Abstract
The patellofemoral joint is a joint that can be an area of concern for athletes of various sports and ages. The joint is somewhat complex with multiple contact points and numerous tissues that attach to the patella. Joint forces are variable and depend on the degree of knee flexion and whether the foot is in contact with the ground. The sports medicine specialist must have a good working knowledge of the anatomy and biomechanics of the patellofemoral joint in order to treat it effectively.
Keywords: Anatomy, biomechanics, patella
INTRODUCTION
Patellofemoral joint pain (PFP) is one of the most common conditions presented to the sports physical therapist.1 Disorders of this articulation are found in a variety of active individuals including runners,2 tennis players,3 and military personnel.4 Females tend to report more patellofemoral pain due to numerous speculations for this reason.5-8
One of the most common contributory factors causing PFP is biomechanical dysfunction.5 The patella and trochlea articulation is variable and for some individuals the patella does not fit well.9 Also, the patellofemoral joint requires an intricate balance of the soft tissue structures that surround the joint. Unequal pull from one set of structures can cause increased force distribution between the patella and femur leading to pain.10-12 To treat PFP effectively, it is imperative that the clinician understand the anatomy and biomechanics of this joint.13 The purpose of this clinical commentary is to provide the reader with a thorough understanding of anatomy and biomechanics of the patellofemoral joint.
FUNCTIONAL ANATOMY
Osseous Structure/cartilage
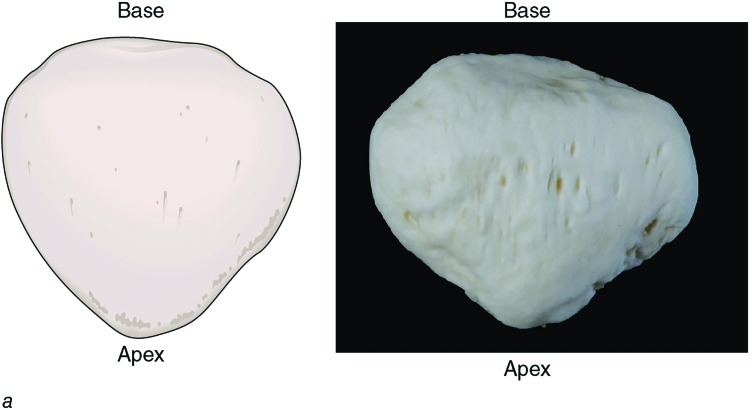
The patellofemoral joint is a diarthrodial plane joint that consists of the posterior surface of the patella and the trochlear surface of the distal anterior femur. The patella is the largest sesamoid bone in the body. Geometrically, the patella is shaped like an upside-down triangle that sits distal to the muscle bulk of the quadriceps that forms the patellar tendon. The superior surface is referred to as the base and the inferior patella is the apex (Figure 1). The peak dimensions of the average patella are 4 - 4.5 centimeters in length, 5 -5.5 centimeters in width and 2 - 2.5 centimeters thick.14,15
Figure 1.
Anterior view of the patella (14.4a in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
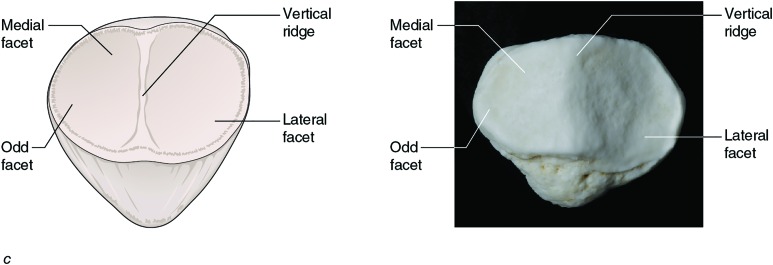
The patella is composed of a thin cortical shell with a trabecular core. The anterior surface of the patella is convex in both anterior-posterior, and medial-lateral planes. The posterior surface of the patella is divided into a variety of facets (Figure 2). A major vertical ridge divides this surface into a medial and lateral half. The two halves can be further divided into seven facets, three horizontal pairs: proximal, middle, and distally and an odd facet that is located on the far medial, posterior aspect of patella. The patellar facets are convex in shape in order to accommodate the concave femoral surface with the lateral side wider to help maintain patellar position. The majority of the articulating surface of the patella is covered with a thick layer of articular cartilage, up to seven millimeters.16 This thick cartilage is thought to dissipate large joint reaction forces that are created during forceful contractions of the quadriceps muscle.
Figure 2.
