODS
Participants
Data were collected for 4 football seasons (2004 through 2007) from colleges and universities participating in NCAA Division I or III football. Each school was placed into 1 of 6 regions based on the longitude and latitude lines and defined as Northeast, Southeast, Upper Midwest, Lower Midwest, Northwest, and Southwest. Participants were identified by position, practice type, amount of equipment worn, and type of EHI. Data for all participants during each season were entered into the data logger on a Web site developed for this study. Descriptive information, such as equipment worn, playing surface, player position, and practice type, was recorded for each EHI occurrence. A total of 60 colleges and universities began the study, with equal representation from each of the 6 regions. Over the 4 years of data collection, we recorded 114 team-seasons; institutions that did not submit complete season data or had errors in data recording in that year of data were not included in this study. The University of Georgia Institutional Review Board provided an exemption for athlete consent and approved this study.
Definitions of EHI and AE
We defined EHI according to the National Athletic Trainers' Association (NATA) position statement1 (Table 1). A reportable heat illness event was defined as one that resulted in missed participation or in evaluation by a member of the athletic medical staff. Based on the NCAA criteria, we defined a reportable AE as an individual participating in 1 team practice session.4 An AT at each participating institution was responsible for documenting all EHIs and exposures using a standardized form. To standardize data collection, an instructional packet with detailed information about data recording, instrument use, and illness and injury definitions was mailed to each participating AT. We assumed that ATs could recognize the signs and symptoms of EHIs and accurately diagnose these illnesses.
Terminology
All athletic practices were defined as either a practice day (calendar day) or practice session (when multiple practice sessions were held in a single day). Practice sessions were identified in an aggregate format through the reporting period. Practice number reflected the specific practice session of multiple practices held on the same day (double sessions).
We defined illness rate by preseason practice session number according to NCAA regulations.18 These regulations require that, during the first 5 days (eg, August 1, 2, 3) of practice, each session must be no longer than 3 hours, with helmets only on practice days 1 and 2, helmets and shells on practice days 3 and 4, and full equipment on day 5. Beginning on practice day 5, double practice sessions can start and single- and double-session days can be alternated.
Illness rate by practice day indicated that the illness rate was calculated for each practice day. Practice began on August 1 per NCAA policy. Practice days were labeled as day 1, day 2, day 3, etc.
Environmental Data
Daily environmental data were recorded using either a WBGT weather instrument or by estimated weather-station data for each participating site. The portable weather monitor (model QT-34; Quest Technologies, Oconomowoc, WI) was used to record environmental data (WBGT) daily at each participating site. It was placed adjacent to where most practices took place at each school. This weather monitor has data-logging capabilities that store environmental data on an internal memory card; we downloaded the data to a computer and transmitted them to the research team. The data-logging interval was set at 15 minutes, and data were recorded from the beginning to the end of a scheduled practice session. The QT-34 measures WBGT based on 3 environmental variables: ambient air or dry bulb temperature (DB), wet bulb temperature (WB), and globe temperature (G). The WBGT calculations use a weighted average of the 3 temperature sensors as follows19:
At schools without QT-34 units, we used observational measures of WBGT by assessing DB and relative humidity from nearby weather stations. These weather observations were obtained from the National Climatic Data Center US Global Surface Airways Hourly Observations dataset (DSI-3280).20 Next, we estimated WBGT based on the following algorithm:
where Ta represents DB in Celsius and e indicates water vapor pressure (hPa). To calculate e, we used the formula20:
If the practice occurred between the recording periods for weather-station data, the variables were averaged between the times. Estimates of WBGT based on weather-station data correlate highly with on-field measures of WBGT.21
The high and average WBGTs were recorded for each session. Of the total number of WBGT values recorded (n = 3942), 2204 (55.9%) observations used the QT-34, and 1738 (44.1%) observations used estimated numbers.
To ensure that field and weather-station measures of WBGT were equal, we randomly selected 1% (n = 1984) of all data points from the complete dataset. This subset consisted of 1143 points based on the QT-34 and 841 points based on estimated WBGT. A 1-way analysis of variance indicated no difference (F1,1982 = 1.541, P = .22) between the QT-34 (23.94°C ± 4.60°C) and estimated WBGT data (23.72°C ± 3.10°C). Based on this analysis and previous use of weather-station data,2,21,22 the estimated data were included in the analysis. We recorded the EHI rates by WBGT in 2° increments from 61.0°F (16.1°C) to 92.0°F (33.3°C) continuously throughout the practice session. The WBGT unit was stabilized before recording as directed by the manufacturer's recommendations.
