Abstract
Objective:
To discuss the case of a 49-year-old man who presented to the sports medicine staff with pelvic pain of 10 years' duration consistent with pudendal neuralgia.
Background:
Testicular pain in men is often provoked by direct trauma or may indicate an oncologic process.
Differential Diagnosis:
Epididymitis, athletic pubalgia, testicular tumor, sacroiliac joint dysfunction, lumbar radiculopathy.
Treatment:
The patient responded positively to treatment and rehabilitation to restore normal mechanics to the lumbo-pelvic-hip complex. Several flare-ups since the initial treatment have been of short duration (<2 days) and less intense.
Uniqueness:
Pudendal neuralgia tends to affect females more than males due to changes in the alignment and stability of the pelvis from a combination of a shorter, wider pelvis and muscle imbalances associated with childbirth. Typically, males with testicular pain suffer from epididymitis or some type of testicular torsion, which was not the situation in this case. Compression is also a common cause of pudendal neuralgia, although it was not responsible for this patient's pain, making diagnosis and treatment complex.
Conclusions:
Many pain syndromes can be treated with removal of the original stimulus. However, recognizing the factors contributing to pelvic pain and dysfunction in males can be a challenge for the sports medicine professional. A vigilant and unassuming approach to male pelvic pain is warranted, particularly by health care providers in diverse practice settings.
Key Words: pudendal nerve, sacroiliac joint dysfunction, pelvic pain
Athletic trainers have traditionally worked with healthy, younger populations in settings ranging from high school and collegiate to professional sports. In these settings, they often provide the initial medical screening for injured and ill patients. As athletic trainers branch into nontraditional settings, such as outpatient clinics and industrial medicine, they will likely encounter patients from diverse populations who have a greater array of degenerative medical conditions and comorbidities.1
Testicular pain (orchialgia) is often associated with acute trauma; chronic orchialgia is less apparent and can be highly debilitating. A common cause of acute testicular pain is direct trauma, such as being hit or kicked. However, acute-onset pain in the absence of direct trauma is less understood and may be considered a medical emergency that requires immediate medical referral. Pain in the absence of trauma could indicate infection, referred pain, or tumor growth and cancer. Although pain rarely results in death, the underlying cause can lead to testicular atrophy, necrosis, sterility, and other associated morbidities.2 In less urgent cases, pain is frequently associated with torsion of the spermatic cord, which, if left untreated, can lead to more severe outcomes, such as necrosis.3 Other causes of testicular and pelvic discomfort in males include palpable masses presenting as a hydrocele, spermatocele, or varicocele.2 These conditions are less acute as compared with immediate pain and dysfunction, but patients must be referred for imaging to rule out neoplasms.4
An estimated 7% to 24% of the general population will develop chronic pelvic pain syndrome.5 Formerly termed abacterial prostatitis, chronic pelvic pain syndrome in males is characterized by pain in the rectum, perineum, penis, and testicles without confirmation of infection.6 Visceral pain, due to its varied referred-pain patterns, is inherently difficult to assess and treat; this is further complicated by its duration and variability.7
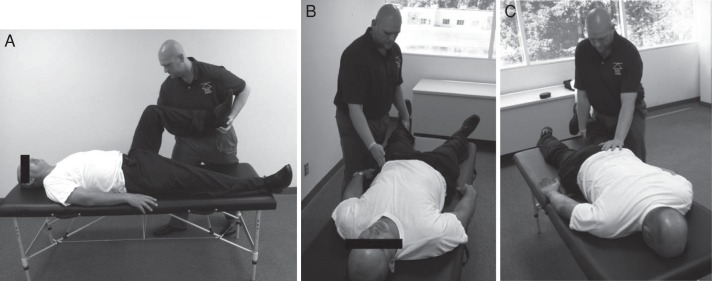
Pudendal neuralgia can be caused by compression or entrapment of the pudendal nerve, which innervates the rectum and genitalia (Figure 1). Both males and females can be diagnosed with pudendal neuralgia; however, rates are often higher in females due to a combination of altered structure and stability during and after pregnancy.5,8 Correct diagnosis commonly takes several years (average = 5.52 years).8 Pudendal nerve injury often occurs from compression of the nerve in the Alcock canal, a small opening between the obturator fascia and the obturator internus muscle that houses the pudendal vein, artery, and nerve.9 Treatments vary from prescription of anti-inflammatory medication to surgical decompression via fasciotomy.5,8
Figure 1. .
