Abstract
Patellofemoral pain is one of the leading causes of knee pain in athletes. The many causes of patellofemoral pain make diagnosis unpredictable and examination and treatment difficult. This clinical commentary discusses a detailed physical examination routine for the patient with patellofemoral pain. Critically listening and obtaining a detailed medical history followed by a clearly structured physical examination will allow the physical therapist to diagnose most forms of patellofemoral pain. This clinical commentary goes one step further by suggesting an examination scheme and order in which it should be performed during the examination process. This step-by-step guide will be helpful for the student or novice therapist and serve as review for those that are already well versed in patellofemoral examination.
Keywords: Patellofemoral assessment and Clinical reasoning, evaluation
INTRODUCTION
Patellofemoral pain syndrome (PFPS) is considered to be one of the most common medical diagnoses made in outpatient orthopedics in patients complaining of knee pain.1 PFPS has an incidence between 15-25%.2 Additionally, PFPS accounts for up to 25% of sports related knee injuries.3 Recent consensus statements have elucidated the importance of this sometimes perplexing condition.4,5 The seemingly simple design of the patellofemoral joint, is, in reality, a very complex articulation with contributing factors that are both intrinsic and extrinsic in nature, noncontractile and contractile, some of which include substantial interplay from other more distant sources, such as the hip or foot. In order to determine what form of intervention is needed in a patient with knee pain, the clinician must initially perform an accurate, comprehensive, yet concise physical examination. Examination findings are not always consistent, nor directly related to symptoms. Additionally, there is no single definitive clinical test used to diagnose patellofemoral pain syndrome.2 At times important clues and findings regarding PFPS may be very subtle. Clinical experience examining and treating many patients with knee conditions is helpful in making a correct diagnosis. Following an examination scheme consistently will provide the clinician with a good foundation to decipher what findings may be considered normal and abnormal. This systematic, complete, and detailed approach to examination will allow the clinician to identify all contributing factors, ultimately leading to optimal treatment approaches by addressing all potential causative factors, which should result in a more compliant patient and better outcomes.6
HISTORY
The cornerstone of any examination is the medical history. If the clinician listens closely enough, and asks the appropriate questions during any medical history the patient will often describe what their diagnosis is. Knowledge about the symptoms’ onset, mechanism of injury, location, character or description, severity under different conditions, and any aggravating or alleviating factors will help with the diagnosis.6 Classical red or yellow flag symptoms such as weight loss, lack of appetite, erythema, and unusual lumps should clearly be ruled out prior to assuming this condition is localized to the patellofemoral joint.7 A systems review should be performed to identify any potential medical problems (red flags) that may be causing or contributing to the patient's symptoms. If indicated, it is important to understand that it is always prudent to refer back to the original referral source or to another medical provider in order to rule out any suspicious symptoms that are out of the ordinary or may not be attributable to musculoskeletal factors.
The patient's activities of daily living, vocational activities, recreational or sporting activities are also important to understand because they may contribute to the patient's symptoms. Oftentimes, changing or modifying the cause of the problem may help resolve some of the symptoms.
PFPS is in many instances a nonspecific complaint that can be traced to or associated with multiple conditions. These include compressive issues, instability, biomechanical dysfunction, direct patellar trauma, soft tissue lesions, overuse syndromes, osteochondritis dissecans, and neurologic disorders.8 Compressive issues usually are characterized by aching symptoms that worsen when the knee is positioned in flexion for long periods of time. Going to a movie, sitting in a car or plane during long trips often aggravate the symptoms. Deep squats and stairs are also commonly symptomatic. In more severe conditions both ascending and descending steps will cause or increase the pain. In less acute conditions ascending stairs, which requires a concentric contraction of the quadriceps muscle, may not create symptoms. However, because descending steps (Figure 1) requires an eccentric contraction, it may create pain due to the increased compressive loads placed upon the articular cartilage of the posterior patellar facets during eccentric loading.
Figure 1.
Descending a step using an eccentric contraction of the quadriceps can cause patellar pain due to increased compressive loads placed upon the articular cartilage of the posterior patellar facets.
The patient with patellar instability will usually describe symptoms such as though the knee is slipping, giving way or giving out. Instability does not have to be the result of a macrotraumatic patellar dislocation or injury and is oftentimes subtle and microtraumatic in nature.
Biomechanical issues such as increased knee valgus, increased hip adduction and tibial abduction or foot pronation are generally reported as vague complaints of pain that are generalized throughout the anterior knee. These symptoms can be precipitated by a miserable malalignment syndrome in which the athlete has an internally rotated femur, externally rotated tibia and pronated foot.9
Direct patellar trauma is acute in nature and can be extremely painful as a result of fractures, fracture/dislocations, and associated articular cartilage lesions, such as osteochondritis dissecans (OCD). If the injury is acute, the clinician should suspect a contusion, or patellar dislocation. Acute conditions can occur from a fall on the anterior knee or planting and cutting maneuvers that create an increased valgus force at the knee resulting in a lateral patellar subluxation or dislocation.
Soft tissue lesions should be separated from overuse lesions, although it may sound as though there is some overlap. Soft tissue lesions can be aching in nature or can present as more sharp in nature depending on the extent of tissue irritability. These soft tissue lesions include plica syndrome, fat pad syndrome (Hoffa's Syndrome), and bursitis. In contrast, overuse syndromes more typically involve tendon or apophyseal injuries. Soft tissue tendon disorders usually cause pain along or near a tendon or its attachment site to the bone via the Sharpey's fibers. Pain is usually aggravated with activity, quick starts, stops and jumping sports. A common apophyseal injury in teenagers during times of rapid growth that directly involves the patella is Sindig-Larsen-Johannsen's Syndrome.
Overuse injuries occur when training type, frequency, duration or intensity exceeds the body's ability to repair itself. These types of conditions are more common in athletes such as runners, or someone starting an overzealous exercise program. At times overuse of the anterior knee can also occur as a result of vocational activities, especially those that require repetitive squatting, stair climbing or walking. It must be remembered though that overuse injuries can present as an acute re-exacerbation of a condition; consequently an acute on chronic condition is not uncommon with PFPS.
Osteochondritis dissecans (OCD) can create PFPS symptoms that are deep in the knee often described as behind the patella. Patellar chondral OCDs are less common than those at the lateral portion of the medial femoral condyle.10 Patellar dislocations frequently result in an OCD lesion. However because these lesions both lie directly behind the patella they are often very symptomatic and seem to be patellar in nature. Intermittent knee effusions and painful weight bearing would indicated a need for special imaging to rule this condition out.11
Lastly, complex regional pain syndrome or reflex sympathetic dystrophy can cause anterior knee pain. This condition is usually trauma or surgically induced. An exaggerated pain response due to sympathetically maintained pain would be the presentation of this condition.
In most instances a patient with PFPS will simply complain of anterior knee pain, oftentimes with bilateral complaints. This pain may be localized in a small area or it may be a large, vague general pain complaint that is not easily isolated. Grelsamer and McConnell10 report that the location of pain may indicate specific tissues involved. Table 1 presents information that may assist with differential diagnosis by listing location and possible causes. Lastly, it is important to know if the patient has had any past surgeries. Knowing the exact procedure and what the complaints were prior to that surgery are both important.
Table 1.
Location and Possible Cause of Anterior Knee Pain
| Location of Pain | Possible Cause of Anterior Knee Pain |
|---|---|
| Lateral | Small nerves (retinacular neuromas) in lateral retinaculum, ITB syndrome, Popliteal tendonitis |
| Medial | Recurrent stretching of medial retinaculum, medial patellofemoral ligament, plica syndrome, retinacular neuromas |
| Retropatellar | Articular cartilage damage, stress on subchondral bone, OCD, bone contusions |
| Superior | Quadriceps tendonitis/tendinosis |
| Inferior | Patella tendonitis/tendinosis, fat pat syndrome (Hoffa's Syndrome), Sindig-Larsen-Johannsen's Syndrome |
ITB = Iliotibial band
OCD = Osteochondritis dessicans
PHYSICAL EXAMINATION OVERVIEW
The patient's knees, and ideally the entire lower extremity, should be exposed for the examination. The uninvolved knee should be evaluated first to establish a baseline “normal” for the patient before the involved extremity is examined.
Observation/Posture
Following the medical history and subjective examination, the clinician should begin the observation portion of the examination. The clinician begins by looking for obvious signs of deformity, discoloration, swelling or scars. Abnormal protuberances, ecchymosis, joint effusion or edema should be noted in or around the knee. Scars may be from history of trauma or surgery. The examination will progress from standing, to seated, to supine.
Standing Examination
General standing examination should be evaluated in the three basic cardinal planes. Each plane has certain unique aspects that should be examined to ensure the clinician has a good understanding of structural or functional adaptations or compensations that may be a source of PFPS symptoms.