Posterior view of the patella (14.4c in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
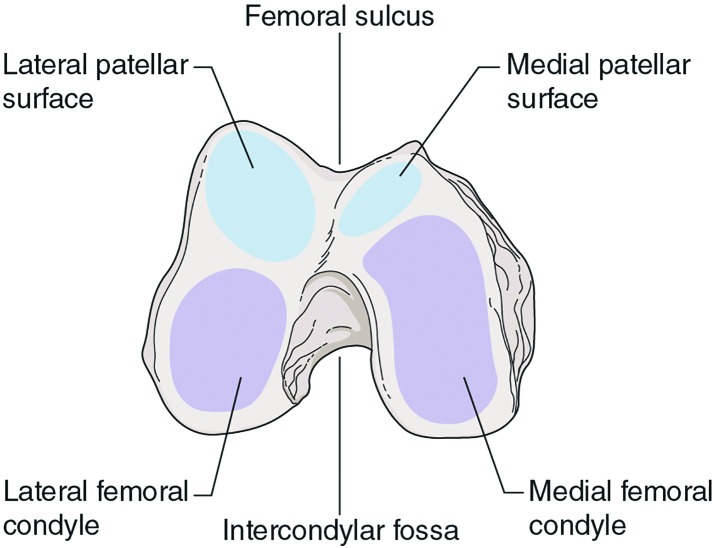
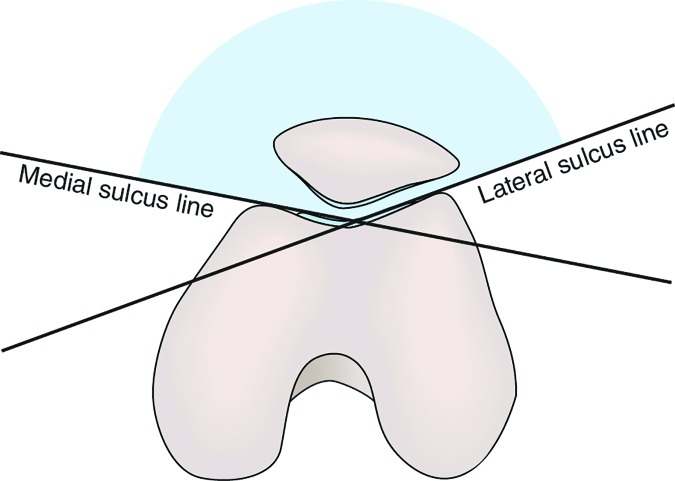
The distal femur forms into an inverted U-shaped intercondylar groove (or trochlear sulcus) with concave lateral and medical facets covered by a thin layer of articular cartilage (Figure 3). As with the patella, the lateral facet of the femur is larger and extends more proximally to provide a bony buttress to improve patellar stability. A sulcus angle can be identified with radiograph (skyline view) that measures the angle between the lateral and medial femoral condyle (Figure 4). Normally, this angle averages around 138 ± 6 degrees.16 A greater angle would indicate trochlear dysplasia (less depth of the trochlea) and a tendency for patellar subluxation.
Figure 3.
The distal femur and articulating surface with the patella (14.2 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
Figure 4.
Sulcus Angle – (25.5 in Reiman – Orthopedic Clinical Exam) © Human Kinetics
Soft tissue
Due to the shallow and incongruent fit between the patella and the trochlea, the stability of the patellofemoral joint is dependent on the static and dynamic soft tissue structures.15 Static stability is offered by the patellar tendon, joint capsule, and ligamentous structures. The medial structures become important in minimizing lateral translation and the primary structure to lateral restraint is the medial patellofemoral ligament (MPFL) This ligament runs from the adductor tubercle to the medial border of patella. Desio et al. describe the MPFL as providing 60% total restraint at 20 degrees of knee flexion.15,17 A secondary restraint includes the medial mensicopatellar ligament which originates from the anterior aspect of the menisci and inserts into the inferior 1/3 of patella and the medial retinaculum with superficial fibers that interdigitate with the medial collateral ligament and the medial patellar tendon.17
On the lateral side of the patellofemoral joint, the following structures aide in stability: lateral patellofemoral ligament, joint capsule, iliotibial band (ITB), and lateral retinaculum. The lateral retinaculum consists of a thinner superficial layer that extends from the ITB to the patella and quadriceps expansion and a thicker deep layer that interdigitates with the vastus lateralis, patellofemoral ligament, and patellotibial ligament.18 The joint must rely on the medial and lateral retinaculum and joint capsule at angles less than 20-30 degrees of flexion because there is minimal to no bony stability.
Dynamically, the contractile structure of the quadriceps, pes anserine muscle group, and biceps femoris muscle help to maintain patellar alignment. The importance of the vastus medialis oblique (VMO) has been discussed extensively in the literature.18-20 The VMO attaches to the mid-portion of patella, the MPFL and adductor magnus tendon. Its more oblique alignment (as compared to the vastus medialis longus) provides mechanical advantage to promote medial stabilizing force to the patella.21,22 The rectus femoris inserts on the anterior portion of superior aspect of patella22. The vastus intermedius inserts posteriorly at the base of patella. The vastus lateralis provides lateral dynamic reinforcement in conjunction with the ITB and the superficial oblique retinaculum.23 Tightness in the ITB can cause the patella to glide and/or tilt laterally. Inferiorly, the patella is secured via the patellar tendon and its attachment to the tibial tubercle.
KINESIOLOGY/BIOMECHANICS
Function
The function of the patella is multifaceted. Its primary purpose is to serve as a mechanical pulley for the quadriceps as the patella changes the direction of the extension force throughout knee range of motion. Its contribution increases with progressive extension. According to Huberti and Hayes the patella is critical in the last 30 degrees of knee extension.24 At full knee extension the patella provides 31% of total knee extension torque, while between 90 and 120 degrees of flexion it provides only 13%. Additionally, the patella acts as a bony shield for the anterior trochlea and due to its interposed position between the quadriceps tendon and femur it prevents excessive friction between the quadriceps tendon and the femoral condyles.25,26
Static Alignment
The static alignment of patella is related to the depth of the femoral sulcus, height of the lateral femoral condyle wall, and the shape of patella. Typically, gross alignment is assessed with the patient in a supine position. McConnell27 has established assessment criteria; however the inter-reliability of this method has been questioned28. For the clinician, observational analysis of obvious abnormalities remains clinically useful but is subjective and cannot be easily quantified.
When observing in the frontal plane with the knee in full extension the patella typically sits midway between the two condyles, although some sources suggest a slight lateral deviation.12 In this position, the patella is superior to the trochlea and minimal contact exists between the patella and femur, thus, in this position the patella is most mobile. Clinically, the Q-angle is commonly used to identify alignment of the quadriceps muscle pull. The Q-angle is the angle between the line of pull of the quadriceps (anterior superior iliac spine to mid-patella) and a line connecting the center of patella with tibial tuberosity (Figure 5). Normal Q-angle for males is 10-13 degrees and 15-17 degrees for females. An increased Q-angle is thought to create excessive lateral forces on the patella through a bowstring effect.10,16 Recently, studies have shown no association between the static Q-angle and patellofemoral kinematics or pain.29,30 Therefore the best way to assess Q-angle is during dynamic active function using video analysis.31
Figure 5.
