Abstract
Patellofemoral instability is a painful and commonly recurring condition, which often must be managed surgically. Diagnosis can be aided by the use of a variety of physical exam signs, such as the Q angle, Beighton hypermobility score, glide test, J sign, patellar tilt test, and apprehension test. Imaging modalities including x-ray, CT, and MRI guide both diagnosis and management by revealing trochlear dysplasia, bony malalignment, and ligamentous injury that contribute to instability. Following an initial patellar dislocation, nonoperative management with bracing and physical therapy is an acceptable option, despite limited evidence that operative management may improve functional outcome and reduce recurrent dislocations.
For recurrent dislocations, operative management is indicated, and the appropriate procedure depends on the patient's anatomy and the cause of instability. Reconstruction of the medial patellofemoral ligament (MPFL) restores the primary soft tissue restraint to lateral patellar dislocations, and can be performed using a variety of techniques. In patients whose instability is related to bony malalignment, a tibial tubercle osteotomy is commonly performed to realign the extensor mechanism and establish proper patellar tracking. In patients with trochlear dysplasia, a trochleoplasty may be performed to create a sufficient groove for the patella to traverse. Often these procedures must be combined to address all causes of instability. The reported outcomes following all three of these procedures are generally very good, with the majority of patients experiencing functional improvements and a low rate of recurrent instability, although more large randomized controlled trials are needed to determine which techniques are most effective. The purpose of this clinical commentary is to provide an overview of the current methods employed by orthopedic surgeons to diagnose and manage patellar instability.
Level of Evidence
5
Keywords: knee instability, patella, trochlea, patellofemoral, patella alta, medial patellofemoral ligament
INTRODUCTION
Recurrent patellofemoral instability is a painful and often chronic condition following dislocation of the patella from its position within the trochlear groove. This condition has been estimated to affect 5.8 per 100,000 individuals and is more prevalent among females and 10-17 year olds (29 per 100,000).1 Once a single dislocation has occurred, patients are nearly seven times more likely to experience subsequent dislocations.1 Patellar dislocations are commonly associated with damage to articular cartilage, which can lead to chronic knee pain.2,3 Patellar instability has been associated with a number of anatomical factors including: ligamentous laxity, genu valgum, femoral anteversion, excessive tibial torsion, trochlear dysplasia, patella alta, and insufficiency or rupture of the medial patellofemoral ligament (MPFL). Patellofemoral instability often responds poorly to nonoperative management and must be addressed surgically. The purpose of this clinical commentary is to provide an overview of the current methods employed by orthopedic surgeons to diagnose and manage patellar instability.
CLINICAL EVALUATION
History and Physical Exam
The first step in managing a patient with patellofemoral instability is to perform a thorough clinical evaluation. Critical elements of the patient's history include the precise mechanism of injury and whether this was their first dislocation. If patients have experienced recurrent instability, they should be questioned about the frequency, mechanism, duration, and prior management of these events.
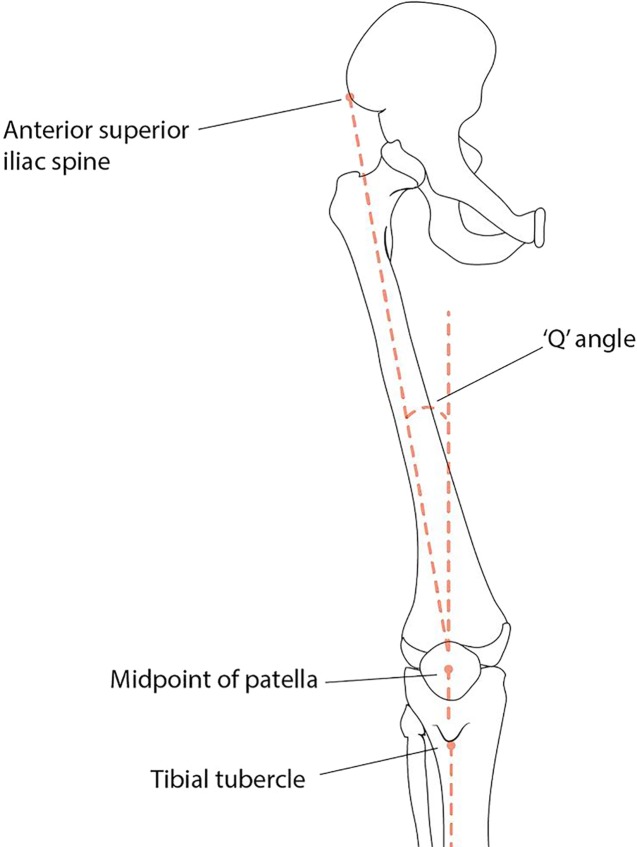
There are a number of physical exam signs and maneuvers which can help diagnose patellofemoral instability.4 Knee alignment should be assessed, particularly for presence of genu valgum. The Q angle is an important indicator of knee alignment; it comprises the angle between a line drawn from the anterior superior iliac spine to the center of the patella and line from the center of the patella to the tibial tubercle (Figure 1). This angle is typically larger in women, 15-20 ° compared to 10-15 ° in men. An abnormally large Q angle imposes a lateral direction of force on the extensor mechanism, causing a predisposition for lateral patellar instability and dislocation. The Beighton hypermobility score can be obtained to asses for overall generalized ligamentous laxity.5 This involves a 9-point scale on which a score greater than 5 indicates hypermobility; one point is assigned for each of the following findings: passive hyperextension of each small finger >90 °, passive abduction of each thumb to the volar/radial surface of the forearm, hyperextension of each elbow >10 °, hyperextension of each knee >10 °, and forward flexion of the trunk with the ability to place both palms flat on the floor with full knee extension.5 The passive patellar glide test is a simple maneuver to evaluate for patellar hypermobility. With the patient supine and the knee in extension, the examiner pushes the patella medially and laterally; the patella is divided into four vertical quadrants, and a glide longer than the width of three quadrants is consistent with hypermobility. The J-sign is demonstrated when the patient sits on the edge of the examination table and moves their knee from a position of flexion to extension; in patients with a tight lateral retinaculum, the patella may appear to shift laterally as the knee extends. The patellar tilt test can also be performed to identify a tight lateral retinaculum. With the patient supine and the knee in extension, the examiner pushes on the patella in an attempt to flip the lateral edge upwards. In a normal patient, the lateral edge may elevate up to 20 °; however, in a patient with a tight lateral retinaculum, the lateral edge will not elevate past neutral. The apprehension test is another useful test for instability; it is performed with the patient supine and the knee extended. The examiner pushes the patella laterally as though to dislocate it. The test is considered positive when the patient verbally expresses apprehension or involuntarily contracts the quadriceps to maintain stability. Finally, Bassett's sign may indicate a rupture of the MPFL; it consists of pain with palpation of the adductor tubercle, which is the femoral attachment of the MPFL.4
Figure 1.