Postural Anterior/Posterior View for Frontal Plane Alignment
A varus or valgus knee posture can usually be seen clearly in the anterior sagittal plane view (Figure 2). A reduction of the normal 125-degree inclination of the femoral neck and femoral shaft (coxa vara) will create a genu valgus at the knee, while an increase in the normal angle (coxa valga) will create genu varus at the knee. The clinician should ensure that femoral rotation and foot pronation are not contributing to the varus or valgus angulation at the knee. The patella position should also be evaluated to determine its position relative to internal or external rotation. The patellar position relative to the proximal tibia should be assessed for a bayonet sign or excessive external tibial torsion. The tibial alignment for tibia varum should also be assessed realizing that some distal tibia varum is normal. The foot should be evaluated from the anterior view to check for a forefoot dysfunction, midtarsal joint position (using the Navicular Drop test, Feiss’ Line, or Medial longitudinal arch angle) and from the posterior view (Figure 3) to check the weightbearing subtalar joint position.
Figure 2.
Anterior view can be used to assess valgus/varus angulation of knee, coxa valga/vara and overall patellar position.
Figure 3.
Posterior view can be used to assess valgus/varus angulation of the knee, and to assess forefoot, mid-tarsal, and subtalar joint position.
Postural Lateral View for Sagittal Plane Alignment
The lateral view (Figure 4) is best to observe for either genu recurvatum or a flexion contracture. Excessive genu recurvatum can create a Hoffa's syndrome due to impingement of the infrapatellar fat pad and the inferior pole of the patella. Quadriceps weakness due to either strength loss or inhibition may present as knee hyperextension. A flexion contracture is the result of loss of knee extension range of motion. This can be caused from motion limitations post-surgery, trauma, injury, or excessive hamstring tightness. This posture will cause overuse of the quadriceps muscle due to inability to achieve end range extension. This view also allows for a clinical assessment of a patella alta or infera (baja). Additionally, this view permits assessment of a camel sign of the knee which may be normal or be a contributing factor to a Hoffa's syndrome.
Figure 4.
Lateral view can be used to assess for genu recurvatum, knee flexion contracture, and patella alta or baja.
Anterior View for Transverse Plane Alignment
Transverse plane views are best to observe femoral rotation. Excessive femoral anteversion will create increased medial rotation of the patella position, while excessive femoral anteversion will create increased lateral rotation of the patella position. Much like viewing the sagittal plane, the clinician must ensure that the rotation component they are viewing is not coming distally from foot pronation. General alignment of the hips and pelvis will give the indication of either a short or long leg or pelvic rotation. Palpation of the iliac crest, anterior superior iliac spine (ASIS), anterior inferior iliac spine (AIIS) and posterior superior iliac spine (PSIS) is done by kneeling in front of or behind the athlete. These are generally palpated bilaterally with use of the dominant eye to gauge for symmetry. Asymmetry may be due to pelvic obliquity, hip abnormalities, or leg length differences. While viewing anteriorly the clinician will usually be able to note atrophy of the quadriceps. Atrophy can occur anywhere around the knee or calf therefore the clinician should view both above and below the knee joint.
Q-Angle
The “law of valgus” describes the natural tendency for the patella to track laterally during dynamic movements.11 This valgus angulation occurs due to the quadriceps attachments to the femur. Q-angle is a measurement of the angle formed by the intersection of a line drawn from the anterosuperior iliac spine to the midpoint of the patella and the proximal extension of a line drawn from the tibial tubercle to the midpoint of the patella.12 A larger Q-angle may create a larger lateral vector and potentially a greater predisposition to lateral patellar tracking when compared to a smaller Q-angle.13 A greater Q-angle in women (15-18 degrees) compared to men (12 degrees) may partly explain higher incidences of patellofemoral pain in women due to a larger lateral valgus vector, although complaints of pain are usually multifactorial.14 Due to the variability of measurement techniques performed in supine, standing, with quadriceps contracted, with quadriceps relaxed, etc; the clinical utility of measuring Q-angle cannot be supported.15 Based on a meta-analysis examining the Q-angle, it was determined that this measurement by itself is not a risk factor for development of patellofemoral pain.1 Additionally, the relationship between Q-angle and signs and symptoms has not always been consistent.16 It is possible that an excessive Q-angle may only be problematic in a subpopulation of those with PFPS pain. Other factors that are unrelated to Q-angle may be more predominant in certain patellofemoral patients. Clinicians have to remember that in most measurement methods, Q-angle is a static measurement that is hypothetically measuring a dynamic function of the quadriceps.
Leg Length Measurements
Leg length differences alter gait symmetry and joint mechanics during weight bearing, potentially contributing to atypical compressive and tensile stresses on the joint structures of the lower limb.17
The clinician can palpate several bony landmarks to see if the pelvis and hips are in normal alignment. Palpation of the iliac crests bilaterally (unshod) will determine pelvis height or level (Figure 5). The clinician should ensure that the patient's feet are both in neutral position. A higher iliac crest could indicate a long leg, while a lower iliac crest could indicate a short leg. The body will normally try to equalize this length through compensations to restore homeostasis. Anterior knee pain could result from either a long or short leg. The long leg may require compensation by pronating at the foot and subtalar joint, while the shorter foot may compensate by having to supinate in an attempt to equalize the leg length. Additionally, in standing the clinician can measure with a flexible tape measure the distance from the anterior superior iliac spine (ASIS) to the medial malleolus (Figure 6). A difference more than 1.5 cm may be considered pathologic.7 The authors encourage clinicians to take leg length measurements in weight bearing positions so they do not miss any potential compensatory patterns. As an example, if a patient has unilateral recurvatum or unilateral pronation, those conditions will not show up in a non-weight bearing leg length measurement position.
Figure 5.
Palpation of the iliac crest to examine for pelvis height. Higher iliac crest could indicate a longer leg, while a lower iliac crest could indicate a shorter leg.
Figure 6.
Measurement of standing leg length measurement taken with flexible tape measure from anterior superior iliac spine to medial malleolus. A difference in length of limbs greater than 1.5 cm is thought to be pathologic.
The clinician can also measure leg lengths with the patient supine. The patient should lie with the legs at right angle to the two ASIS. With a flexible tape measure the clinician measures as they did in standing from the ASIS to the medial malleolus. A difference of as much as 1.0 to 1.5 cm is considered normal.7 A follow up test to see where the discrepancy lies is to measure from the iliac crest to the greater trochanter (for coxa vara, and from the greater trochanter to the lateral knee joint line (for femoral shaft length), and from the medial knee joint line to the medial malleolus (for tibial length). Tibial length can also be examined in prone. The clinician flexes the patient's knee to 90 degrees while they are lying prone. The relative heights of the heels are noted. Another way to view femur length is to simply compare the heights of knees while the patient is lying supine with hips flexed 45 degrees. A longer distal femur (knee) would indicate a longer femur.
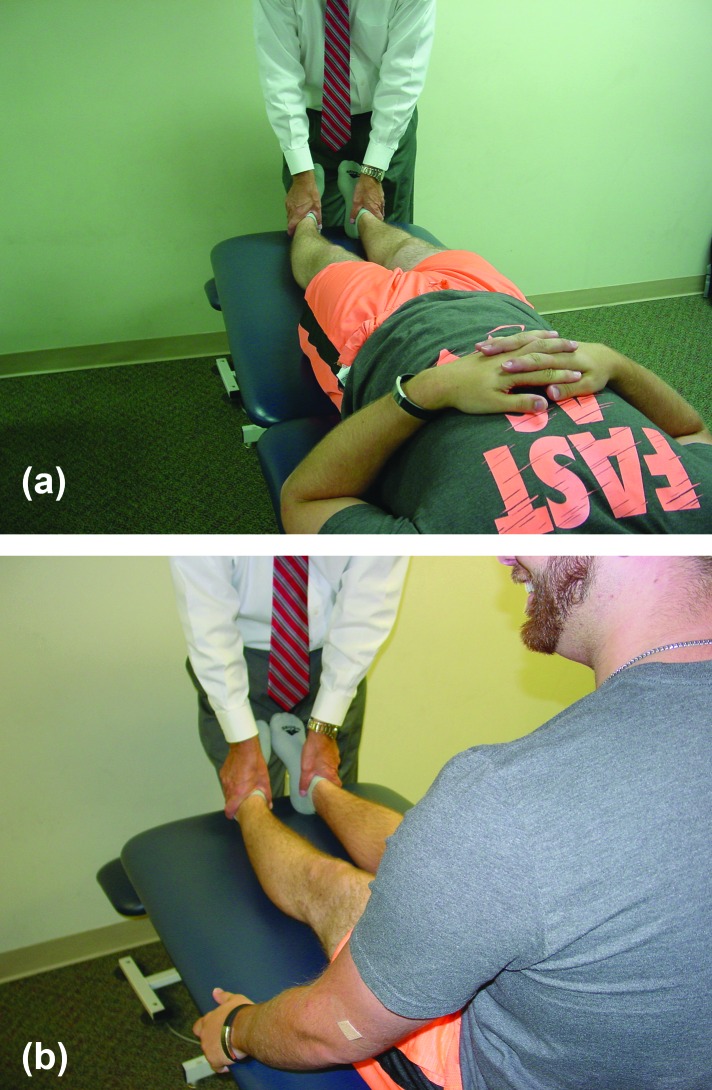
The Weber-Barstow maneuver is also used in supine to measure leg length differences.7 To begin the patient lies supine with hips flexed 45 degrees. While the clinician holds the patient's feet while the patient lifts their hips off the supportive surface, and then returns them to resting position. The clinician then passively extends the knees and hips and compares bilaterally the position (length) of the medial malleoli. This measurement can be taken in supine (Figure 7a) or in long sitting (Figure 7b). A difference would present as either a shorter or longer leg.
