Abstract
Chronic obstructive pulmonary disease (COPD) patients are at higher risk of developing lung cancer and its metastasis, but no suitable biomarker has been reported for differential diagnosis of these patients. Levels of serum biomarkers (VEGF, IL-8, MMP-9 and MMP-2) were analyzed in these patients, which were compared with healthy donors (HD). Levels of VEGF (P < 0.005) and MMP-9 (P < 0.05) were significantly higher in COPD patients than HD. Compared to HD, a decrease in IL-8 (~8.1 folds; P < 0.0001) but an increase in MMP-9 (~1.6 folds; P < 0.05) levels were observed in the lung cancer patients. Cancer patients showed significantly (P < 0.005) lower levels of serum VEGF (1.9 folds) and IL-8 (~9 folds) than the COPD patients. VEGF level was significantly higher (2.6 folds; P < 0.0005) in metastatic than non-metastatic cancer patients. However, MMP-2 didn’t show significant variation in these patients. The Youden’s index (YI) values for lung cancer diagnosis in HD using IL-8 was 0.55 with 83.3% overall accuracy. VEGF was able to diagnose COPD in HD with better YI (0.38) and overall accuracy (70.6%). IL-8 was able to diagnose cancer in COPD patients and HD with YI values of 0.35, 0.55 with 71% and 83.3% overall accuracy, respectively.
According to World Health Organization Report (2012) chronic obstructive pulmonary disease (COPD) and lung cancer are the most rapidly growing diseases globally and fall within the top 10 causes of death. COPD is the third and lung cancer (with trachea and bronchus cancer) is the fourth worldwide health problem with 3.1 and 1.6 million annual deaths, respectively1. Interestingly, COPD and lung cancer are interlinked closely with cause and effect relationship2,3,4. Both the diseases are known to be induced by exposure of toxic gases and air pollutants especially cigarette/tobacco smoke, which initially induce systemic inflammatory changes and subsequently localized chronic inflammation in the lungs. About 8–50% prevalence of COPD is reported in patients diagnosed with lung cancer5, which are mostly associated with obstruction of air passage to lungs due to tumor mass. The association of these two diseases becomes further critical as COPD patients are reported to be at higher risk to develop lung cancer6,7. In a matched case-control study, it was found that ~1% of COPD patients develop lung cancer each year, while only 0.2% of patients with normal pulmonary function develop lung cancer (~5 folds increase in risk of lung cancer)7. According to a recent study, smoking poses almost four folds higher risk of developing lung cancer than non-smoking COPD patients8. It is interesting to note that the histological characteristics of lung cancer developed in COPD patients are different than those developed in non-COPD patients9. Management of lung cancer with COPD condition adds another line of complication as these patients show meager prognosis because of poor pulmonary function and quality of life in these patients5. Moreover, lung cancers developed in COPD patients tended to be at the higher grade of malignancy. The five year survival rate in lung cancer patients with COPD was significantly lower than patients with normal pulmonary function (77% versus 91.6%) due to higher recurrence rate10.
Usually lung cancer is asymptomatic until the disease is already at an advanced stage. Many times, lung cancer symptoms are mistaken with other problems, such as infection or effect of smoking, which further delays the diagnosis. Therefore, majority of lung cancer cases are diagnosed at either stage III or IV, thus making curative surgery difficult for the clinicians. In this direction, chest radiography and sputum cytology had been employed for lung cancer screening in the 1980 s. However, noticeable advantage in terms of decrease in patient mortality due to the screening remains inconclusive11. Even though, low dose computed tomography achieved early detection and increased resectability rates for lung cancer, its mortality benefits have not been proved12. Initial results from National Lung Screening Trail in USA showed 20% fewer lung cancer deaths among trail participants compared with subjects screened by chest radiography13. However, being radiation based and costly technique, routine use of computed tomography for mass screening of patients is rather impractical and unaffordable, especially in developing countries like India. In this direction, the potential of biomarkers (e.g. circulating DNA in peripheral blood, circulating tumor-derived exosome, micro-RNAs, comparative protein profiling) in lung cancer diagnosis has been discussed and reviewed14. Recently, evaluation of VEGF-C and other tumor markers in bronchoalveolar lavage fluid showed ability of neuron-specific enolase for lung cancer diagnosis15. However, serum cytokine based markers to differentially diagnose lung cancer, its metastasis and COPD patients is not known to the best of our knowledge. Compared to other techniques, serum cytokine analysis using ELISA could be better suited for lung cancer screening/diagnosis due to the ease in sample collection with quick and economic way to obtain the results.
