Abstract
Purpose
In radiotherapy treatment planning, dose homogeneity inside the target volume plays a significant role in the final treatment outcome. Especially in brachytherapy where there is a steep dose gradient in the dose distribution inside the target volume, comparing the plans based on the dose homogeneity helps in assessing the high dose volume inside the final treatment plan. In brachytherapy, the dose inhomogeneity inside the target volume depends on many factors such as the type of sources, placement of these radioactive sources, distance between the applicators/implant tubes, dwell time of the source, etc. In this study, a simple index, the dose volume uniformity index (DVUI), has been proposed to study the dose homogeneity inside the target volume. This index gives the total dose volume inhomogeneity inside a given prescription isoline.
Material and methods
To demonstrate the proposed DVUI in this study, a single plane implant (breast: 6 catheters), a double plane implant (breast: 9 catheters) and a tongue implant (5 catheters) were selected. The catheters were reconstructed from the CT image datasets in the Plato treatment planning system. The doses for the single, double and tongue implants were prescribed to the reference dose rate as per the Paris technique. DVUI was computed from the cumulative dose volume histogram.
Results
For a volume receiving a uniform dose inside the prescription isoline, the DVUI is 1. Any value of DVUI > 1 shows the presence of a relatively high dose volume inside the prescription isoline. In addition to the concept of DVUI, a simple conformality index, the dose volume conformality index (DVCI), has also been proposed in this study based on the DVUI.
Conclusion
The DVUI and the proposed DVCI in this study provide an easy way of comparing the rival plans in brachytherapy.
Keywords: brachytherapy, dose volume histogram, dose volume uniformity index, conformality index
Introduction
In radiotherapy treatment planning, dose homogeneity inside the target volume poses a serious problem both in external beam as well as in brachytherapy [1, 2]. In contrast to external beam radiotherapy, brachytherapy implants provide great dose conformity with significant dose inhomogeneity inside the treatment volume. The dose inhomogeneity inside the target volume depends on many factors such as the type of sources, placement of these radioactive sources, distance between the applicators/ implant tubes, dwell time of the source, etc. Several methods have been developed to assess the dose inhomogeneity inside the target volume and the dose coverage.
Brachytherapy plan evaluation is performed either qualitatively or quantitatively. The qualitative evaluation of the brachytherapy plan is usually carried out by visualizing the dose distribution in each and every slice of the CT. For quantitative evaluation several indices and ratios have been defined by various authors. Some of the indices routinely used for plan evaluation are coverage index [3], external volume index [3], overdose volume index (ODI) [3], dose homogeneity index (DHI) [4], dose non-uniformity ratio (DNR) [5], etc. Besides these indices and ratios, the rival plans are also analysed with a dose volume histogram such as the cumulative dose volume histogram (cDVH), the differential dose volume histogram (dDVH) and the natural dose volume histogram (nDVH) [6].
In brachytherapy, besides assessing the hyperdose sleeve, it is also advisable to assess the total dose inhomogeneity inside the target volume. The hyperdose sleeve is the volume receiving a dose equal to or greater than 200% of the reference dose. Most of the current indices which quantify the inhomogeneity inside the treatment volume are based on either 1.5 or 2.0 times that of the reference dose. But there are high dose volumes beyond the hyperdose sleeve and in between the hyperdose sleeve and the reference dose. None of the above indices or the natural dose volume histograms evaluates the complete inhomogeneity inside the treatment volume quantitatively.
For complete plan evaluation, taking into account the complete inhomogeneity inside the reference isoline will help in assessing the implant. Hence, this paper describes simple indices that take into account the complete inhomogeneity inside the reference isoline for evaluating the rival plans.
Material and methods
Three different cases – a single plane implant (breast: 6 catheters), a double plane implant (breast: 9 catheters) and a tongue implant (double plane: 5 catheters) were selected to demonstrate the newly proposed indices in this study. All the patients underwent CT scanning in a Philips wide bore Brilliance CT scanner and digital radiographic images were also obtained on a Simulator-CT (Simulix HP, Nucletron BV). The catheters were reconstructed from the CT image datasets in the Plato Sunrise™ treatment planning system (Nucletron BV™). The doses for the single, double and tongue implants were prescribed to the reference dose rate as per the Paris technique. The DHI, ODI and DNR were computed from the following relations: DHI = (Vref – V1.5ref)/Vref; ODI = V2ref/Vref; DNR = V1.5ref/Vref. Similarly, for PTV volumes, the DHI, ODI, DNR and coverage index were computed from the following relations: DHI = (PTVref – PTV1.5ref)/ PTVref; ODI = PTV2ref/PTVVref; DNR = PTV1.5ref/PTVref; coverage index = PTVref/TV.