Figure 7.
Weber-Barstow measurement comparing position of malleoli in supine (a) and long sitting (b).
Foot Posture
While standing, foot posture can be assessed. Excessive pronation can be seen usually in relaxed standing (Figure 8) and during normal walking or running. Flatfoot, or a flattened medial longitudinal arch, or a valgus hindfoot could indicate excessive pronation. Examination of heel position for pronation has been performed for some time and has demonstrated good intertester and intratester ICC's ranging from .68 to .91.18
Figure 8.
Excessive pronation seen as medial arch collapse in relaxed standing.
A true pronated flat foot may be either from congenital problems, trauma, muscle weakness, ligament laxity, dropping of the talar head, paralysis, or just be excessively pronated.7 Not all flatfeet cause problems. Flatfoot comes in two forms, rigid or congenital and flexible or acquired. Rigid is fairly rare and occurs with the heel in valgus, and midfoot in pronation. A flexible flatfoot may be caused by tibial torsion, femoral torsion, coxa vara or injury to the posterior tibial tendon (PTT).7,19 Generally determining if the flatfoot is rigid or flexible is achieved by having the patient stand on their toes. If the arch is still not present when they stand on tiptoes, they have rigid flatfoot. If the arch appears when standing on toes it is flexible.
To determine the position of the subtalar joint the examiner palpates the head of the talus on the dorsal medial aspect of the right foot with the forefinger and the talar dome on the dorsal lateral aspect of the foot with the thumb. The clinician will have the patient slowly rotate their trunk to right and left causing the tibia to medially and laterally rotate. As this occurs the foot will concomitantly supinate and pronate. Once the neutral position is found (when talar head and dome does not appear to bulge either medially or laterally) (Figure 9) a measurement can be taken from the navicular to the ground. The patient is then asked to relax and another measurement is taken. This is described as the uncompensated to compensated position of the foot. The difference of these two measurements is called the navicular drop and is used to quantify midfoot mobility. If the navicular drop is 10 mm or less, it is considered to be within normal limits (WNL). Feiss line and the medial longitudinal arch angle are other methods that have been described to identify a static pronated foot.20-22
Figure 9.
Assessment of subtalar joint in weight bearing functional position. Clinician will palpate the head of the talus on the dorsal medial aspect of the right foot with the finger and the talar dome on the lateral foot with the thumb.
DYNAMIC MOVEMENT ASSESSMENTS
Because in many instances cardinal plane deviations may not be seen in relaxed standing or during general gait assessment an activity with greater demand placed upon the knees is needed to be a part of the examination process. The step down test or the single leg squat is a method of examination that can be used.
Step-Down Test
A step-down test can be performed to assess hip and leg strength and endurance. The patient is asked to stand on a 20 cm box with leg to be tested. Patient should stand with arms folded across chest and be instructed to squat down on one lower extremity (Figure 10) 5-10 times consecutively, in a slow and controlled manner until the heel touches the floor, maintaining their balance at a rate of approximately 1 squat per 2 seconds. Examples of alterations seen during the step-down tests can be seen in Table 2.
Figure 10.
The step-down test is performed to test hip and leg strength and endurance. Patient stands with arms folded across chest as they lower themselves in a slow and controlled manner until heel touches the floor.
Table 2.
Step Down Test Alterations
| Overall Impression | Trunk | Pelvis | Hip | Knee |
|---|---|---|---|---|
| Maintain balance | Lateral deviation/shifting | Lateral rotation | Adduction | Valgus |
| Perturbation | Rotation | Rotation | Internal rotation | Varus |
| Depth of movement | Lateral flexion | Tilt | Position relative to foot | |
| Speed of movement | Forward flexion |
Crossley compared those with patellofemoral pain who scored “good” on the step down test to those who performed poorly.23 To be considered good the patient must have shown none of the deviations in 4 of the 5 criterion listed in table 2. Those who were rated as poor had decreased onset timing of the anterior gluteus medius, had decreased hip abduction torque (29 percent), and decreased lateral trunk strength (23 percent) compared to those with good scores. Additionally, they found excellent inter-rater (k=.80) and intra-rater (k=.80) reliability with the scoring system described.
Lateral Step Down Test
Rabin and collegues,24 developed a scoring system for criteria for the lateral step-down test (Table 3). The lateral step-down test is a modification of standard step-down test in which the movement is lateral versus anterior. Instructions for the lateral step down test are as follows: patient is to stand with involved leg on a 15 cm step. This will require most to bend the knee at about 60 degrees. Patients are asked to reach down and touch the opposite, non-involved heel to the ground, then return to the starting position. Patient should be rated on the criterion listed in Table 3. Rabin scored participants with patellofemoral pain as good (score, 0-1) or moderate (score 2 or greater). Participants in their study with moderate scores exhibited dorsiflexion range of motion limitations and less hip external rotation and knee extension muscle strength.
Table 3.
Scoring for Lateral Step-Down Test
| Criterion | Interpretation | Score |
|---|---|---|
| Arm strategy | Removes hands from waist | 1 |
| Trunk alignment | Leaning in any direction | 1 |
| Pelvic plane | Loss of horizontal plane | 1 |
| Knee posture | Tibial tuberosity medial to 2nd toe | 1 |
| Tibial tuberosity medial to medial border of foot | 2 | |
| Steady | Stepping down on non-tested limb, or wavering from side to side | 1 |
Single-Leg Squat
Nunes at al report that the best available test for PFP is anterior knee pain elicited during a squatting maneuver. PFP is evident in 80% of people who are positive in this test.2 Consequently the single leg squat is a test of dynamic hip and quadriceps strength in the examination (Figure 11). This maneuver imposes higher mechanical demands, than a bilateral squat, that may induce compensatory movements such as knee valgus. This may partially be due to the smaller base of support and increased amounts of dynamic control that are needed in all planes during the single limb squat.
Figure 11.
Single-leg squat with proper form and good control.
Nakagawa25 reports that compared to controls, males and females with patellofemoral pain showed increased ipsilateral trunk lean (Figure 12), contralateral pelvic drop (Figure 13), hip adduction and knee abduction (Figure 14) during a single-leg squat. These altered kinematics were associated with decreased strength of the hip abductors and external rotators as measured eccentrically on an isokinetic dynamometer.
Figure 12.
Single-leg squat with compensatory increased ipsilateral trunk lean.
Figure 13.
Single-leg squat with compensatory increased contralateral pelvic drop.
Figure 14.
Single-leg squat with compensatory hip adduction and knee abduction.
The patella can also be palpated for grating or crepitus, in both closed kinetic and open kinetic chain movements, which may be an indication of articular cartilage damage. If the crepitus correlates with patient's symptoms at a particular point in the range of motion (ROM), then it assists in clinical reasoning and forming guidelines for designing the therapeutic exercise program. Likewise, palpating the peri-patellar soft tissue in a weight-bearing position may also produce symptoms, which are not present in a non-weight bearing position.
Gait
Qualitative gait evaluation begins as soon as the patient enters the clinic, even with informally observing gait when moving into the clinic. The formal gait evaluation needs to be performed with appropriate shoes (if in sports, then those shoes should be used; if specified work shoes like OSHA hard soled, steel toe shoes are required, then the gait evaluation should be performed in those shoes) If the patient wears orthotics themselves should also be evaluated to see if they are still functionally and structurally sound. With shoes on, it is difficult to actually see some of actual food mechanics. Ideally, the gait evaluation is also performed bare footed so the actual mechanics of the foot can also be assessed. The observation should be performed from anterior, posterior and lateral views. Because the patient is in one place by walking on a treadmill, this allows for consistent observation of the foot and lower extremity mechanics. However, if performing a qualitative gait analysis with the patient walking in the clinic, because they are moving toward or away from the clinician with the anterior or posterior views, each step and observational perspective of the patient is different because of the varying distances from the examiner.
