Abstract
Background
Traumatic finger/thumb amputations are some of the most prevalent traumatic injuries affecting Americans each year. Rates of replantation after traumatic finger/thumb amputation, however, have been steadily declining across U.S. hospitals, which may make these procedures less accessible to minorities and vulnerable populations. The specific aim of this study was to examine racial variation in finger replantation after traumatic finger/thumb amputation.
Methods
Using a two-level hierarchical model, we retrospectively compared replantation rates for African-American patients with those of Whites, adjusting for patient and hospital characteristics. Patients younger than 65 with traumatic finger/thumb amputation injuries who sought care at a U.S. trauma center between 2007 and 2012 were included in the study sample.
Results
We analyzed 13,129 patients under 65 years of age with traumatic finger/thumb amputation. Replantation rates declined over time from 19% to 14% (p = 0.004). Adjusting for patient and hospital characteristics, African-Americans (OR=0.81; CI: 0.66–0.99; p = 0.049) were less likely to undergo replantation procedures than Whites, and uninsured patients (OR=0.73; CI: 0.62–0.84; p < 0.0001) were less likely than those who were privately insured.
Conclusions
Despite advancements in microsurgical techniques and the increasing use of reconstructive surgery in other fields, finger/thumb replantation rates are declining in the U.S. and vulnerable populations are less likely to undergo replantation after amputation injuries. Regionalization of care for these injuries may not only provide a higher quality care but also reduce variations in treatment.
Keywords: Race, Disparity, Trauma, Finger/Thumb, Replantation, Amputation
INTRODUCTION
Every year, nearly 45,000 traumatic finger amputation injuries occur in the United States.1,2 The impact of finger amputation on function, quality of life, and vocational choices is substantial.3 Finger-dexterity is integral to many jobs, and amputation may result in a loss of productivity and income.4 Victims of finger amputations are usually young and in their prime income earning years.5 Thus, choosing appropriate treatment in cases of finger amputation can have substantial economic effects, not only on trauma patients, but also on the lives of their families and society.
Since the introduction of microsurgical reconstruction in the 1960s, the versatility and availability of reconstructive procedures have expanded in application.6 Although revision amputation is a relatively inexpensive and uneventful procedure, persistent pain and loss of digit length are problematic. Replantation, although a costly and challenging procedure, offers substantial functional and aesthetic benefits, such as maintaining digit length. Previous studies reveal that the estimated cost of replantation per Quality Adjusted Life Year (QALY) varies substantially depending on the level and complexity of the injury. For example, replantation of single digit injuries has the highest incremental cost effective ratio (ICER) of $136,400/QALY.7 Replantation of three or four digit, and thumb amputation injuries, however, has relatively low ICER of $27,100 and $23,800 and $26,300/QALY, respectively.7
Finger replantation procedures have been steadily declining in the U.S., which may make these procedures less accessible to minorities and vulnerable populations.8 Racial and ethnic disparities in access to quality healthcare have been a challenge for the U.S. healthcare system. To partially address this inequity, the Emergency Medicine Treatment and Active Labor Act (EMTALA) was enacted in 1986 to ensure that all trauma patients, regardless of race, insurance, or socioeconomic status have timely and high-quality access to emergency care.9 Unfortunately, there are still substantial disparities in access to quality trauma care. For example, African-Americans and other minority trauma patients are more likely to be treated at hospitals with higher mortality rates and experience higher mortality rates compared with White trauma patients.10 Despite the high prevalence of finger amputation injuries and their effects on a patient’s vocation and quality of life, little is known about disparities in treatment of these injuries.
Using 2007 to 2012 data from the National Trauma Data Bank (NTDB), the largest trauma database in the U.S., we examined variations in treatment between Whites and African-Americans, using a two-level hierarchical model and adjusting for relevant patient and hospital characteristics. The three specific aims of this study were: (1) to examine the most recent trends in prevalence of replantation vs. revision amputation, (2) to examine whether racial variations in replantation exist, and (3) to examine contributing factors associated with replantation vs. revision amputation.
MATERIALS AND METHODS
Data Source
Created by the American College of Surgeons (ACS) with the intent of providing high-quality data about trauma cases nationwide,11 the NTDB is the largest repository of trauma case data reported by trauma centers across the U.S.12 In 2012, 805 trauma centers provided data to NTDB, including 235 Level I, 267 Level II, 240 Level III or IV trauma centers.13
We examined patients who suffered digit amputation injuries between 2007 and 2012 and whose injuries were captured by the NTDB. We used the International Classification of Diseases, Ninth Revision Codes (ICD-9-CM), included in the NTDB, for diagnosis of finger and thumb amputation injuries (885.0, 885.1, 886.0, 886.1) and ICD-9-CM procedure codes for treatment of amputated fingers and thumbs (finger and thumb reattachment: 84.21 and 84.22; finger and thumb revision amputation: 84.01 and 84.02).