Metastasis is a critical clinical factor in the disease management perspective of COPD. A large variety of inflammatory mediators present in the lungs of COPD patients promote the development of lung cancer and subsequent metastasis16,17. In this regard, developing suitable biomarkers for early diagnosis of lung cancer/its metastasis in COPD patients, may help for lung cancer surveillance and hence better management of the disease. In this regard, our previous study in human lung cancer cells (A549) showed role of autocrine cytokines [vascular endothelial growth factor (VEGF), interleukin-8 (IL-8), matrix metallo-protease-2 (MMP-2)] in the process of epithelial-to-mesenchymal transition and associated metastatic features18,19. This study is a further attempt to distinguish lung cancer (metastatic and non-metastatic) and COPD conditions by assaying serum levels of these analytes.
Results
Serum levels of VEGF, IL-8, MMP-9 and MMP-2 in COPD and lung cancer patients
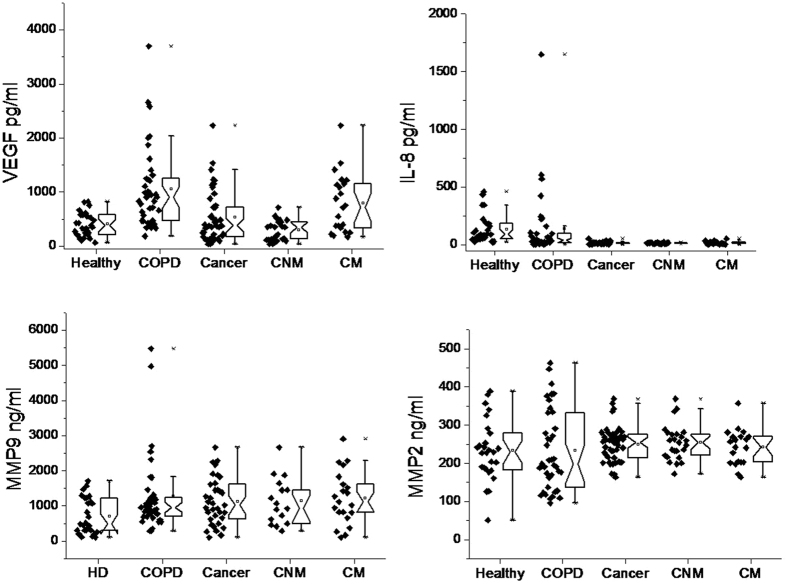
Levels of VEGF, IL-8, matrix metallo-protease-9 (MMP-9) and MMP-2 were measured in serum samples of COPD and lung cancer patients, which were compared with HD (Figs 1 and 2, Table 1). Significantly higher (P < 0.0001) levels of serum VEGF (~2.1 folds; COPD: 1009.2 ± 122.8 pg/ml; HD: 459 ± 45.3 pg/ml) and MMP-9 (1.8 folds; COPD: 1289.6 ± 193.3 ng/ml; HD: 703.6 ± 98.2 ng/ml) were observed in COPD patients than HD. However, changes in the levels of IL-8 and MMP-2 were found to be insignificant between COPD patients and HD. Furthermore, results obtained in lung cancer patients were compared with other groups. Compared to HD, levels of VEGF and MMP-2 were insignificantly changed in lung cancer patients. Interestingly, level of IL-8 was found to be decreased by ~8.1 folds (cancer: 16.5 ± 1.3 pg/ml; HD: 134.4 ± 23.9 pg/ml; P < 0.0001) but MMP-9 level was found to be increased by ~1.6 folds (cancer: 1126.2 ± 112.4 ng/ml; HD: 703.6 ± 98.2 ng/ml; P < 0.05) in lung cancer patients compared to HD. Compared to COPD patients, insignificant change in the levels of MMP-9 and MMP-2 were observed in the serum samples of lung cancer patients. However, the levels of VEGF (1.9 folds; cancer: 528.3 ± 67.9 pg/ml; COPD: 1009.2 ± 122.8 pg/ml) and IL-8 (~9 folds; cancer: 16.5 ± 1.3 pg/ml; COPD: 146.7 ± 50.9 pg/ml) were significantly lower (P < 0.005) in lung cancer patients than COPD patients. Among the cancer patients, level of serum VEGF was significantly higher (2.6 folds, P < 0.0005) in metastatic (792.8 ± 115.7 pg/ml) than non-metastatic (295.6 ± 38.5 pg/ml) patients. Other serum biomarkers showed insignificant difference between non-metastatic and metastatic groups of patients. In the two COPD patients (out of 39), who were incidentally diagnosed with lung cancer metastasis, the levels of these serum biomarkers were determined [VEGF (2658.0, 1013.5 pg/ml), IL-8 (11.8, 23.7 pg/ml), MMP-9 (661.8, 1166.7 ng/ml) and MMP-2 (209.2, 95.7 ng/ml)]. In these patients, except for MMP-2, the levels of other biomarkers (VEGF, IL-8 and MMP-9) followed a close proximity to COPD and lung cancer patients, but clearly differed from HD.