If the patient is a runner, then they also need to be evaluated under various running conditions. Additionally, with cell phones so common and numerous biomechanical apps available (Dartfish, SloPro, CMV, Coach's Eye, Hudl, SkyCoach, etc.), it is easy to video the patients gait using their own phone so that they can see the mechanics of their walking, running, etc.
Examination for systemic hypermobility (Beighton Index)
To examine for overall widespread joint hypermobility throughout the body the clinician can utilize the Beighton scale of hypermobility. The test criterion is presented in Table 4. Although no studies have clearly described positive findings of hypermobility, most sources state that a score of 4 or more points indicates generalized hypermobility.26-28
Table 4.
Beighton Hypermobility Scoring
| Thumb can be bent to the radial side of the forearm (1 point each thumb) |
| 5th finger can be extended past 90 degrees (1 point each 5th finger) |
| Knee can hyperextend past 0 (1 point each knee) |
| Elbow can be hyperextend past 0 (1 point each elbow) |
| Patient can bend forward at the trunk and place hands on floor flat without bending knees (1 point) |
| Maximum score of 9 points |
Sendur and colleagues29 assessed knees and compared Q-angle in those with normal mobility compared to those with joint hypermobility. They placed subjects in three groups of 20 based on presence of Beighton scale score. The mean Q angle values for healthy hypermobile patients was significantly higher than those that were non-hypermobile. In their population they found the frequency of joint hypermobility, (Beighton scale of 4 or more) to be 29.25%. Quatman et al30 found that in contrast to males, females may have greater generalized joint laxity following onset of puberty, while pre-pubertal males and females were similar. Due to these findings it would seem important to perform generalized laxity testing on those with larger Q angles or on females at any time in their growth period to determine if hypermobility may be contributory factor to patellofemoral pain.
SEATED EXAMINATION
Tibial tubercle sulcus angle
The tibial tubercle sulcus angle is measured with the patient sitting on the edge of the treatment table with knee flexed to 90 degrees. To determine this measurement the clinician observes the position of the tibial tubercle relative to the patellar center. A vertical line is drawn from the center of the patella to the center of the tibial tubercle. A second horizontal line is drawn through the femoral epicondyle. The patella should be completely captured within the femoral trochlea when flexed to 90 degrees. Measurement in this degree of flexion would indicate the amount of lateral displacement of the tubercle with reference to the femoral sulcus. Controversy exists as to what a normal angle is. Hughston31 reports a normal angle to be 0 degrees, while Kolowich32 considers upper limits of normal to be 10 degrees.
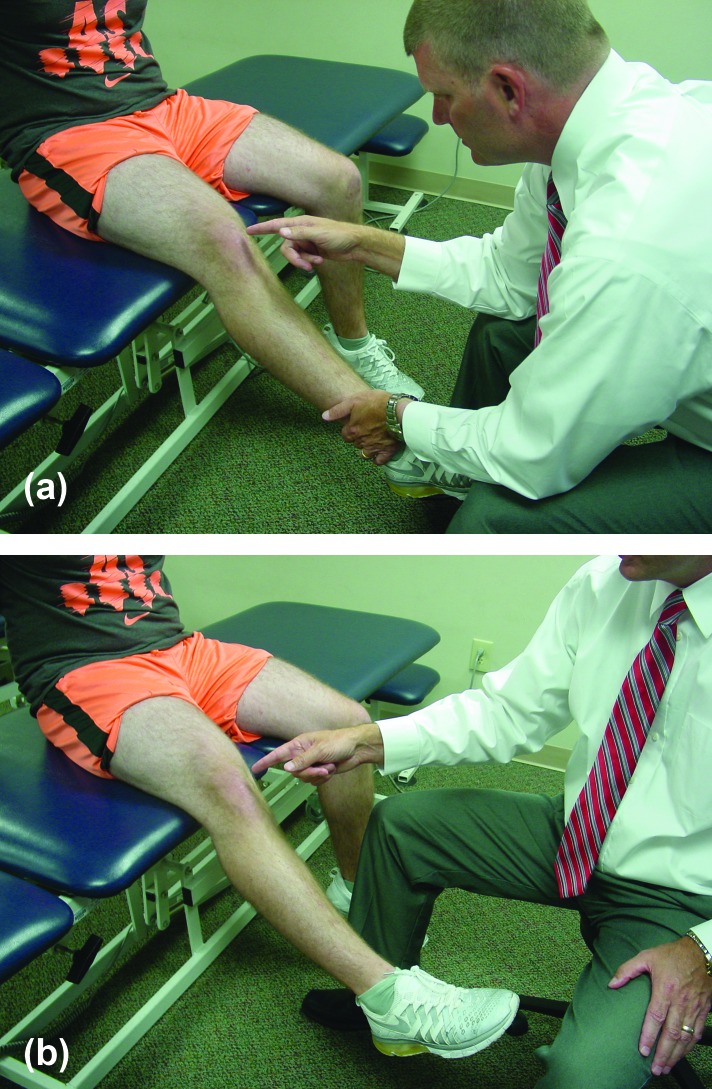
Passive and active patellar tracking
Passive and active patellar tracking is performed in the seated position. The patient is asked to sit back in the tripod position with arms extended behind for balance and to hold onto table and to decrease the tension on the hamstrings. This position also allows the pelvis to posteriorly rotate to put slack onto the hamstrings which may limit knee extension motion if sitting in more upright position. To begin with the clinician asks the patient to relax as the clinician passively extends the patients knee from 90 degrees’ flexion to full extension (Figure 15a). Normal patellar motion is for the patella to move slightly medial and then slightly laterally back to the original neutral position upon terminal knee extension or to track in a relatively straight line. As normal slight variations exist between individuals and sometimes between individuals’ two knees, small differences should not be cause for concern. Larger degrees of changes may be more indicative of pathology. Because this test is performed passively, it assesses the osseous and non-contractile tissues. If there is excessive gliding, it usually indicates tightness of the superficial retinacular fibers, whereas, if the patella has excessive tilting, then it implicates the deep retinacular fibers. Understanding this difference is important for determining how to treat the dysfunction. This test is then performed with the patient actively extending the knee from flexion to extension (Figure 15b). Careful attention should be paid to the range between 20-30 degrees of flexion to full extension as this is the location that most subluxation events occur. A lateral J-sign, or abrupt lateral deviation near terminal extension during an active quadriceps contraction may be indicative of a dysfunctional vastus medialis obliquus muscle lacking dynamic medial stabilization. The results of the passive and active tracking tests will contribute to the clinical reasoning for selection of appropriate interventions based on the cause of the dysfunction.
Figure 15.
Passive (a) and active (b) patellar tracking.
Strength Testing (Hip Flexion, Knee Extension, Hip External Rotation, Hip Internal Rotation)
Strength testing for a patient with patellofemoral pain is performed in both sitting and laying supine, side lying, and prone. Nicholas et al,33 was the first to demonstrate the concept of regional interdependency and total leg strength (TLS). Forty years ago, Nicholas suggested the inter-relationships between knee conditions and hip weaknesses. A subpopulation of patellofemoral pain patients that demonstrate proximal hip weakness may exist. Therefore, both knee and hip strength should be routinely tested. In normal individuals these groups are all very strong and rarely exhibit weakness. Testing of these groups are substantiated by the fact that Pappas and Wong-Tom34 found that using pooled data, decreased strength of knee flexion and hip abduction is associated with those who have patellofemoral pain. Boling et al35 found that decreased knee extension isometric strength was a predictor for patellofemoral pain syndrome, which is supported further by systematic reviews from Kooiker et al36 and Lankhorst and collegues.37
SUPINE EXAMINATION
Related/Referral Joints (Some of these tests may also be performed in the standing position)
All joints proximal and distal to the knee that can refer or influence functioning at the knee should be assessed. There are various techniques used to perform “clearing” tests. The lumbar spine, sacro-iliac joint, hip joint, proximal tibio-fibular joint, ankle and subtalar joints should be checked. Various methods to clear the joints can be used such as active range of motion (AROM), passive range of motion (PROM), resistive range of motion (RROM), or special tests of the respective areas.