The dose volume uniformity index (DVUI) proposed in this study is defined as follows.
Volume (Dosei) is the volume receiving a given dose i.
Vpresc is the volume of the prescription isoline.
PD is the prescription dose.
This index gives an idea of the total dose volume inhomogeneity inside a given prescription isodose. For a volume receiving a uniform dose inside the prescription isoline, DVUI is 1. Any value of DVUI above 1 shows the presence of a high dose volume inside the prescription isoline. If no target volume is defined for plan evaluation, then equation (1) can be used for assessing the dose volume homogeneity for the implant.
A generalized equation for comparing two plans with the DVUI apart from the absolute value of DVUI defined from Eq. (1) for a plan is to compare with the relative distribution of DVUI by modifying equation (1) as follows.
where j is the dose.
With no such tools available in the current planning system, a simple and easy way of analysing the plan with the DVUI is to obtain the product of isodose volumes in between the dose values with the dose range values and incorporate those values in Eq. (1). For example, the volumes for the dose ranges greater than the prescription doses in steps of 50 cGy (dose bins) up to the maximum dose can be easily obtained from the cumulative dose volume histogram generated from the treatment plan. These values can be incorporated in equation (1) for computation of the DVUI.
The conformity index in radiotherapy is a complementary tool for scoring a treatment plan over its rival plans for a given patient. Several indices have been introduced for the quantitative evaluation of the conformality of the treatment plan, e.g., conformation number [7], radiation conformity index [8], conformal index (COIN) [9], and conformality index [10]. COIN takes into account the coverage of the planning target volume (PTV) and dose outside the PTV and it is defined as COIN = c1 * c2, where c1 = PTVref/VPTV and c2 = PTVref/Vref.
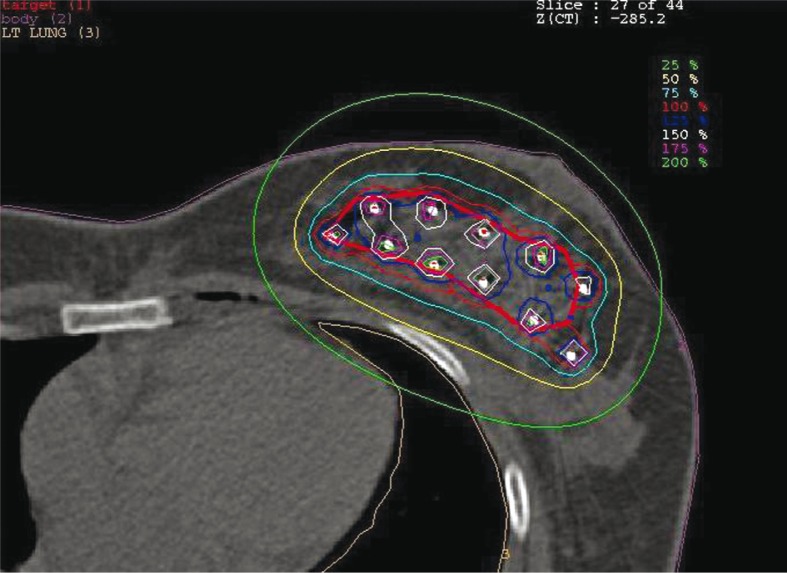
One of the drawbacks of the conformality index defined so far is that it does not take into account the complete inhomogeneity inside the target volume. Hence, a simple conformality index, the dose volume conformality index (DVCI), based on the DVUI, has been defined in this study. To demonstrate this index, a double plane breast implant with 9 catheters as shown in Fig. 1 was selected. The target volume was contoured and two plans employing geometric optimization and graphical optimization were generated. A generalized form of conformality index (CIGeneralized) [11], which is the inverse of the CI introduced by Lomax et al. [10], can be derived from the ratio of the volume of the reference isoline (Vref) to the volume of the PTV receiving the prescription dose (PTVref). The DVCI is obtained by multiplying the CIGeneralized with the respective DVUI as shown below.