Figure 1. Levels of serum analytes in healthy donors, COPD and lung cancer patients.
*Significantly different to each other at P < 0.05; **significantly different to each other at p < 0.005. HD: healthy donors; COPD: Chronic Obstructive Pulmonary Disease; Cancer: Lung Cancer; CNM: Cancer non-metastatic; and CM: Cancer metastatic.
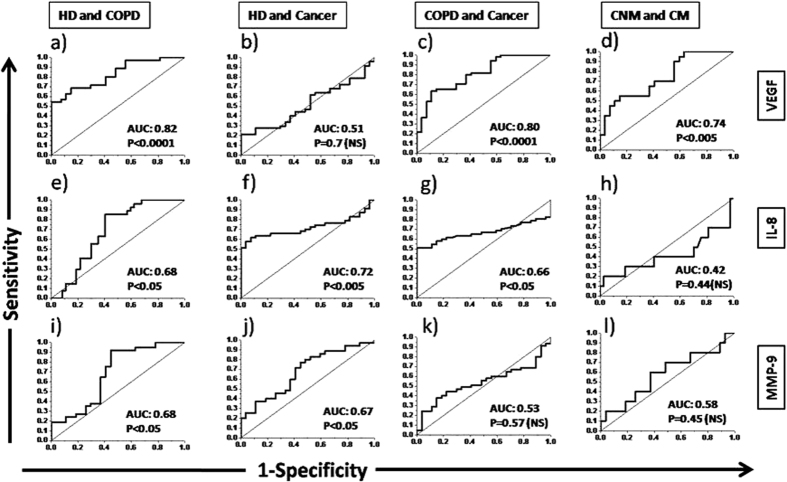
Figure 2. Individual values for different analytes were shown along with respective box-and-whisker plots.
The notched point of plots show the mean value and upper and lower parts represent 25 and 75%, respectively. x: represent lower or upper values of the range. Abbreviations are same as Fig. 1.
Table 1. Serum levels of analytes in various groups.
| Groups | Mean ± SEM Values of Analytes (95% CI of mean) |
|||
|---|---|---|---|---|
| VEGF (pg/ml) | IL-8 (pg/ml) | MMP-9 (ng/ml) | MMP-2 (ng/ml) | |
| HD | 459 ± 45.3(366.3–552.8) | 134.4 ± 23.9(85.1–183.7) | 703.6 ± 98.2(501.6–905.6) | 233.2 ± 15.2(201.9–264.4) |
| COPD | 1009.2 ± 122.8(801.9–1306.5) | 146.7 ± 50.9(41.6–237.9) | 1289.6 ± 193.3(907.4–1649.3) | 237.2 ± 17.2(198.9–266.8) |
| Cancer | 528.3 ± 67.9(391.6–665) | 16.5 ± 1.3(13.9–19.2) | 1126.2 ± 112.4(897.8–1354.7) | 249.4 ± 6.9(235.4–263.4) |
| CNM | 295.6 ± 38.5(216.1–375.1) | 15.5 ± 0.8(13.7–17.2) | 1132.7 ± 166(778.9–1486.5) | 254.6 ± 9.3(235.2–274) |
| CM | 792.8 ± 115.7(552.1–1033.5) | 17.8 ± 2.6(12.2–23.3) | 1225.0 ± 165.8(879–1571.1) | 242.9 ± 10.4(221.1–264.7) |
Diagnostic ability of serum biomarkers for lung cancer, its metastasis and COPD
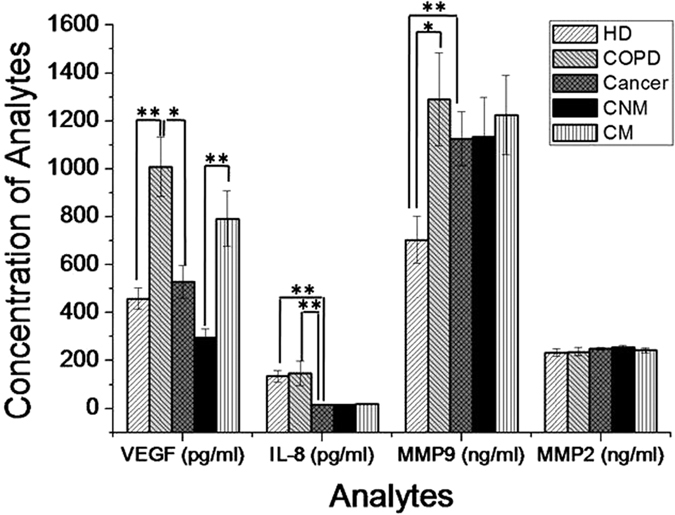
The area under curve (AUC) values for VEGF to diagnose COPD in HD and cancer in COPD patients were found to be 0.82 and 0.80, respectively (Fig. 3). Serum VEGF has also shown good sensitivity to distinguish between metastatic and non-metastatic lung cancer patients (AUC: 0.74). Serum IL-8 showed good sensitivity to diagnose cancer in HD (AUC: 0.72) and cancer in COPD patients (AUC: 0.66). But, IL-8 didn’t show good sensitivity to distinguish between metastatic and non-metastatic lung cancer patients. MMP-9 showed its ability to fairly diagnose COPD (AUC: 0.68) and cancer (AUC: 0.67) in healthy subjects. Other patient groups showed lower AUC values (<0.6) for other analytes suggesting their poor diagnostic ability.