Palpation
Although palpation does not always correlate exactly to the location of pathology in general musculoskeletal conditions, it does appear to be more sensitive in the patient with anterior knee pain than in those without.38 In their study following examination and palpation, the physicians were blinded from the patient pain diagram. The physicians filled out a pain diagram to see if their perception from physical examination was similar to the patient self-reported diagram. Eighty-five percent of all patient complaint zones were included in the physician's diagram. Additionally, Nunes et al2 indicate tenderness on palpation of the patellar edges is evident in 71-75% of people with patellofemoral pain syndrome.
Table 5 lists bony and soft tissue palpation areas around the knee that should be consistently and methodically palpated, rather than randomly during the physical examination, in the authors’ opinion. Palpating in a systematic manner with every patient will ensure that the clinician does not miss important structures due to inconsistent palpation technique. Because there is normally little adipose tissue around the knee, structures around the anterior knee are generally easier to find consistently. These structures listed in Table 5 should be palpated bilaterally as some of the areas of concern may just be sensitive on the uninvolved knee. The clinician should palpate for pain, temperature, effusion, edema, tissue thickness, or unusual nodules or protuberances.
Table 5.
Selected Bony and soft tissue areas of knee palpation
| Bony and Soft Tissue Knee Palpation | ||
|---|---|---|
| Bony | Muscular | Other |
| Patella | Vastus medialis | Patellar tendon |
| Inferior pole | Vastus lateralis | Quadriceps tendon |
| Superior pole | Rectus femoris | Patellar retinaculum |
| Tibial tubercle | Biceps femoris | Medial patellofemoral ligament |
| Adductor tubercle | Semitendinosus | Knee bursa |
| Medial femoral condyle | Semimemebranosis | Synovial plica |
| Medial tibial plateau | Gracillis | Medial collateral ligament |
| Lateral femoral condyle | Sartorius | Lateral collateral ligament |
| Lateral trochlear ridge | Tensor fascia lata | Superior capsule |
| Lateral tibial plateau | Iliotibial band | Ilio-tibial band |
| Patellar facets | Adductor muscle group | |
| Tibiofemoral joint line | Popliteus tendon insertion | |
| Fibular head | Gastrocnemius | |
| Gerdy's tubercle | ||
Neurological Examination
A screening neurological examination including sensation in dermatomes, reflexes, balance and/or proprioceptive testing should be performed. Some form of balance testing, whether it be a simple stork stand test (Figure 16), or completed using various testing instruments, should be performed because many patients with knee problems exhibit balance deficits. Proprioceptive testing in both open kinetic chain and closed kinetic chain positions can be accomplished using angular joint replication testing.
Figure 16.
Standing stork test for static balance deficits
Active ROM of Knee, Hip, Ankle and STJ
Goniometric measurements should be performed with functional AROM. The typical documentation for the knee motion is: 10-0-135 degrees beginning with hyperextension, moving through neutral (0) and into flexion. Proximal ROM measurements at the hip and ankle and STJ measurements distally need to also be taken because limitations in these joints can contribute to problems at the patellofemoral joint due to the regional interdependency interaction.
Passive ROM of Knee
Goniometric measurements should also be performed during PROM. One can always obtain more PROM compared to AROM. Assessing the qualitative aspects of the end feels often provides guidelines for treatment interventions.
Flexibility Tests
There are numerous flexibility tests (length tests of the musculo-tendinous unit) for musculature around the knee that are important because of the regional interdependence model and biarticular nature of several muscles around the hip and knee. Flexibility deficits may influence the function of the muscles affecting the patellofemoral joint and/or the tracking of the patella. Specific length tests that should be performed in the supine position include: hamstring 90/90 test, Thomas test, rectus femoris test, gastrocnemius, soleus, hip adductors, and gracilis tests.
Hamstring flexibility can be tested in several different methods. The 90/90 active straight leg raise test is performed in supine by flexing both hips to 90 degrees (Figure 17). The patient grasps behind the knee with both hands to keep the thigh vertical. The patient actively extends the knee as much as possible. Normal flexibility should be around 160 degrees (or 20 degrees from 0) of popliteal angle. The sitting hamstring flexibility test can be done with both knees extended (Figure 18) or one knee flexed against the chest and the other extended. The patient will flex at the trunk and attempt to touch the toes of the extended test limb. The test can be repeated to both sides. An inability to touch the toes indicates tight hamstring muscles.7
Figure 17.
90/90 leg raise test for hamstring flexibility.
Figure 18.
Sitting hamstring flexibility test
Hip flexors are tested in supine using the Thomas test. The examiner flexes the opposite knee until the lower back is flattened and lordosis is decreased, and the contralateral hip is held in 120 of hip flexion. When this position is reached the examiner holds it there. In this position the clinician examines the opposite limb. If there is tightness in the hip flexors, the hip being tested will remain elevated off the table and a muscular stretch end feel can be found. If the test is negative the tested limb will remain on the table. When this test is being performed the tested thigh may be pulled into hip abduction. This is indicative of a tight iliotibial band. This test can be performed at the end of the table with the mid-thigh at end of table the clinician can also assess for rectus femoris tightness. If a contracture of the rectus is present, the knee extends slightly. The clinician can attempt to passively flex the knee to see whether it remains at 90 degrees on its own. If during passive flexion of the knee, the thigh flexes it is indicative of tightness.7
Gastrocnemius/soleus flexibility is tested in supine. The gastrocnemius is a two joint muscle as it crosses the knee proximally and the ankle distally. To test the gastrocnemius the patient is asked to dorsiflex the ankle with the knee fully extended. The angle of the ankle at that point is the degree of flexibility. Because the soleus does not cross the knee proximally the patient is asked to flex the knee and dorsiflex the ankle. This angle is flexibility of the soleus.
Special Tests
When the patellofemoral joint is involved, it oftentimes creates a sero-sanginous synovitis response. Therefore, the first tests to be performed are effusion (intra-articular) vs edema, bursitis, hematoma, etc. (extra-articular) tests. There are several tests that can be performed, including milking tests, sweeping, and ballotment tests.
Both superficial and deep patellar retinacula need to be assessed in supine. Passive patellar glides are performed to assess the superficial lateral retinaculum and are performed with the knee in 30 degrees of flexion.39,40 Others report that testing should be done in full extension.41,42 Testing in full extension examines peripatellar soft tissue passive mobility solely. The authors preferred position is to test mobility in 30 degrees of knee flexion as the patella has started to enter the trochlea and provides a functionally stable position. In this position of slight flexion the clinician cannot only feel resistance from soft tissues, but also from the bony engagement of the patella into the trochlea. Most commonly patellar dislocations occur in this range, therefore it seems to be a functional position of testing.
To perform the test of passive patellar glide the patients relaxed knee is placed in 30 degrees of flexion over a bolster or towel roll. Patient relaxation is critical to obtain accurate results with this test. Even slight amounts of guarding will decrease the amount of patellar mobility. The clinician, on the lateral side of the knee, will use their thumbs to passively glide the patella in the medial direction (Figure 19). The clinician then moves their hands to the medial side and repeats the same technique to assess lateral mobility. The lateral glide is also known as the Fairbank's sign or apprehensive test. Therefore, it should be performed after the medial glide testing. The amount of patellar tilt must be kept constant during testing, as altering this factor will change the soft tissue mechanics. When tilt is not controlled the patella may rotate more giving the appearance of translation that is actually rotation. The clinician will estimate the amount of translation by dividing the patella into longitudinal quadrants and estimating the degree of number of quadrants worth of translation that can be induced during examination.43 Kolowich32 tested passive mobility in 20-30 degrees of flexion and reports that if the medial glide is less than one quadrant there is less than adequate medial mobility, while a medial glide of three to four quadrants suggests excessive hypermobility. Two quadrants of passive mobility are considered normal.. Additional patellar glides can be performed to assess superior and inferior motion (Figure 20 and 21)
Figure 19.
Examination test to assess for medial patellar glide performed in 30 degrees of knee flexion that assess for limitation of mobility in the superficial lateral patellar retinaculum.
Figure 20.
Examination test to assess for superior patellar glide performed in 30 degrees of knee flexion that assess the limitation of mobility of the inferior patellar tendon and soft tissue structures.
Figure 21.
Examination tests to assess for inferior patellar glide performed in 30 degrees of knee flexion that assess the limitation of mobility of the Quadriceps tendon and other quadriceps muscles.
The moving patellar apprehension test is performed with the patient supine with the thigh on the examining table and the clinician holding the leg in full extension off the table.44 The clinician then translates the patella laterally using their thumb (Figure 22), holding the patella laterally as the clinician flexes the knee to 90 degrees and then returns the knee to full extension. If there are symptoms while performing this movement the test is considered positive for lateral instability. To confirm this test, the clinician uses their thumbs to translate the patella medially while performing the same maneuver. If there are no symptoms on the second portion of this test, lateral instability is thought to be present. Again, the purpose of the testing is to assist in the clinical decision making to select appropriate interventions. So a positive finding may indicate the patient may benefit from patellofemoral taping, bracing, or total leg strengthening. If not successful, then a surgical procedure may be indicated.
