Abstract
Persistent left cranial vena cava (PLCVC) is an uncommon congenital thoracic venous anomaly in dogs. This study examines the clinical and CT findings of dogs diagnosed with PLCVC incidentally. In this study, complete type of PLCVC was diagnosed in 26 dogs with CT angiography. Shih tzu (17 cases) and Pekingese dogs (3 cases) were overrepresented. There was no gender predisposition, and the average age at presentation was 10.3 years. Of 26 dogs, one dog had a bridging vein connecting right and left cranial vena cavae, and another dog showed azygos vein terminating PLCVC. On the thoracic CT images in the third dog, the right cranial vena cava was absent so that right brachiocephalic vein ended to PLCVC. However, the right costocervical vein drained another vein coursing caudally to the right atrium with azygos vein. In conclusion, CT angiography is a very useful method to diagnose PLCVC and variations of related thoracic vein anomalies in dogs.
Keywords: azygos vein, CT, dog, PLCVC, thoracic vein anomaly
Persistent left cranial vena cava (PLCVC) is an uncommon congenital vascular anomaly in dogs. PLCVC is a remnant vessel that represents persistence of the embryonic left anterior cardinal vein, which normally regresses during development. The prevalence is less than 5% in dogs with congenital cardiovascular defects [1, 14]. A specific breed predilection and clinical features have not been described for PLCVC in dogs. PLCVC usually connects with the coronary sinus and drains into the right atrium; therefore, most PLCVC cases do not show significant clinical signs [1, 14]. The diagnosis of PLCVC can be made using angiography, echocardiography, computed tomography (CT) or magnetic resonance imaging in humans and dogs [1, 3, 5, 6, 14]. The present study describes clinical and morphologic characteristics of dogs diagnosed with PLCVC on CT examinations.
MATERIALS AND METHODS
Medical imaging records of dogs that underwent post-contrast thoracic CT at the Ian Diagnostic Center from January 2011 to March 2014 were examined for an incidental diagnosis of PLCVC. Post-contrast CT images were used for diagnosis of PLCVC. The representation of each breed, age and sex in the dogs with PLCVC was compared with the proportion of that breed in the population of dogs that underwent contrast-enhanced thoracic CT examinations from 2011 to 2014 by chi-square analysis of contingency tables by using SPSS (IBM SPSS Statistics for Windows, version 20.0; IBM Corp., New York, NY, U.S.A.). Significance was considered as P <0.05. All dogs were imaged using multi-detector CT with a 4-slice scanner (Asteion 4TM, Toshiba, Otawara, Japan). Anesthesia was performed using various anesthetic protocols according to each patient’s condition. The kVp and mA were not standardized, because patient conditions varied. Slice thickness ranged from 1 to 3 mm. Scans were acquired after IV administration of iohexol (Omnipaque®, GE Healthcare, Cork, Ireland) at 600 mg iodine/kg via the cephalic vein through an IV catheter. All post-contrast images were acquired approximately 1 min after contrast medium administration. The CT images were evaluated using a commercial software program (Rapidia®, Infinitt Healthcare Co., LTD., Seoul, Korea).
Clinical data were analyzed for clinical symptoms, the existence of heart disease, other pathologic conditions and morphologic type of PLCVC.
RESULTS
Nine hundred ninety-seven dogs underwent contrast-enhanced thoracic CT examinations during 2011–2014 at our institution. A total of 26 PLCVC (2.6%) cases were identified on the thoracic CT images. All patients were incidentally diagnosed to have PLCVC regardless of clinical signs. The mean age of the dogs with PLCVC was 10.3 years (range, 1–14). There were 9 intact female (34%), 1 spayed female (4%), 3 intact male (12%) and 13 castrated male (50%) patients. The 26 PLCVC cases included 7 breeds: Shih Tzu (17/26), Pekingese (3/26), cocker spaniel (2/26), Poodle (1/26), German shepherd (1/26), English bulldog (1/26) and Boston terrier (1/26). Shih Tzu (P <0.001) and Pekingese (P <0.05) dogs were significantly overrepresented. The dogs were presented for various clinical signs unrelated to any cardiac abnormalities or PLCVC. Fifteen of 26 dogs were diagnosed with abdominal or thoracic mass, and 2 dogs had no significant findings. Otitis media, gastric wall thickening, periodontitis, lung consolidation, sialoadenitis, rhinitis, pneumothorax and intervertebral degenerative disk disease were each identified in 1 dog. A cardiovascular anomaly (right ventricular diverticulum or aneurism) was identified incidentally in 1 dog from the CT images, and the dog suddenly died just after CT examination.