Patient Selection
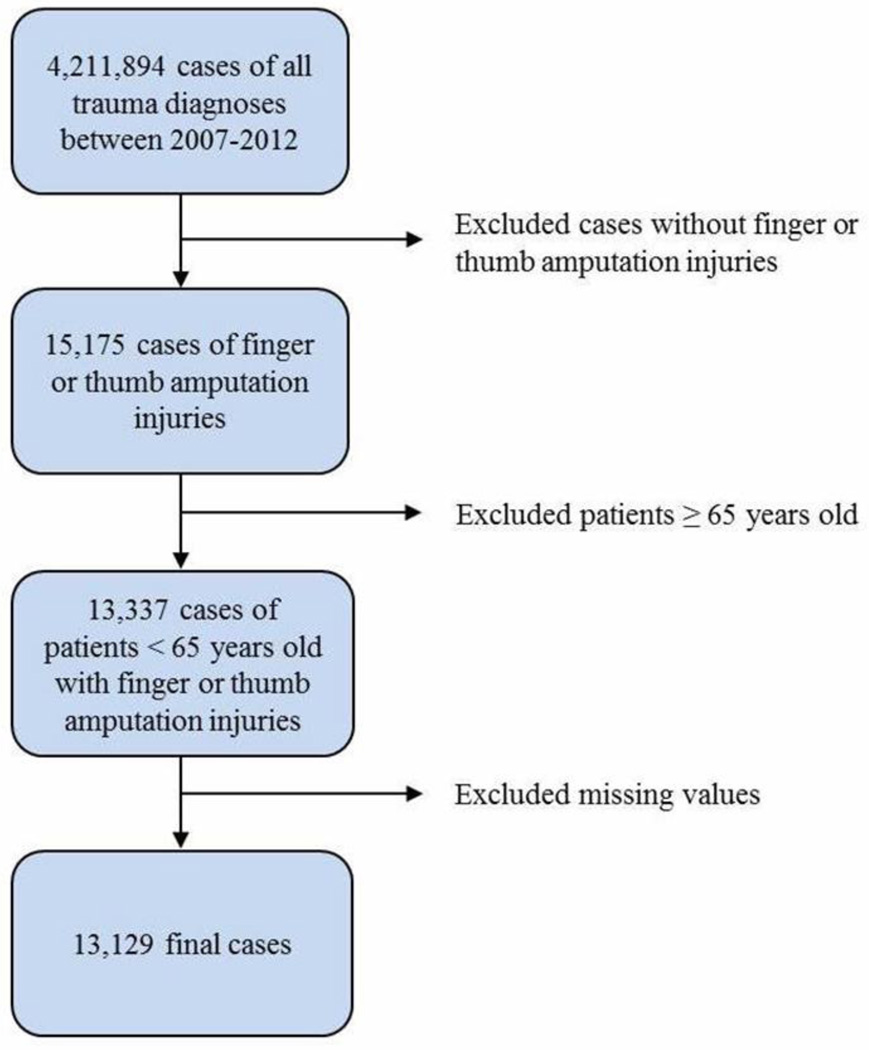
We included all patients who underwent revision amputation or replantation after experiencing traumatic digit amputation. We identified a total of 15,175 cases of finger/thumb revision amputation or replantation recorded between 2007 and 2012 in the NTDB. We excluded patients 65 years of age or older because of the confounding effects of age, health, and comorbid conditions among older individuals on treatment option. Our final sample size after excluding cases with missing values included 13,129 cases of finger/thumb revision amputation or replantation (Figure 1).
Figure 1.
Study flow diagram detailing the selection of patients in the National Trauma Data Bank (NTDB).
Source: The 2007–2012 NTDB
Explanatory and Outcome Variables
Our primary outcome of interest was the probability of undergoing replantation after traumatic finger or thumb amputation. At the patient level, we included age, sex, race, injury severity score (ISS), having multiple-digit amputation injuries (vs. one), thumb amputation injury (vs. finger), and insurance status. Age was reported as the patient’s age at the time of injury. We categorized age into three exclusive categories: less than 18, between 18 and 44, and between 45 and 65. Race was reported according to the patient’s self-reported information. We measured race by creating four distinct categories: Whites, African-Americans, other races, and unspecified. Seven percent of patients did not specify their race. To be able to include them in our analysis, we created a separate category for patients for whom race was not known. Additionally, we did not include ethnicity as one of our variables because the percentage of missing values was higher than the threshold of 30%. Insurance was measured using five distinct categories: private (including commercial, Blue Cross Blue Shield, and worker’s compensation), public (including Medicaid and Medicare), other (including no fault and other insurance), self-pay (no insurance), and unspecified (about 10%), with private insurance serving as the reference category. Thumb replantation was identified via the ICD-9 procedure codes. We used the Injury Severity Score (ISS) to control for the overall severity of the injury.14
At the hospital level, we controlled for being public vs. for-profit, teaching status, trauma center level, and region of the hospital. Teaching status was measured using three distinct categorical variables of community, non-teaching, and teaching hospitals. Trauma level was measured using four mutually exclusive categories: level I, level II, level III, and other hospitals. The ACS verifies the level of care and resources at each trauma center.15 Level I trauma centers are considered regional centers of care for any type of injury. Level II trauma centers should have enough resources to initiate care for all types of injuries. Level III or higher trauma centers are those that are capable of treating non-complex emergency cases; these centers should transfer patients who may need more comprehensive care to Level I or II trauma centers.15 Additionally, there are hospitals that are not officially trauma centers but do provide emergent care; we included them as ‘other hospitals’ in our model. Finally, we included each hospital’s geographic region.
Analysis
We used three logistic models to examine the association between race and replantation after traumatic finger/thumb amputation. In our first model, we included age, sex, and race as explanatory variables. We added injury characteristics and patient insurance status to the second model. In models 1 and 2, to obtain the robust cluster estimators based on hospital identifier, we used the vce (cluster)16 option in Stata to adjust for potential intra-hospital correlation. Finally, in model 3, we used a two-level hierarchical model (meqrlogit) to include all relevant patient and hospital characteristics and adjust for intercept random effects for hospitals. We used Stata version 13.1 for all analyses.
RESULTS
Table 1 displays the characteristics of patients who experienced traumatic finger/thumb amputation injuries. The average age of patients was 37 and 87% were male. White, African-American, and other races represented 70%, 8%, and 22% of the patients in our sample, respectively. Compared with those who underwent revision amputation, patients who underwent replantation were younger, had lower injury severity scores, had a higher rate of multiple digit or thumb amputation injuries, and were more likely to have private insurance. African-Americans and other races were younger than Whites in both treatment groups (p < 0.05). Regardless of race, a higher percentage of uninsured patients underwent revision amputation; however, the percentage of uninsured African-American patients who underwent revision amputation was 10 percentage points higher than Whites (26% vs. 16%; p < 0.001).
Table 1.