Figure 22.
The moving patellar apprehension test is done with the patient supine The clinician translates the patella laterally while moving from a extended to a flexed position A positive test is indicated by symptoms of instability with this test.
Excessive lateral subluxation that is symptomatic is also known as the apprehension sign. Lax medial retinaculum or medial patellofemoral ligaments cause apprehension from repetitive subluxation events or from a previous dislocation, or from a congenital condition. Most patellar subluxations and dislocations occur toward the lateral side of the knee joint. This abnormal amount of lateral passive mobility is due to tearing of the medial patellofemoral ligament and the medial patellomeniscal ligament that contribute 23-80% and 22% of the lateral static restraint, respectively.45
Another much less common problem is that of the reverse apprehension that occurs with excessive passive patellar mobility in the medial direction. One must be very astute to pick out this pathology as it is rare and may be seen following patellar malalignment surgical procedures used to help resolve lateral translation pathology. The patient may have had an overzealous tibial tubercle transfer or had their vastus lateralis transected at the time of a lateral release, and an overly tight and/or malpositioned medial patella femoral ligament graft.46-51 Underlying hyperlaxity, trochlear dysplasia, and deficient vastus lateralis musculature may also play a role in the development of medial patellofemoral subluxation. The patients with medial subluxation will report that the patella shifts laterally, invoking the clinician to assume that lateral subluxation is the pathology. However what the patient is actually feeling is the medial subluxed patella dramatically shifting laterally into the trochlea during early knee flexion.49 The key finding with medial patellar instability is a reproduction of the patient's symptoms with the medial patella subluxation test. This is done with starting the test in full knee extension. The clinician applies a medial translational force to the lateral side of the patella. As the knee is flexed somewhere in the first 30 degrees the patient will report symptomatic pain, instability as the patella snaps laterally back into the trochlear groove.52 The gravity subluxation test is performed with the patient in the sidelying position, with the suspected leg abducted in the air. The patient is then asked to contract their quadriceps. A positive test is shown by the inability to pull the subluxed patella laterally into the trochlear groove and would be indicative of laxity of the lateral retinaculum and or detachment of the vastus lateralis from the patella.51
The opposite of excessive laxity is patellar hypomobility. Lateral deep retinacular tightness is a condition that is very common in those with anterior knee pain. The lateral retinacular structures also include contributions from the IT band and the lateral patellofemoral and patellotibial ligaments. The force vector of these tissues is more posterior than lateral, which is why when tight they create more of a tilt than a lateral glide. The patellar tilt test assesses the deep retinacular fibers. This test is performed with the knee in full extension. With the patellar entered into the trochlea, even at 30-40 degrees of flexion create such a tightness of the deep retinacular fibers that no tilt would be possible. While the clinician is on the lateral side of the knee to be tested, they will push posteriorly on the medial anterior border while pushing anterior with the thumbs under the lateral border to assess whether the patella corrects its tilt to at least neutral (Figure 23). If the patient's patella is unable to tilt back to neutral it is indicative of excessive lateral tightness and the potential to have excessive lateral pressure syndrome. Comparisons to the opposite noninvolved side is extremely important as wide ranges of variation of tightness are the norm. The patella should tilt 15 degrees with both medial and lateral tilts.
Figure 23.
Examination test to determine patellar tilt for assessment of the deep patellar retinacular fibers. Test for tightness of deep lateral structures is done by attempting to tilt in a medial direction. Inability to obtain a neutral position indicates tightness of deep lateral structures.
Clarkes “patellar grind” test has been described as a confirmatory test for patellar chondromalacia. In this test the patella is compressed against the trochlea manually while the clinician asks the patient to contract their quadriceps. A positive test is indicated by an exacerbation of the patient's symptoms. Nunes et al2 and Doberstein et al52 have demonstrated that the patellar grinding and apprehension test (eg, Clarkes Test) have low sensitivity and limited diagnostic accuracy for patellofemoral pain syndrome. Furthermore, from a clinical perspective, performing the test creates a lot of false positive findings and can exacerbate the patient's condition, therefore should not be used.
Screening for Knee Ligaments (Rule-Out Instability)
Testing of the four major knee ligaments can be performed in supine and is imperative to rule out major ligament instability that could create anterior knee pain. There is a philosophy that NO ONE TEST IS THE BEST TEST to implicate or rule out a structure. Consequently, the authors recommend performing the Anterior Drawer and Lachman's Test to screen the ACL; Posterior Drawer and Clancy's Step up Test to screen for the PCL; the rotary instability tests in 70 Degrees of flexion to rule out rotational instabilities which could influence patellofemoral tracking and resultant patellofemoral pain; MCL valgus stress test and 0 and 30 degrees; and the varus stress test at 0 and 30 degrees.
Screening for Meniscus
Although not commonly associated with patellofemoral symptoms, using the McMurray's and dynamic McMurray's test to screen for potential meniscus involvement should be performed to rule out any co-morbidities.
SIDE LYING EXAMINATION
Flexibility Testing
Iliotibial band and TFL flexibility is assessed with the Ober's test and modified Ober's test. The patient is positioned in side-lying with the affected side up. The bottom leg is passively flexed slightly for stability. The tested extremity is passively abducted and extended with either the knee straight or flexed. The clinician slowly lowers the leg toward the table. If a contracture is present, the thigh will remain elevated past horizontal. Testing with the knee flexed was the original description of this test, however the iliotibial band passes over the greater trochanter and has a greater stretch placed on it when the knee is fully extended.
Strength Testing (Hip Abductors, Adductors)
Strength testing of the hip abductors is performed in side lying. With the bottom leg slightly flexed for stability, the top hip is brought into slight abduction. Resistance is given toward the table with the clinician's hand on distal thigh near the knee joint. Replication of same placement of resistance is important for reassessment at a later date to ensure same moment arm is placed on the extremity. With the top leg in front of the bottom, the patient is asked to adduct the hip to be tested. Pressure is given on distal thigh in direction of table.
PRONE EXAMINATION
Flexibility Testing
Flexibility of the quadriceps is tested in the prone position. Because the rectus femoris crosses both the hip and the knee joint it can easily become passively insufficient. Ely's test is performed prone by placing the hip in neutral or extension (Figure 24), which places the rectus femoris on stretch proximally at the hip and again distally as the knee is further flexed.7 A common compensatory indicative of an inflexible rectus femoris while in this position is seen by the hip flexing due to tightness. Some clinicians will also evaluate hip rotation in the prone position because the anterior capsule is tight which replicates the more functional standing or walking positions.
Figure 24.
Ely's prone test for rectus femoris flexibility is done with hip in neutral extension.
Strength Testing (Hip Extensors, Knee Flexors)
The hip extensor muscle group is tested with the patient prone. The hip is extended slightly off of the supporting surface. Pressure in the downward direction is given just proximal to the knee joint. When the knee is completely extended testing would include both hamstrings and hip extensors. Testing with the knee flexed would just test the hip extensors. The hamstrings are tested in the prone position to assess the muscle's function against gravity. By rotating the knee, the medial or lateral hamstrings can be selectively biased during the manual muscle testing.
Isokinetic Testing
If it is not contraindicated, and if isokinetic equipment is available, then dynamic muscle testing is performed in an open kinetic chain position. The rationale for such testing is because so many patients with knee conditions have significant deficits in the quadriceps strength. By performing objective dynamic muscle performance documentation of the muscle groups allows for bilateral muscle comparison, unilateral ratios, allometric scaling of the test results, and power measurements, such as time rate of torque development, torque acceleration energy, etc.
FUNCTIONAL TESTING
In order to determine if a patient is safe to return to activity, activity testing should be performed, whether it be for ADLs, an ergonomic assessment, or sports performance testing. The authors recommend using a functional testing algorithm that is a systematic qualitative and quantitative functional assessment of the patient's performance abilities.54 Patients are stratified into different categories based on their activity levels. Then all patients must meet all the basic testing criteria described throughout this article such as full strength, flexibility and ROM. There are many functional tests that can be used, however, the authors recommend a sequence of the following: 2-legged jump, single-leg hop, Lower Extremity Functional Test (LEFT), and then functional specificity testing.
To begin, the 2-legged jump test is used to help the patient prepare for the concentric propulsive push-off motion and more importantly the eccentric deceleration landing phase. The patient is always instructed to perform four gradient (25, 50, 75, 100%) effort warm-ups for the jump and hop tests. It serves as a screening to make sure the patient is capable of performing the tests safely. Furthermore, having the patient perform a maximum effort test provides a positive transfer of learning and consequently increases the reliability of the test results. The data is evaluated by allometric scaling and normalizing the data relative to the patient's height. Normative values are included in Table 6.