All patients had a complete-type PLCVC, which is defined when the non-atrophied left cranial cardinal vein retains connection with the coronary sinus draining to the right atrium. Representative CT images from normal dog and PLCVC dog are shown in Fig. 1. Additional variations of complete PLCVC were detected in three dogs, and these variations were schematized in Fig. 2. Dog 1 (cocker spaniel, castrated male, 10 years of age and 15 kg) had an anastomosis by an bridging vein between the right and left cranial vena cavae at the level of the thoracic inlet (Fig. 2C). The PLCVC coursed caudally and joined a severely dilated coronary sinus. Pre-contrast CT images also showed aortic arch calcification. Right atrial and ventricular enlargement were identified, and a large right ventricular outpouching (3 × 2.5 cm in size) was observed in the caudo-apical area with multiple small outpouchings on the right ventricular free wall (Fig. 3). CT images of Dog 2 (Pekingese, female, 9 years and 5.8 kg) with complete-type PLCVC revealed that the azygos vein coursed slightly along the right side of the aorta, then extended transversely toward the left side and entered the PLCVC at the level of the main pulmonary trunk (Fig. 4). Dog 3 (Poodle, female, 7 years and 4.6 kg) exhibited PLCVC without the right cranial vena cava, and blood from the right jugular and the right brachiocephalic veins drained to the PLCVC (Fig. 5). In this dog, the left costocervical vein and internal thoracic vein joined the PLCVC, while the right costocervical vein and right internal thoracic vein joined to form a vein, which coursed caudally and drained to the right atrium with the right azygos vein. Therefore, this vein looked like a right cranial vena cava. The visceral organs of this dog were normally positioned.
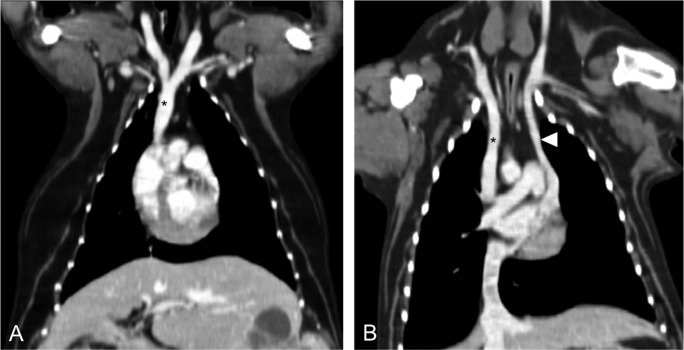
Fig. 1.
Post-contrast reconstructed dorsal CT images with soft tissue window of thorax. (A) Normally, the Rt. and Lt. brachiocephalic veins are joined cranial to the heart forming right cranial vena cava (*). (B) Note the PLCVC (arrow head) courses toward the heart and then connects to the coronary sinus.