The Q angle can be used to assess knee alignment.
Diagnostic Imaging
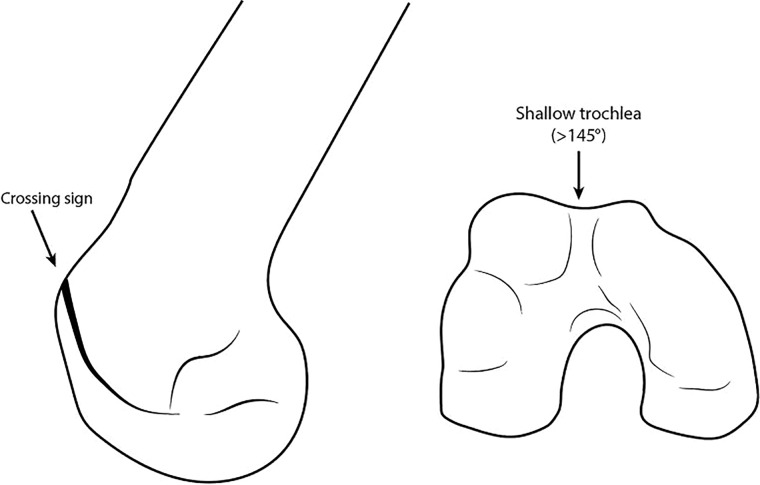
Imaging also plays a critical role in the diagnosis and management of patellofemoral instability. Imaging should begin with weight bearing anteroposterior (AP), posteroanterior (PA) (45 ° flexion), and true lateral (30 ° flexion) radiographs of the knee. AP and PA views are valuable for assessing knee alignment and congruity, while the lateral view provides insight into patellofemoral anatomy. Trochlear dysplasia can be appreciated on a true lateral view. The crossing sign occurs when a line drawn along the floor of the trochlear groove crosses the anterior surface of the femoral condyles (Figure 2).6,7 Other signs of trochlear dysplasia include a trochlear depth less than 4 mm and an anterior trochlear bump greater than 3 mm.7
Figure 2.
The crossing sign and a shallow trochlea are indicators of trochlear dysplasia.
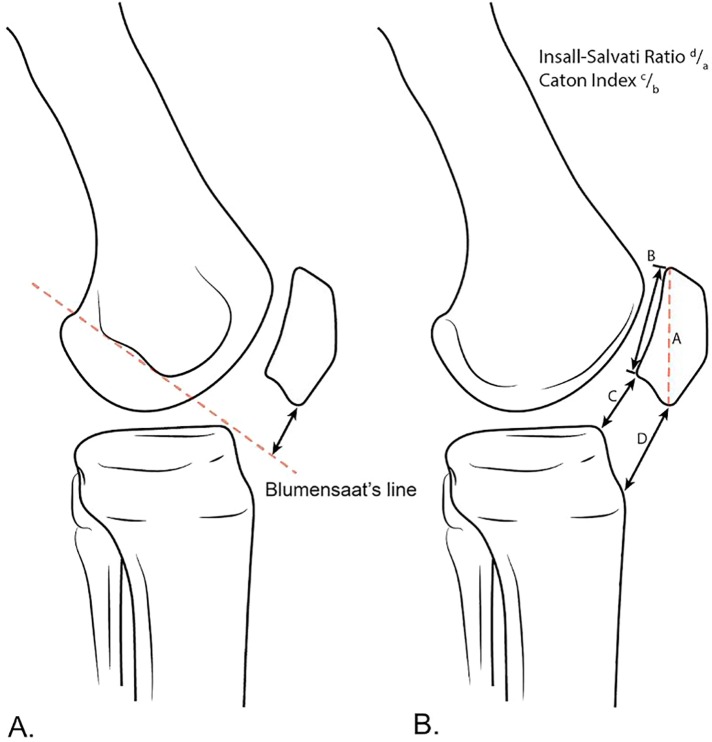
Patella alta can also be noted on the lateral view. There are a number of methods for measuring patella alta.8 On a true lateral view, Blumensaat's line (along the roof of the intercondylar femoral notch) will normally meet the inferior pole of the patella (Figure 3A). The Insall-Salvati index is obtained by dividing the length of the patellar tendon by the length of the patella; the normal range is between 0.8 and 1.2, with an index >1.2 indicating patella alta (Figure 3B).9 Alternative methods for identifying patella alta include the Caton-Deschamps, Blackburne-Peel, and the modified Insall-Salvati indices.10-12
Figure 3.