Figure 3. ROC curves of different analytes between various groups.
Abbreviations are same as Fig. 1. NS: Non-significant.
The upper or lower threshold values (mean of 95% CI) for the analytes were determined in different patient groups (COPD and cancer) depending on their increase or decrease in serum compared to HD. On this basis, the upper CI of mean for VEGF and MMP-9 were found to be >552.8 pg/ml and >905.6 ng/ml, respectively, however, the lower CI of mean for IL-8 was <85.1 pg/ml. Based on these cut off values, the diagnostic ability of these analytes were evaluated for calculating the Youden’s index (YI) and the overall accuracy of the test. These values were calculated for VEGF, IL-8 and MMP-9 between four groups i.e. (i) HD and COPD, (ii) HD and cancer, (iii) COPD and cancer and (iv) non-metastatic and metastatic (Table 2). For VEGF, YI values were found to be 0.38 and 0.33 with 70.6% and 65% overall accuracy for diagnosis of COPD in HD and cancer in COPD patients, respectively. However, IL-8 was able to diagnose cancer in COPD patients and HD with YI 0.35, 0.55 and 71%, 83.3% overall accuracy, respectively. For diagnosis of COPD in HD, serum MMP-9 showed YI of 0.21 with overall accuracy 60.3%. Serum MMP-9 showed almost similar ability to diagnose cancer in healthy subjects (YI: 0.17; overall accuracy: 58.1%). The YI and overall accuracy values for VEGF, IL-8 and MMP-9 were found to be very low with poor diagnostic ability for other combination of HD/patients.
Table 2. Youden’s index to diagnose COPD and cancer from healthy donors.
| Analyte at 95% CI of mean | HD versus COPD | HD versus Cancer | COPD versus Cancer | CNM versus CM |
|---|---|---|---|---|
| VEGF >552.8 pg/ml (upper limit) | 0.38 (70.6%) | 0.10 (59.7%) | 0.33 (65%) | 0.28 (63%) |
| IL-8 <85.1 pg/ml (lower limit) | 0.28 (66.2%) | 0.55 (83.3%) | 0.35 (71%) | 0 |
| MMP-9 >905.6 ng/ml (upper limit) | 0.21 (60.3%) | 0.17 (58.1%) | 0.05 (51%) | 0.03 (51.4%) |
Youden’s index (scale of 0–1) was calculated as mentioned in materials and methods. The values in parentheses represent overall accuracy.