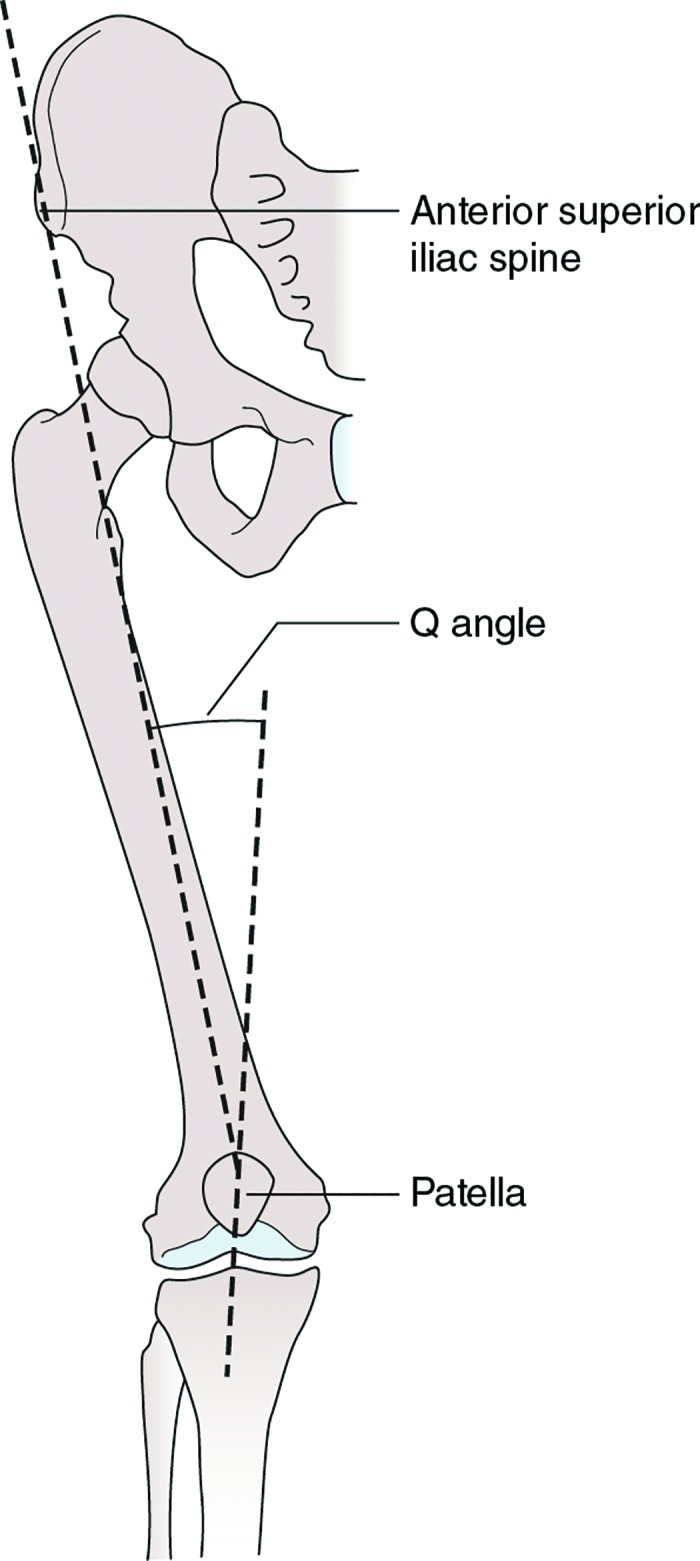
Quadriceps Angle (Q-angle) (Figure 14.9 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
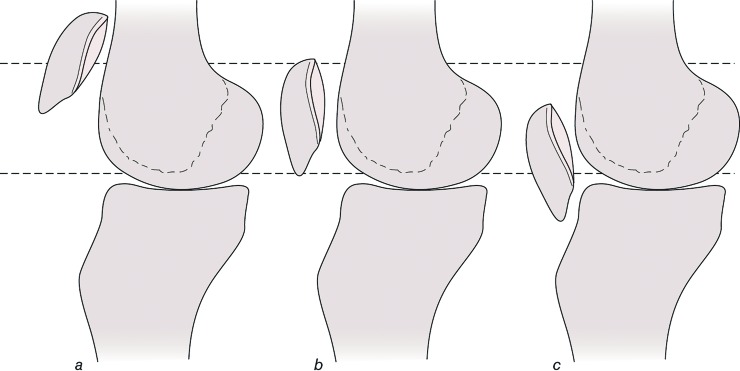
In the sagittal plane with the knee in slight flexion, the apex of the patella rest just at or slightly proximal to the joint line. A more sophisticated method to measure sagittal plane patellar position is the Insall-Salvati ratio.32 This measurement is the ratio of the patellar tendon length compared to the patellar height with the knee bent to around 30 degrees. A ratio of around 1.0 is considered normal. A ratio less than 0.80 is indicative of an inferior patella or “patellar baja” that may be due to a shortened patellar tendon. A ratio greater than 1.2 is termed “patella alta” (Figure 6). In this more superior position it takes longer for the patella to reach the bony constraint of the femoral trochlea, thus the patella is at a greater risk for subluxation.
Figure 6.
Patellar reference positions (Figure 14.15 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
Additionally, the patella should be lined up so that the superior and inferior borders are equidistant from the femur. If any surface of the patella deviates either anterior or posterior this is termed “tilt”. In the sagittal plane, these motions are described by the location of the inferior pole of the patella in either a depressed (inferior tilt) or elevated (superior tilt) position (Figure 7). An inferiorly tilted patella can be problematic as it may pinch or irritate the patellar fat pad that lay underneath the patellar tendon.