Fig. 1.
Isodose distribution of a double plane breast implant. Thick red line shows the target
where:
Vref – volume receiving a dose greater than or equal to the reference dose,
PTVref – volume of the PTV receiving a dose greater than or equal to the reference dose.
DVUI(Target), the DVUI for the target volume, is defined as below.
i starts with the dose value equal to the prescription dose.
Target volume (Dosei) is the target volume receiving a given dose i.
VTarget is the volume of the target.
PD is the prescription dose.
Results
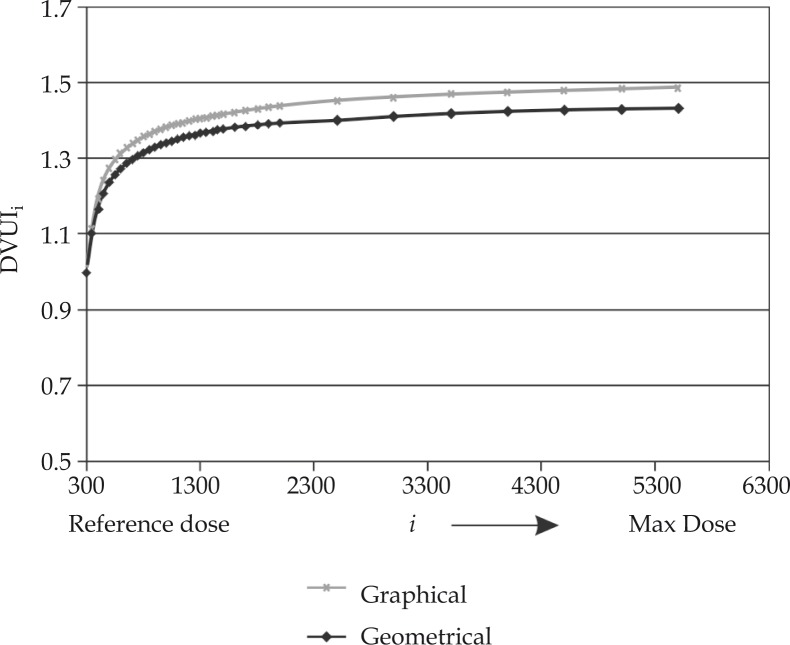
Table 1 shows the comparison of dosimetric parameters between the Paris and the geometric optimization based plans for the single plane breast and tongue implant. The DVUI for the single plane breast implant based on Paris and geometrically optimized plans are 1.49 and 1.55 respectively. Similarly for the tongue implant it is 1.55 and 1.64 for the Paris and geometrically based plans. Figure 1 shows the isodose distribution of a double plane breast implant. Figure 2 shows the comparison of DVUIi between the graphically optimized and the geometrically optimized plans for a double plane implant. Table 2 shows the comparison of dosimetric parameters between graphically and geometrically optimized plans for a double plane breast implant. The values of DVCI for the graphically and geometrically optimized plans were 1.81 and 1.76 respectively, which is less than the generalized CI. Another important thing that can be observed from the table is that the DVUI for the target is higher than the implant, which shows the presence of dose volume closer to the prescription isoline lying outside the target. In the situation where the DVUI for the target is less than the implant, then one can observe the presence of a high dose volume outside the target. The ideal DVCI value for an implant is 1.
Table 1.
Comparison of dosimetric parameters between Paris and geometric optimization based plans for single plane breast and tongue implant
| Single plane breast implant | ||
|---|---|---|
| Paris system | Geometric optimization | |
| DVUI | 1.49 | 1.55 |
| DHI | 0.68 | 0.67 |
| ODI | 0.14 | 0.14 |
| DNR | 0.32 | 0.33 |
| Base of tongue implant | ||
| Paris system | Geometric optimization | |
| DVUI | 1.55 | 1.64 |
| DHI | 0.58 | 0.60 |
| ODI | 0.17 | 0.17 |
| DNR | 0.42 | 0.40 |
Fig. 2.
Comparison of DVUIi between the graphically optimized and the geometrically optimized plans for a double plane implant
Table 2.