Discussion
Previously, our in-vitro study has shown that cytokines (VEGF, IL-8 and MMP-2) secreted from A549 cells result in metastatic features in these cancer cells18,19. To further evaluate the changes of these biomarkers in clinical conditions, levels of these serum markers were monitored in non-metastatic and metastatic lung cancer patients. These results were compared with COPD patients, who are at high risk of developing lung cancer. The important characteristics of COPD is the increased recruitment of inflammatory cells (such as CD8+ T-lymphocytes, neutrophils and macrophages) producing pro-inflammatory cytokines (like VEGF, TNF-α, IL-1, IL-6 and IL-8, IL-17) in the lung tissue20. Moreover, vascular remodeling occurs during COPD pathogenesis21, which involves angiogenesis, bronchial vascularization and structural changes in vascular walls. The increased level of serum VEGF in COPD patients may be associated with these inflammatory and angiogenic changes. Moreover, the level of VEGF has been reported to be differentially modulated depending on the lung condition. In case of chronic bronchitis, VEGF level was found to be increased, however, in case of emphysema it was found to be decreased22 with lower expression of VEGF receptors23. The lower serum level of VEGF in lung cancer patients (than the COPD) could be due to its utilization by proliferating tumor cells and its vasculature, which needs further investigation. In order to metastasize in the distant organs, tumor cells need to degrade basement membrane and gain entry into the systemic circulation through tumor vasculature24,25,26. VEGF secreted by tumor and/or other cells of tumor microenvironment is the key mediator of vasculogenesis, which plays a crucial role in the process of metastasis. These facts support our observation of significantly increased level of VEGF in metastatic than non-metastatic lung cancer patients. MMP-9 has been known to cause emphysema in COPD and angiogenesis/metastasis during lung cancer16, which supports our observation of increased serum levels of MMP-9 in COPD and lung cancer patients. However, we didn’t find significant difference between the levels of serum MMP-9 in metastatic and non-metastatic lung cancer patients. These results are in agreement with recent meta-analysis, where the activity but the not the level of MMP-9 in serum was found to be correlated with lung cancer metastasis27. Moreover, our results also showed increased levels of serum VEGF and MMP-9 in lung cancer patients compared to the healthy donors, which are in agreement with studies showing higher level of these markers in lung cancer patients compared to benign or normal counterparts28,29. Even though, majority of literature suggest increased level of IL-8 in lung cancer patients30,31,32, our results showed decreased IL-8 in serum samples of cancer patients than HD/COPD patients. Our results get supported by study in which human lung cancer cells (A549) clones (3B4) producing low level of IL-8 showed higher proliferation than clones (2B2) producing higher level of IL-833. It is possible that the higher proliferation rate in lung cancer may be associated with the lower level of IL-8 as observed in our study. Our results were also supported by decreased level of serum IL-8 in the COPD patients, who were incidentally diagnosed with lung cancer. Compared to HD, the level of serum MMP-9 was significantly (P < 0.05) increased in case of COPD and lung cancer patients. However, it did not show difference between COPD and lung cancer patients. MMP-2 didn’t show any difference amongst HD, COPD and lung cancer patients, which is not in agreement in change in the level of serum MMP-2 reported in lung cancer patients34,35. In addition, MMP-2 was found to be better prognostic marker in non-small cell lung carcinoma patients than MMP-936. However, our results are in agreement of another study, which showed MMP-9 as better prognostic marker than MMP-2 in patients with mixed types of lung cancer37. A limited literature exists studying the level of MMP-2 in COPD patients, which however were contradictory in terms of increased38 or decreased39 levels in COPD patients compared to healthy subjects. Our results also showed slight decrease in the level of MMP-2 in COPD patients (than HD), which is in agreement with the recent study39. Moreover, this study also showed genetic polymorphism and protein level variation in COPD patients of Mexican population. Even though, such genetic and protein level variation for MMP-2 is not known in the Indian population, its existence may cause higher variability of the biomarker and hence, non-significant changes between various patient groups as observed in our study.
The changes in level of these serum biomarkers were further analysed for their diagnostic ability by plotting the ROC curves (Fig. 3a–c) and calculation of Youden’s Index (Table 2). Ability of MMP-9 and VEGF to diagnose COPD patients in HD was found better (YI: 0.21 and 0.38, AUC: 0.68 and 0.82) than IL-8. Moreover, the ability of serum MMP-9 (AUC: 0.67; P < 0.05) and IL-8 (AUC: 0.72; P < 0.005) to diagnose cancer (from HD) were found to be significant. On the other hand, decrease in IL-8 (YI: 0.35; AUC: 0.66; P < 0.05) and increase in VEGF (YI: 0.33; AUC: 0.80; P < 0.0001) showed significant ability to diagnose cancer in COPD patients. For differential diagnosis between non-metastatic and metastatic patients, VEGF showed better AUC (0.74; P < 0.005) value than other markers. The lower YI (0.28) in this condition seems to be associated with lower sample size. Based on 95% CI of mean, HD can be differentially diagnosed as COPD with serum levels of VEGF (801.9–1306.5 pg/ml) and MMP-9 (907.4–1649.3 ng/ml). However, COPD patients can be diagnosed as lung cancer with serum level of IL-8 (13.9–19.2 pg/ml). Within lung cancer patients, VEGF (552.1–1033.5 pg/ml) can be used to differentially diagnose the metastatic condition. It may also be important to emphasize here that the overall accuracy was found to be high (65–80%) for the serum biomarkers suggesting their significant differential diagnostic ability for lung cancer, its metastasis and COPD. However, further studies are required to evaluate the variation of these biomarkers in COPD patients, who are at high-risk to develop lung cancer. Moreover, a follow up in non-metastatic patients, which may eventually become metastatic, would help to decide the threshold values for these biomarkers for better management of lung cancer patients.