Figure 7.
Inferior tilted patella (Figure 14.14 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
In the transverse plane, the patella should lie horizontally such that the medial and lateral borders are equidistant from the femur. A lateral tilt, when the medial border is higher than the lateral border, can lead to lateral patellofemoral compression syndrome (Figure 8).4
Figure 8.
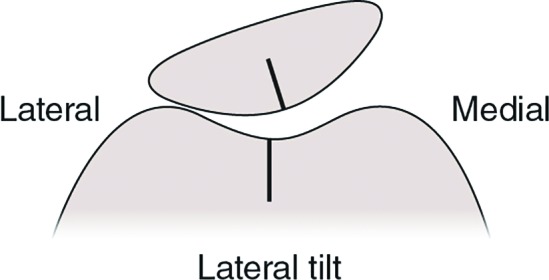
Lateral tilted patella (Figure 14.14 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
Rotation of the patella occurs around an anterior – posterior axis and is described by the direction of the inferior pole of the patella. A lateral rotation occurs when the inferior pole is directed toward the lateral side of the knee, while a medial rotation occurs when the inferior pole is directed medially (Figure 9). This rotational position may indicate underlying torsion of the tibia such as lateral tibial torsion.
Figure 9.
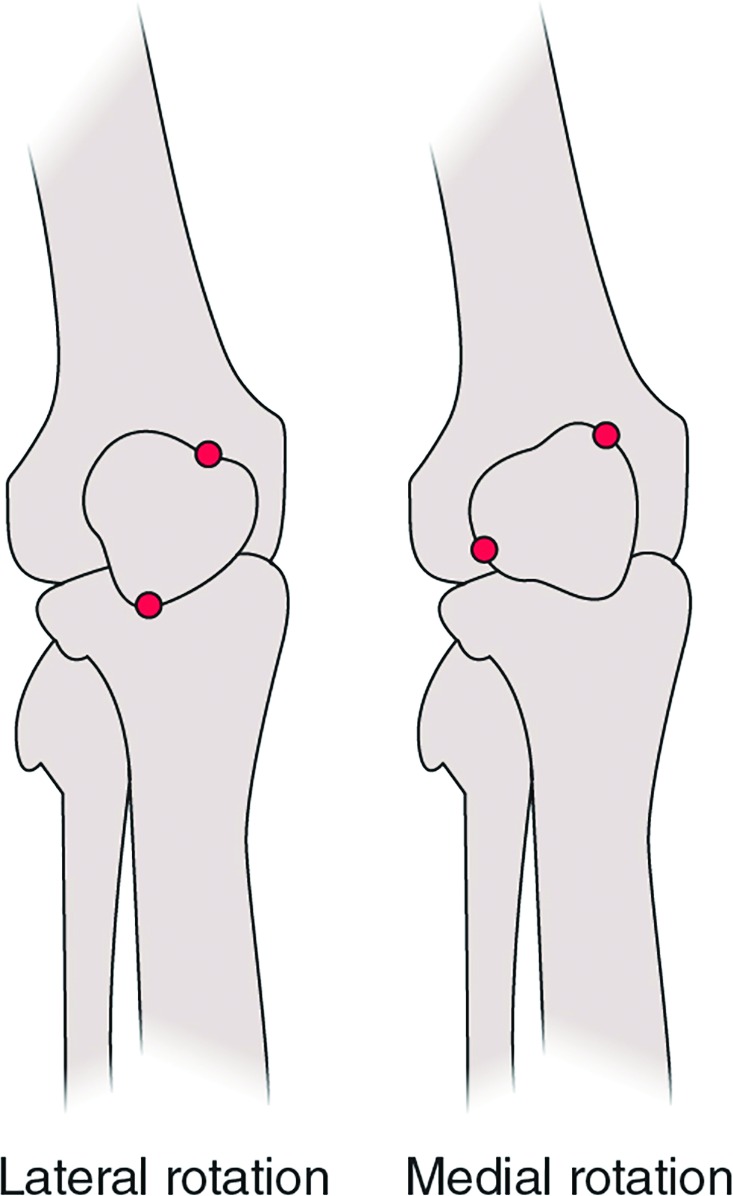
Lateral and medial rotation of the patella (Figure 14.14 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
DYNAMIC MOVEMENT/KINEMATICS
More important than assessing static alignment is for the clinician to understand the dynamic movement of the patella, commonly referred to as patellar tracking. Movement of the patella during tibiofemoral motion is dependent upon the active contraction of the quadriceps, the extensibility of the connective tissue about the patella, and the geometry of the patella and trochlear groove. As a gliding joint, the patella has movement in multiple planes. These motions include superior/inferior glide, medial and lateral glide, medial and lateral tilt, and medial and lateral rotation. Superior glide is also termed patellar extension and this motion occurs during tibiofemoral extension when the quadriceps contract creating a superior pull on the patella. An inferior glide is patellar flexion and occurs in conjunction with tibiofemoral flexion. Lateral and medial glide occur as translations in the frontal plane that correspond with tibiofemoral motion. During lateral glide the lateral edge of the patella moves closer to the lateral side of the knee (Figure 10), and during medial glide the medial side moves toward the medial edge of the knee. Tilt occurs about a longitudinal axis. Tilts are described by which direction the reference facet is moving. In a medial tilt, the medial posterior facet moves closer to the medial femoral condyle, while a lateral tilt is movement of the lateral posterior patellar facet moving closer toward the lateral femoral condyle.
Figure 10.