Comparison of dosimetric parameters between graphically and geometrically optimized plans for double plane breast implant
| Breast implant (double plane) | ||
|---|---|---|
| Graphical optimization | Geometric optimization | |
| DVUI (implant) | 1.49 | 1.43 |
| DVUI (target) | 1.55 | 1.44 |
| DVCI | 1.81 | 1.76 |
| CI (generalized) | 1.88 | 1.77 |
| Coverage index | 0.92 | 0.77 |
| DHI | 0.64 | 0.74 |
| ODI | 0.12 | 0.1 |
| DNR | 0.36 | 0.26 |
| COIN | 0.49 | 0.44 |
Discussion
In brachytherapy, the dose is prescribed to an isodose encircling the tumour volume where the dose distribution is very heterogeneous. The inhomogeneity is minimal at a distance from the radioactive sources, but much higher doses and dose rates are delivered in their immediate vicinity. The average dose given to the target volume is therefore always higher than the prescribed dose, prescribed at the periphery of the implant. Hence, it is advisable to quantify the total inhomogeneity inside the prescription isoline. Moderately high-dose regions may enhance the likelihood of cure in brachytherapy but in the presence of critical structures the high regions may lead to normal tissue complications and there are studies showing that the reduction of high dose regions decreases the likelihood of normal tissue toxicity [12–14]. Melzner et al. have shown in their study of 210 patients treated with PDR brachytherapy for head and neck tumours that there is a significant influence of high dose and peak dose on the development of osteoradionecrosis [12]. Wallner et al. have demonstrated in their study that high dose regions do not appear to affect control rates as long as > 90% of the prostate is covered by the prescription dose [13]. These studies clearly indicate the importance of reducing the high dose regions and stress the need to evaluate the plan based on dose inhomogeneity. Wust et al. have shown that high dose regions in the prostate and large heterogeneities in the post-implantation analysis correlated with the urethral toxicities for prostate brachytherapy. They concluded that more homogeneous dose distribution is required to lower the toxicity [14]. Cormack et al. have shown that non-centred source dwell positions led to an increase in the volume of high dose regions, corresponding to the toxicity with partial breast irradiation [15]. Several studies have shown that improvement in the dose homogeneity index and reduction of high dose regions result in optimized local control and reduction in the risk of complications, especially in accelerated partial breast brachytherapy [16, 17].
The formalism described in this study gives the relative amount of inhomogeneity inside the prescription isoline. DVUI can be used alone for comparing the rival plans based on the inhomogeneity when no target volume is defined in cases where radiographs are used for treatment planning from equation 1. It can be observed from Table 1 that as compared to the DHI, ODI and DNR the concept of DVUI gives a better estimation of the relative dose inhomogeneity inside the reference isoline. We are gradually moving from a simple radiograph-based brachytherapy procedure where the tumour volume and critical structure are not clearly demarcated to sophisticated three-dimensional treatment planning where the treatment delivery is based on the volume-based dosimetric plan evaluation. When CT-based or MRI-based planning is performed, in addition to DVUI, DVCI can be used to evaluate the treatment plans. The conformality index defined in this article depends on the dose volume uniformity index and it is a comprehensive index which takes into account the complete inhomogeneity inside the prescription isoline. The tool provided constitutes an additional tool to the current available indices for treatment plan evaluation.
Conclusions
The dose volume uniformity index proposed in this study provides a method for comparing the rival plans based on the inhomogeneity inside the implant in brachytherapy. Similarly, the conformality index based on the DVUI concept helps in assessing the relative dose coverage of the prescription dose to the target volume.