Procedures
Data collection occurred from the first official day of football practice (approximately August 1) until September 30. The data were sent to a common collection site for evaluation of accuracy and data entry. Game-day data were not included in this study.
Data Cleaning
At the end of the project, all data were evaluated for accuracy and integrity. If a school submitted partial information for a season, the entire dataset for that season was excluded from the analysis. In the Southwest, only 2 schools complied with the project procedures. We did not believe this was an accurate representation of the EHI experiences for that region; therefore, all data for that region were excluded from the analysis. Sufficient data were received from the remaining 5 regions. Therefore, all analyses were completed based on data obtained from 5 regions of the country: Northeast, Southeast, Upper Midwest, Lower Midwest, and Northwest.
Statistical Analysis
We used basic descriptive statistics (mean ± SD) to describe patterns and trends among player position and academic year, WBGTs, practice day, session number, and EHI types. The EHI rates were calculated by adding the number of EHI cases and dividing by the number of AEs; only practice EHI rates were calculated. An incidence density ratio was calculated for each geographic region. We calculated 95% confidence intervals (CIs) for all illness rates (IRs). The 95% CI was used to estimate the range of the likely population examined. Given the low number of reported heat syncope (HS) occurrences, we combined these occurrences with reported HE cases to form 1 variable (HS/HE). All data were aggregated to represent the data trends for all years. We used SPSS (version 22; IBM Corporation, Armonk, NY) to analyze the statistics.
RESULTS
Exertional Heat Illness Rates
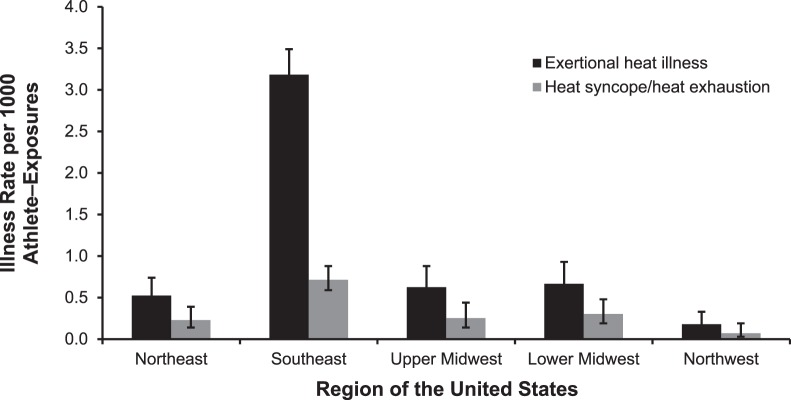
A total of 553 EHI cases and 365 810 AEs were recorded for an overall heat IR of 1.52/1000 AEs (95% CI = 1.42, 1.68). Approximately 74% (n = 407) of the reported EHI cases were exertional heat cramps (IR = 1.14/1000 AEs; 95% CI = 1.03, 1.25), and about 26% (n = 146) were a combination of exertional HS and HE (IR = 0.40/1000 AEs; 95% CI = 0.35, 0.48). No participating university reported any cases of heat stroke or hyponatremia. When the data were analyzed by region, the Northeast had 32 EHI cases (0.52/1000 AEs); the Southeast, 446 cases (3.18/1000 AEs); the Upper Midwest, 32 cases (0.62/1000 AEs); the Lower Midwest, 33 cases (0.67/1000 AEs); and the Northwest, 10 cases (0.18/1000 AEs). Furthermore, the Southeast had the highest EHI rate, whereas the Northeast, Upper Midwest, and Lower Midwest had about the same EHI rates (Figure 1). The Northwest had a lower EHI rate than all other regions. Overall, the Southeast ratio was 4.78 times higher than the Lower Midwest ratio, which was the next highest region. For the more severe EHIs (HS/HE), the Southeast ratio was 2.36 times higher than the Lower Midwest ratio (Figure 1).
Figure 1. .
Exertional heat illness rate by region of the United States.