Blumensaat's line (A), the Insall-Salvati ratio, and Caton index (B) can be used to identify patella alta.
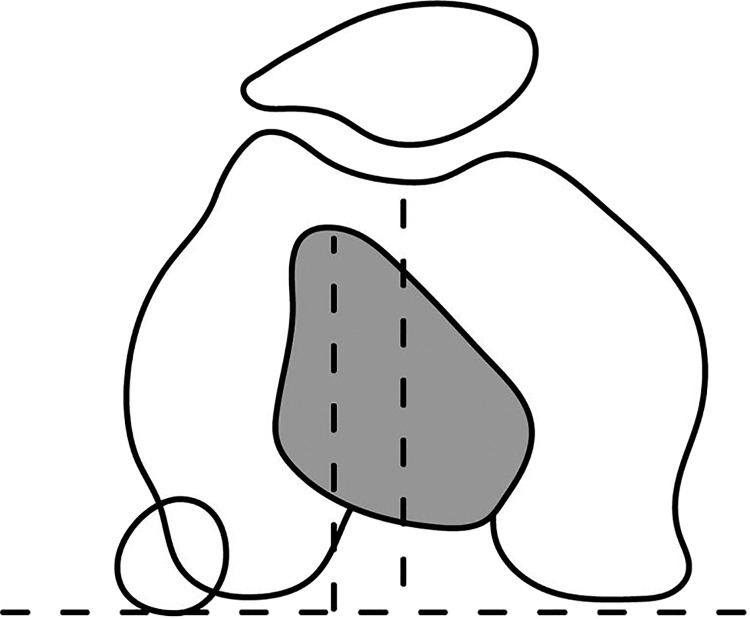
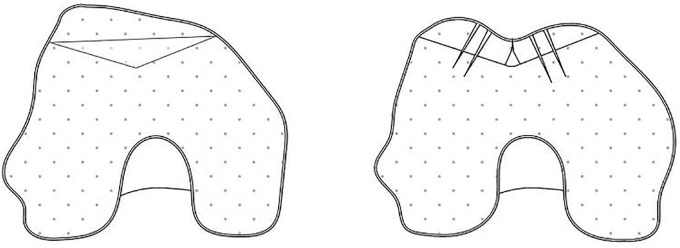
A Merchant view is also useful for identifying patellar tilt, trochlear dysplasia, and lateral subluxation; this view is obtained with the knee in 30 ° flexion and the beam directed distally to view the patella as it sits within the trochlear groove.13 Patellar tilt can be evaluated by measuring the lateral patellofemoral angle, which is formed by a line drawn between the anterior points of the medial and lateral femoral condyles, and a line that goes along the lateral articular facet of the patella (Figure 4B). Normally these lines open laterally; however, the lines may be parallel or open medially in the presence of abnormal patellar tilt. The sulcus angle is the angle between two lines drawn from the medial and lateral condyles to the deepest part of the intercondylar sulcus (Figure 4C).14 A normal sulcus angle is approximately 130-140 °; abnormal values have been associated with trochlear dysplasia.14,15 The congruence angle is measured by drawing a line that bisects the sulcus angle and another line from the apex of the sulcus angle to the deepest point of the patellar articular surface; the angle between these two lines is considered negative if it is medial to the line bisecting the sulcus and positive if it is lateral to this line (Figure 4A). An angle greater than -6 ° has been associated with lateral patellar subluxation.15
Figure 4.
The congruence angle (A), lateral patellofemoral angle (B), and sulcus angle (C) are used to evaluate patellar tilt.
Advanced imaging modalities such as magnetic resonance imaging (MRI) and computed tomography (CT) provide valuable information that may guide surgical interventions. Osseous anatomy and limb alignment can be assessed by both MRI and CT. The tibial tuberosity-trochlear groove (TT-TG) distance is a useful indicator of malalignment (Figure 5). This can be assessed by superimposing two axial images of the tibial tuberosity and the trochlear groove and measuring the medial-lateral distance between the tibial tuberosity and the deepest point of the trochlear groove. A TT-TG distance > 15-20 mm is generally considered abnormal; an increased TT-TG has been associated with instability, as it represents a lateralized insertion of the patellar tendon relative to the trochlear groove.7 Additionally, MRI is useful for identifying injuries to the MPFL and articular cartilage.3,16 MRI may reveal whether the etiology of a patient's instability is bony or ligamentous in nature, dictating which surgical intervention is most appropriate.
Figure 5.
The TT-TG distance can be used to determine the presence of bony malalignment.