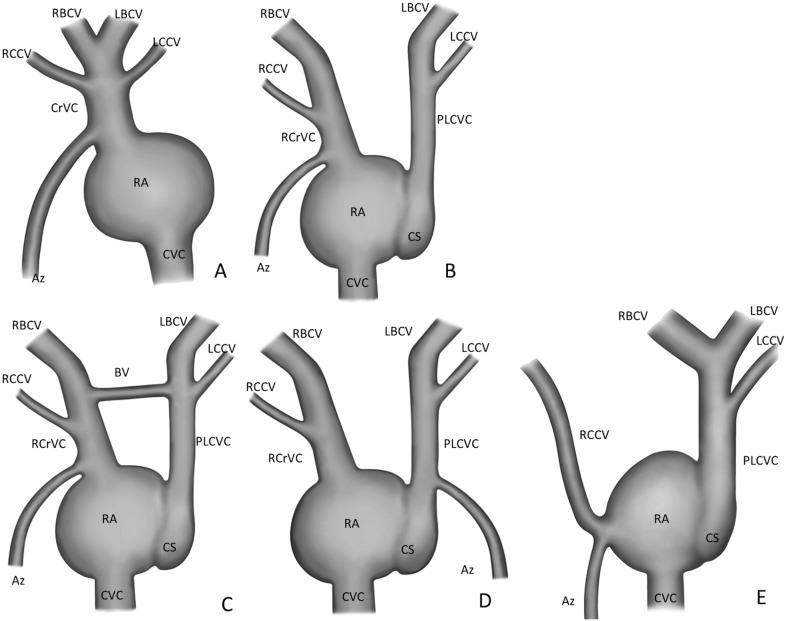
Fig. 2.
Illustrations of the appearance of thoracic vein anomalies associated with PLCVC in dogs. RBCV, right brachiocephalic vein; LBCV, left brachiocephalic vein; RCCV, right costocervical vein; LCCV, left costocervical vein; CrVC, cranial vena cava; RCrVC, right cranial vena cava; RA, right atrium; PLCVC, persistent left cranial vena cava; CS, coronary sinus; Az, azygos vein; CVC, caudal vena cava; BV, bridging vein. Schematization of a normal cranial vena cava and associated veins (A). The most common type of PLCVC (B). The bridging vein between right and left cranial vena cavae (C). Azygos vein ending to PLCVC (D). Absent right cranial vena cava and right costocervical vein ending to right atrium with azygos vein (E).
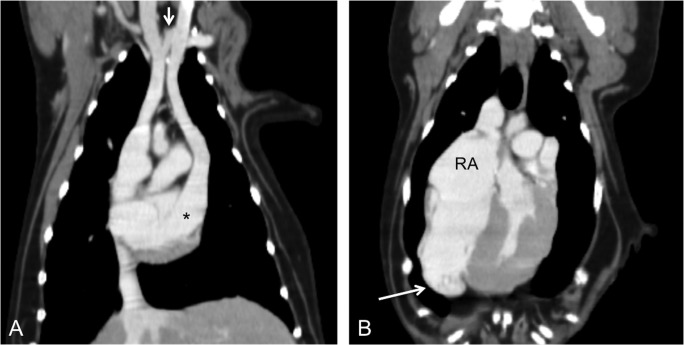
Fig. 3.
Post-contrast reconstructed dorsal (A) and transverse (B) CT images of the thorax in Dog 1. There is a bridging vein (arrow) between the right and left cranial vena cavae at the level of the thoracic inlet. In addition, a PLCVC is connected to a severely dilated coronary sinus (asterisk). Note the dilated right atrium and ventricular diverticulum (arrow).
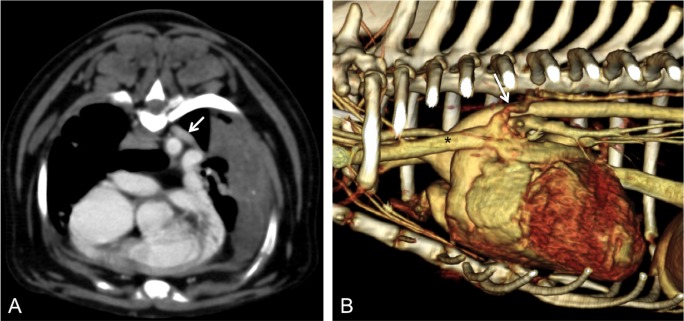
Fig. 4.
Transverse (A) and left lateral volume-rendering (B) images of Dog 2. Azygos vein (arrow) crossed over the aorta to the left side (A) and drained to PLCVC (B). Left pulmonary consolidation was identified in transverse image (A).