Characteristics of individuals under 65 with finger and thumb amputationa injuries between 2007 and 2012
| Treatmentb | Replantation | Revision Amputation | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White | African- American |
Other Races | White | African- American |
Other Races | |||||||
| Avg (%) |
SE | Avg (%) |
SE | Avg (%) |
SE | Avg (%) |
SE | Avg (%) |
SE | Avg (%) |
SE | |
| N=13,337c | 1,592 | 147 | 559 | 7,520 | 941 | 2,578 | ||||||
| Age: | ||||||||||||
| Less than 18 | 18 | 0.01 | 26§ | 0.04 | 14§ | 0.01 | 10* | 0.00 | 13§* | 0.01 | 9* | 0.01 |
| 18 to 44 | 46 | 0.01 | 38§ | 0.04 | 63§ | 0.02 | 48 | 0.01 | 57§* | 0.02 | 62§ | 0.01 |
| 45 to 65 | 36 | 0.01 | 37 | 0.04 | 24§ | 0.02 | 43* | 0.01 | 30§ | 0.01 | 30§* | 0.01 |
| Female | 14 | 0.01 | 15 | 0.03 | 11 | 0.01 | 13 | 0.00 | 15 | 0.01 | 12 | 0.01 |
| Injury Characteristics: | ||||||||||||
| Injury severity scored (n) | 4.1 | 0.07 | 3.99 | 0.25 | 4.01 | 0.10 | 4.78* | 0.06 | 5.5§* | 0.20 | 4.74* | 0.09 |
| Multiple digit amputation | 35 | 0.35 | 25§ | 0.25 | 38 | 0.38 | 19* | 0.00 | 16§* | 0.01 | 18* | 0.01 |
| Thumb amputation | 38 | 0.38 | 36 | 0.36 | 35 | 0.35 | 15* | 0.00 | 11§* | 0.01 | 14* | 0.01 |
| Insurancee | ||||||||||||
| Private insurance | 63 | 0.01 | 46§ | 0.04 | 45§ | 0.02 | 58* | 0.01 | 39§ | 0.02 | 43§ | 0.01 |
| Public insurance | 9 | 0.09 | 19§ | 0.19 | 10 | 0.10 | 10 | 0.00 | 18§ | 0.01 | 9§ | 0.01 |
| No insurance | 12 | 0.12 | 19§ | 0.19 | 20§ | 0.20 | 16* | 0.00 | 26§* | 0.01 | 23§* | 0.01 |
| Other insurance | 6 | 0.06 | 7 | 0.07 | 6 | 0.06 | 7 | 0.00 | 8 | 0.01 | 8 | 0.01 |
| Insurance missing | 10 | 0.01 | 9 | 0.02 | 19§ | 0.02 | 9 | 0.00 | 9 | 0.01 | 18§ | 0.01 |
Source: the 2007 to 2012 NTDB
Type of injury is defined based on ICD-9 diagnosis codes provided in DCODE table in the NTDB database (Appendix Table A1).
Treatment is defined based on ICD-9 procedure codes provided in PCODE table in the NTDB database (Appendix Table A2).
Total number of patients under 65 with traumatic amputation injuries of finger or thumb who treated at one of the registered trauma centers in the U.S.
Injury severity score is based on abbreviated injury scale (AIS 98) reported in the NTDB database.
Private insurance includes commercial private insurance and blue cross blue shield; public insurance includes Medicare and Medicaid; other insurance includes work compensation and other unspecified insurance.
Significantly different between White and African-Americans or Whites and other race within each treatment group at the 95% confidence interval.
Significantly different within the same race between revision amputation and replantation groups at the 95% confidence interval.
Abbreviations: NTDB, National Trauma Data Bank; SE, Standard Error; Avg, Average (mean).
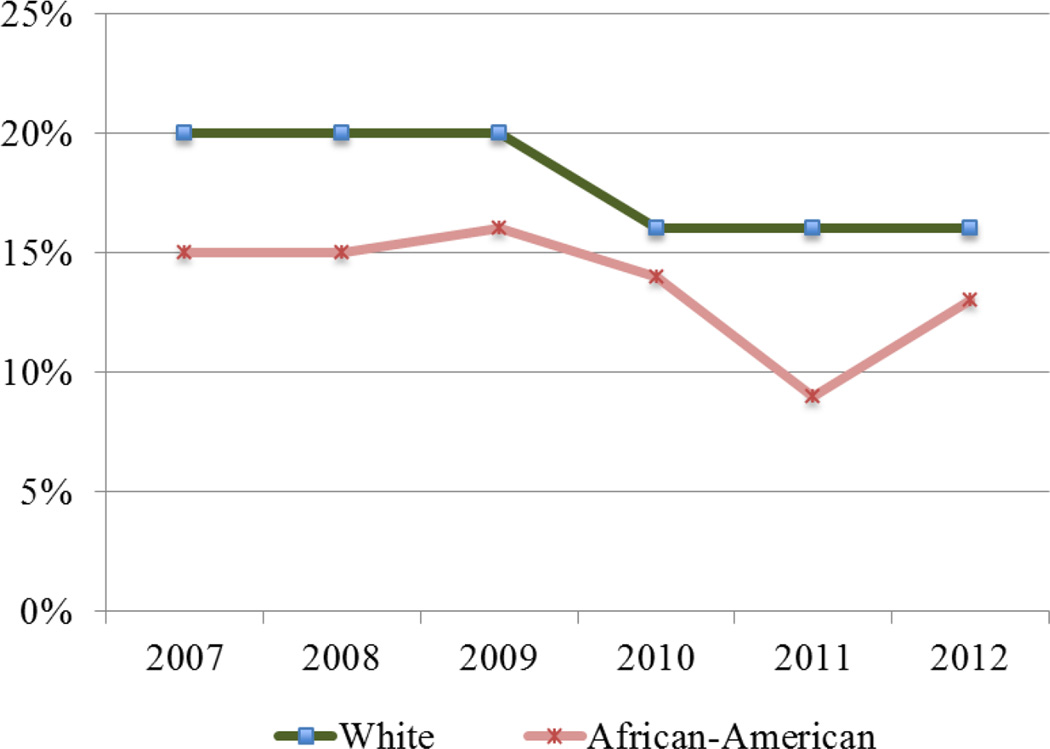
Number of participating hospitals that cared for patients with finger amputation injuries increased in NTDB from 204 hospitals in 2007 to 313 hospitals in 2012 (Figure 2). Despite an increase in the number of reported finger amputation injuries from 1,679 cases in 2007 to 2,530 cases in 2012, the replantation rate dropped from 19% to 14% (p = 0.004). In 2007, Whites had a replantation rate that was five percentage points higher than that of replantation for African-Americans; this dropped to a three percentage point difference in 2012 (not statistically significant).
Figure 2.
Unadjusted trends in finger/thumb replantation rate in the U.S. between 2007 and 2012, stratified by race.
Source: The 2007–2012 NTDB
Note: White/African-American differences in finger/thumb replantation rate were significant at 95% CI.
We stratified hospitals by the annual number of finger/thumb replantations (Table 2). Nearly half of all finger/thumb amputation injuries (6,072 out of 13,337) were treated in hospitals with no or just one replantation procedure a year. About half of these hospitals were public, community hospitals with 200–400 beds. Only 12% of patients with finger amputation injuries presented to hospitals that performed more than 10 annual finger replantation procedures. More than 90% of high-volume (more than 10 annual replantations) hospitals were public, university hospitals with more than 400 beds; they were either Level I trauma centers (88%) or were not registered as an official trauma center (12%).
Table 2.