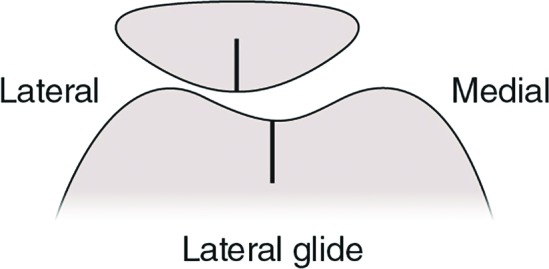
Lateral glide of patella during knee motion (Figure 14.14 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
Open chain
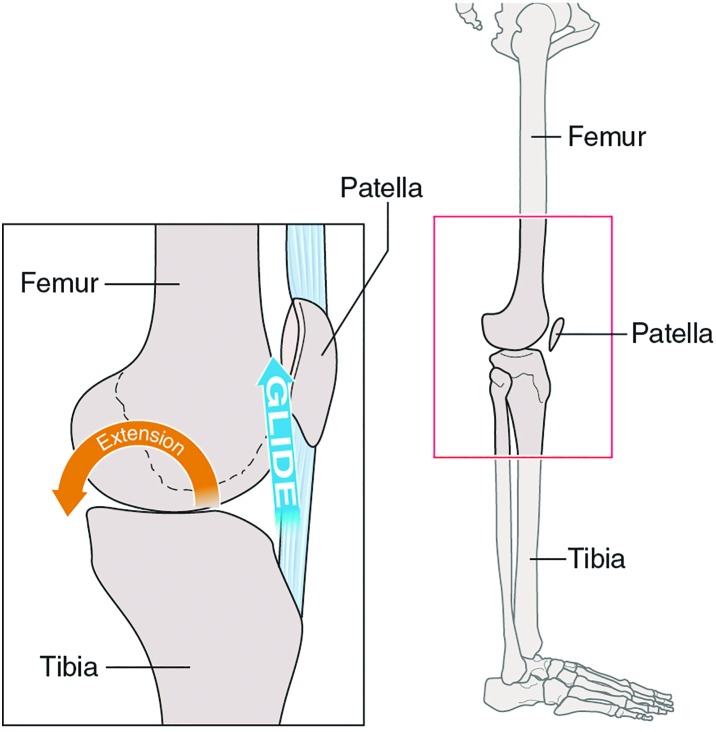
During open chain knee motion, the patella follows the path of the tibia due to the distal insertion of the patellar tendon to the tibial tubercle. The patella glides inferiorly with knee flexion and superiorly with knee extension (Figure 11). With a quadriceps set the patella should migrate approximately 10 mm superiorly.32
Figure 11.
Open chain patellar motion with knee extension (superior glide) and knee flexion (inferior glide) (Figure 14.13 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
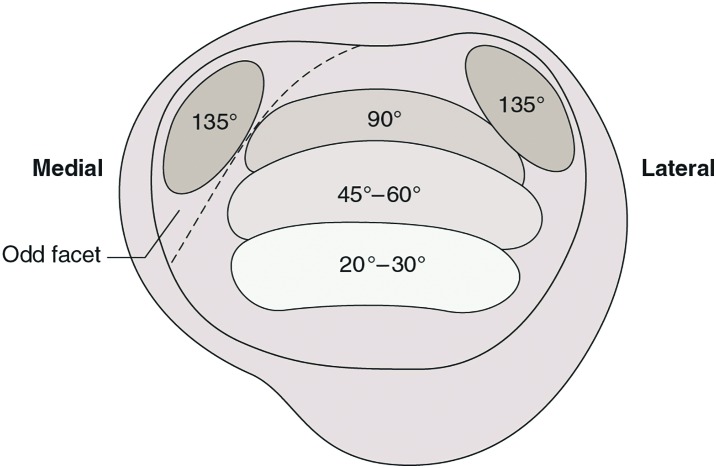
As the knee flexes, the articulating surface of the patella changes throughout the range of knee motion. The contact point moves proximally along the patella and inferior-posterior along the femoral condyles (Figure 12). The overall pattern of patellar contact area increases with increasing knee flexion, which serves to distribute joint forces over a greater surface area. In those with normally aligned patellofemoral joints, this distribution of force allows the knee to resist the deleterious effects that could occur from routine exposure to high compressive forces.
Figure 12.
Patellar contact points during knee motion. (Figure 14.16 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
Several references report that in full knee extension, the patella lies just proximal to the trochlea of the femur, resting on the suprapatellar fat pad and suprapatellar synovium.15,16,25,26 Contrary results by Powers et al. indicate that there is contact of the patella and the trochlea at full knee extension.33 Nevertheless, the trochlear groove is shallow at this point resulting in compromised stability of the patella and there is a greater potential for instability at this position.
As the knee begins to flex, the inferior aspect of the patella contacts the uppermost portion of the femoral condyles. This contact begins between the lateral femoral condyle and the lateral facet of the patella, but by 30 degrees the contact is evenly distributed on both sides of the condyles and the total contact area has been estimated to be approximately 2.0cm2. The contact area initially is small and gradually increases as the joint become more congruent. At 60 degrees of knee flexion, the superior half of the patella contacts part of the femoral groove slightly inferior to the contact area at 30 degrees. The contact area gradually increases as the joint becomes more congruent. The contact area continues to increase as the knee flexes to 90 degrees and is estimated to be 6.0cm2. At this point, the superior portion of patella is contacting an area of the femoral groove just above the notch.
After 90 degrees and until 120 degreed of knee flexion the superior aspect of the patella contacts the area of the femoral groove immediately surrounding the intercondylar notch. In deep flexion the patella actually bridges the span of the intercondylar notch and there is only contact on the far medial and lateral edges of the patella.34 At full flexion, the odd facet is the only articulating contact between the patella and the lateral surface of medial femoral condyle.