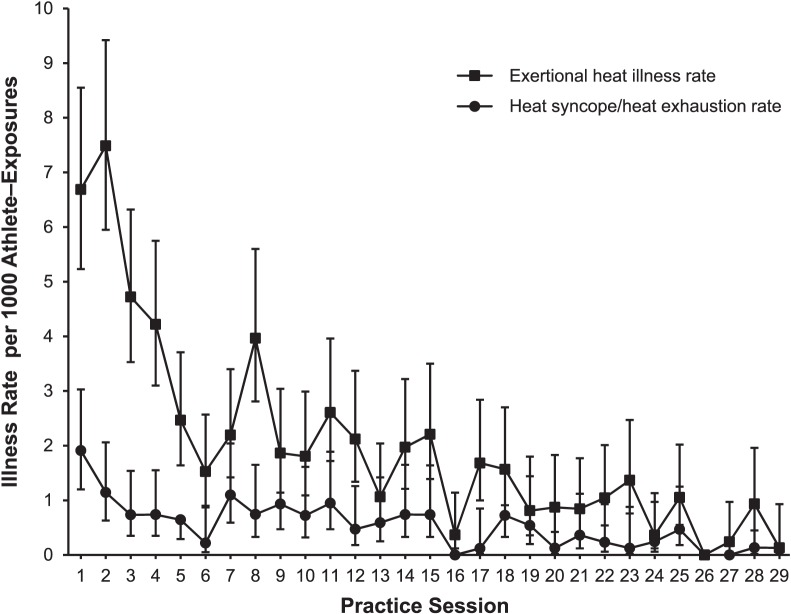
Illness Rate by Preseason Practice Session Number
As seen in Figure 2, the greatest risk of EHI occurred during the first 3 practice sessions. The data also indicated an increase in EHI occurrence during practice sessions 8 and 11. For EHI IRs that were different, the IR remained less than 1.0/1000 AEs for practice sessions 19 through 29 (Figure 2). Of the total EHI cases, 92.8% (n = 478) occurred during the first 29 practice sessions of the defined preseason period, with most EHI cases recorded in the first 15 practice sessions (Table 2).
Figure 2. .
Exertional heat illness rate by preseason practice session.
Table 2. .
Percentage of Exertional Heat Illness Cases by Preseason Practices
| Days of Practice |
Exertional Heat Illness Occurrences, No. |
% (No.) |
|
| Preseason Period |
Season |
||
| First 5 d of practice | 243 | 47.18 (115) | 43.78 (106) |
| First 10 d of practice | 340 | 66.02 (224) | 61.26 (208) |
| First 15 d of practice | 423 | 82.14 (347) | 76.22 (322) |
| Entire preseason period | 515 | 100.00 (515) | 92.79 (478) |
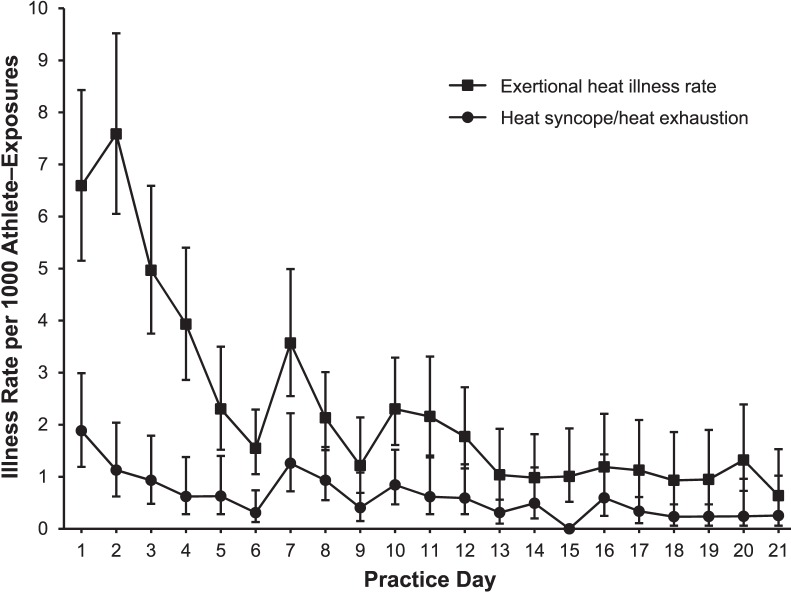
Illness Rate by Practice Day
The first 3 practice days, which represent practice sessions 1 through 3, demonstrated the greatest EHI risk (Figure 3). When double sessions were permitted on practice day 6, we noted an increase in the EHI IR on practice days 7 and 10. The EHI IR remained relatively stable beginning with practice day 14.