Hospital characteristics based on number of finger/thumb replantation procedures performed between 2007 and 2012.
| Trauma Centers | Between 0–1 replantation |
Between 2–5 replantation |
Between 6–10 replantation |
More than 10 replantation |
|---|---|---|---|---|
| Total number of hospitals=764 | 571 | 133 | 43 | 17 |
| Total number of cases=13,337 | 6,072 (46%) | 3,575 (27%) | 2,100 (16%) | 1,590 (12%) |
| Total number of replantation=2,298 | 346 (15%) | 831(36%) | 539 (23%) | 582 (25%) |
| Public/Private* | ||||
| For Profit | 64 (11%) | 9 (7%) | 2 (5%) | 1 (6%) |
| Public | 505 (88%) | 124 (93%) | 41 (95%) | 16 (94%) |
| Not specified | 2 (1%) | - | - | - |
| Teaching Status* | ||||
| Community | 251 (44%) | 32 (24%) | 5 (12%) | 1 (6%) |
| Non-teaching | 155 (27%) | 11 (8%) | 1 (2%) | 0 (0%) |
| University hospital | 165 (29%) | 90 (68%) | 37 (86%) | 16 (94%) |
| Number of beds* | ||||
| < 200 | 98 (17%) | 6 (5%) | 1 (2%) | 0 (0%) |
| 200 to 400 | 239 (42%) | 30 (23%) | 2 (5%) | 0 (0%) |
| 401 to 600 | 140 (25%) | 43 (32%) | 11 (26%) | 5 (29%) |
| More than 600 | 94 (16%) | 54 (41%) | 29 (68%) | 12 (71%) |
| Trauma level* | ||||
| Level I | 134 (23%) | 84 (63%) | 35 (82%) | 15 (88%) |
| Level II | 201 (35%) | 21 (16%) | 1 (2%) | 0 (0%) |
| Level III or higher | 109 (19%) | 2 (1%) | 0 (0%) | 0 (0%) |
| Other | 127 (22%) | 26 (20%) | 7 (16%) | 2 (12%) |
| Trauma Center Region* | ||||
| Midwest | 202 (35%) | 42 (32%) | 12 (28%) | 4 (24%) |
| Northeast | 84 (15%) | 24 (18%) | 8 (19%) | 4 (24%) |
| South | 173 (30%) | 48 (36%) | 15 (35%) | 5 (29%) |
| West | 108 (19%) | 19 (14%) | 8 (19%) | 4 (23%) |
| Not specified | 4 (1%) | - | - | - |
Source: The 2007–2012 NTDB
Significantly different between the groups at 95% confidence interval.
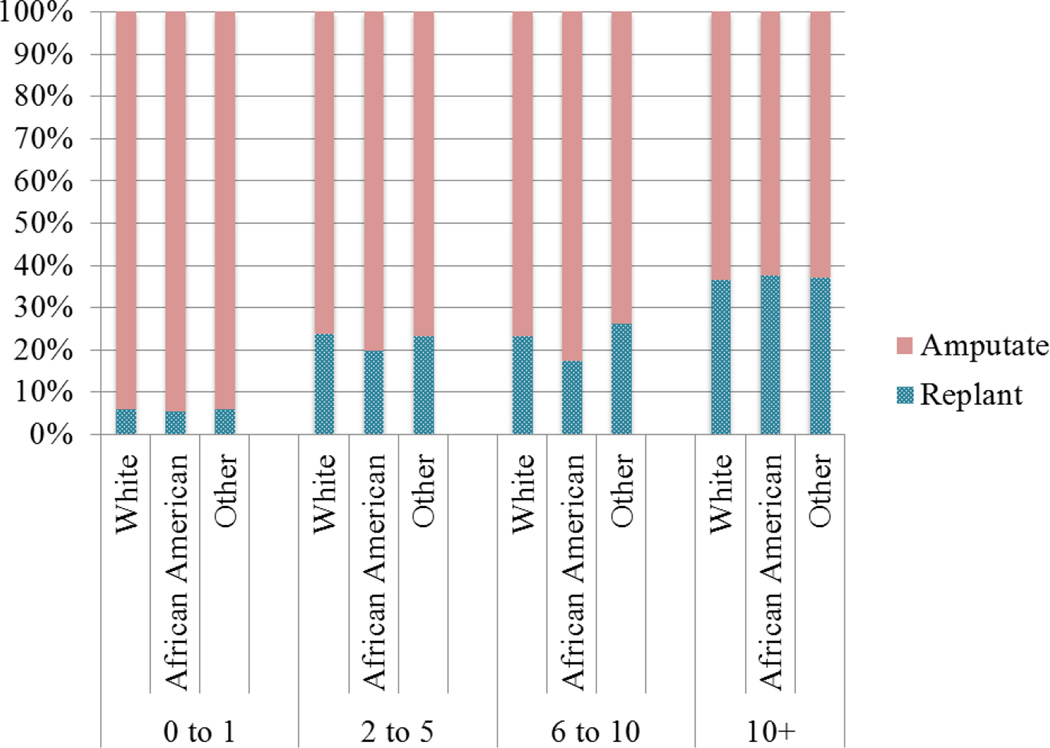
Figure 3 illustrates the rate of replantation in each category of hospitals. The rate of finger/thumb replantation was about 5%, with no difference between Whites and African-Americans or Whites and other races in hospitals with 0 to 1 replantations per year. The rate of finger/thumb replantation in hospitals with 2–5 replantation procedures a year jumped to about 20%. In hospitals with 6 to 10 replantation procedures a year, replantation rates among Whites, African-Americans, and other races were 23%, 17%, and 26%, respectively. There were only 17 hospitals that performed more than 10 finger replantation procedures annually; in these hospitals, the rate of replantation jumped to about 36%, with no significant difference between Whites and African-Americans or Whites and other races. However, only 12% (or 1,590 patients out of 13,337 patients in our cohort) presented to these hospitals.
Figure 3.
Rate of finger/thumb replantation versus revision amputation, stratified by hospital replantation volume and race.
Source: The 2007–2012 NTDB
Note: White/African American differences in finger/thumb replantation rate were significant at 95% CI in hospitals with 2–5 and 6–10 replantations per year.