Table 6.
Suggested Descriptive Normative Data for Functional Tests
| Test | Males Absolute | Males Allometric Scaled | Female Absolute | Female Allometric Scaled |
| Double leg jump | Sports Specific Normative data | 100% height ±10% | Sports Specific Normative data | 90% height ± 10% |
| Single leg hop | Limb symmetry index (10%) | 90% height ± 10% | Limb symmetry index (10%) | 80% height ± 10% |
| LEFT test | Average 100s (range: 90-125s) | Not applicable | Average 135s (range: 120-150s) | Not applicable |
Following the double-legged jump test, also known as a single leg hop test is performed because it is the recommended functional test by the IKDC form. There are several variation of the hop test including the single hop, triple hop, timed hop, and criss-cross (zig-zag) hop. These authors also think this test is an important psychological test for the patient to be able to eccentric land with deceleration on the involved side. The authors evaluate the results based on a bilateral comparison for limb symmetry and allometric scaling to normalize to the patient's height. The norms are listed in Table 6.
The final functional test is the LEFT test.55-60 The purpose of the LEFT test is to incorporate many different lower extremity movement patterns into one test which replicates many activities of functional performance. Important aspects of the test are: 1) subjects perform the test in all directions, 2) there is a deceleration component inherent in the test, and 3) it incorporates a fatigue factor. Most return to play tests are performed in the “fresh” state. Studies have demonstrated that when patients performed a hop test when not fatigued, 100% of the patients passed the test following ACL reconstructions.61-65 However, when the tests were performed in the fatigued state, approximately 70% of the patients failed the tests. Normative data for the LEFT test are included in Table 6.
Imaging
Often imaging studies are indicated in order to facilitate the clinical examination and diagnosis of patellofemoral pain. Commonly used radiographic views may include: AP, Lateral, Long Leg Standing, Insall-Salvanti, Merchant, and or Sunrise views. In selected cases the MRI may be indicated to assist with the definitive diagnosis. Particularly assessing the chondral surfaces of the patellofemoral joint and any soft tissue abnormalities; such as plica syndrome, hoffa's syndrome, retinacular neuroma's, etc.
Patient Reported Outcomes
Over the past 10-15 years it has become commonplace to utilize patient reported outcomes so that clinicians can better determine the amount of improvement in symptoms and function described from the perspective of the patient. The authors of this manuscript utilize the Kujala Anterior Knee Pain Scale for orthopedic or sports medicine populations. Both Bennel and collegues66 and Crossley and collegues67 have reported adequate reliability of the Kujala scale for clinical use. More recently Ittenbach et al68 have reported to have high internal consistency, equivalence across short and long forms, acceptable standard errors of measurement and moderate to high criterion related validity with use of the Kujala scale.
CONCLUSIONS
Using the guidelines presented in this manuscript the sports physical therapist can utilize the suggestions for examination and define the complicated pathology known as patellofemoral joint dysfunction. Once a clearer diagnosis can be made using procedures outlined in this manuscript, the patient will be able to be treated more appropriately based on their classification of injury type. Because of the perplexity of this pathology it is critical to use a systematic, thorough and all-inclusive examination including careful review of both proximal and distal factors that could be contributing to this problem.
REFERENCES
- 1.Lankhorst NE Bierma-Zeinstra SM van Middelkoop M. Risk factors for patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2012;42(2):81-94. [DOI] [PubMed] [Google Scholar]
- 2.Nunes GS Stapait EL Kirsten MH de Noronha M Sanatos GM. Clinical test for diagnosis of patellofemoral pain syndrome: systematic review with meta-analysis. Phys Ther Sport. 2013;14(1):54-59. [DOI] [PubMed] [Google Scholar]
- 3.Fredricson M Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil. 2006;85(3):234-243. [DOI] [PubMed] [Google Scholar]
- 4.Crossley KM Stefanik JJ Selfe J, et al. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 1: Terminology, definitions, clinical examination, natural history, patellofemoral osteoarthritis and patient-reported outcome measures. Br J Sports Med. 2016;50:839-843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crossley KM van Middelkoop M Callaghan MJ Collins NJ Rathleff MS Barton CJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: Recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions. Br J Sports Med. 2016;50:844-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lester JD Watson JN Hutchinson MR. Physical examination of the patellofemoral joint. Clin Sports Med. 2014;33:403-412. [DOI] [PubMed] [Google Scholar]
- 7.Magee DJ. Orthopedic Physical Assessment, 6th ed Elsevier; St. Louis, MO, 2014. [Google Scholar]
- 8.Wilk KE Davies GJ Mangine RE Malone TR. Patellofemoral disorders: Classification system and clinical guidelines for non-operative rehabilitation. J Orthop Sports Phys Ther. 1998;28:307-322. [DOI] [PubMed] [Google Scholar]
- 9.Bruce WD Stevens PM. Surgical correction of miserable malalignment syndrome. J Pediatr Orthop. 2004;24(4):392-396. [DOI] [PubMed] [Google Scholar]
- 10.Grelsamer RP McConnell J. The Patella: A Team Approach. Aspen Publishers, Gaithersburg, MD: 1998. [Google Scholar]
- 11.Fulkerson JP. Disorders of the Patellofemoral Joint. 4th ed Lippincott Williams and Wilkins, Philadelphia, PA, 2004. [Google Scholar]
- 12.Smith LK Weiss W Lehmkuhl LD. Brunnstrom's Clinical Kinesiology, 5th ed FA Davis, Philadelphia, PA, 1996. [Google Scholar]
- 13.Schulthies SS Francis RS Fischer AG Van de Graaff KM. Does the Q-angle reflect the force on the patella in the frontal plane. Phys Ther. 1995; 75:24-30. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher J Tierney P Murray P, et al. The infrapatellar fat pad: anatomy and clinical correlations. Knee Surg Sports Traumatol Arthrosc. 2005;13:268-272. [DOI] [PubMed] [Google Scholar]
- 15.Smith TO Hunt JH Donell ST. The reliability and validity of the Q-angle: A systematic review. Knee Surg Sports Traumatol Arthrosc. 2008;16(12):1068-1079. [DOI] [PubMed] [Google Scholar]
- 16.Livingston LA. The quadriceps angle: a review of the literature. J Orthop Sports Phys Ther. 1998;28:105-109. [DOI] [PubMed] [Google Scholar]
- 17.Golightlyy YM Allenzx KD Helmickk CG Renner JB Jordany JM. Symptoms of the knee and hip in individuals with and without limb length inequality. Osteoarthr Cart. 2009. 17:596-600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sell KE Verity TM Worrell TW Pease BH Wiglesworth J. Two measurements of assessing subtalar joint position: a reliability study. J Orthop Sports Phys Ther. 1994;19:162-176. [DOI] [PubMed] [Google Scholar]
- 19.Wukich DK Tuason DA. Diagnosis and treatment of chronic ankle pain. J Bone Joint Surg Am. 2010;92:2002-2016. [Google Scholar]
- 20.Mueller MH Host JV Norton BJ. Navicular drop a composite measure of excessive pronation. J Am Pod Med Assoc. 1993;83:198-202. [DOI] [PubMed] [Google Scholar]
- 21.Loudon J Jenkins W Loudon KL. The relationships between static posture and ACL injury in female athletes. J Orthop Sports Phys Ther. 1996;24:91-97. [DOI] [PubMed] [Google Scholar]
- 22.Shrader JA Poporich JM Gracey GC, et al. Navicular drop measurement in people with rheumatoid arthritis: interrater and intrarater reliability. Phys Ther. 2005;85:656-664. [PubMed] [Google Scholar]
- 23.Crossley KM Zhang WJ Schache AG Bryant A Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866-873. [DOI] [PubMed] [Google Scholar]
- 24.Rabin A Kozol Z Moran U Efergan A Geffen Y Finestone AS. Factors associated with visually assessed quality of movement during a lateral step-down test among individuals with patellofemoral pain. J Orthop Sports Phys Ther. 2014;44(12):937-946. [DOI] [PubMed] [Google Scholar]
- 25.Nakagawa TH Moriya ETU Maciel CD Serrao FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2012;42(6):491-501. [DOI] [PubMed] [Google Scholar]