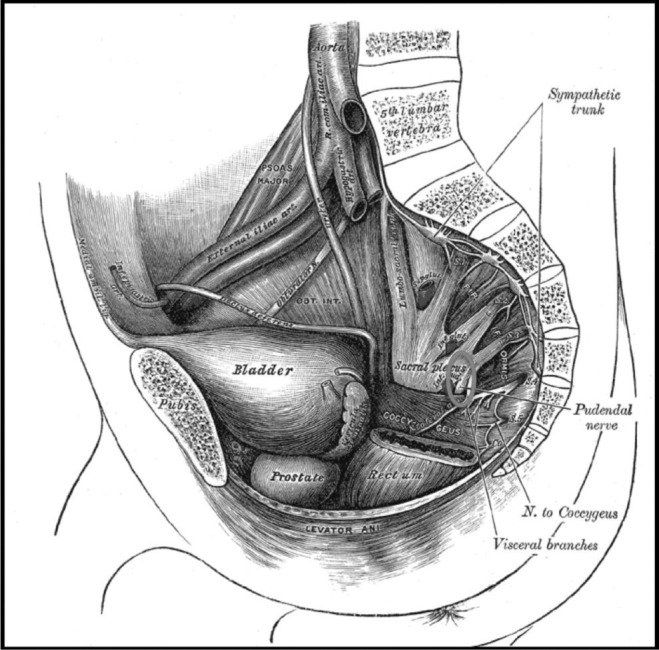
Illustration of the pudendal nerve. From Gray H, Carter HV. Gray's Anatomy. London, England: J.W. Parker Publishing; 1858.
Typically, the pudendal nerve is thought to comprise nerve roots S2−S4 (Figure 1). Although some variations exist, most of the innervation (85%) is from the S2 level.10 The pudendal nerve may be compressed at its root in the presence of sacroiliac joint dysfunction (SIJD). As the joint becomes dysfunctional, the pudendal nerve can be compressed by the osseous innominate, fascia of the obturator and iliacus muscles, or more frequently, between the sacrotuberous and sacrospinous ligaments (Figure 1).9 These possibilities may be overlooked on initial examination because individuals with SIJD often complain of lumbar spine pain and may experience radicular symptoms consistent with sciatica.
Evidence-based literature11 shows some efficacy of lumbar spine manipulation for alleviating testicular pain. In a case study,12 conservative management of the thoracolumbar spine was used to treat testicular pain. The purpose of our report is 3-fold: (1) present the case history of a 49-year-old man with diffuse testicular pain and pelvic discomfort, (2) discuss the successful management and treatment of his condition, and (3) compare this case with other conditions in the differential diagnosis.
CASE REPORT
Patient Medical History
The patient was a 49-year-old man. He reported a work history as a traveling salesman when symptoms first presented but stated he was currently employed as a machinist. The patient described the onset of “tailbone bone” pain approximately 13 years earlier (2002) while traveling in an automobile. He stated that he was positioned “on the hump” in the center of the backseat between 2 other people for about 4 hours when the pain began. The pain was intermittent but had worsened in frequency, intensity, and duration over the past several years. He characterized the pain as a “knife being stuck through the left side of the rectum” that also radiated into both testicles. Pressure at the base of his spine was exacerbated by sitting. He also noted persistent numbness across both buttocks. Pain increased with any bending or lifting activities, and he found relief by performing Kegel exercises, which caused a “popping” sensation that temporarily eased the pressure. He also reported a decrease in pain when he lay on his back with his right knee bent and his left ankle across it (ie, figure-4 position). He had been a chiropractic patient during this time, but treatment that included manual manipulation, instrument-assisted mobilization, and flexion-distraction failed to relieve the pain. A full timeline of the patient's symptoms, treatments, and progress is shown in the Table.
Table.