Table 3 presents the odds of undergoing finger replantation after a finger/thumb amputation injury. In our first model, we adjusted for patients’ age, sex, and race. African-Americans had lower odds of undergoing replantation after a finger amputation injury (OR=0.70; CI: 0.58 – 0.85; p < 0.001). In our second model, we further adjusted for injury characteristics and type of health insurance. The odds of undergoing replantation increased for African-Americans, but still remained significantly lower than the odds for Whites (OR=0.82; CI: 0.68 – 0.99; p = 0.048). Finally, after adjusting for relevant and available patient and hospital characteristics in our third model, African-Americans showed lower odds of undergoing replantation procedures compared to their White counterparts (OR=0.81; CI: 0.66 – 0.99; p = 0.049). Other patient factors that were associated with the probability of undergoing replantation after finger/thumb amputation injury were age and injury characteristics. For example, being younger than 18 years of age increased the odds of replantation (OR=2.64; CI: 2.21 – 3.14; p < 0.001). A higher injury severity score decreased the odds of replantation (OR=0.92; CI: 0.91 – 0.94; p < 0.001). In contrast, having multiple digit amputations (OR=1.86; CI: 1.66 – 2.09; p < 0.001) and thumb amputations (OR=3.51; CI: 3.14 – 3.94; p < 0.001) increased the odds of replantation. Having public (OR=0.79; CI: 0.66 – 0.95; p = 0.011) or no insurance (OR=0.73; CI: 0.62 – 0.84; p < 0.001) compared with having private insurance decreased the odds of undergoing replantation. At the hospital level, attending community (OR=0.59; CI: 0.45 – 0.79; p < 0.0001) and non-teaching hospitals (OR=0.57; CI: 0.38 – 0.85; p = 0.006), compared with teaching hospitals, and attending Level II (OR=0.65; CI: 0.47 – 0.90; p = 0.009) or higher (OR= 0.61; CI: 0.37 – 0.99; p = 0.045) trauma centers, compared with Level I trauma centers, decreased the odds of undergoing replantation.
Table 3.
Logistic regression models examining probability of replantation after a finger/thumb traumatic amputation injury
| Replantation | Model 1 - Patient Factors | Model 2 – Patient Factors | Model 3 - Hierarchical Model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | P | OR | 95% CI | p | |
| Patient Characteristics: | |||||||||
| Age: | |||||||||
| Less than 18 | 2.15 | 1.75 – 2.65 | 0.000 | 2.50 | 2.15 – 2.91 | 0.000 | 2.64 | 2.21 – 3.14 | 0.000 |
| 18 to 44 | 1.15 | 1.03 – 1.28 | 0.015 | 1.18 | 1.06 – 1.31 | 0.003 | 1.19 | 1.06 – 1.33 | 0.003 |
| 45 to 65 (ref.) | 1.00 | ||||||||
| Female | 0.94 | 0.82 – 1.08 | 0.386 | 1.06 | 0.92 – 1.22 | 0.452 | 1.11 | 0.95 – 1.30 | 0.178 |
| Race: | |||||||||
| White (ref.) | 1.00 | 1.00 | 1.00 | ||||||
| African-American | 0.70 | 0.58 – 0.85 | 0.000 | 0.82 | 0.68 – 0.99 | 0.048 | 0.81 | 0.66 – 0.99 | 0.049 |
| Other race | 0.98 | 0.79 – 1.21 | 0.843 | 1.08 | 0.95 – 1.23 | 0.248 | 0.96 | 0.82 – 1.13 | 0.654 |
| Race not specified | 1.10 | 0.86 – 1.41 | 0.463 | 1.07 | 0.89 – 1.28 | 0.457 | 1.18 | 0.96 – 1.46 | 0.124 |
| Injury Characteristics: | |||||||||
| Injury severity score | 0.93 | 0.91 – 0.94 | 0.000 | 0.92 | 0.91 – 0.94 | 0.000 | |||
| Multiple digit | 2.13 | 1.92 – 2.36 | 0.000 | 1.86 | 1.66 – 2.09 | 0.000 | |||
| Thumb (vs. finger) | 3.59 | 3.24 – 3.99 | 0.000 | 3.51 | 3.14 – 3.94 | 0.000 | |||
| Insurance: | |||||||||
| Private (ref.) | 1.00 | 1.00 | |||||||
| Public | 0.73 | 0.61 – 0.86 | 0.000 | 0.79 | 0.66 – 0.95 | 0.011 | |||
| No insurance | 0.69 | 0.60 – 0.79 | 0.000 | 0.73 | 0.62 – 0.84 | 0.000 | |||
| Other insurance | 0.81 | 0.67 – 0.98 | 0.034 | 0.83 | 0.67 – 1.03 | 0.097 | |||
| Insurance not specified | 0.96 | 0.82 – 1.12 | 0.595 | 0.89 | 0.72 – 1.11 | 0.298 | |||
| Trauma Center Characteristics: |
|||||||||
| For profit | 0.96 | 0.62 – 1.50 | 0.861 | ||||||
| Teaching status: | |||||||||
| Community hospital | 0.59 | 0.45 – 0.79 | 0.000 | ||||||
| Non teaching | 0.57 | 0.38 – 0.85 | 0.006 | ||||||
| University (ref.) | 1.00 | ||||||||
| Trauma Level: | |||||||||
| Level 1 (ref.) | 1.00 | ||||||||
| Level 2 | 0.65 | 0.47 – 0.90 | 0.009 | ||||||
| Level 3 or higher | 0.61 | 0.37 – 0.99 | 0.045 | ||||||
| Other | 0.96 | 0.72 – 1.27 | 0.768 | ||||||
| Trauma Center Region: | |||||||||
| Midwest | 0.82 | 0.58 – 1.16 | 0.265 | ||||||
| Northeast | 1.37 | 0.92 – 2.04 | 0.121 | ||||||
| South | 0.76 | 0.54 – 1.07 | 0.118 | ||||||
| West (ref.) | 1.00 | ||||||||
| Intercept | 0.18 | 0.15 – 0.22 | 0.000 | 0.15 | 0.14 – 0.17 | 0.000 | 0.16 | 0.12 – 0.23 | 0.000 |
| N=13,315; | Chi2=75.83; | P=0.000 | N=13,314; | Chi2=838.88 | P=0.000 | N=13,129 | Chi2=797.16 | P=0.000 | |
Source: The 2007 – 2012 NTDB
Sensitivity Analysis
Between 2007 and 2012, number of NTDB participating hospitals providing care for finger amputation injuries increased from 204 hospitals in 2007 to 313 hospitals in 2012. In addition to our open cohort analyses of hospitals, we repeated our analyses with the 97 hospitals that participated in NTDB during all six years. Number of observations reduced to 6,937, but our qualitative results were the same. Between 2007 and 2012, among the 97 participating hospitals the overall rate of finger/thumb replantation reduced by five percentage points from 21% to 16%, and variations in replantation between Whites and African-Americans remained intact, with Whites having a higher rate of replantation (18% vs. 13%; p=0.003; CI=0.016–0.076).