References
- 1.Peiffert D. Risk factors of late complications after interstitial 192Ir brachytherapy in cancers of the oral cavity. Cancer Radiother. 1997;1:283–291. doi: 10.1016/s1278-3218(97)81495-3. [DOI] [PubMed] [Google Scholar]
- 2.Ritter M, Forman J, Kupelian P, et al. Hypofractionation for prostate cancer. Cancer J. 2009;15:1–6. doi: 10.1097/PPO.0b013e3181976614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meertens H, Borger J, Steggerda M, et al. Evaluation and optimization of interstitial brachytherapy dose distribution. In: Mould RF, Battermann JJ, Martinez AA, Speiser BL, editors. Brachytherapy from radium to optimization. Veenendaal, The Netherlands: Nucletron International; 1994. pp. 300–306. [Google Scholar]
- 4.Wu A, Ulin K, Sternick ES. A dose homogeneity index for evaluating 192Ir interstitial breast implants. Med Phys. 1988;15:104–107. doi: 10.1118/1.596152. [DOI] [PubMed] [Google Scholar]
- 5.Saw CB, Suntharalingam N, Wu A. Concept of dose nonuniformity in interstitial brachytherapy. Int J Radiat Oncol Biol Phys. 1993;26:519–527. doi: 10.1016/0360-3016(93)90971-w. [DOI] [PubMed] [Google Scholar]
- 6.Anderson LL. A “natural“ volume dose histogram for brachytherapy. Med Phys. 1986;13:898–903. doi: 10.1118/1.595815. [DOI] [PubMed] [Google Scholar]
- 7.van’t Riet A, Mak AC, Moerland MA, et al. A conformation number to quantify the degree of conformality in brachytherapy and external beam irradiation: application to the prostate. Int J Radiat Oncol Biol Phys. 1997;37:731–736. doi: 10.1016/s0360-3016(96)00601-3. [DOI] [PubMed] [Google Scholar]
- 8.Knöös T, Kristensen I, Nilsson P. Volumetric and dosimetric evaluation of radiation treatment plans: radiation conformity index. Int J Radiat Oncol Biol Phys. 1998;42:1169–1176. doi: 10.1016/s0360-3016(98)00239-9. [DOI] [PubMed] [Google Scholar]
- 9.Baltas D, Kolotas C, Geramani K, et al. A conformal index (COIN) to evaluate implant quality and dose specification in brachytherapy. Int J Radiat Oncol Biol Phys. 1998;40:515–524. doi: 10.1016/s0360-3016(97)00732-3. [DOI] [PubMed] [Google Scholar]
- 10.Lomax NJ, Scheib SG. Quantifying the degree of conformity in radiosurgery treatment planning. Int J Radiat Oncol Biol Phys. 2003;55:1409–1419. doi: 10.1016/s0360-3016(02)04599-6. [DOI] [PubMed] [Google Scholar]
- 11.Prabhakar R, Julka PK, Rath GK. Can field-in-field technique replace wedge filter in radiotherapy treatment planning: a comparative analysis in various treatment sites. Australas Phys Eng Sci Med. 2008;31:317–324. doi: 10.1007/BF03178601. [DOI] [PubMed] [Google Scholar]
- 12.Melzner WJ, Lotter M, Sauer R, Strnad V. Quality of interstitial PDR-brachytherapy-implants of head-and-neck-cancers: predictive factors for local control and late toxicity? Radiother Oncol. 2007;82:167–173. doi: 10.1016/j.radonc.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 13.Wallner K, Merrick G, Sutlief S, et al. High-dose regions versus likelihood of cure after prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2005;62:170–174. doi: 10.1016/j.ijrobp.2004.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Wust P, Postrach J, Kahmann F, et al. Postimplantation analysis enables improvement of dose-volume histograms and reduction of toxicity for permanent seed implantation. Int J Radiat Oncol Biol Phys. 2008;71:28–35. doi: 10.1016/j.ijrobp.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 15.Cormack RA, Devlin PM. Brachytherapy partial breast irradiation: analyzing effect of source configurations on dose metrics relevant to toxicity. Int J Radiat Oncol Biol Phys. 2008;71:940–944. doi: 10.1016/j.ijrobp.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Cuttino LW, Todor D, Arthur DW. CT-guided multi-catheter insertion technique for partial breast brachytherapy: reliable target coverage and dose homogeneity. Brachytherapy. 2005;4:10–17. doi: 10.1016/j.brachy.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 17.Wazer DE, Kaufman S, Cuttino L, et al. Accelerated partial breast irradiation: an analysis of variables associated with late toxicity and long-term cosmetic outcome after high-dose-rate interstitial brachytherapy. Int J Radiat Oncol Biol Phys. 2006;64:489–495. doi: 10.1016/j.ijrobp.2005.06.028. [DOI] [PubMed] [Google Scholar]