Abstract
Purpose
To report a single case of macular hole opening, spontaneous closure, and reopening in the three month period after pars plana vitrectomy for rhegmatogenous retinal detachment
Methods
Case report
Patient
A 59-year-old man with a macula-sparing rhegmatogenous retinal detachment who underwent uncomplicated pars plana vitrectomy with gas tamponade
Results
The patient developed a full-thickness macular hole two months post-operatively. The hole was noted to spontaneously close three months post-operatively, but then reopened four months post-operatively and required repeat pars plana vitrectomy and inner limiting membrane peel for definitive closure. The rapidity with which the macular hole developed after pars plana vitrectomy for macula-sparing rhegmatogenous retinal detachment and its dynamic behavior have not been previously reported.
Conclusions
Full-thickness macular holes may rarely develop rapidly, spontaneous close, and reopen after pars plana vitrectomy for rhegmatogenous retinal detachment, even in macula-sparing cases.
Keywords: Full thickness macular hole, pars plana vitrectomy, retinal detachment, spontaneous closure, reopening
Introduction
Full thickness macular holes (FTMH) have been reported to occur in less than 1% of patients after repair of rhegmatogenous retinal detachment (RRD).1,2 The majority have occurred after macula-involving RRD repair with scleral buckling or pneumatic retinopexy, although there are isolated cases occurring after pars plana vitrectomy (PPV).1–7 Only one case of FTMH after PPV for macula-sparing RRD has been previously described with FTMH developing 18 months after the initial surgery.5 In the literature there is also only one case of FTMH undergoing spontaneous closure and re-opening in a vitrectomized eye.8 Once again, the development of the macular hole was delayed by 7 years, the hole closed in 4 months and re-opened in 1 year. Our case is unique due to rapidity of the MH development, closure, and re-opening.
Case Report
A 59-year-old man presented with macula-sparing superior single break RRD in his right eye and best-corrected visual acuity (BCVA) of 20/30. His past ocular history included myopia and uncomplicated cataract extraction, Nd:YAG posterior capsulotomy, and laser retinopexy for retinal tear in the right eye. The left eye was pseudophakic with BCVA of 20/25.
The patient underwent uneventful PPV to the right eye with confirmation of posterior vitreous detachment, fluid-air exchange, endolaser, and instillation of 16% octafluoropropane (C3F8) gas tamponade. Post-operatively the retina remained attached and by one month post-operatively the patient’s BCVA was 20/30 in the right eye with no report of metamorphopsia or aniseikonia. The patient returned two months post-operatively noting deterioration of vision. BCVA was 20/60 with the new finding on dilated fundoscopic examination and optical coherence tomography (OCT) of a FTMH (Figure 1a). The patient was observed and returned one month later (three months post-operatively) with noted improvement in his vision and BCVA of 20/30 in the right eye. OCT demonstrated resolution of the FTMH with a small amount of residual subretinal fluid (Figure 1b). At five months post-operatively his BCVA deteriorated to 20/70 and the hole had reopened (Figure 1c). After a brief period of observation, the patient underwent PPV with inner limiting membrane peeling six months after the original RRD repair. The histopathological analysis of the peeled membrane revealed a periodic acid–Schiff positive inner limiting membrane with fibrocellular tissue present along one margin. Seven months after the original surgery the hole was closed with BCVA of 20/60 (Figure 1d).
Figure 1.