TREATMENT
Nonoperative Management
Conservative management is most appropriate in patients who have experienced their first episode of instability and have no evidence of an osteochondral injury. A variety of rehabilitation protocols have been described, ranging from full mobilization with a bandage or neoprene sleeve to short-term immobilization with a brace or a cast.17-21 Physical therapy is also commonly recommended to improve neuromuscular control of the knee; exercises should focus on stretching, range of motion, and strengthening, particularly of the quadriceps muscles.22 A number of small randomized controlled trials have compared the outcomes of nonoperative versus operative management of primary acute patellar dislocations.21,23-27 These studies have provided mixed results; some have reported no significant difference in the rate of recurrence or subjective functional outcome (Kujala score).23,26,27 However, others have reported significantly lower rates of recurrence and improved outcomes with surgery.21,24,25 A Cochrane meta-analysis reported a significant risk reduction for recurrent dislocation (RR = 0.53, 95% CI: 0.33-0.87) and higher Kujala scores (mean difference 13.93, 95% CI: 5.33-22.53) at 2-5 years for patients undergoing operative treatment; although the authors cautioned that the quality of this evidence was poor due to the limitations of available data.19 The overall rate of recurrence in this meta-analysis was 24% for nonoperative patients and 13% for operative patients at 2-5 years after initial injury.19 However, there is currently no consensus regarding the utility of nonoperative management, and it remains an acceptable option in patients with a primary acute patellar dislocation.
MPFL Reconstruction
The MPFL is a major soft tissue restraint to lateral patellar translation when the knee is in 0-30 ° of flexion, and it is commonly injured during a patellar dislocation.28,29 Its femoral origin lies 1 cm distal to the adductor tubercle, approximately 9 mm proximal and 13 mm posterior to the medial epicondyle, and it inserts along the superomedial border of the patella.30,31 Reconstruction or repair of the MPFL is indicated in patients who have a torn or incompetent MPFL and those who have recurrent instability without evidence of bony malalignment. Techniques utilizing various grafts and fixation methods have been described; however, the goal with all reconstructions is to restore the soft tissue restraint to lateral patellar motion.32-40 A diagnostic arthroscopy should also be performed before MPFL reconstruction to identify any osteochondral lesions or loose bodies.
One method of MPFL reconstruction involves a hamstring autograft being passed through a patellar bone tunnel.40 A hamstring tendon such as the gracilis or semitendinosus is harvested from the distal insertion on the pes anserinus. A bone tunnel is then drilled from the anterosuperior surface to the midpoint of the medial surface of the patella, and the graft is passed through. The femoral attachment of the MPFL is then identified proximal and posterior to a line joining the medial epicondyle and adductor tubercle. A hole is drilled into the femur, the graft is inserted, and its positioning is checked at 30 ° flexion. If the graft is tight in flexion, the insertion site is either too proximal or anterior; whereas, if the graft is loose in flexion, the insertion is either too distal or posterior. The graft should not be tensioned, as this may interfere with knee range of motion and impose harmful joint reactive forces. Once optimal positioning has been achieved, the graft is fixed into the femur using an interference screw.40
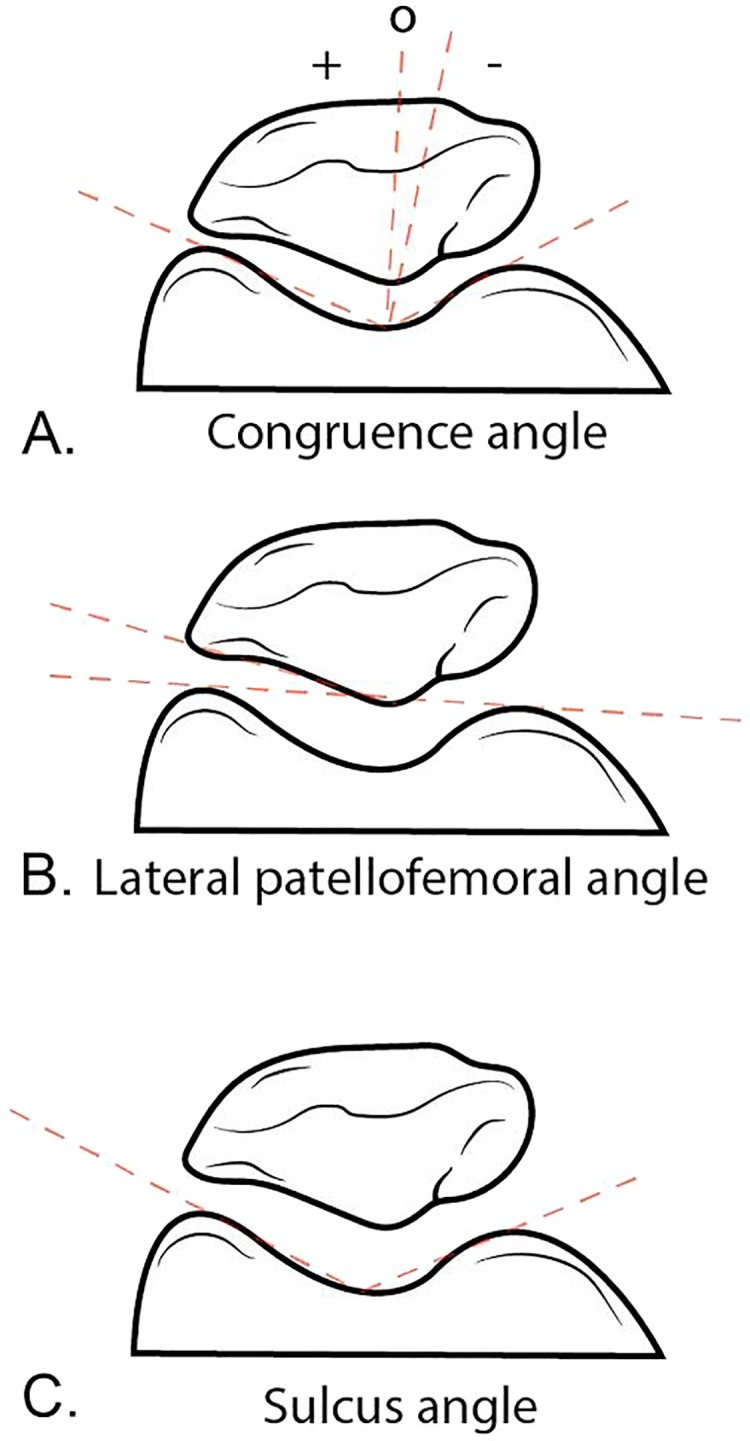
Another method also makes use of a hamstring autograft, except the graft is fixed to the patella with suture anchors rather than via a bone tunnel (Figure 6).40 In this procedure, a gracilis or semitendinosus graft is harvested from its distal insertion. The superomedial border of the patella is then exposed and two suture anchors are inserted. The graft is then placed through the suture anchors and tightened down. The femoral origin of the MPFL is identified, a hole is drilled, and the graft is positioned and fixed using an interference screw.40
Figure 6.