Besides the superior and inferior motion of the patella, it also tracks lateral-medial-lateral during tibiofemoral extension to flexion.16 In the normal knee little excessive medial or lateral motion occurs during flexion as the patella remains relatively centered on the trochlea. It is important to note that in full knee extension the patella sits slightly lateral because of the external rotation of the tibia. The estimated amount of medial and lateral displacement is about 3 mm in each direction. As the knee flexes, the patella glides medially and centers itself within the trochlear groove. During knee extension from 45 degrees to 0 the patella tilts medially 5–7 degrees from a laterally tilted position related to the geometry of the femoral trochlear groove.35 At around 30 degrees of flexion the patella glides back towards the lateral side where it maintains this lateralization for the remaining knee flexion. The motion has been described as a C-curve pattern.26
In normals, the patella may be tilted laterally (lateral side down) when the knee is in extension and in earlv flexion, but this tilt is slight and considered “reducible” (the lateral border can easily be lifted off the lateral femoral condvle to make the patella horizontal).
Closed Chain
In closed kinetic chain movements the patella is relatively tethered within the quadriceps tendon so as the femur rotates in the transverse plane, it is the femoral surface that glides behind the patella.12 With excessive femoral internal rotation, the lateral facet of the patella approximates to the lateral anterior femoral condyle.35 Increased hip adduction/internal rotation has been proposed to be a risk factor associated with PFP.36 The frontal plane projection angle has been clinically useful in determining faulty kinematics with individuals with PFP (Figure 13).37
Figure 13.
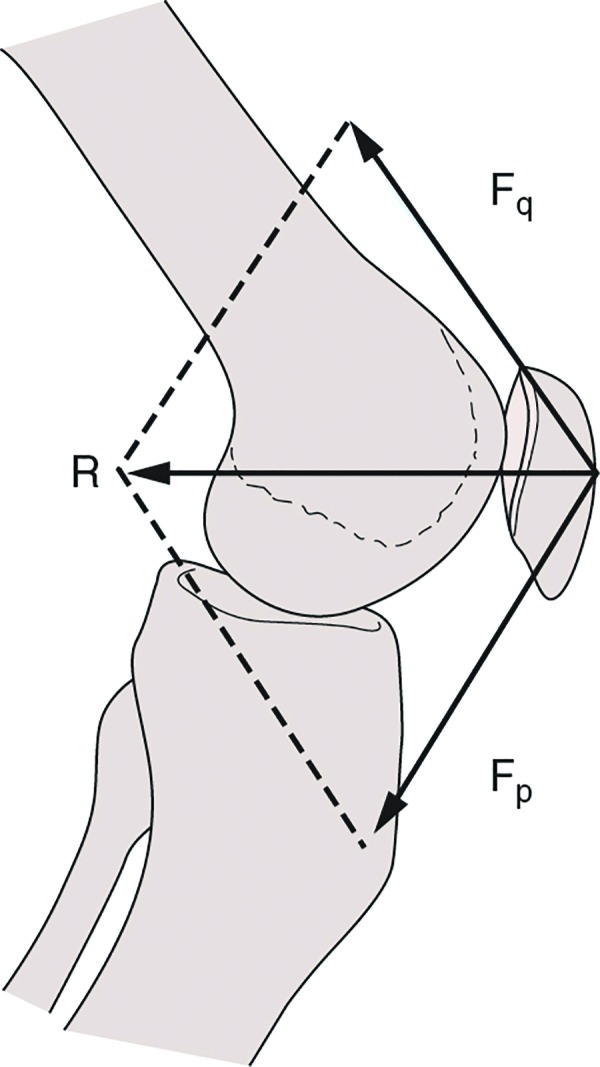
Patellofemoral joint reaction force (Figure 14.17 in Loudon – Clinical Mechanics and Kinesiology) © Human Kinetics
PATELLOFEMORAL JOINT REACTION FORCE (PFJRF)
Patellofemoral joint reaction force (PFJRF) is the resultant compression force acting on the joint and is dependent on knee joint angle and muscle tension (Figure 13).26 The actual stress placed on the patellofemoral joint is the PFJRF divided by the patellofemoral joint contact area and referred to as joint stress measured as force per unit area. The greater the contact area between the patellar surface and femur the less stress is placed on the articular tissue.16 A high PFJRF combined with a small contact area results in high patellofemoral joint stress and may be harmful to the joint cartilage. This stress can be amplified with poor patellar positioning which will be discussed in the next section.
As the contact point changes between the patella and trochlea throughout the range of motion; accordingly, the joint forces change too due to a change in the lever system. In non-weightbearing, the contact area between patella and trochlea increases as the knee flexes from 0-90 degrees and therefore less patellofemoral stress occurs as knee flexion increases. It has been commonly accepted to minimize patellofemoral joint stress open chain exercises should occur from 90 to 30 of knee flexion.
When the foot is fixed, the PFJRF increases from 90 to 45 degrees, then decreases as the knee approaches full extension.16 PFJRF and patellofemoral joint stress can be tremendous during even the simplest of activities of daily living, not to mention with sports and recreational activities.38 Studies have demonstrated forces of 1.3 times body weight (BW) during level ambulation, 3.3 times BW during stair ambulation, 5.6 times BW during running, and up to 7.8 times BW during a deep knee bend or squat.39
CLINICAL APPLICATION
Excessive patellofemoral joint stress appears to be the cause of PFP.3,10 The joint stress can be caused by abnormal anatomy or alignment, abnormal patellar tracking, lower kinetic chain factors, and general overuse.8 The goal of the evaluation is to identify the likely cause of symptoms.