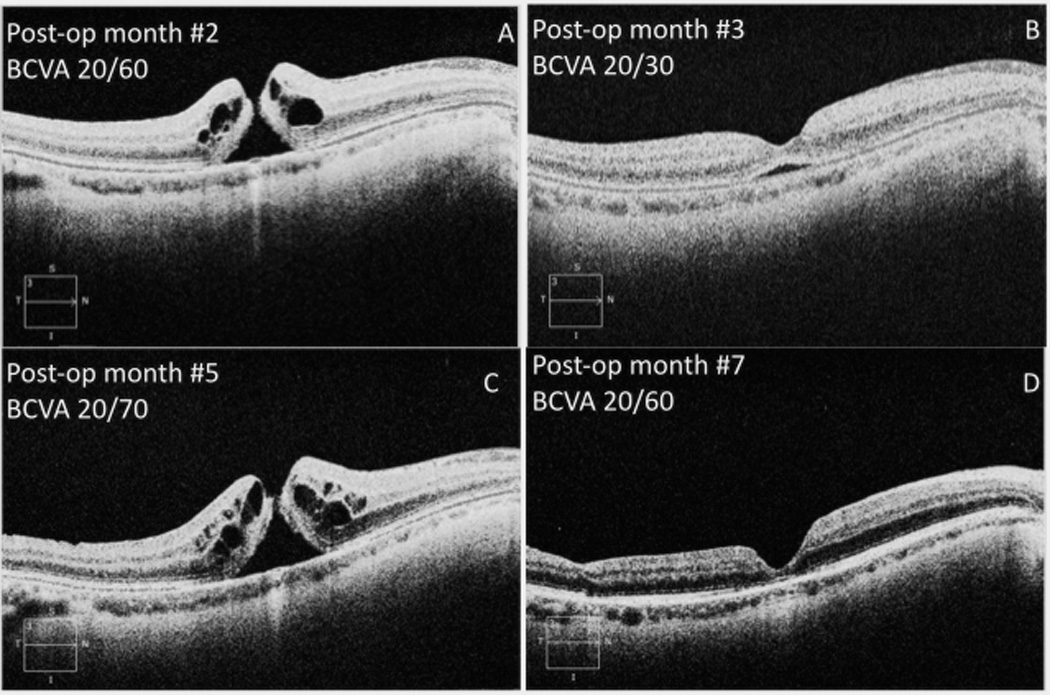
A. Right eye spectral-domain optical coherence tomography two months after pars plana vitrectomy demonstrating full-thickness macular hole (Cirrus™ HD-OCT; Carl Zeiss Meditec, Inc., USA)
B. Right eye spectral-domain optical coherence tomography three months after pars plana vitrectomy demonstrating spontaneous closure of full-thickness macular hole with small residual subretinal fluid (Cirrus™ HD-OCT; Carl Zeiss Meditec, Inc., USA)
C. Right eye spectral-domain optical coherence tomography five months after pars plana vitrectomy demonstrating reopening of the full-thickness macular hole (CirrusTM HD-OCT; Carl Zeiss Meditec, Inc., USA)
D. Right eye spectral-domain optical coherence tomography seven months after original pars plana vitrectomy demonstrating closure of full-thickness macular hole after PPV and inner limiting membrane peel (Cirrus™ HD-OCT; Carl Zeiss Meditec, Inc., USA)
Discussion
While the exact pathogenesis of FTMH is not defined, it is believed that vitreomacular traction plays a key role along with inner retinal layer degeneration at the central fovea.9
Less than 1% of patients develop MH after an RRD repair. The majority of these cases undergo repair with scleral buckle or pneumatic retinopexy and are thus not vitrectomized.1–7 In the rare cases of MH formation after pars plana vitrectomy for RRD repair, the majority of patients had macula-involving RRDs. In contrast, our patient had a macula-sparing RRD. The only previously described case of macula-sparing RRD developed FTMH 18 months after the initial surgery.5 Our patient developed FTMH 2 months post-operatively.
Spontaneous closure of MHs in non-vitrectomized eyes is well described; Sugiyama et al reported a spontaneous closure rate of 3.5% for eyes with full-thickness MHs prior to planned PPV repair.10 There have been fewer cases of spontaneous closure observed in vitrectomized eyes, with the original reason for vitrectomy including MH, vitreous hemorrhage, central retinal vein occlusion, and macula-involving RRD.6,7,11,12 Once again, in none of the previous reports did the FTMH re-open as fast as in our patient.
The timing of our patient’s pathology relative to the PPV surgery reinforces the notion that surface changes at the fovea after induction of a posterior vitreous detachment continue post-operatively. There are several hypotheses regarding how FTMH form in vitrectomized eyes. Progressive epiretinal membrane formation may cause new traction, and the fibrocellular tissue seen on histopathology in this case may represent early membrane formation. Cystoid macular edema might be an inciting factor in formation of the macular hole, although our patient had no evidence of post-operative edema precipitating the FTMH. Also, residual cortical vitreous might provide vitreofoveal traction. In previously detached macula, the retinal tissue is already compromised by hypoxia and a deficiency of nutrients provided by the retinal pigment epithelium.7 Remodeling of the inner retinal surface after induction of a PVD appears to be a dynamic process not necessarily leading unidirectionally towards MH closure.8
In conclusion, FTMH may rarely develop rapidly, spontaneous close, and reopen after PPV for RRD, even in macula-sparing cases. Multiple mechanisms might play a role, and initial observation of post-vitrectomy FTMH is warranted given the possibility of spontaneous closure.