An illustration demonstrating MPFL reconstruction.
Alternatively, the quadriceps tendon may be used to create a new MPFL.37,40 This method involves separating a strip of the quadriceps tendon and releasing it proximally. The strip is then turned down on its distal attachment to the superior patella and tunneled medially through the prepatellar soft tissues. Again, the femoral MPFL origin is identified, a hole is drilled, and the graft is positioned and fixed using an interference screw.40,41
A number of studies have reported the outcomes of patients who have undergone some form of MPFL reconstruction.38,42-50 Outcomes are generally positive, with most authors reporting improvements in pain and functional outcome and a low incidence of recurrent dislocation. Complications most often arise from poor graft positioning, which can cause abnormal joint forces that result in cartilage damage, pain, and graft failure; other complications include patella fracture and stiffness.51 A meta-analysis of 320 patients in nine studies examining outcomes after MPFL reconstruction with a double-bundle hamstring tendon autograft reported a mean post-operative Kujala score of 92.0/100 (Standard error = 1.4, p = 0.001) and a complication rate of 12.5%, with stiffness being the most common complaint.42 However, the authors cautioned that the study was limited by small and limited design of many existing studies.42 Although authors generally report positive outcomes for MPFL reconstruction, the numerous techniques currently being used complicate the comparison between studies; more large randomized controlled trials are needed to determine whether any technique is superior to others.
Tibial Tubercle Osteotomy
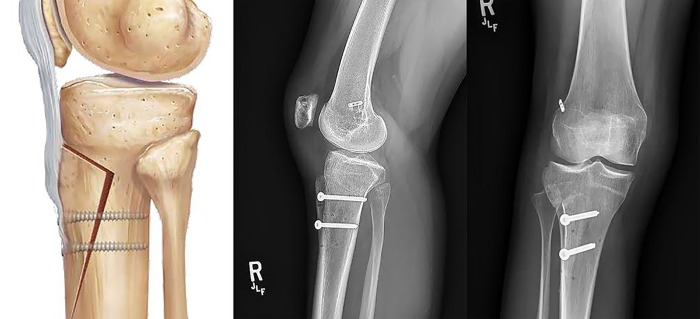
Tibial tubercle osteotomy is another option for treating patients with patellofemoral instability. This procedure involves altering the position of the tibial tubercle on the tibia, thereby realigning the extensor mechanism of the knee and correcting malalignment and instability.7,52,53 This procedure is indicated in patients with recurrent instability who have an increased TT-TG distance, patella alta, or high grade osteochondral lesions in the patellofemoral joint.
One of the most prominent surgical techniques is the anteromedialization osteotomy described by Fulkerson et al.54 This procedure is indicated for patients with instability due to maltracking, particularly those who have an increased TT-TG distance, patella alta, or patellofemoral osteochondral lesions. The procedure involves making a bony cut beneath the tibial tubercle, translating the fragment anteromedially 1-2 cm, and fixing it in place with screws (Figure 7).54 If patella alta is present, distalization may also be performed to restore proper patellar tracking.7,55,56
Figure 7.
An illustration and AP and lateral radiographs demonstrating a tibial tubercle osteotomy.