- 26.Aslan UB Celik E Cavlak U, et al. Evaluation of interrater and intrarater reliability of Beighton and Horan joint mobility index. Fizyoterapi Rehabilitasyon. 2006;17(3):113-119. [Google Scholar]
- 27.Boyle KL Witt P Riegger-Krugh C. Intrarater and interrater reliability of the Beighton and Horan joint mobility index. J Athl Train. 2003;28(4):281-285. [PMC free article] [PubMed] [Google Scholar]
- 28.Juul-Krstensen B Rogind H Jensen DV, et al. Inter-examiner reproducibility of tests and criteria for generalized joint hypermobility and benign joint hypermobility syndrome. Rheumatology 2007;46:1835-1841. [DOI] [PubMed] [Google Scholar]
- 29.Sendur OF Gurer G Yildirim T Ozturk E Aydeniz A. Relationship of Q angle and joint hypermobility and Q angle values in different positions. Clin Rheumatology. 2006;25(3):304-308. [DOI] [PubMed] [Google Scholar]
- 30.Quatman CE Ford KR Myer DG Paternal MV Hewett TE. The effects of gender and pubertal status on generalized joint laxity in young athletes. J Sci Med Sport. 2008;11(3):257-263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hughston JC Walsh WM Puddu G. Patellar Subluxation and Dislocation. WB Saunders; Philadelphia, PA: 1984. [Google Scholar]
- 32.Kolowich PA Paulos LE Rosenberg TD Farnsworth S. Lateral release of the patella: Indications and contraindications. Am J Sports Med. 1990;18(4):359-365. [DOI] [PubMed] [Google Scholar]
- 33.Nicholas JA Strizak AM Veras G. A study of thigh muscle weakness in different pathologic states of the lower extremity. Am J Sports Med. 1976. 4(6):241-248. [DOI] [PubMed] [Google Scholar]
- 34.Pappas E Wong-Tom WM. Prospective predictors of patellofemoral pain syndrome: A systematic review with meta-analysis. Sports Health. 2012;4(2):115-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boling MC Padua DA Marshall SW Guskiewicz K Pyne S Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the joint undertaking to monitor and prevent ACL injury (JUMP-ACL) cohort. Am J Sports Med. 2009;37(11):2108-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kooiker L Van De Port IG Weir A Moen MH. Effects of physical therapist-guided quadriceps-strengthening exercises for the treatment of patellofemoral pain syndrome: a systematic review. J Orthop Sports Phys Ther. 2014;44(6):391-? [DOI] [PubMed] [Google Scholar]
- 37.Lankhorst NE Bierma-Zeinstra SM van Middeldoop M. Factors associated with patellofemoral pain syndrome: A systematic review. Br J Sports Med. 2013;47(4):193-206. [DOI] [PubMed] [Google Scholar]
- 38.Post WR Fulkerson J. Knee pain diagrams: correlation with physical examination findings in patients with anterior knee pain. Arthroscopy 1984;10(6):618-623. [DOI] [PubMed] [Google Scholar]
- 39.Fithian DC Mishra DK Balen F Stone ML Daniel DM. Instrumented measurement of patellar mobility. Am J sports Med. 1995;23(5):607-615. [DOI] [PubMed] [Google Scholar]
- 40.Skalley TC Terry GC Teitge RA. The quantitative measurement of normal passive medial and lateral patellar motion limits. Am J Sports Med. 1993;21:728-732. [DOI] [PubMed] [Google Scholar]
- 41.Fulkerson Hungerford DS. Disorders of the Patellofemoral Joint, 2nd ed Baltimore, MD: William and Wilkins, 1990. [Google Scholar]
- 42.Kujala UM Kvist M Osterman K, et al. Factors predisposing army conscripts to knee exertion injuries incurred in a physical training program. Clin Orthop 1986;210;203-212. [PubMed] [Google Scholar]
- 43.Post WR. History of Physical Examination. In: Fulkerson JP. Disorders of the Patellofemoral Joint, 4th ed Lippencott Williams and Wilkins, Philadelphia, PA, 2004. [Google Scholar]
- 44.Ahmed CS McCarthy M Gomez JA, et al. The moving patellar apprehension test for lateral patellar instability. Am J Sports Med 2009;37:791-796. [DOI] [PubMed] [Google Scholar]
- 45.Conlan T Garth WP Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682-693. [DOI] [PubMed] [Google Scholar]
- 46.Aksahin E Yumrukcal F Yuksel HY Dogruyol D Celebi L. Role of pathophysiology of patellofemoral instability in the treatment of spontaneous medial patellofemoral subluxation: a case report. J Med Case Rep, 2010;4:148-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bollier M Fulkerson J Cosgarea A Tanaka M. Technical failure of medial patellofemoral ligament reconstruction. Arthroscopy 2011; 27(8): 1153-1159. [DOI] [PubMed] [Google Scholar]
- 48.Hughston JC Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med 1988; 16:383-388. [DOI] [PubMed] [Google Scholar]
- 49.McCarthy MA Boolliwe MJ. Medial patella subluxation: Diagnosis and treatment. Iowa Orthop J 2015;35:26-33. [PMC free article] [PubMed] [Google Scholar]
- 50.Miller PR Klein RM Teitge RA. Medial dislocation of the patella. Skeletal Radiol 1991;20:429-431. [DOI] [PubMed] [Google Scholar]
- 51.Nonweiler DE DeLee JC. The diagnosis and treatment of medial subluxation of the patella after lateral retinacular release. Am J Sports Med. 1994; 22(5):680-686. [DOI] [PubMed] [Google Scholar]
- 52.Fulkerson JP. A clinical test for medial patella tracking. Tech Orthop. 1997;12:144. [Google Scholar]
- 53.Doberstien ST Romeyn RL Reineke DM. The diagnostic value of Clarke sign in assessing chondromalacia patella. J Athl Train. 2008;43(2):190-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davies GJ Zilmer D. Functional progression of a patient through a rehabilitation program. Orthop Phys Ther Clin N Am. 2000;9(2):103-118. [Google Scholar]
- 55.Brumitt J Heiderscheit BC Manske RC Niemuth PE Rauh MJ. Lower extremity functional tests and risk of injury in division III collegiate athletes. Int J Sports Phys Ther. 2013; 8:216-227. [PMC free article] [PubMed] [Google Scholar]
- 56.Brumitt J Heiderscheit BC Manske RC Niemuth PE Rauh MJ. Off-season training habits and preseason functional test measures of division III collegiate athletes: a descriptive report. In J Sports Phys Ther. 2014;9:447-455. [PMC free article] [PubMed] [Google Scholar]
- 57.Brumitt J Heiderscheit BC Manske RC Niemuth PE Rauh MJ. The lower-extremity functional test and lower-quadrant injury in NCAA division III athletes: a descriptive and epidemiologic report. J Sport Rehab. 2016;25(3):219-226. [DOI] [PubMed] [Google Scholar]
- 58.Manske R Reiman M. Functional performance testing for power and return to sport. Sports Health. 2013;5:244-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Reiman MP Manske RC. Functional Testing in Human Performance. Champaign, IL: Human Kinetics, 2009. [Google Scholar]
- 60.Tabor MA Davies GJ Kernozek TW Negrete RJ Hudson V. A multicenter study of the test-retest reliability of the lower extremity functional test. J Sport Rehabil. 2002;11(3):190-201. [Google Scholar]
- 61.Augustsson J Thomee R Karlsson J. Ability of a new hop test to determine functional deficits after ACL-R. Knee Surg Sports Traumatol Arthrosc. 2004;12(5):350-260. [DOI] [PubMed] [Google Scholar]
- 62.Augustsson J Thomee R Linden C, et al. Single-leg hop testing following fatiguing exercise: reliability and biomechanical analysis. Scand J Med Sci Sports. 2006;16(2):111-120. [DOI] [PubMed] [Google Scholar]
- 63.Frisch A Urhausen A Seil R Croisier JL Windal T Theisen D. Association between preseason functional tests and injuries in youth football: a prospective follow-up. Scand J Med Sci Sports. 2011;21(6):e468-476. [DOI] [PubMed] [Google Scholar]
- 64.Ortiz A Olson SL Etnyre B, et al. Fatigue effects on knee joint stability during two jump tasks in women. J Strength Cond Res. 2010;24(4):1019-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Orishimo KF. Adaptations in single-leg hop biomechanics following ACL-R. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1587-1593. [DOI] [PubMed] [Google Scholar]
- 66.Bennell K Bartam S Crossley K Green S. Outcome measures in patellofemoral pain syndrome: test retest reliability and inter-relationships. Phys Ther Sport. 2000;1(2):32-41. [Google Scholar]
- 67.Crossley KM Bennell KL Cowan SM Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815-822. [DOI] [PubMed] [Google Scholar]
- 68.Ittenback RF Huang G Barber Foss KD Hewett TE Myer GD. Reliability and validity of the anterior knee pain scale: Applications for use as an epidemiologic screener. PLOS one. 2016;11(7):e0159204 doi:10.1371/journal.pone.0159204. [DOI] [PMC free article] [PubMed] [Google Scholar]