Materials and Methods
Patients and serum collection
COPD patients (n = 39) were from BARC Hospital, Mumbai. Out of them two patients were later diagnosed with lung cancer metastasis and were excluded from the analysis. Serum samples of lung cancer patients (n = 45) were obtained from the depository (stored at liquid nitrogen) at Tata Memorial Hospital, Mumbai. Out of 45 lung cancer patients, 20 patients were diagnosed to be metastatic. Wherever required, analysis of lung cancer patient’s samples was performed either as all lung cancer samples together (cancer) or as non-metastatic (CNM) and metastatic (CM) patient groups. Serum samples from age matched healthy donors (n = 27) were collected from the volunteers, who came for regular checkup at Bhabha Atomic Research Centre Hospital, Mumbai. These patients were non-COPD and without past history of any lung disorder. Details of HD, COPD and lung cancer patients are provided in Table 3. The methods were carried out in accordance with the approved experimental protocols and guidelines of Institutional Ethical Committees at BARC Hospital, Mumbai (HD and COPD patients) and Tata Memorial Hospital, Mumbai (lung cancer patients). Written informed consent was obtained from all the subjects for the collection of samples. Fresh serum samples were isolated from 5 ml blood obtained from COPD and HD, which was stored at −80 °C until use.
Table 3. Details of healthy donors, and COPD and lung cancer patients.
| Parameters | Healthy Donors | COPD | Lung cancer |
|---|---|---|---|
| Number | 27 | 37 | 45 |
| Age (mean ± SD) | 61.1 ± 10.4 | 70.1 ± 10.2 | 56.7 ± 10.6 |
| Gender | |||
| Male | 20 | 19 | 41 |
| Female | 7 | 18 | 4 |
| Lung Cancer Patients Categories | |||
| Non-Metastatic | 25 | ||
| Adenocarcinoma | — | — | 22 |
| Squamous cell carcinoma | — | — | 3 |
| Metastatic | 20 | ||
| Adenocarcinoma | — | — | 15 |
| Squamous cell carcinoma | — | — | 5 |
Enzyme Linked Immunosorbent Assay (ELISA) for VEGF, IL-8, MMP-9 and MMP-2 in serum samples
VEGF, IL-8, MMP-9 and MMP-2 levels in serum samples were quantified using ELISA kits (Quantikine ELISA, R&D Systems, USA) following standard procedure provided along with the kits. For MMP-9, 35 lung cancer serum samples (CNM: 16; CM: 19) were analysed. For other analytes, sample numbers remain the same as mentioned in the previous section (Table 3). Serum samples stored at −80° were thawed to room temperature and where ever required dilutions were made (1:20 for MMP-2 and 1:100 for MMP-9). Assay buffer (100 μl) and serum samples (100 μl for VEGF and MMP-9 and 50 μl for MMP-2 and IL-8) were added to the wells of a micro-titer plate coated with respective human specific VEGF, IL-8, MMP-9 and MMP-2 antibody followed by incubation (2 h; room temperature) on a horizontal orbital micro plate shaker. After incubation, plates were washed with buffer three times for 5 min each. Then 200 μl of respective conjugates (VEGF, IL-8, MMP-9 and MMP-2) were added to respective plates, and then incubated for 2 h at room temperature. Further, 200 μl of substrate solution was added to each well and incubated for 30 min at room temperature in the dark. Finally, after the addition of 50 μl of stop solution, color development was determined at 450 and 540 nm using micro plate reader (Infinite, M-200 PRO, Tecan, Switzerland). Absorbance at 540 nm was subtracted from the reading at 450 nm and analyte concentrations were calculated from the respective standard curves.
Statistical Analysis
Statistical analysis was done using OriginPro 8.0 software. Frequency distribution values of analytes were represented in mean ± SEM. The significance between different groups was evaluated by un-paired t test. To evaluate the diagnostic ability of these analytes, AUC values were determined from receiver operating characteristics (ROC) curves [sensitivity versus (1 − specificity)] for the selected patient groups/analytes. This kind of calculation was made as our data has more number of discrete values on continuous rating scale. AUC curves were prepared for each of the three analytes (i.e. VEGF, IL-8 and MMP-9) between (i) HD and COPD (to diagnose COPD in HD), (ii) HD and cancer (to diagnose cancer in HD), (iii) COPD and cancer (to diagnose cancer in COPD patients) and (iv) non-metastatic and metastatic (to distinguish between metastatic and non-metastatic lung cancer patients). Youden’s index was calculated by determining cut off values either by taking upper or lower 95% CI of mean (depending on the upward/downward trend of the particular analyte) compared to healthy donors. Sensitivity and specificity was calculated based on the number of cases that meet the conditions of lower or higher than the cut off values. Overall accuracy for diagnostic test was calculated as following: (sum of true negatives and true positives)/(sum of true negatives, true positives, false negatives and false positives) × 100.