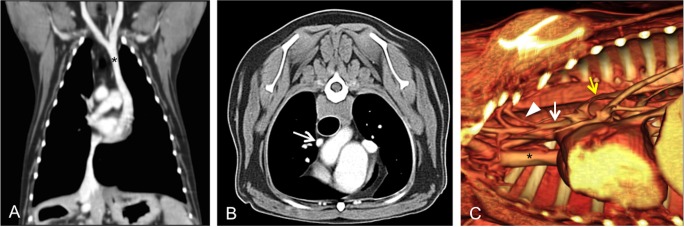
Fig. 5.
Reconstructed dorsal (A), transverse (B) and right lateral volume rendered images (C) of Dog 3. The right and left brachiocephalic veins drained into the PLCVC (asterisks in A and C). The right cranial vena cava was absent. The right costocervical vein (arrowhead in C) drained into another small vein (white arrows in B and C), which coursed caudally and ended to right atrium with the right azygos vein (yellow arrow) (C).
DISCUSSION
The prevalence of PLCVC in humans is 0.3% in healthy individuals and 4.4% in patients with congenital heart disease [22]. PLCVC is the most common congenital anomaly of the thoracic venous drainage system and is observed in 5% of dogs with congenital heart diseases [14]. In the present study, PLCVC was observed in 2.6% of the dogs that underwent thoracic CT examinations, because of reasons unrelated to cardiac anomalies.
In this study, the Shih Tzu and Pekingese breeds were significantly overrepresented. Although the Shih Tzu comprised a large proportion of the dog population underwent the contrast thoracic CT examination (196/997), no PLCVC was observed in the other major breeds, such as the Maltese (201/997), Yorkshire terrier (96/997) and Schnauzer (76/997). For PLCVC in dogs, breed and gender predilections have not been known. A genetic basis for PLCVC has been suggested in the German shepherd dog on the basis of breeding trials in dogs with concurrent persistent right aortic arch [14]. PLCVC has been diagnosed in various breeds of dogs including the German shepherd, Boston terrier, Irish setter, French bulldog, cocker spaniel, Brittany spaniel and Beagle [1,2,3, 9, 10, 23]. Similar to previous results, 1 case was identified with PLCVC in each of the German shepherd, English bulldog and Boston terrier breeds in the present study. However, the proportion of each of these breeds of the dog population in this study was too small to evaluate breed predilection.
In previous studies of dogs with PLCVC, most dogs were under 1 year of age [1, 14]. The reason for this finding might have been that the dogs were presented for the examination of other congenital cardiovascular defects. An exception is a report of a 10-year-old dog incidentally diagnosed with PLCVC during pacemaker placement [3]. In our study, the mean age of the dogs with PLCVC was greater than that previously reported. An explanation for this result might be that most dogs in our study underwent CT examination to screen for pulmonary metastasis of primary tumors at other sites. Because most dogs with PLCVC show no clinical signs, an incidental finding of PLCVC might occur at any age.
Echocardiography is a useful method to diagnose PLCVC by visualization of a dilated coronary sinus between the left atrium and pericardium at the level of the aorta [3, 4, 9]. Additionally, echocardiography allows examination of all the cardiac structures to detect any other congenital heart malformation. However, the echocardiographic diagnosis of PLCVC in man may be missed one-third of the time [24]. In a report of transvenous pacemaker placement in a dog, initial echocardiography failed to identify a dilated coronary sinus, which was diagnosed incidentally during catheterization [3]. CT and magnetic resonance imaging have been used to diagnose PLCVC in humans and dogs [5, 9, 22]. In particular, multi-detector CT angiography has proved its value in the visualization of vessels for detection of venous anomalies. A direct venogram is a method for obtaining images during the first passage of a contrast agent via the veins. The main disadvantage of this method results from artifacts caused by the inflow of undiluted contrast medium with high attenuation. To eliminate these artifacts, CT images can be acquired during the delayed phase after the contrast agent has passed through the pulmonary and circulatory systems. However, the difficulty of predicting the timing of acquisition and the insufficient opacity resulting from low contrast concentration have to be considered [17]. In a human study, 2 venous lines were used to visualize all venous connections, which may not be detected with injection of contrast agent via only 1 side, to diagnose persistent left superior vena cava (PLSVC) with CT angiography [17]. A similar technique was used in a dog with PLCVC and pulmonary arteriovenous fistula, in which contrast medium was injected into the left and right cephalic veins 10 min apart, respectively [9].