COMMENT
In this study, we examined recent trends and racial variations in the treatment of traumatic finger/thumb amputation. Three findings emerged. First, for all races, the rate of finger/thumb replantation has been steadily declining in the U.S. among trauma centers participating in the NTDB. Second, even after adjusting for relevant patient and hospital characteristics, compared with Whites, African-Americans had a lower probability of undergoing finger replantation. Third, factors such as having private insurance and presenting to a hospital with a higher volume of replantation procedures increased the probability of undergoing replantation compared with revision amputation.
Although in our sample number of hospitals and finger amputation injuries increased over time, rate of replantation declined. Research suggests that replantation surgery is performed less frequently today than it was 20 years ago.17,18 The decline in replantation procedures is likely attributable to the declining reimbursement and changing economic and surgical landscapes.17,18 A 2007 survey of members of the American Society for Surgery of the Hand (ASSH) found that 44% of their members opt not to perform microsurgeries. They cite busy elective schedules (51%), low microsurgical confidence (39%), and inadequate compensation (25%) as their primary motives for avoiding replantation surgery.17 Several authors have suggested that the declining number of replantation procedures may have diminished confidence among surgeons in their microsurgical skill set.17,19,20 This lack of confidence across hand surgeon groups is corroborated by the decreasing success rates of digit replantation over the last 20 years.21–24 Today, despite recent microsurgical advancements, evidence suggests that in contrast to other developed countries, replantation success rates in the U.S. have fallen to approximately 60%,25 Replantation remains uncommon in the U.S. compared with other developed countries.26–29 For example, in 2001, 2004, and 2007 combined, only 27% of thumb and 12% of finger traumatic amputations were replanted.6 Surgeons who perform replantation staff only 15% of U.S. trauma centers,30–32 and microsurgical expertise remains a scarce resource.33,34 Additionally, previous studies have demonstrated that the distribution of surgeons with skills in microsurgical techniques is not uniform, and replantation is most commonly performed in large public teaching hospitals.6,35
The existence of racial disparities in the surgical setting has been well-documented. For example, African-American patients are at greater risk of suffering lower limb amputation for advanced limb ischemia when compared with their White counterparts.36 In fact, African-Americans are less likely to undergo attempts at revascularization before their surgeons resort to amputation.37 The literature points to similar disparities in access to other surgical procedures, such as total knee and hip arthroplasty,38,39 kidney transplantation,40 and coronary-artery bypass graft.41
Although our unadjusted data did not show statistically significant gap between Whites and African-Americans in replantation rate, our adjusted analytical models reveal lower odds of replantation for African-Americans compared to Whites. Research suggests that racial disparities in surgical settings are associated with system-level differences in access to care. For example, in their study of amputation frequency in patients with lower limb ischemia, Eslami et al. found that primary amputation was performed more frequently on non-White, low-income, uninsured patients.42 The authors postulated that lack of patients’ access to adequate primary care and surgery providers delayed diagnosis and ultimately created a greater need for limb amputation. Furthermore, Squitieri et al. found that pediatric patients with private insurance were more likely to receive replantation than uninsured patients.43 Their results were extended by Shale et al., who found that private insurance and worker’s compensation were associated with the highest rates of replantation in patients of all ages.44
This study has a few important limitations. This study has a few important limitations. First, although the NTDB is the largest trauma registry in the U.S., it lacks granularity at the patient and hospital levels. For example, like most large datasets, patient/cultural preferences over treatment options or desire to return to work were not included in the NTDB. Patient and cultural preferences do differ across races and are important contributing factors to be included in analytical models, if available.40 Second, using the NTDB, we were unable to follow patients longitudinally to capture important information such as number of transfers prior to final treatment or success rates of replantation. Third, owing to a high percentage of missing values for certain variables such as ethnicity or mechanisms of injury, we were unable to examine their associations with treatment of finger amputation injuries. Despite these limitations, our study shows that even after adjusting for available confounding patient- and hospital-level variables, racial disparity between African-Americans and Whites in receiving replantation vs. revision amputation persists.
In 2006, the Institute of Medicine report entitled “Hospital-Based Emergency Care: At the Breaking Point” emphasized the need for an “efficient, accountable, and equitable” regionalized trauma care system in the U.S.45 Yet, numerous studies demonstrate multiple barriers to emergency care among economically vulnerable individuals who suffer traumatic injuries.46 For other traumatic conditions such as burn injuries or penetrating and blunt trauma, several policy initiatives have been developed to streamline access to care and improve quality.47 In 1976, the ACS developed specific guidelines to create designated trauma centers.48 These designations created great interest in the selective referral of patients toward high-volume or high-performing centers, or the “regionalization” of care. There is growing empirical evidence that the integration of trauma care services into a regionalized system reduces mortality.49 Our findings are consistent with these studies. We show that receiving treatment in high-volume centers is not only associated with an increased probability of undergoing replantation versus revision amputation, but it is also associated with reduced racial disparities in the likelihood of undergoing such replantation procedures.
To date, despite many unresolved challenges, the regionalization and systematic coordination of trauma care have continued to become the standard of emergency care.50 However, the extent to which regionalization and systematic coordination could be applied to finger/thumb amputation injuries remains uncertain. The complexity of replantation suggests that procedures performed at higher-volume centers could shorten operative times, improve outcomes, and decrease expenses.6,26
In conclusion, after controlling for relevant patient and hospital factors, our findings indicate that African-American patients are less likely to undergo a replantation procedure after experiencing a finger/thumb amputation injury. Given that finger/thumb amputation injuries constitute a substantial portion of all surgical trauma cases, and considering that these injuries may have a long and devastating effects on one’s career and life, and potentially on the public support system as well, reducing barriers to quality treatment, particularly for vulnerable populations, should be a priority for policy makers and surgeons.
Supplementary Material
Acknowledgments
Sources of Funding: Dr. Kevin C. Chung is currently receiving the Midcareer Investigator Award in Patient-Oriented Research (2 K24-AR053120-06) from the NIH.