Figure 3. .
Exertional heat illness rate by preseason practice day.
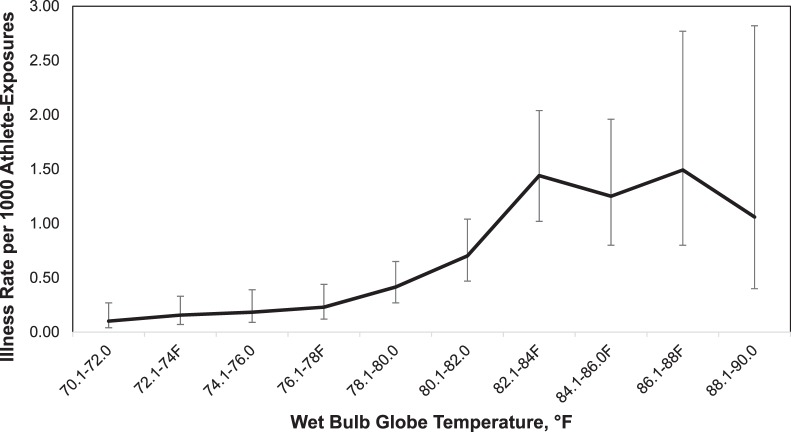
Illness Rate by WBGT
As stated, the WBGT data for HS/HE were recorded in 2° increments from 61.0°F (16.1°C) to 92.0°F (33.3°C) and plotted from 70.1°F (21.2°C) to 90.0°F (32.2°C) as seen in Figure 4. The HS/HE IR remained less than 0.23/1000 AEs (95% CI = 0.09, 0.39) when the WBGT was less than 78.0°F (25.6°C). The IR was 6 times higher (1.44/1000 AE) when a WBGT of 82.0°F (27.8°C) to 84.0°F (28.9°C; 95% CI = 1.02, 2.04) was recorded than when a WBGT of 76.0°F (24.5°C) to 78.0°F (25.6°C) was recorded.
Figure 4. .
Heat syncope/heat exhaustion rate by every 2°F of wet bulb globe temperature.
The EHIs were also categorized based on the ACSM EHI scale7 of low risk (<82.0°F [27.8°C]), moderate risk (82.1°F [27.9°C] to 86.0°F [30.0°C]), high risk (86.1°F [30.1°C] to 90.0°F [32.2°C]), and extreme risk (>90.0°F [32.2°C]), as seen in Table 3. Low- and moderate-risk categories accounted for 96.6% of the practice sessions (Table 4). More severe EHI cases of HS/HE exhibited an IR of 1.34/1000 AEs for both the moderate- and high-risk categories.
Table 3. .
American College of Sports Medicine Wet Bulb Globe Temperature Index Scale7a
| Wet Bulb Globe Temperature, °F (°C) |
Nonacclimated |
Acclimated |
| <82.0 (27.8) | Increase work-to-rest ratio. Decrease total duration of activity. | Normal activity. Monitor fluid intake of participants. |
| 82.1–86.0 (27.9–30.0) | Increase work-to-rest ratio to 1:1. Limit intense exercise and watch at-risk athletes. | Plan intense or prolonged exercise with discretion. Watch at-risk individuals. |
| 86.1–90.0 (30.1–32.2) | Cancel or stop practice and competition. | Limit intense exercise and total exposure to heat and humidity. Watch for early signs and symptoms of exertional heat illness. |
| >90.0 (32.2) | Cancel exercise. | Cancel exercise. Uncompensable heat stress exists for athletes. |
Reprinted with permission from American College of Sports Medicine, Armstrong LE, Casa DJ, et al. American College of Sports Medicine position stand: exertional heat illness during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572. Promotional and commercial use of the material in print, digital, or mobile device format is prohibited without the permission from the publisher Wolters Kluwer. Please contact healthpermissions@wolterskluwer for further information.
Table 4. .