In a human study, PLSVC was incidentally identified by an bridging vein connecting the 2 superior venous drainage systems, which was observed in approximately 30% of PLSVC cases [16]. This connecting vessel has been reported to be used for the placement of a right ventricular lead during implantable cardioverter defibrillator/cardiac resynchronization therapy [11]. The accurate incidence of this connecting vein has not been known in dogs. Of 26 dogs with PLCVC in the present study, only 1 dog (Dog 1) had the connecting bridging vein on CT images. Dog 1 also had a right ventricular outpouching lesion and aortic arch calcification on CT images. Differential diagnosis consisted of an epicardial cyst, ventricular aneurism and ventricular diverticulum. These diseases could not be differentiated with only CT examination [7].
Absent right cranial vena cava with PLCVC is very rare in dogs and humans. In a human study, PLSVC in the absence of the right superior vena cava was identified in 0.15% of patients catheterized for suspected congenital cardiac disease [15, 19]. The overall proportion of patients among those previously reported with PLSVC who had no right superior vena cava was approximately 20% [17]. In the veterinary literature, the right cranial vena cava was entirely absent in 10% of dogs with PLCVC [1]. This frequency is similar to the findings in humans. Absence of the right cranial vena cava may be normal in cases of heterotaxia, dextrocardia, situs inverses and visceral transposition [21]. There are a few literature reports describing that the main coronary sinus size was significantly increased in patients without the right superior vena cava, because all venous blood from the head, neck and upper extremities drained to the PLSVC and coronary sinus [8, 12, 13]. PLSVC and absent right superior vena cava may be associated with multiple arrhythmias due to dilation of the coronary sinus opening and stretching of the AV node and bundle of His [15]. Clinical problems that might be caused by absent right superior vena cava in humans include inability to insert central venous cannulas, pulmonary artery catheters and transvenous pacing leads through the right internal jugular/subclavian vein [13]. In this study, the dog without the right cranial vena cava was situs solitus and had no associated congenital heart disease, similar to the previously reported cases in humans and dogs. In addition, the coronary sinus in this dog was not severely dilated. Absent right cranial vena cava could be diagnosed by a bilateral forelimb venogram with a bubble study during echocardiography as well as CT angiography [21].
The arrangement of azygos and hemiazygos veins may be variable in the presence of PLSVC in human reports [16, 18]. A PLCVC may be associated with the presence of left azygos veins [20]. In a human report of PLSVC with absent right superior vena cava, CT images showed an accessory azygos vein joining the PLSVC and the azygos vein connecting with a bridging vein [8]. A similar finding was revealed in an angiocardiogram of a dog with incomplete-type PLCVC [1]. In this dog, a hemiazygos vein was visualized opening into the proximal segment of a PLCVC. In the present study, 1 dog had an azygos vein joining the PLCVC not the right cranial vena cava. Similar CT findings were shown in an old man with PLSVC and absent right superior vena cava, in whom the azygos vein ran dorsal to the descending aorta and changed its course to the left side, ending in the PLSVC [17].
Two types of PLCVC have been reported in the dog, the complete and incomplete types [1]. In the complete type, the non-atrophied left cranial cardinal vein retains its embryological connection with the coronary sinus. In the incomplete type, the distal portion of the left cranial vein atrophies, whereas the proximal portion persists and receives the hemiazygos, or a vein that drains the left costocervical vertebral trunk [1]. Interestingly, the dog with the absent right cranial vena cava in the present study had a vein that received the right costocervical vertebral trunk, and ran caudally and joined with the azygos vein at the level of the main pulmonary trunk. This vein resembled the right cranial vena cava, but did not receive the right jugular and brachiocephalic veins. This dog appeared like having a mirror image of incomplete-type PLCVC. This type of anomaly has not been reported in dogs.