Footnotes
Conflicts of Interest None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Author Contributions:
Access to data: Dr. Mahmoudi had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Mahmoudi, Elham, Swiatek, Peter, Chung, Kevin
Acquisition, analysis, or interpretation of data: Mahmoudi, Elham, Swiatek, Peter, Chung, Kevin, Ayanian, John
Drafting the manuscript: Mahmoudi, Elham, Swiatek, Peter
Critical revision of the manuscript for important intellectual content: Ayanian, John, Chung, Kevin
Statistical analysis: Mahmoudi, Elham
Study supervision: Chung, Kevin
REFERENCES
- 1.Conn JM, Annest JL, Ryan GW, Budnitz DS. Non-work-related finger amputations in the United States, 2001–2002. Annals of emergency medicine. 2005 Jun;45(6):630–635. doi: 10.1016/j.annemergmed.2004.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Bureau of Labor Statistics. [Accessed November 7, 2011];2011 http://data.bls.gov/data.
- 3.Sears ED, Shin R, Prosser LA, Chung KC. Economic analysis of revision amputation and replantation treatment of finger amputation injuries. Plastic and reconstructive surgery. 2014 Apr;133(4):827–840. doi: 10.1097/PRS.0000000000000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyle D, Parker D, Larson C, Pessoa-Brandao L. Nature, incidence, and cause of work-related amputations in Minnesota. American journal of industrial medicine. 2000 May;37(5):542–550. doi: 10.1002/(sici)1097-0274(200005)37:5<542::aid-ajim10>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 5.Chung KC, Alderman AK. Replantation of the upper extremity: indications and outcomes. JASSH. 2002;2:78–94. 2002. [Google Scholar]
- 6.Friedrich JB, Poppler LH, Mack CD, Rivara FP, Levin LS, Klein MB. Epidemiology of upper extremity replantation surgery in the United States. J Hand Surg Am. 2011 Nov;36(11):1835–1840. doi: 10.1016/j.jhsa.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Sears ED, Shin R, Prosser LA, Chung KC. Economic Analysis of Revision Amputation and Replantation Treatment of Finger Amputation Injuries. Plastic and reconstructive surgery. 2014;133(4):827. doi: 10.1097/PRS.0000000000000019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Payatakes AH, Zagoreos NP, Fedorcik GG, Ruch DS, Levin LS. Current practice of microsurgery by members of the American Society for Surgery of the Hand. The Journal of hand surgery. 2007;32(4):541–547. doi: 10.1016/j.jhsa.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 9.Lee TM. EMTALA Primer: The Impact of Changes in the Emergency Medicine Landscape on EMTALA Compliance and Enforcement, An. Annals Health L. 2004;13:145. [PubMed] [Google Scholar]
- 10.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Archives of Surgery. 2012;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Russe O. Reproduction and Hollerith system in the service of documentation on accident surgery. Klinische Medizin; osterreichische Zeitschrift fur wissenschaftliche und praktische Medizin. 1960 Sep;15:434–437. [PubMed] [Google Scholar]
- 12.Haider AH, Saleem T, Leow JJ, et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: is it time to set research best practices to further enhance its impact? Journal of the American College of Surgeons. 2012 May;214(5):756–768. doi: 10.1016/j.jamcollsurg.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Trauma Data Bank 2014: Annual Report. [Accessed June 23, 2015];2014 https://www.facs.org/~/media/files/quality%20programs/trauma/ntdb/ntdb%20annual%20report%202014.ashx. [Google Scholar]
- 14.Babu MA, Nahed BV, DeMoya MA, Curry WT. Is trauma transfer influenced by factors other than medical need? An examination of insurance status and transfer in patients with mild head injury. Neurosurgery. 2011;69(3):659–667. doi: 10.1227/NEU.0b013e31821bc667. [DOI] [PubMed] [Google Scholar]
- 15.American Trauma Society (ATS) Trauma Center Levels Explained. [Accessed March 15, 2015];2015 http://www.amtrauma.org/?page=TraumaLevels. [Google Scholar]
- 16.Cameron AC, Miller DL. A practitioner’s guide to cluster-robust inference. Journal of Human Resources. 2015;50(2):317–372. [Google Scholar]
- 17.Payatakes AH, Zagoreos NP, Fedorcik GG, Ruch DS, Levin LS. Current practice of microsurgery by members of the American Society for Surgery of the Hand. The Journal of hand surgery. 2007 Apr;32(4):541–547. doi: 10.1016/j.jhsa.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Fufa D, Calfee R, Wall L, Zeng W, Goldfarb C. Digit replantation: experience of two US academic level-I trauma centers. The Journal of Bone & Joint Surgery. 2013;95(23):2127–2134. doi: 10.2106/JBJS.L.01219. [DOI] [PubMed] [Google Scholar]
- 19.Sabapathy SR, Venkatramani H, Bharathi RR, Bhardwaj P. Replantation surgery. The Journal of hand surgery. 2011 Jun;36(6):1104–1110. doi: 10.1016/j.jhsa.2011.03.039. [DOI] [PubMed] [Google Scholar]
- 20.Chen MW, Narayan D. Economics of upper extremity replantation: national and local trends. Plastic and reconstructive surgery. 2009 Dec;124(6):2003–2011. doi: 10.1097/PRS.0b013e3181bf8008. [DOI] [PubMed] [Google Scholar]
- 21.Lin PY, Sebastin SJ, Ono S, Bellfi LT, Chang KW, Chung KC. A systematic review of outcomes of toe-to-thumb transfers for isolated traumatic thumb amputation. Hand. 2011 Sep;6(3):235–243. doi: 10.1007/s11552-011-9340-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morrison WA, McCombe D. Digital replantation. Hand clinics. 2007 Feb;23(1):1–12. doi: 10.1016/j.hcl.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 23.Waikakul S, Sakkarnkosol S, Vanadurongwan V, Un-nanuntana A. Results of 1018 digital replantations in 552 patients. Injury. 2000 Jan;31(1):33–40. doi: 10.1016/s0020-1383(99)00196-5. [DOI] [PubMed] [Google Scholar]
- 24.Sebastin SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plastic and reconstructive surgery. 2011 Sep;128(3):723–737. doi: 10.1097/PRS.0b013e318221dc83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fufa D, Calfee R, Wall L, Zeng W, Goldfarb C. Digit replantation: experience of two U.S. academic level-I trauma centers. The Journal of bone and joint surgery. American volume. 2013 Dec 4;95(23):2127–2134. doi: 10.2106/JBJS.L.01219. [DOI] [PubMed] [Google Scholar]