Medialization of the tubercle, also known as the Elmslie-Trillat procedure, is an option to address maltracking in patients without patella alta.57 Medialization is commonly performed in conjunction with MPFL reconstruction, and addresses instability by decreasing the lateral forces imposed by the quadriceps muscle across a malaligned patellofemoral joint.7,52,58 During this procedure, the tibial tubercle is detached and translated medially 1-2 cm to establish a normal TT-TG distance.52
The outcomes following tibial tubercle transfer have generally been reported to be very good.52,59-62 The authors of a systematic review reported a 7% recurrence rate in an analysis of 38 articles with 1182 surgeries.61 Complications are uncommon and can be minimized by proper surgical technique but include tibia fracture, overmedialization, nonunion, painful hardware, and wound complications.62-65
Trochleoplasty
Various procedures exist to alter the bony architecture of the trochlear groove, including proximal open trochleoplasty, deepening trochleoplasty, and trochlear lengthening osteotomy. Since trochlear dysplasia has been found in 85% of patients with recurrent patellofemoral instability, these surgical techniques may be of benefit for specific patients.7 Some experts consider trochleoplasty to be a salvage procedure and recommended in cases of severe trochlear dysplasia, given the associated pain and technical complexity.66 Specific indications include patients with a flat or convex lateral trochlear facet with hypoplasia of the medial trochlear facet, in the presence of normal or near normal articular cartilage. Normal or near normal articular cartilage within the trochlear groove is required to allow for successful reshaping.67,68 A trochleoplasty is contraindicated in patients with open physes or those with diffuse patellofemoral arthritis.68 This procedure is also contraindicated in patients with patellofemoral pain with no history of patellar dislocation.69
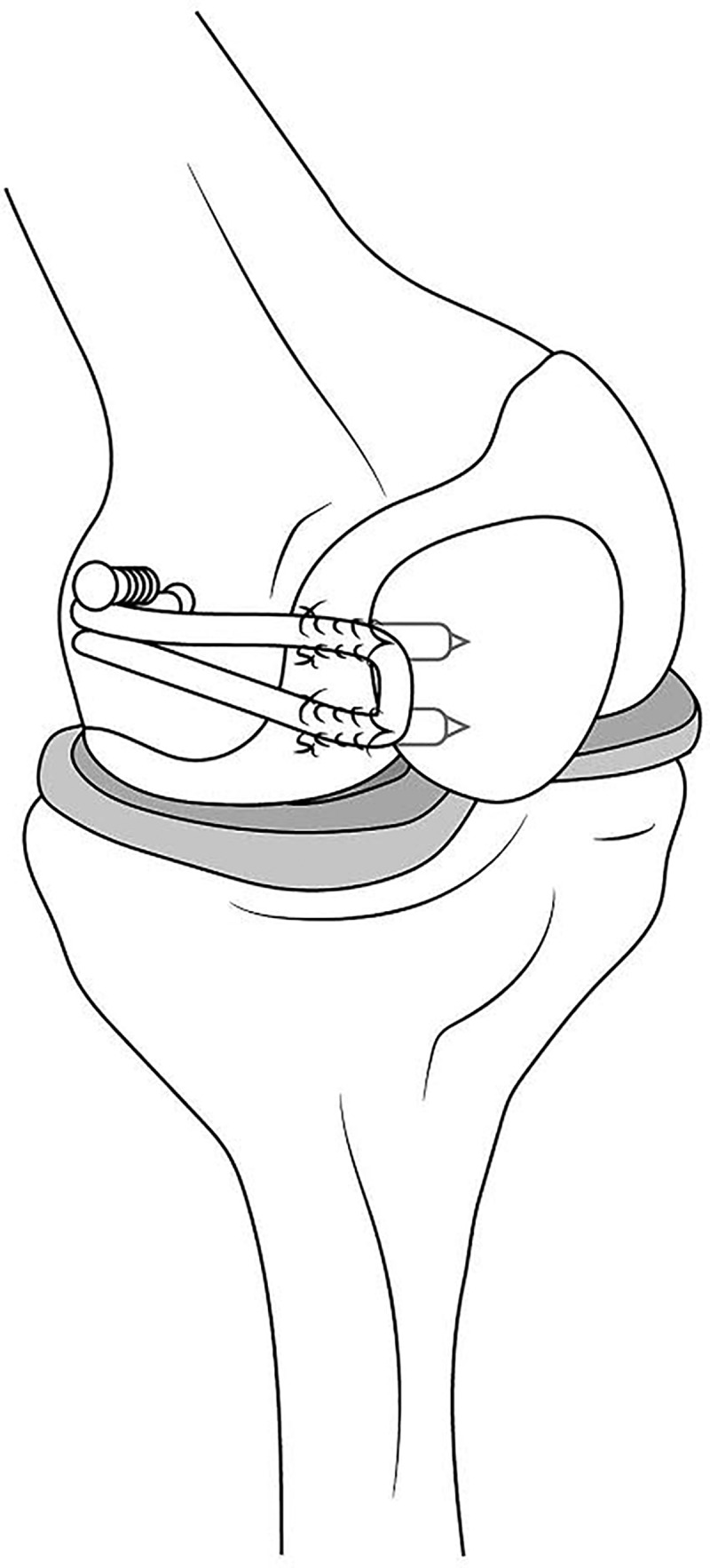
There are a number of trochleoplasty techniques that have been described in the literature. Proximal open trochleoplasty is used in cases where instability is related to a supratrochlear spur. The goal of this procedure is to create a concave surface on the proximal trochlea.70 A line is measured from the proximal trochlea distally to the top of the center of the intercondylar notch and a V-shaped outline is formed on the trochlear groove; this serves as a guide for the removal of cartilage and bone.67 A deepening trochleoplasty may be done to address a shallow trochlear groove. This procedure is performed by elevating the articular cartilage from the femur and using a burr to deepen the sulcus; the sulcus may also be narrowed and lateralized to improve patellofemoral tracking (Figure 8).69 The supratrochlear spur is also removed, and the cartilage flap is then secured with biocompression screws or suture anchors through the medial and lateral trochlear facets.68,69,71 In patients who have a hypoplastic lateral trochlea, a trochlear lengthening osteotomy may be appropriate.72 This procedure involves lengthening the lateral trochlear facet by means of an osteotomy; the facet may also be elevated by inserting cancellous autograft.67,70
Figure 8.