Wiberg has suggested that the shape of the patella as an influencing factor in the development of patellar pain.40 Wiberg devised a classification system based on the articular facet shape of the patella40. However, the various shapes are hard to identify radiographically and may not be as helpful as Wiberg proposed. Different forms of dysplastic patellae are associated with subluxation and dislocation. Examples of dysplastic patellae include alpine hunter's cap, pebble, patella magna, and patella parva. Some individuals have trochlear dysplasia in which the facets are not properly formed. Those who have a smaller lateral trochlea than normal tend to be more prone to lateral dislocations or subluxations of the patellofemoral joint. Beyond anatomy, patellar malalignment (lateralization) causes excessive compressive stress to the lateral patella facets inducing PFP.
Abnormal tracking will also create undue stress on the patellofemoral joint. The balance between medial and lateral stability is essential for maintaining appropriate biomechanics of the patellofemoral joint. According to Powers, only 50% of patients with PFP demonstrate tracking abnormalities, which would indicate that other factors must be involved. More recently, a different approach has been advocated for treatment of PFP that involves assessment and intervention of strength and movement of the hip. Researchers41,42 have examined hip strength and consistently found hip abductor, external rotator, and extensor weakness in females with PFPS. Some have found this weakness to be associated with kinematic changes such as increased hip adduction and internal rotation in subjects with PFPS. This hip position promotes a dynamic Q-angle12 or a medialization of the knee resulting in the patella tracking laterally relative to the trochlea. Females tend to exhibit a greater dynamic Q-angle than males during tasks such as stair descent, running, cutting and jumping.43-45
Further, there is thought that foot position influences patellar position.7,46 Because of the biomechanical relationship between anatomical segments, it would seem intuitive that a distal fault at the foot (pes planus or cavus) would have an effect on the proximal segment. Tiberio describes a theoretical model that discusses the influence of subtalar joint pronation on the knee.7 In his model, excessive pronation drives the tibia into internal rotation followed by subsequent femoral internal rotation causing a relative laterally positioned patella, a possible cause of PFPS. In contrast, two separate research groups have reported the development of PFPS in subjects who exhibited lack of pronation during gait.46,47 Other distal factors that may influence the kinematics at the knee are limited dorsiflexion and excessive midfoot mobility.
CONCLUSIONS
Excellent comprehension of the structures and forces that influence patellofemoral function is paramount to understanding the wide variety of clinical problems found at the patellofemoral joint. This information may be applied when examining and assessing athletes, as well as when prescribing rehabilitation interventions so that exercises are performed in ranges of motion that place minimal strain on damaged or vulnerable structures.
REFERENCES
- 1.Crossley KM Callaghan MJ Linschoten R van. Patellofemoral pain. Br J Sports Med. 2016;50(4):247-250. [DOI] [PubMed] [Google Scholar]
- 2.van Gent RN Siem D van Middelkoop M van Os AG Bierma-Zeinstra SMA Koes BW. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41(8):469-480; discussion 480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renström AF. Knee pain in tennis players. Clin Sports Med. 1995;14(1):163-175. [PubMed] [Google Scholar]
- 4.Zhang D Wu Z Zuo X Li J Huang C. Diagnosis and treatment of excessive lateral pressure syndrome of the patellofemoral joint caused by military training. Orthop Surg. 2011;3(1):35-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boling MC Padua DA Marshall SW Guskiewicz K Pyne S Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boling M Padua D Marshall S Guskiewicz K Pyne S Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20(5):725-730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiberio D. The effect of excessive subtalar joint pronation on patellofemoral mechanics: a theoretical model. J Orthop Sports Phys Ther. 1987;9(4):160-165. [DOI] [PubMed] [Google Scholar]
- 8.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639-646. [DOI] [PubMed] [Google Scholar]
- 9.Powers CM. Patellar kinematics, part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther. 2000;80(10):965-978. [PubMed] [Google Scholar]
- 10.Witvrouw E Lysens R Bellemans J Cambier D Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am J Sports Med. 2000;28(4):480-489. [DOI] [PubMed] [Google Scholar]
- 11.Salsich GB Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther. 2007;37(9):521-528. [DOI] [PubMed] [Google Scholar]
- 12.Powers CM Ward SR Fredericson M Guillet M Shellock FG. Patellofemoral kinematics during weight-bearing and non-weight-bearing knee extension in persons with lateral subluxation of the patella: a preliminary study. J Orthop Sports Phys Ther. 2003;33(11):677-685. [DOI] [PubMed] [Google Scholar]
- 13.Rothermich MA Glaviano NR Li J Hart JM. Patellofemoral pain: epidemiology, pathophysiology, and treatment options. Clin Sports Med. 2015;34(2):313-327. [DOI] [PubMed] [Google Scholar]
- 14.Tria AJ Palumbo RC Alicea JA. Conservative care for patellofemoral pain. Orthop Clin North Am. 1992;23(4):545-554. [PubMed] [Google Scholar]
- 15.Reider B Marshall JL Koslin B Ring B Girgis FG. The anterior aspect of the knee joint. J Bone Joint Surg Am. 1981;63(3):351-356. [PubMed] [Google Scholar]
- 16.Grelsamer RP Klein JR. The biomechanics of the patellofemoral joint. J Orthop Sports Phys Ther. 1998;28(5):286-298. [DOI] [PubMed] [Google Scholar]