Exertional Heat Illness Rates for Each American College of Sports Medicine Risk Category20
| Risk Category18 |
Exertional Heat Illness Type, No. |
No. of Exposures |
Overall Exertional Heat Illness Ratea |
Heat Syncope/Heat Exhaustion Exertional Heat Illness Ratea |
|||
|
Heat Cramps |
Heat Syncope |
Heat Exhaustion |
Total |
||||
| Low | 191 | 21 | 52 | 264 | 315 326 | 0.84 | 0.23 |
| Moderate | 178 | 6 | 45 | 229 | 38 067 | 6.02 | 1.34 |
| High | 32 | 4 | 10 | 46 | 10 475 | 4.39 | 1.34 |
| Extreme | 6 | 0 | 8 | 14 | 1942 | 7.21 | 4.12 |
| Total | 407 | 31 | 115 | 553 | 365 810 | 1.52 | 0.40 |
Overall exertional heat illness rate and heat syncope/heat exhaustion exertional heat illness rate are normalized per 1000 athlete-exposures.
DISCUSSION
Our goal was to evaluate EHI occurrence in a national sample of US collegiate football athletes, and we showed that the greatest risk of EHI occurred within the first 14 days of practice. We believe that the increased number of practice sessions, consecutive days of practice, intensity of practices, and WBGT levels at the start of the football season place greater demands on the physiologic systems of the athlete's body, causing a higher EHI incidence than at other times in the season.
Our data suggested that EHI rates can also be tied to the number of practice sessions held during the preseason period. Referencing Figure 3, our data indicated a spike in EHI occurrences during the initial 2 practice sessions, with a gradual decline in rates through session 6. The incidence rose again during practice session 7, which corresponds with the beginning of double-session practices as allowed by the NCAA practice policy,17 and remained elevated through session 15. Thereafter, for the EHI IRs that were different, the IRs decreased to less than 1.00/1000 AEs. However, when evaluating by practice day, the EHI IR began high and gradually declined until practice day 14. When interpreting both the practice-session and practice-day data, it appears to take 14 days for collegiate football players to become acclimated, as demonstrated by the decline in both the EHI IR and frequency of EHI occurrences. Recently, researchers4,16,23 evaluating large participant samples have also found that the occurrence of EHI increases when individuals participate in activities under adverse environmental conditions. When seeking the exact cause of an EHI, one must understand that it is the result of multiple factors. These variables may be either environmental or nonenvironmental and, therefore, require the AT to act on a variety of aspects. The NATA's position statement on EHIs1 includes recommendations to reduce these occurrences through injury-prevention techniques. We found similar indicators for this athletic population and agree with the implementation of prevention strategies to reduce the risk.
The revised ACSM EHI scale7 (Table 3) has 4 WBGT categories for the acclimatized athlete, which include suggestions for participation restrictions. Whereas this scale was developed for general use by athletes of all calibers and not specifically for football players, the WBGT categories provide useful information for the clinician. For EHI prediction, our data suggested that, when WBGT was less than 82.0°F (27.8°C), the relative risk of EHI was low (0.84/1000 AEs). However, when the WBGT was between 82.0°F (27.8°C) and 86.0°F (30.0°C), the EHI rate was 6.02/1000 AEs. We suggest that, when the WBGT is less than 82.0°F (27.8°C), normal hydration strategies are warranted and should be implemented by the medical staff for fluid replacement, rest, electrolyte balance, and body weight management.1,13 When the WBGT is greater than 82.0°F (27.8°C), we recommend that medical personnel closely monitor all participants at high risk1 (eg, those with increased body mass index, dehydration, sickle cell trait) for signs of EHI during all events. Essentially, all ATs should be on high alert for EHI occurrence and institute more frequent rest breaks and hydration opportunities during practice sessions held in these temperature extremes. Additional interventions, such as practice-length modification, equipment modification, and coach education, are valuable and can lessen EHI occurrence rates. Our study demonstrated very few cases of EHI at temperatures greater than 90.0°F (32.2°C) because teams revised practice times or practice type when WBGT reached this level. Athletic trainers and all medical personnel should limit practice sessions in this extreme environmental condition.
The ACSM,7 the Department of the Navy,15 and the NATA1 have published position statements about athletic participation in extreme environmental conditions. These position statements agree that a WBGT index is the best measure of environmental conditions and should be adopted to prevent EHI and dictate practice protocols during extreme environmental conditions. Our study supports the recommendations of the ACSM, US Department of Defense, and NATA, and we encourage the medical community to implement these guidelines.