Additional Information
How to cite this article: Balla, M. M. S. et al. Differential diagnosis of lung cancer, its metastasis and chronic obstructive pulmonary disease based on serum Vegf, Il-8 and MMP-9. Sci. Rep. 6, 36065; doi: 10.1038/srep36065 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Acknowledgments
Sejal Desai would like to acknowledge Department of Atomic Energy Graduate Fellowship Scheme for financial support. Authors would like to thank Mrs Hansa D. Yadav and Dr. J. Malhotra for assisting in the collection of serum samples from BARC hospital.
Footnotes
Author Contributions M.M.S.B. and S.D. conducted the experiments, M.M.S.B., S.D., A.K., P.P., Y.K.S., C.S.P., S.L. and B.N.P. designed the study. M.M.S.B., S.D., A.K., P.B. and B.N.P. analysed the results. M.M.S.B. and B.N.P. wrote and other authors edited the manuscript.
References
- The top 10 causes of death in world in 2012. Fact sheet N°310 published by World Health Organization (WHO), http://www.who.int/mediacentre/factsheets/fs310/en/ Updated May 2014, Last date accessed September 7, 2016.
- Durham A. L. & Adcock I. M. The relationship between COPD and lung cancer. Lung Cancer 90(2), 121 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sekine Y. et al. Early detection of COPD is important for lung cancer surveillance. European Respiratory Journal 39(5), 1230 (2012). [DOI] [PubMed] [Google Scholar]
- Punturieri A. et al. Lung cancer and chronic obstructive pulmonary disease: needs and opportunities for integrated research. Journal of National Cancer Institute 101(8), 554 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurishima K. et al. Lung cancer patients with chronic obstructive pulmonary disease. Oncology Report 8(1), 63 (2001). [PubMed] [Google Scholar]
- de Torres J. P. et al. Lung cancer in patients with chronic obstructive pulmonary disease– incidence and predicting factors. Am J Respir Crit Care Med 184(8), 913 (2011). [DOI] [PubMed] [Google Scholar]
- Skillrud D. M., Offord K. P. & Miller R. D. Higher risk of lung cancer in chronic obstructive pulmonary disease. A prospective, matched, controlled study. Annals of Internal Medicine 105(4), 503 (1986). [DOI] [PubMed] [Google Scholar]
- Huang R. et al. Associated Links Among Smoking, Chronic Obstructive Pulmonary Disease, and Small Cell Lung Cancer: A Pooled Analysis in the International Lung Cancer Consortium. EBioMedicine 2, 1677 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caramori G. et al. Mechanisms involved in lung cancer development in COPD. The International Journal of Biochemistry & Cell Biology 43, 1030 (2011). [DOI] [PubMed] [Google Scholar]
- Sekine Y. et al. Association of chronic obstructive pulmonary disease and tumor recurrence in patients with stage IA lung cancer after complete resection. The Annals of Thoracic Surgery 84(3), 946 (2007). [DOI] [PubMed] [Google Scholar]
- Fontana R. S. et al. Early lung cancer detection: results of the initial (prevalence) radiologic and cytologic screening in the Mayo Clinic study. American Review of Respiratory Disease 130(4), 561 (1984). [DOI] [PubMed] [Google Scholar]
- Infante M. et al. A randomized study of lung cancer screening with spiral computed tomography: three-year results from the DANTE trial. Am J Respir Crit Care Med 180(5), 445 (2009). [DOI] [PubMed] [Google Scholar]
- National Lung Screening Trial (NLST) Initial Results: Fast Facts. National Cancer Institute, http://www.cancer.gov/news-events/press-releases/2011/NLSTFastFacts, Posted: November 4, 2010, Updated: June 29, 2011, Last date accessed September 7, 2016.