Summary of the Patient's Medical Timeline
| Date |
Signs and Symptoms |
Treatments |
Progression |
| May 29, 2012 | Low back pain Radicular testicular pain Tight hip musculature (adductors, gluteus maximus, iliacus, rectus femoris) |
Manual therapies Postisometric relaxation SIJ distraction METs to gluteus maximus, medial hamstrings, piriformis, psoas |
Noted improvement ↓ Neurologic symptoms ↑ Lumbo-pelvic-hip mobility, forward bending |
| June 5, 2012 | Continued pressure and numbness in buttocks SIJ had left inferior rotation, posterior upslip, right side had anterior upslip |
IASTM for gluteal muscles, prone stretching PIR to ↑ left hip flexion, extension METs to left psoas, inferior rotation Distraction to right ilium HEP to improve left hip extension |
Noted ↓ sharp pain Improved mobility |
| June 14, 2012 | Pain isolated to left SIJ Continued SIJ dysfunction with 1/4 in (0.64 cm) leg-length discrepancy |
IASTM to gluteal fascia Left ilium distraction HEP progressed to ↑ flexion, flexibility in latissimus dorsi, paraspinals, quadratus lumborum |
Pain much improved ↓ Radiating testicular pain Left hip extension still restricted but inferior rotation resolved |
| July 9, 2012 | ↑ Lower back pain due to work ↓ Left hip external rotation, flexion, rotation |
IASTM, PIR to improve motions METs to left psoas Left SIJ distraction HEP progressed to stretch left extensors, hip flexors, hip internal rotation and strengthen left psoas |
Minimal tingling Setback due to work |
| July 26, 2012 | ↑ Pain due to prolonged sitting Left-leg discrepancy back to 1/4 in (0.64 cm) Inferior, medial rotation of left ilium |
Same treatment as 7/9/12 Kinesiology taping of SIJ Continued HEP adding left hip-abductor isometrics |
Some setback No tingling |
| August 9, 2012 | Minimal pain, tingling 1/4 in (0.64 cm) Leg-length discrepancy in prone position Medial tilt, rotation of left ilium |
PIR to left hip adductors, internal rotators METs to hip abductors, external rotators Left ilium distraction |
Overall much improved Tingling accompanied by SIJ pain |
| August 29, 2012 | Transient tingling in posterior left hip with certain movements (forward flexion) Left medial tilt |
Left medial tilt corrected with METs to left hip abductors | Overall improvement Released from treatment Advised to continue HEP |
Abbreviations: HEP, home exercise program; IASTM, instrument-assisted soft tissue mobilization; METs, muscle energy techniques; PIR, postisometric relaxation; SIJ, sacroiliac joint.
Physical Evaluation
The patient was a well-nourished man, 177.8 cm tall, who weighed 74.8 kg. Postural evaluation revealed the left iliac crest and right acromioclavicular joints as superior, which corresponded with left trunk lateral flexion. He had external rotation of the hips; the left demonstrated more rotation than the right. The right hip was abducted.
Palpations revealed a functionally short left leg that was 0.75 in (1.9 cm) shorter than the right when supine and 0.5 in (1.27 cm) shorter when prone. Marked tenderness over the left sacroiliac (SI) joint was consistent with the Fortin area. The left anterior-superior iliac spine was posteriorly rotated with a medial tilt. Both the left anterior-superior and posterior-superior iliac spines demonstrated superior translations (upslips).
Diagnosis
The initial differential diagnosis included epididymitis, athletic pubalgia, testicular tumor, SIJD, and lumbar radiculopathy. No formal imaging was obtained during this time. The patient was treated with various muscle-energy techniques (METs) to help correct the SIJD. After treatment, he reported an immediate 90% improvement when he stood up from the treatment table. Based on the initial physical findings, treatment results, and consultation with the referring chiropractor, we determined the patient had pudendal neuralgia due to bilateral SIJD. Because tissue-specific impairments were identified via palpatory and mobility assessments as well as pain-provocation tests, the condition was treated as being of musculoskeletal origin. Treatment of the impairments resulted in objective improvements in both position and mobility that corresponded with the patient's reporting a decrease in symptoms. If symptoms had not improved or the index of suspicion for neoplasm was high based on the previous medical history and systems review, further diagnostic tests and referral would have been obtained. However, in this case, costs were controlled, and the patient experienced pain relief from therapy.