- 17.Desio SM Burks RT Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65. [DOI] [PubMed] [Google Scholar]
- 18.Powers CM Landel R Perry J. Timing and intensity of vastus muscle activity during functional activities in subjects with and without patellofemoral pain. Phys Ther. 1996;76(9):946-955; discussion 956-967. [DOI] [PubMed] [Google Scholar]
- 19.Chang W-D Huang W-S Lai P-T. Muscle activation of vastus medialis oblique and vastus lateralis in sling-based exercises in patients with patellofemoral pain syndrome: A cross-over study. Evid-Based Complement Altern Med ECAM. 2015;2015:740315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lack S Barton C Vicenzino B Morrissey D. Outcome predictors for conservative patellofemoral pain management: a systematic review and meta-analysis. Sports Med Auckl NZ. 2014;44(12):1703-1716. [DOI] [PubMed] [Google Scholar]
- 21.Goh JC Lee PY Bose K. A cadaver study of the function of the oblique part of vastus medialis. J Bone Joint Surg Br. 1995;77(2):225-231. [PubMed] [Google Scholar]
- 22.Lieb FJ Perry J. Quadriceps function. An anatomical and mechanical study using amputated limbs. J Bone Joint Surg Am. 1968;50(8):1535-1548. [PubMed] [Google Scholar]
- 23.Terry GC Hughston JC Norwood LA. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14(1):39-45. [DOI] [PubMed] [Google Scholar]
- 24.Huberti HH Hayes WC. Patellofemoral contact pressures. The influence of q-angle and tendofemoral contact. J Bone Joint Surg Am. 1984;66(5):715-724. [PubMed] [Google Scholar]
- 25.Steinkamp LA Dillingham MF Markel MD Hill JA Kaufman KR. Biomechanical considerations in patellofemoral joint rehabilitation. Am J Sports Med. 1993;21(3):438-444. [DOI] [PubMed] [Google Scholar]
- 26.Hungerford DS Barry M. Biomechanics of the patellofemoral joint. Clin Orthop. 1979;(144):9-15. [PubMed] [Google Scholar]
- 27.McConnell J. The physical therapist's approach to patellofemoral disorders. Clin Sports Med. 2002;21(3):363-387. [DOI] [PubMed] [Google Scholar]
- 28.Watson CJ Propps M Galt W Redding A Dobbs D. Reliability of McConnell's classification of patellar orientation in symptomatic and asymptomatic subjects. J Orthop Sports Phys Ther. 1999;29(7):378-385; discussion 386-393. [DOI] [PubMed] [Google Scholar]
- 29.Freedman BR Brindle TJ Sheehan FT. Re-evaluating the functional implications of the Q-angle and its relationship to in-vivo patellofemoral kinematics. Clin Biomech Bristol Avon. 2014;29(10):1139-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Silva D de O Briani RV Pazzinatto MF, et al. Q-angle static or dynamic measurements, which is the best choice for patellofemoral pain? Clin Biomech Bristol Avon. 2015;30(10):1083-1087. [DOI] [PubMed] [Google Scholar]
- 31.Almeida GPL Silva AP de MCCE França FJR Magalhães MO Burke TN Marques AP. Relationship between frontal plane projection angle of the knee and hip and trunk strength in women with and without patellofemoral pain. J Back Musculoskelet Rehabil. September 2015. [DOI] [PubMed] [Google Scholar]
- 32.Insall J Salvati E. Patella position in the normal knee joint. Radiology. 1971;101(1):101-104. [DOI] [PubMed] [Google Scholar]
- 33.Powers CM Lilley JC Lee TQ. The effects of axial and multi-plane loading of the extensor mechanism on the patellofemoral joint. Clin Biomech Bristol Avon. 1998;13(8):616-624. [DOI] [PubMed] [Google Scholar]
- 34.Feller JA Amis AA Andrish JT Arendt EA Erasmus PJ Powers CM. Surgical biomechanics of the patellofemoral joint. Arthroscopy. 2007;23(5):542-553. [DOI] [PubMed] [Google Scholar]
- 35.Powers CM Shellock FG Pfaff M. Quantification of patellar tracking using kinematic MRI. J Magn Reson Imaging . 1998;8(3):724-732. [DOI] [PubMed] [Google Scholar]
- 36.Pappas E Wong-Tom WM. Prospective Predictors of Patellofemoral Pain Syndrome: A Systematic Review With Meta-analysis. Sports Health. 2012;4(2):115-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Willson JD Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008;38(10):606-615. [DOI] [PubMed] [Google Scholar]
- 38.Reilly DT Martens M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Orthop Scand. 1972;43(2):126-137. [DOI] [PubMed] [Google Scholar]
- 39.Flynn TW Soutas-Little RW. Patellofemoral joint compressive forces in forward and backward running. J Orthop Sports Phys Ther. 1995;21(5):277-282. [DOI] [PubMed] [Google Scholar]
- 40.Wiberg G. Roentgenographic and anatomic studies of the femoro-patellar joint. Acta Orthop Scand. 12(3):319-410. [Google Scholar]
- 41.Bolgla LA Malone TR Umberger BR Uhl TL. Hip strength and hip and knee kinematics during stair descent in females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2008;38(1):12-18. [DOI] [PubMed] [Google Scholar]
- 42.Robinson RL Nee RJ. Analysis of hip strength in females seeking physical therapy treatment for unilateral patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2007;37(5):232-238. [DOI] [PubMed] [Google Scholar]
- 43.Willson JD Binder-Macleod S Davis IS. Lower extremity jumping mechanics of female athletes with and without patellofemoral pain before and after exertion. Am J Sports Med. 2008;36(8):1587-1596. [DOI] [PubMed] [Google Scholar]
- 44.Willson JD Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech Bristol Avon. 2008;23(2):203-211. [DOI] [PubMed] [Google Scholar]
- 45.Dierks TA Manal KT Hamill J Davis IS. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 2008;38(8):448-456. [DOI] [PubMed] [Google Scholar]
- 46.Thijs Y Van Tiggelen D Roosen P De Clercq D Witvrouw E. A prospective study on gait-related intrinsic risk factors for patellofemoral pain. Clin J Sport Med . 2007;17(6):437-445. [DOI] [PubMed] [Google Scholar]
- 47.Hetsroni I Finestone A Milgrom C, et al. A prospective biomechanical study of the association between foot pronation and the incidence of anterior knee pain among military recruits. J Bone Joint Surg Br. 2006;88(7):905-908. [DOI] [PubMed] [Google Scholar]