Limitations
We relied on ATs to be knowledgeable about and able to recognize EHI and to record and report all EHI events to the project staff. We provided each AT with definitions of EHIs and requested that they review the NATA's position statement on EHIs.1 Whereas every effort was made to obtain accurate data, we recognize that EHIs could have been underreported or overreported. In addition, given that we used estimated data for a portion of the WBGT readings, some measurement error could have occurred.
Clinical Applications
We believe that ATs and all medical personnel associated with football are doing an excellent job with EHI prevention. First, no heat strokes or deaths occurred at the reporting schools. Furthermore, very few practice sessions were held when the WBGT reached 90.0°F (32.2°C) or higher. Although we cannot substantiate if any practices were canceled or moved to a different part of the day due to environmental conditions, less than 0.5% of the exposures occurred at a WBGT greater than 90.0°F (32.2°C). Additional consideration should be given to at-risk individuals, player position, practice day, and practice session at the beginning of the football season and when the WBGT reaches high levels. More practice modifications may be needed to reduce the risk of a catastrophic incident for these individuals.
No heat strokes were reported during the study period, but this type of EHI potentially can occur during the twice-daily period and the first 19 sessions of football practice. Heat stroke is one of the few medical emergencies for which ATs treat first and transport second. We strongly recommend that all ATs have a tub available for cold-water immersion and assess rectal temperature as an accurate measure of core body temperature. When a heat stroke occurs, the immediate cooling of the body via cold-water immersion rapidly lowers core body temperature and ultimately saves lives.24,25
Considering the substantial number of exertional heat cramps and HE cases, prevention of EHI requires the medical professional to institute appropriate prevention strategies1 as well as provide educational resources for those who are participating in extreme environmental conditions. Attention to hydration strategies based on an individual's sweat rate and the replacement of sodium and electrolytes through counseling on good dietary habits are sound prevention strategies that will also benefit the athlete.
CONCLUSIONS
Our study represents a 4-year data analysis of EHI rates among US collegiate football players and demonstrates that the risk of EHI increases during the initial 14 days of preseason practice. Sports medicine professionals should evaluate the effect of the environment (WBGT), practice day, and practice session when developing and implementing appropriate EHI prevention strategies.
ACKNOWLEDGMENTS
We thank the NCAA, NATA College/University Committee, and all the ATs who participated in this project.
REFERENCES
- 1. Binkley HM, Beckett J, Casa DJ, Kleiner DM, Plummer PE. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2002; 37 3: 329– 343. [PMC free article] [PubMed] [Google Scholar]
- 2. Mueller FO, Colgate B. Annual Survey of Football Injury Research 1931–2009. Chapel Hill, NC: The American Football Coaches Association, National Collegiate Athletic Association, and National Federation of State High School Associations; 2010. http://www.unc.edu/depts/nccsi/2009AnnualFootball.pdf. Accessed April 6, 2016. [Google Scholar]
- 3. Mueller FO, Colgate B. Annual Survey of Football Injury Research 1931–2010. National Center for Catastrophic Sport Injury Research Web site. http://nccsir.unc.edu/files/2014/05/2010FBAnnual.pdf. Published 2011. Accessed May 20, 2016. [Google Scholar]
- 4. Dick R, Ferrara MS, Agel J, et al. Descriptive epidemiology of collegiate men's football injuries: National Collegiate Athletic Association Injury Surveillance System, 1988–1989 through 2003–2004. J Athl Train. 2007; 42 2: 221– 233. [PMC free article] [PubMed] [Google Scholar]
- 5. Grundstein AJ, Ramseyer C, Zhao F, et al. A retrospective analysis of American football hyperthermia deaths in the United States. Int J Biometeorol. 2012; 56 1: 11– 20. [DOI] [PubMed] [Google Scholar]