In conclusion, most dogs in this study were incidentally diagnosed with complete-type PLCVC at a relatively old age. On the basis of the results in this study, Shih Tzu and Pekingese dogs are overrepresented to PLCVC. A bridging vein between the right and left cranial vena cavae and absence of the right cranial vena cava were each found in 1 dog on CT angiographic images as a variation of PLCVC. CT angiography is a very useful modality for visualizing PLCVC and variations of related thoracic veins in dogs.
REFERENCES
- 1.Buchanan J. W.1963. Persistent left cranial vena cava in dogs: angiocardiography, significance, and coexisting anomalies. J. Am. Vet. Rad. Soc. 4: 1–8. doi: 10.1111/j.1740-8261.1963.tb01524.x [DOI] [Google Scholar]
- 2.Christiansen K. J., Snyder D., Buchanan J. W., Holt D. E.2007. Multiple vascular anomalies in a regurgitating German shepherd puppy. J. Small Anim. Pract. 48: 32–35. doi: 10.1111/j.1748-5827.2006.00105.x [DOI] [PubMed] [Google Scholar]
- 3.Cunningham S. M., Rush J. E.2007. Transvenous pacemaker placement in a dog with atrioventricular block and persistent left cranial vena cava. J. Vet. Cardiol. 9: 129–134. doi: 10.1016/j.jvc.2007.06.001 [DOI] [PubMed] [Google Scholar]
- 4.Fernandez del Palacio M. J., Bayon A., Agut A.1997. Dilated coronary sinus in a dog with persistent left cranial vena cava. Vet. Radiol. Ultrasound 38: 376–379. doi: 10.1111/j.1740-8261.1997.tb02101.x [DOI] [PubMed] [Google Scholar]
- 5.Gonzalez-Juanatey C., Testa A., Vidan J., Izquierdo R., Garcia-Castelo A., Daniel C., Armesto V.2004. Persistent left superior vena cava draining into the coronary sinus: report of 10 cases and literature review. Clin. Cardiol. 27: 515–518. doi: 10.1002/clc.4960270909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goyal S. K., Punnam S. R., Verma G., Ruberg F. L.2008. Persistent left superior vena cava: a case report and review of literature. Cardiovasc. Ultrasound 6: 50. doi: 10.1186/1476-7120-6-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herráez P., Rodríguez F., Aguirre-Sanceledonio M., Edwards J. F., Suárez-Bonnet A., Espinosa de Los Monteros A.2011. Congenital biventricular cardiac diverticula in a dog. Vet. Pathol. 48: 456–459. doi: 10.1177/0300985810375243 [DOI] [PubMed] [Google Scholar]
- 8.Heye T., Wengenroth M., Schipp A., Johannes Dengler T., Grenacher L., Werner Kauffmann G.2007. Persistent left superior vena cava with absent right superior vena cava: morphological CT features and clinical implications. Int. J. Cardiol. 116: e103–e105. doi: 10.1016/j.ijcard.2006.08.067 [DOI] [PubMed] [Google Scholar]
- 9.Jenni S. D., Makara M. A., Jenni R., Ohlerth S., Glaus T. M.2009. Diagnosis of pulmonary arterio-venous fistula and persistent left cranial vena cava by 3-dimensional computed tomographic reconstruction. J. Vet. Intern. Med. 23: 190–195. doi: 10.1111/j.1939-1676.2008.0228.x [DOI] [PubMed] [Google Scholar]
- 10.Larcher T., Abadie J., Roux F. A., Deschamps J. Y., Wyers M.2006. Persistent left cranial vena cava causing oesophageal obstruction and consequent megaoesophagus in a dog. J. Comp. Pathol. 135: 150–152. doi: 10.1016/j.jcpa.2006.05.002 [DOI] [PubMed] [Google Scholar]
- 11.Larsen A. I., Nilsen D. W.2005. Persistent left superior vena cava. Use of an innominate vein between left and right superior caval veins for the placement of a right ventricular lead during ICD/CRT implantation. Eur. Heart J. 26: 2178. doi: 10.1093/eurheartj/ehi516 [DOI] [PubMed] [Google Scholar]