Treatment
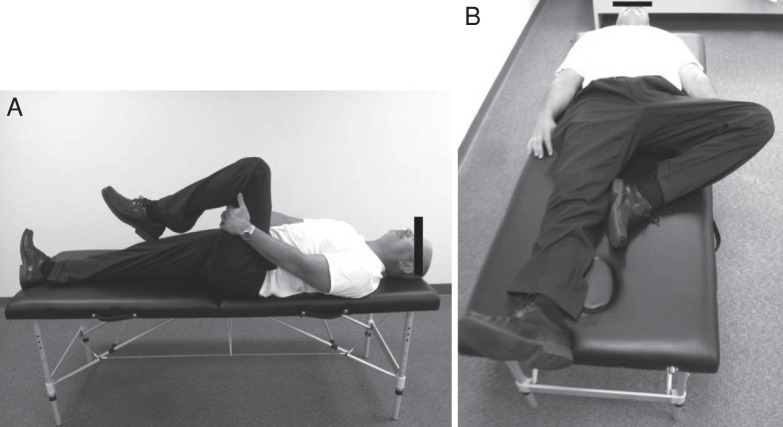
Treatment focused on restoring hip mobility and SI-joint alignment via manual-therapy techniques. Contract-relax techniques, a form of postisometric relaxation (PIR), were used to increase hip mobility and specifically flexion, extension, and abduction of the left hip. The use of PIR helps to decrease muscle guarding at points of soft tissue barriers.13−15 The contraction decreases muscle tone and initiates a hyperreactive response that allows further stretching.13,14 Joint mobilizations were used to distract the left ilia inferiorly with the patient both prone (Figure 2) and supine (Figure 3). Muscle-energy techniques were used to facilitate the left iliotibial band and hip abductors to correct the medial tilt (Figure 4).15 A summary of the clinical course and treatment is provided in the Table, and a detailed description follows.
Figure 2. .

Prone distraction.
Figure 3. .

Supine distraction.
Figure 4. .

Muscle-energy techniques for extension for the tensor fascia latae and iliotibial band.
Clinical Course
Visit 1: May 29, 2012. A chiropractor worked with the patient on alignment concerns. The patient was taking over-the-counter pain relievers but no prescription medications. He was treated with manual-therapy techniques to address hip hypomobility and SI-joint alignment. He was restricted in left hip flexion (tight gluteus maximus), extension (tight rectus femoris), abduction (tight adductors), and external rotation (tight iliacus). Postisometric relaxation was used to improve mobility in those directions (Figure 5). The left SI joint was distracted in the supine and prone positions to correct the functionally short leg. Lastly, METs were applied to the hypotonic muscles (psoas, medial hamstrings, gluteus medius, and piriformis) to activate them and restore normal positioning of the left ilium. After treatment, the patient noted a reduction in symptoms with improved lumbo-pelvic-hip mobility, most notably with forward bending.
Figure 5. .
Postisometric relaxation for A, hip flexion; B, adduction; and C, extension.
Treatment 2: June 5, 2012. The patient stated he had not had any sharp pain since the first treatment 1 week prior. He reported continued pressure with numbness in his buttocks but noted that it was not as bad as before. He did carry a wallet in his back left pocket. Palpation of the SI joint revealed left inferior rotation with posterior upslip, whereas the right presented with an anterior upslip. Instrument-assisted soft tissue mobilization was performed to the left gluteal and lumbar paraspinals with significant petechiae formation (Figure 6). He demonstrated restricted left hip flexion and extension; PIR was applied to improve these movements. To activate the left psoas and correct the inferior rotation, METs were applied. The right ilium was distracted with the patient supine, whereas the left was distracted in the prone position. He was assigned a home exercise program (HEP) consisting of lying with his left lower leg off his bed to work on improving left hip extension (Figure 7).
Figure 6. .

Petechiae formation as a result of instrument-assisted soft tissue mobilizations.
Figure 7. .

Home exercise program to improve hip extension.
Treatment 3: June 14, 2012. The patient had only “minimal pain on occasion” at this time. He also had “occasional” tingling that no longer radiated into his testicles but was isolated to the left of his coccyx. Palpation of the SI revealed anterior and posterior upslips of the left ilium, resulting in the left leg being 1/4 in (0.64 cm) short in both positions. Left hip extension continued to be restricted, but the inferior rotation had resolved. He was again treated with instrument-assisted soft tissue mobilization to the left gluteal fascia. The left ilium was distracted in both the supine and prone positions. His HEP was progressed to include seated right trunk flexion with left shoulder abduction (Figure 8) to lengthen the left latissimus dorsi, lumbar paraspinal, and quadratus lumborum muscles to prevent further upslips.
Figure 8. .
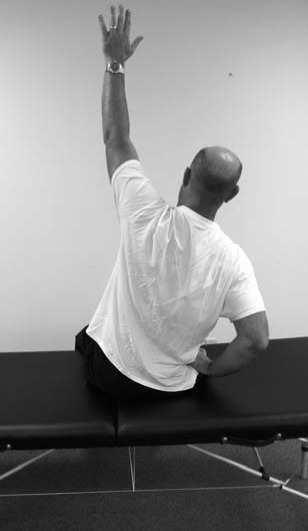
Home exercise program: seated right trunk flexion with left shoulder abduction to lengthen the left latissimus dorsi, lumbar paraspinals, and quadratus lumborum.