- 6. Sawka MN, Wenger CB, Pandolf KB. Thermoregulatory responses to acute exercise-heat stress and heat acclimation. : Fregly MJ, Blatteis CM. Handbook of Physiology. Section 4: Environmental Physiology. New York, NY: Oxford University Press, for the American Physiological Society; 1996: 157– 185. [Google Scholar]
- 7. American College of Sports Medicine, LE Armstrong Casa DJ et al. . American College of Sports Medicine position stand: exertional heat illness during training and competition. Med Sci Sports Exerc. 2007; 39 3: 556– 572. [DOI] [PubMed] [Google Scholar]
- 8. Budd GM. Wet-bulb globe temperature (WBGT): its history and its limitations. J Sci Med Sport. 2008; 11 1: 20– 32. [DOI] [PubMed] [Google Scholar]
- 9. Kraemer WJ, Armstrong LE, Hubbard RW, et al. Responses of plasma human atrial natriuretic factor to high intensity submaximal exercise in the heat. Eur J Appl Physiol Occup Physiol. 1988; 57 4: 399– 403. [DOI] [PubMed] [Google Scholar]
- 10. Smalley B, Janke RM, Cole D. Exertional heat illness in Air Force basic military trainees. Mil Med. 2003; 168 4: 298– 303. [PubMed] [Google Scholar]
- 11. Yeargin SW, Casa DJ, Armstrong LE, et al. Heat acclimatization and hydration status of American football players during initial summer workouts. J Strength Cond Res. 2006; 20 3: 463– 470. [DOI] [PubMed] [Google Scholar]
- 12. Wenger CB. Human adaptation to hot environments. In: Pandolf KB, Burr RE. eds Medical Aspects of Harsh Environments. Vol 1. Falls Church, VA: Office of The Surgeon General, Department of the Army, United States of America; 2001: 51– 86. http://www.cs.amedd.army.mil/Portlet.aspx?ID=eebb9338-2027-46d5-a5f2-f245e2019b6c. Accessed April 6, 2016. [Google Scholar]
- 13. Kulka TJ, Kenney WL. Heat balance limits in football uniforms. Physician Sportsmed. 2002; 30 7: 463– 470. [DOI] [PubMed] [Google Scholar]
- 14. Maresh CM, VanHeest JL. Recommendations for athletes and weekend warriors. : Armstrong LE. Exertional Heat Illnesses. Champaign, IL: Human Kinetics; 2003: 197– 205. [Google Scholar]
- 15. Cleary M. Predisposing risk factors on susceptibility to exertional heat illness: clinical decision-making considerations. J Sport Rehabil. 2007; 16 3: 204– 214. [DOI] [PubMed] [Google Scholar]
- 16. Preventative medicine for ground forces. United States Navy Medicine Web site. http://www.med.navy.mil/directives/Pub/5010-9.pdf. Published 1991. Accessed May 13, 2016. [Google Scholar]
- 17. Cooper ER, Ferrara MS, Broglio SP. Exertional heat illness and environmental conditions during a single football season in the southeast. J Athl Train. 2006; 41 3: 332– 336. [PMC free article] [PubMed] [Google Scholar]
- 18. Guideline 2C: prevention of heat illness. National Collegiate Athletic Association Web site. http://www.ncaapublications.com/productdownloads/MD15.pdf. Published 2014. Accessed May 17, 2016. [Google Scholar]
- 19. Yaglou CP, Minard D. Control of heat casualties at military training centers. AMA Arch Ind Health. 1957; 16 4: 302– 316. [PubMed] [Google Scholar]
- 20. Data tools: find a station. National Centers for Environmental Information Web site. http://www.ncdc.noaa.gov/cdo-web/datatools/findstation. Accessed May 13, 2016. [Google Scholar]
- 21. Resch J, Keeler K, Brown C, Cooper ER, Ferrara MS. Relationship between weather station data and heat stress/thermal environment monitors [abstract]. J Athl Train. 2007; 42 suppl 2: S51. [Google Scholar]
- 22. Orchard JW, Powell JW. Risk of knee and ankle sprains under various weather conditions in American football. Med Sci Sports Exerc. 2003; 35 7: 1118– 1123. [DOI] [PubMed] [Google Scholar]
- 23. Carter R, 3rd, , Cheuvront SN, Williams JO, et al. Epidemiology of hospitalizations and deaths from heat illness in soldiers. Med Sci Sports Exerc. 2005; 37 8: 1338– 1334. [DOI] [PubMed] [Google Scholar]
- 24. Mazerolle SM, Lopez RM, Casa TM, Casa DJ. Heat and hydration curriculum issues: part 4 of 4. Cold water immersion. Athl Ther Today. 2009; 14 5: 12– 17. [Google Scholar]
- 25. Inter-Association Task Force on Exertional Heat Illnesses: consensus statement. National Athletic Trainers' Association Web site. http://www.nata.org/sites/default/files/inter-association-task-force-exertional-heat-illness.pdf. Accessed September 20, 2011. [Google Scholar]