- 26.Trybus M, Lorkowski J, Brongel L, Hľadki W. Causes and consequences of hand injuries. The American journal of surgery. 2006;192(1):52–57. doi: 10.1016/j.amjsurg.2005.10.055. [DOI] [PubMed] [Google Scholar]
- 27.De Putter C, Selles R, Polinder S, Panneman M, Hovius S, van Beeck EF. Economic impact of hand and wrist injuries: health-care costs and productivity costs in a population-based study. The Journal of Bone & Joint Surgery. 2012;94(9):e56. doi: 10.2106/JBJS.K.00561. [DOI] [PubMed] [Google Scholar]
- 28.Boulas HJ. Amputations of the fingers and hand: indications for replantation. J Am Acad Orthop Surg. 1998 Mar-Apr;6(2):100–105. doi: 10.5435/00124635-199803000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Davis Sears E, Chung KC. Replantation of finger avulsion injuries: a systematic review of survival and functional outcomes. J Hand Surg Am. 2011 Apr;36(4):686–694. doi: 10.1016/j.jhsa.2010.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chung KC, Kowalski CP, Walters MR. Finger replantation in the United States: rates and resource use from the 1996 Healthcare Cost and Utilization Project. J Hand Surg Am. 2000 Nov;25(6):1038–1042. doi: 10.1053/jhsu.2000.16356. [DOI] [PubMed] [Google Scholar]
- 31.Potini VC, Bratchenko W, Jacob G, Chen L, Tan V. Repeat Emergency Room Visits for Hand and Wrist Injuries. J Hand Surg Am. 2014;39(4):752–756. doi: 10.1016/j.jhsa.2014.01.019. [DOI] [PubMed] [Google Scholar]
- 32.Hartzell TL, Kuo P, Eberlin KR, Winograd JM, Day CS. The overutilization of resources in patients with acute upper extremity trauma and infection. J Hand Surg Am. 2013;38(4):766–773. doi: 10.1016/j.jhsa.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 33.Peterson BC, Mangiapani D, Kellogg R, Leversedge FJ. Hand and microvascular replantation call availability study: a national real-time survey of level-I and level-II trauma centers. J Bone Joint Surg Am. 2012 Dec 19;94(24):e185. doi: 10.2106/JBJS.K.01167. [DOI] [PubMed] [Google Scholar]
- 34.Richards WT, Barber MK, Richards WA, Mozingo DW. Hand injuries in the state of Florida, are centers of excellence needed? Journal of Trauma and Acute Care Surgery. 2010;68(6):1480–1490. doi: 10.1097/TA.0b013e3181bb8c70. [DOI] [PubMed] [Google Scholar]
- 35.Soucacos P. Indications and selection for digital amputation and replantation. Journal of Hand Surgery (British and European Volume) 2001;26(6):572–581. doi: 10.1054/jhsb.2001.0595. [DOI] [PubMed] [Google Scholar]
- 36.Durazzo TS, Frencher S, Gusberg R. Influence of race on the management of lower extremity ischemia: revascularization vs amputation. JAMA surgery. 2013 Jul;148(7):617–623. doi: 10.1001/jamasurg.2013.1436. [DOI] [PubMed] [Google Scholar]
- 37.Huber TS, Wang JG, Wheeler KG, et al. Impact of race on the treatment for peripheral arterial occlusive disease. Journal of vascular surgery. 1999 Sep;30(3):417–425. doi: 10.1016/s0741-5214(99)70068-6. [DOI] [PubMed] [Google Scholar]
- 38.Wilson MG, May DS, Kelly JJ. Racial differences in the use of total knee arthroplasty for osteoarthritis among older Americans. Ethnicity & disease. 1994 Winter;4(1):57–67. [PubMed] [Google Scholar]
- 39.Giacomini MK. Gender and ethnic differences in hospital-based procedure utilization in California. Archives of internal medicine. 1996 Jun 10;156(11):1217–1224. [PubMed] [Google Scholar]
- 40.Ayanian JZ, Cleary PD, Keogh JH, Noonan SJ, David-Kasdan JA, Epstein AM. Physicians' beliefs about racial differences in referral for renal transplantation. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2004 Feb;43(2):350–357. doi: 10.1053/j.ajkd.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 41.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. Jama. 1993 May 26;269(20):2642–2646. [PubMed] [Google Scholar]
- 42.Eslami MH, Zayaruzny M, Fitzgerald GA. The adverse effects of race, insurance status, and low income on the rate of amputation in patients presenting with lower extremity ischemia. Journal of vascular surgery. 2007 Jan;45(1):55–59. doi: 10.1016/j.jvs.2006.09.044. [DOI] [PubMed] [Google Scholar]
- 43.Squitieri L, Reichert H, Kim HM, Steggerda J, Chung KC. Patterns of surgical care and health disparities of treating pediatric finger amputation injuries in the United States. Journal of the American College of Surgeons. 2011 Oct;213(4):475–485. doi: 10.1016/j.jamcollsurg.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 44.Shale CM, Tidwell JE, 3rd, Mulligan RP, Jupiter DC, Mahabir RC. A nationwide review of the treatment patterns of traumatic thumb amputations. Annals of plastic surgery. 2013 Jun;70(6):647–651. doi: 10.1097/SAP.0b013e31828986c9. [DOI] [PubMed] [Google Scholar]
- 45.Institute of Medicine (IOM) Emergency Medical Services at the Crossroads. Washington, DC: National Academy Press; 2006. [Google Scholar]
- 46.Mueller MA, Zaydfudim V, Sexton KW, Shack RB, Thayer WP. Lack of emergency hand surgery: discrepancy between elective and emergency hand care. Annals of plastic surgery. 2012 May;68(5):513–517. doi: 10.1097/SAP.0b013e31823b6a35. [DOI] [PubMed] [Google Scholar]
- 47.MacKenzie EJ, Hoyt DB, Sacra JC, et al. National inventory of hospital trauma centers. Jama. 2003;289(12):1515–1522. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 48.Mackersie RC. History of trauma field triage development and the american college of surgeons criteria. Prehospital Emergency Care. 2006;10(3):287–294. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 49.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. The New England journal of medicine. 2006 Jan 26;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 50.Mohan D, Rosengart MR, Farris C, Cohen E, Angus DC, Barnato AE. Assessing the feasibility of the American College of Surgeons' benchmarks for the triage of trauma patients. Arch Surg. 2011;146(7):786–792. doi: 10.1001/archsurg.2011.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.