An illustration demonstrating a deepening trochleoplasty.
Complications associated with trochleoplasty include overcorrection, arthritis as a result of damage to the trochlear cartilage, and arthrofibrosis.68 There are varying reports with regard to the incidence of postoperative stiffness, which is likely correlated to the postoperative rehabilitation protocol instituted by the operating surgeon.73 The risk of intraarticular fracture at the patellofemoral joint has been described in the literature as well, and has a higher likelihood of occurrence in older patients with degenerative changes at baseline.53,73
SUMMARY
Following an initial patellar dislocation, nonoperative management with bracing and physical therapy is an acceptable option, despite limited evidence that operative management may improve functional outcome and reduce recurrent dislocations. For recurrent dislocations, operative management is indicated, and the appropriate procedure depends on the patient's anatomy and the cause of instability. Reconstruction of the MPFL restores the primary soft tissue restraint to lateral patellar dislocations, and can be performed using a variety of techniques. In patients whose instability is related to bony malalignment, a tibial tubercle osteotomy is commonly performed to realign the extensor mechanism and establish proper patellar tracking. In patients with trochlear dysplasia, a trochleoplasty may be performed to create a sufficient groove for the patella to traverse. Often these procedures must be combined to address all causes of instability. The reported outcomes following these three procedures are generally very good, with the majority of patients experiencing functional improvements and a low rate of recurrent instability. Many of the reported postoperative complications are related to technical errors in surgery that generate abnormal joint forces. Although there are many studies demonstrating the benefits of operative management for patellar instability, there is considerable heterogeneity among surgical techniques, and larger randomized controlled trials are needed to determine the most effective methods for managing this complex condition.
REFERENCES
- 1.Fithian DC Paxton EW Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114-21. [DOI] [PubMed] [Google Scholar]
- 2.Nomura E Inoue M Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy. 2003;19(7):717-21. [DOI] [PubMed] [Google Scholar]
- 3.Seeley MA Knesek M Vanderhave KL. Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatric Orthop. 2013;33(5):511-8. [DOI] [PubMed] [Google Scholar]
- 4.Smith TO Davies L O'Driscoll ML Donell ST. An evaluation of the clinical tests and outcome measures used to assess patellar instability. Knee. 2008;15(4):255-62. [DOI] [PubMed] [Google Scholar]
- 5.Beighton P Solomon L Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973;32(5):413-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dejour H Walch G Neyret P Adeleine P. [Dysplasia of the femoral trochlea]. Revue de Chirurgie Orthop et Reparatrice de l'appareil Moteur. 1990;76(1):45-54. [PubMed] [Google Scholar]
- 7.Dejour H Walch G Nove-Josserand L Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthroscopy. 1994;2(1):19-26. [DOI] [PubMed] [Google Scholar]
- 8.van Duijvenbode D Stavenuiter M Burger B van Dijke C Spermon J Hoozemans M. The reliability of four widely used patellar height ratios. Int Orthop. 2016;40(3):493-7. [DOI] [PubMed] [Google Scholar]
- 9.Insall J Salvati E. Patella position in the normal knee joint. Radiol. 1971;101(1):101-4. [DOI] [PubMed] [Google Scholar]
- 10.Caton J Deschamps G Chambat P Lerat JL Dejour H. [Patella infera. Apropos of 128 cases]. Revue de Chirurgie Orthop et Reparatrice de l'appareil Moteur. 1982;68(5):317-25. [PubMed] [Google Scholar]
- 11.Blackburne JS Peel TE. A new method of measuring patellar height. J Bone Joint Surg Br. 1977;59(2):241-2. [DOI] [PubMed] [Google Scholar]
- 12.Grelsamer RP Meadows S. The modified Insall-Salvati ratio for assessment of patellar height. Clin Orthop Rel Res. 1992(282):170-6. [PubMed] [Google Scholar]
- 13.Merchant AC Mercer RL Jacobsen RH Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56(7):1391-6. [PubMed] [Google Scholar]
- 14.Davies AP Costa ML Shepstone L Glasgow MM Donell S. The sulcus angle and malalignment of the extensor mechanism of the knee. J Bone Joint Surg Br. 2000;82(8):1162-6. [DOI] [PubMed] [Google Scholar]
- 15.Aglietti P Insall JN Cerulli G. Patellar pain and incongruence. I: Measurements of incongruence. Clin Orthop Rel Res. 1983(176):217-24. [PubMed] [Google Scholar]
- 16.Sanders TG Morrison WB Singleton BA Miller MD Cornum KG. Medial patellofemoral ligament injury following acute transient dislocation of the patella: MR findings with surgical correlation in 14 patients. J Comp Assisted Tomography. 2001;25(6):957-62. [DOI] [PubMed] [Google Scholar]
- 17.Maenpaa H Lehto MU. Patellar dislocation. The long-term results of nonoperative management in 100 patients. Am J Sports Med. 1997;25(2):213-7. [DOI] [PubMed] [Google Scholar]