Summary Statement.
A patient developed a full-thickness macular hole early post-operatively after pars plana vitrectomy for macula-sparing retinal detachment. The hole was noted to spontaneously close and reopen over the course of weeks.
Acknowledgments
This research was funded in part by an unrestricted grant from Research to Prevent Blindness Inc., New York, NY, USA and the National Institutes of Health NEI Center Grant P30 EY014801. We have no further acknowledgements for other contributors to this paper.
Footnotes
We have no financial and/or proprietary conflicts of interest.
This manuscript has not been previously presented at an academic meeting
References
- 1.Brown GC. Macular hole following rhegmatogenous retinal detachment repair. Arch Ophthalmol. 1988;106:765–766. doi: 10.1001/archopht.1988.01060130835034. [DOI] [PubMed] [Google Scholar]
- 2.Moshfeghi AA, Salam GA, Deramo VA, et al. Management of macular holes that develop after retinal detachment repair. Am J Ophthalmol. 2003;136(5):895–899. doi: 10.1016/s0002-9394(03)00572-5. [DOI] [PubMed] [Google Scholar]
- 3.Smiddy WE. Atypical presentations of macular holes. Arch Ophthalmol. 1993 May;111(5):626–631. doi: 10.1001/archopht.1993.01090050060029. [DOI] [PubMed] [Google Scholar]
- 4.Lipham WJ, Smiddy WE. Idiopathic macular hole following vitrectomy: implications for pathogenesis. Ophthalmic Surg Lasers. 1997;28(8):633–639. [PubMed] [Google Scholar]
- 5.Benzerroug M, Genevois O, Siahmed K, et al. Results of surgery on macular holes that develop after rhegmatogenous retinal detachment. Br J Ophthalmol. 2008;92(2):217–219. doi: 10.1136/bjo.2007.122796. [DOI] [PubMed] [Google Scholar]
- 6.Tsilimbaris MK, Gotzaridis S, Charisis SK, Kymionis G, Christodoulakis EV. Spontaneous closure of macular holes developed after pars plana vitrectomy. Semin Ophthalmol. 2007;22(1):39–42. doi: 10.1080/08820530601182576. [DOI] [PubMed] [Google Scholar]
- 7.Sabani I, Pournaras JA, Wolfensberger TJ. Spontaneous closure of macular hole following rhegmatogenous macula-off retinal detachment. Klin Monbl Augenheilkd. 2010;227(4):336–337. doi: 10.1055/s-0029-1245216. [DOI] [PubMed] [Google Scholar]
- 8.Lo WR, Hubbard GB. Macular hole formation, spontaneous closure, and recurrence in a previously vitrectomized eye. Am J Ophthalmol. 2006;141(5):962–964. doi: 10.1016/j.ajo.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 9.Smiddy WE, Flynn HW., Jr Pathogenesis of macular holes and therapeutic implications. Am J Ophthalmol. 2004;137(3):525–537. doi: 10.1016/j.ajo.2003.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Sugiyama A, Imasawa M, Chiba T, Iijima H. Reappraisal of spontaneous closure rate of idiopathic full-thickness macular holes. Open Ophthalmol J. 2012;6:73–74. doi: 10.2174/1874364101206010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaikh S, Garretson B. Spontaneous closure of a recurrent macular hole following vitrectomy corroborated by optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2003;34(2):172–174. [PubMed] [Google Scholar]
- 12.Shukla D, Rajendran A, Kim R. Macular hole formation and spontaneous closure after vitrectomy for central retinal vein occlusion. Graefes Arch Clin Exp Ophthalmol. 2006;244(10):1350–1352. doi: 10.1007/s00417-006-0258-x. [DOI] [PubMed] [Google Scholar]