- Van’t Westeinde S. C. & van Klaveren R. J. Screening and early detection of lung cancer. Cancer Journal 17(1), 3 (2011). [DOI] [PubMed] [Google Scholar]
- Cao C. et al. Evaluation of VEGF-C and tumor markers in bronchoalveolar lavage fluid for lung cancer diagnosis. Scientific Reports 3, 3473 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- King P. T. Inflammation in chronic obstructive pulmonary disease and its role in cardiovascular disease and lung cancer. Clinical and Translational Medicine 4, 26 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohal S. S. Chronic Obstructive Pulmonary Disease (COPD) and Lung Cancer: Epithelial Mesenchymal Transition (EMT), the Missing Link? EBioMedicine 2(11), 1578 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai S., Kumar A., Laskar S. & Pandey B. N. Cytokine profile of conditioned medium from human tumor cell lines after acute and fractionated doses of gamma radiation and its effect on survival of bystander tumor cells. Cytokine 61(1), 54 (2013). [DOI] [PubMed] [Google Scholar]
- Desai S., Laskar S. & Pandey B. N. Autocrine IL-8 and VEGF mediate epithelial-mesenchymal transition and invasiveness via p38/JNK-ATF-2 signalling in A549 lung cancer cells. Cell Signal 25(9), 1780 (2013). [DOI] [PubMed] [Google Scholar]
- Cosio M. G., Saetta M. & Agusti A. Immunologic aspects of chronic obstructive pulmonary disease. The New England Journal of Medicine 360(23), 2445 (2009). [DOI] [PubMed] [Google Scholar]
- Harkness L. M. et al. Pulmonary vascular changes in asthma and COPD. Pulmonary Pharmacology and Therapeutics 29(2), 144 (2014). [DOI] [PubMed] [Google Scholar]
- Kanazawa H., Asai K., Hirata K. & Yoshikawa J., Possible effects of vascular endothelial growth factor in the pathogenesis of chronic obstructive pulmonary disease. The American Journal of Medicine 114(5), 354 (2003). [DOI] [PubMed] [Google Scholar]
- Santos S. et al. Enhanced expression of vascular endothelial growth factor in pulmonary arteries of smokers and patients with moderate chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine 167(9), 1250 (2003). [DOI] [PubMed] [Google Scholar]
- Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med 285(21), 1182 (1971). [DOI] [PubMed] [Google Scholar]
- Kessenbrock K., Plaks V. & Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141(1), 52 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coussens L. M. & Werb Z. Inflammation and cancer. Nature 420(6917), 860 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong L. et al. Prognostic impact of serum and tissue MMP-9 in non-small cell lung cancer: a systematic review and meta-analysis. Oncotarget 7(14), 18458 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng D., Kong H. & Li Y., Prognostic values of VEGF and IL-8 in malignant pleural effusion in patients with lung cancer. Biomarkers 18(5), 386 (2013). [DOI] [PubMed] [Google Scholar]
- Zhang Y. et al. Detection of circulating vascular endothelial growth factor and matrix metalloproteinase-9 in non-small cell lung cancer using Luminex multiplex technology. Oncology Letters 7(2), 499 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng D., Kong H. & Li Y. Prognostic values of VEGF and IL-8 in malignant pleural effusion in patients with lung cancer. Biomarkers 18(5), 386 (2013). [DOI] [PubMed] [Google Scholar]
- Millar H. J. et al. Circulating human interleukin-8 as an indicator of cancer progression in a nude rat orthotopic human non-small cell lung carcinoma model. Cancer Epidemiol Biomarkers Prev 17(8), 2180 (2008). [DOI] [PubMed] [Google Scholar]
- Song X. Y. et al. Research on the relationship between serum levels of inflammatory cytokines and non-small cell lung cancer. Asian Pac J Cancer Prev 14(8), 4765 (2013). [DOI] [PubMed] [Google Scholar]
- Wang J. et al. Interleukin-8 inhibits non-small cell lung cancer proliferation: a possible role for regulation of tumor growth by autocrine and paracrine pathways. Journal of Interferon and Cytokine Research 16(1), 53 (1996). [DOI] [PubMed] [Google Scholar]
- Farlow E. C. et al. A multi-analyte serum test for the detection of non-small cell lung cancer. British Journal of Cancer 103(8), 1221 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanoh Y., Abe T., Masuda N. & Akahoshi T. Progression of non-small cell lung cancer: diagnostic and prognostic utility of matrix metalloproteinase-2, C-reactive protein and serum amyloid A. Oncology Reports 29(2), 469 (2013). [DOI] [PubMed] [Google Scholar]
- Guo C. B. et al. Relationship between matrix metalloproteinase 2 and lung cancer progression. Mol Diagn Ther 11(3), 183 (2007). [DOI] [PubMed] [Google Scholar]
- Ylisirniö S., Höyhtyä M. & Turpeenniemi-Hujanen T. Serum matrix metalloproteinases -2, -9 and tissue inhibitors of metalloproteinases -1, -2 in lung cancer--TIMP-1 as a prognostic marker. Anticancer Research 20(2B), 1311 (2000). [PubMed] [Google Scholar]
- Navratilova Z. et al. Simultaneous up-regulation of matrix metalloproteinases 1, 2, 3, 7, 8, 9 and tissue inhibitors of metalloproteinases 1, 4 in serum of patients with chronic obstructive pulmonary disease. Respirology 17(6), 1006 (2012). [DOI] [PubMed] [Google Scholar]
- Hernández-Montoya J. et al. Genetic polymorphisms of matrix metalloproteinases and protein levels in chronic obstructive pulmonary disease in a Mexican population. Biomarkers in Medicine 9(10), 979 (2015). [DOI] [PubMed] [Google Scholar]