Treatment 4: July 9, 2012. The patient presented with an exacerbation of left low back pain after being bent over sandblasting at work for 2 hours. He had “very occasional tingling that is there and gone,” which seemed to be movement specific. He demonstrated a decrease in left hip external rotation, flexion, and rotation. Instrument-assisted soft tissue mobilization and PIR were used to improve these motions along with METs to facilitate the left psoas. The left SI joint was again distracted in the prone position. His HEP was progressed to include supine stretching of the left hip flexors, extensors, and hip internal rotators (Figure 9). He was also instructed in a strengthening technique for the psoas in the supine position (Figure 10).
Figure 9. .
Home exercise program: supine stretching of the left hip: A, internal rotators, and B, flexors and extensors.
Figure 10. .

Home exercise program: strengthening technique for the psoas in the supine position.
Treatment 5: July 26, 2012. The patient reported tingling only with sneezing or coughing until 2 days earlier, when he sat in class for more than 5 hours. This led to an initial increase in pain that he rated as moderate, but it had lessened to minimal by the time of the appointment. His left leg was again 1/4 in (0.64 cm) short in the supine and prone positions with inferior and medial rotations of the left ilium. The same treatment given on July 9, 2012, was applied to correct the left ilium. Kinesiology taping (4 in [10–16 cm] I-strip; RockTape USA, Campbell, CA) was then applied horizontally across the SI joints to simulate the use of an SI belt (Figure 11). He was instructed to continue with the previously prescribed HEP and add left hip-abduction isometric exercises.
Figure 11. .
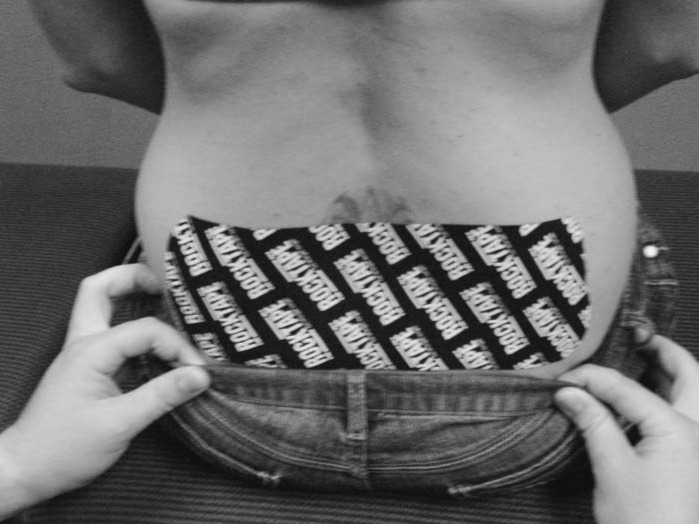
Kinesiology taping to simulate the use of a sacroiliac belt.
Treatment 6: August 9, 2012. The patient felt he was much improved overall, with tingling present “every couple of days.” He had begun noticing that, when the tingling was present, he also had “twinging” in the area of his left SI joint. Evaluation revealed no leg-length discrepancy in the supine position but 1/4 in (0.64 cm) in the prone position. He had also developed a medial tilt and rotation of the left ilium. To lengthen the left hip adductors and internal rotators, PIR was applied; to facilitate the hip abductors and external rotators, METs were applied. The left ilium was again distracted in the prone position.
Treatment 7: August 29, 2012. The patient reported overall improvement in symptoms. His primary complaint was a transient tingling in the back of his left hip that occurred every few days. He had identified the triggering factor: bending forward into a vat at work, a task that he did not perform on a regular basis. Palpation of the SI joints revealed a left medial tilt that corrected with METs to the left hip abductors. At this time, he was released to continue the previously prescribed HEP.
Deviation From Expected
Typically, testicular pain is caused by epididymitis or torsion.3,7 However, this case demonstrates that testicular pain can also be due to neural tensioning of the pudendal nerve. This can occur via compression by the sacrotuberous or sacrospinous (or both) ligaments, pelvic musculature, or innominate bones of the pelvic region. Often, individuals with pelvic floor dysfunction are prescribed Kegel strengthening exercises, but these would have exacerbated our patient's symptoms because his left pelvic floor was overly tight due to the shortened position created by altered left ilium alignment, primarily the superior translations or upslips. With sufficient compression, vascular flow through the internal pudendal artery may also be altered, which could lead to testicular necrosis. Last, despite the complications of pudendal neuralgia, the patient reported no instances of sexual dysfunction.