- 12.Moorthy N., Kapoor A., Kumar S.2013. Isolated persistent left-sided superior vena cava, giant coronary sinus, atrial tachycardia and heart failure in a child. Indian Heart J. 65: 603–606. doi: 10.1016/j.ihj.2013.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neema P. K., Manikandan S., Rathod R. C.2007. Absent right superior vena cava and persistent left superior vena cava: the perioperative implications. Anesth. Analg. 105: 40–42. doi: 10.1213/01.ane.0000265551.06604.0b [DOI] [PubMed] [Google Scholar]
- 14.Patterson D. F.1968. Epidemiologic and genetic studies of congenital heart disease in the dog. Circ. Res. 23: 171–202. doi: 10.1161/01.RES.23.2.171 [DOI] [PubMed] [Google Scholar]
- 15.Pugliese P., Murzi B., Aliboni M., Eufrate S.1984. Absent right superior vena cava and persistent left superior vena cava. Clinical and surgical considerations. J. Cardiovasc. Surg. (Torino) 25: 134–137. [PubMed] [Google Scholar]
- 16.Ratliff H. L., Yousufuddin M., Lieving W. R., Watson B. E., Malas A., Rosencrance G., McCowan R. J.2006. Persistent left superior vena cava: case reports and clinical implications. Int. J. Cardiol. 113: 242–246. doi: 10.1016/j.ijcard.2005.08.067 [DOI] [PubMed] [Google Scholar]
- 17.Szymczyk K., Polguj M., Szymczyk E., Majos A., Grzelak P., Stefańczyk L.2013. Persistent left superior vena cava with an absent right superior vena cava in a 72-year-old male with multivessel coronary artery disease. Folia Morphol. (Warsz) 72: 271–273. doi: 10.5603/FM.2013.0044 [DOI] [PubMed] [Google Scholar]
- 18.Tonse M., Rai R., Prabhu L. V., Mir J., Virupakshamurthy M. B., Vadgaonkar R.2012. Double superior vena cavae with bilaterally symmetrical azygos veins and incomplete left circumflex artery. Eur. J. Anat. 16: 216–220. [Google Scholar]
- 19.Uçar O., Paşaoğlu L., Ciçekçioğlu H., Vural M., Kocaoğlu I., Aydoğdu S.2010. Persistent left superior vena cava with absent right superior vena cava: a case report and review of the literature. Cardiovasc. J. Afr. 21: 164–166. [PMC free article] [PubMed] [Google Scholar]
- 20.Uemura M., Takemura A., Ehara D., Yasumitsu H., Ohnishi Y., Suwa F.2009. Left superior vena cava with left azygos vein. Okajimas Folia Anat. Jpn. 86: 55–60. doi: 10.2535/ofaj.86.55 [DOI] [PubMed] [Google Scholar]
- 21.Waikar H. D., Lahie Y. K. M., De Zoysa L., Chand P., Kamalanesan R. P. P.2004. Systemic venous anomalies: absent right superior vena cava with persistent left superior vena cava. J. Cardiothorac. Vasc. Anesth. 18: 332–335. doi: 10.1053/j.jvca.2004.03.015 [DOI] [PubMed] [Google Scholar]
- 22.Webb W. R., Gamsu G., Speckman J. M., Kaiser J. A., Federle M. P., Lipton M. J.1982. Computed tomographic demonstration of mediastinal venous anomalies. AJR Am. J. Roentgenol. 139: 157–161. doi: 10.2214/ajr.139.1.157 [DOI] [PubMed] [Google Scholar]
- 23.Zani A., Becchetti E., Leonardi P., Sinatra A.2014. Persistent left cranial vena cava draining into the left atrium associated with pulmonary stenosis in a French bulldog. J. Vet. Cardiol. 16: 121–125. doi: 10.1016/j.jvc.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 24.Zellers T. M., Hagler D. J., Julsrud P. R.1989. Accuracy of two-dimensional echocardiography in diagnosing left superior vena cava. J. Am. Soc. Echocardiogr. 2: 132–138. doi: 10.1016/S0894-7317(89)80076-8 [DOI] [PubMed] [Google Scholar]