CONCLUSIONS
Athletic trainers work in a variety of health care settings and are likely to encounter diverse populations. Often, clinicians treat the site of a patient's symptomatic complaints without uncovering the underlying cause, as in this case. If treatment does not resolve the superficial symptoms, the pain is likely radicular. Because we engage with a diverse range of patients, we must be aware that symptoms can present in diverse ways and selectively use tests and techniques to rule in and rule out causes, particularly as the costs of diagnostic testing increase. When treating a patient with testicular pain, the members of the medical team must communicate effectively so as not to miss either a potentially deadly condition (eg, testicular cancer) or the more benign causes of radicular pelvic and testicular pain in men (eg, hydrocele or varicocele). In our patient, a comprehensive review of all systems was not indicated as he had no obvious red flags based on the chronicity of the condition. Additionally, 10 to 15 minutes of palliative and corrective interventions applied after the initial evaluation resulted in a 90% decrease in symptoms. No change in symptoms would have indicated a possible organ or organ system problem, and we would have made the appropriate medical referral. This case illustrates the importance of identifying and treating tissue-specific impairments and the associated clinical decision-making process. Challenging one's clinical paradigm and using various rehabilitation, exercise, and mobilization techniques may allow for better identification, management, treatment, and follow-up care.
REFERENCES
- 1. Mensch J, Mitchell M. Choosing a career in athletic training: exploring the perceptions of potential recruits. J Athl Train. 2008; 43 1: 70– 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Liguori G, Bucci S, Zordani A, et al. Role of US in acute scrotal pain. World J Urol. 2011; 29 5: 639– 643. [DOI] [PubMed] [Google Scholar]
- 3. Mongiat-Artus P. Torsion of the spermatic cord and testicular annexes. Ann Urol (Paris). 2004; 38 1: 25– 34. [PubMed] [Google Scholar]
- 4. Holland JM, Feldman JL, Gilbert HC. Phantom orchalgia. J Urol. 1994; 152 6 pt 2: 2291– 2293. [DOI] [PubMed] [Google Scholar]
- 5. Chiarioni G, Asteria C, Whitehead W. Chronic proctalgia and chronic pelvic pain syndromes: new etiologic insights and treatment options. World J Gastroenterol. 2011; 17 40: 4447– 4455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schaeffer A. Clinical practice. Chronic prostatitis and the chronic pelvic pain syndrome. N Engl J Med. 2006; 355 16: 1690– 1698. [DOI] [PubMed] [Google Scholar]
- 7. Baranowski A, Mallinson C, Johnson N. A review of urogenital pain. Pain Rev. 1999; 6 1: 53– 84. [Google Scholar]
- 8. Vancaillie T, Eggermont J, Armstrong G, Jarvis S, Liu J, Beg N. Response to pudendal nerve block in women with pudendal neuralgia. Pain Med. 2012; 13 4: 596– 603. [DOI] [PubMed] [Google Scholar]
- 9. Loukas M, Louis R, Tubbs R, Wartmann C, Colborn G. Intra-abdominal laparoscopic pudendal canal decompression—a feasibility study. Surg Endosc. 2008; 22 6: 1525– 1532. [DOI] [PubMed] [Google Scholar]
- 10. Matejčík V. Surgical location and anatomical variations of pudendal nerve. ANZ J Surg. 2012; 82 12: 935– 938. [DOI] [PubMed] [Google Scholar]
- 11. Rowell R, Rylander S. Low-back pain, leg pain, and chronic idiopathic testicular pain treated with chiropractic care. J Altern Complement Med. 2012; 18 4: 420– 422. [DOI] [PubMed] [Google Scholar]
- 12. Doubleday KL, Kulig K, Landel R. Treatment of testicular pain using conservative management of the thoracolumbar spine: a case report. Arch Phys Med Rehabil. 2003; 84 12: 1903– 1905. [DOI] [PubMed] [Google Scholar]
- 13. Smith M, Fryer G. A comparison of two muscle energy techniques for increasing flexibility of the hamstring muscle group. J Bodyw Mov Ther. 2008; 12 4: 312– 317. [DOI] [PubMed] [Google Scholar]
- 14. Mehdikhani R, Okhovatian F. Immediate effect of muscle energy technique on latent trigger point of upper trapezius muscle. Clin Chiropractic. 2012; 15 3−4: 112– 120. [Google Scholar]
- 15. Farquharson C. MET versus PNF: what, when and how? SportEX Dynamics. 2010; 25: 12– 16. [Google Scholar]