- 18.Atkin DM Fithian DC Marangi KS Stone ML Dobson BE Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28(4):472-9. [DOI] [PubMed] [Google Scholar]
- 19.Smith TO Donell S Song F Hing CB. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Rev. 2015;2:Cd008106. [DOI] [PubMed] [Google Scholar]
- 20.Palmu S Kallio PE Donell ST Helenius I Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463-70. [DOI] [PubMed] [Google Scholar]
- 21.Sillanpaa PJ Mattila VM Maenpaa H Kiuru M Visuri T Pihlajamaki H. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation. A prospective randomized study. J Bone Joint Surg Am. 2009;91(2):263-73. [DOI] [PubMed] [Google Scholar]
- 22.Smith TO Davies L Chester R Clark A Donell ST. Clinical outcomes of rehabilitation for patients following lateral patellar dislocation: a systematic review. Physiotherapy. 2010;96(4):269-81. [DOI] [PubMed] [Google Scholar]
- 23.Nikku R Nietosvaara Y Aalto K Kallio PE. Operative treatment of primary patellar dislocation does not improve medium-term outcome: A 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop. 2005;76(5):699-704. [DOI] [PubMed] [Google Scholar]
- 24.Bitar AC Demange MK D'Elia CO Camanho GL. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40(1):114-22. [DOI] [PubMed] [Google Scholar]
- 25.Camanho GL Viegas Ade C Bitar AC Demange MK Hernandez AJ. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620-5. [DOI] [PubMed] [Google Scholar]
- 26.Christiansen SE Jakobsen BW Lund B Lind M. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy. 2008;24(8):881-7. [DOI] [PubMed] [Google Scholar]
- 27.Petri M Liodakis E Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg. 2013;133(2):209-13. [DOI] [PubMed] [Google Scholar]
- 28.Conlan T Garth WP Jr. Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682-93. [DOI] [PubMed] [Google Scholar]
- 29.Desio SM Burks RT Bachus KN. Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med. 1998;26(1):59-65. [DOI] [PubMed] [Google Scholar]
- 30.Kang HJ Wang F Chen BC Su YL Zhang ZC Yan CB. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthroscopy, 2010;18(11):1511-6. [DOI] [PubMed] [Google Scholar]
- 31.Nomura E Inoue M Osada N. Anatomical analysis of the medial patellofemoral ligament of the knee, especially the femoral attachment. Knee Surg Sports Traumatol Arthroscopy. 2005;13(7):510-5. [DOI] [PubMed] [Google Scholar]
- 32.Muneta T Sekiya I Tsuchiya M Shinomiya K. A technique for reconstruction of the medial patellofemoral ligament. Clin Orthoped Rel Res. 1999(359):151-5. [DOI] [PubMed] [Google Scholar]
- 33.Nomura E Inoue M. Surgical technique and rationale for medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Arthroscopy. 2003;19(5):E47. [DOI] [PubMed] [Google Scholar]
- 34.Steensen RN Dopirak RM Maurus PB. A simple technique for reconstruction of the medial patellofemoral ligament using a quadriceps tendon graft. Arthroscopy.. 2005;21(3):365-70. [DOI] [PubMed] [Google Scholar]
- 35.Calapodopulos CJ Nogueira MC Eustaquio JM Calapodopulos Junior CJ Rodrigues OA. Reconstruction of the medial patellofemoral ligament using autologous graft from quadriceps tendon to treat recurrent patellar dislocation. Revista Brasileira de Ortopedia. 2016;51(2):187-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goyal D. Medial patellofemoral ligament reconstruction: the superficial quad technique. Am J Sports Med. 2013;41(5):1022-9. [DOI] [PubMed] [Google Scholar]
- 37.Fink C Veselko M Herbort M Hoser C. MPFL reconstruction using a quadriceps tendon graft: part 2: operative technique and short term clinical results. Knee. 2014;21(6):1175-9. [DOI] [PubMed] [Google Scholar]
- 38.Schottle PB Fucentese SF Romero J. Clinical and radiological outcome of medial patellofemoral ligament reconstruction with a semitendinosus autograft for patella instability. Knee Surg Sports Traumatol Arthroscopy. 2005;13(7):516-21. [DOI] [PubMed] [Google Scholar]
- 39.Wylie JD Burks RT. Medial patellofemoral ligament reconstruction with semitendinosus autograft. Arthroscopy Tech. 2013;2(4):e417-e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lording T Heimstra L Fink C Getgood A. Strategies for reconstruction of the medial patellofemoral ligament. Op Tech Sports Med. 2015;23(2):87-94. [Google Scholar]
- 41.Abulencia A Acosta D Adelman J, et al. Observation of B(s)0-->K + K- and measurements of branching fractions of charmless two-body decays of B0 and B(s)0 mesons in pp collisions at square root of s = 1.96 TeV. Phys Reviews. 2006;97(21):211802. [DOI] [PubMed] [Google Scholar]
- 42.Singhal R Rogers S Charalambous CP. Double-bundle medial patellofemoral ligament reconstruction with hamstring tendon autograft and mediolateral patellar tunnel fixation: a meta-analysis of outcomes and complications. Bone Joint J. 2013;95-b(7):900-5. [DOI] [PubMed] [Google Scholar]
- 43.Fernandez E Sala D Castejon M. Reconstruction of the medial patellofemoral ligament for patellar instability using a semitendinosus autograft. Acta Orthopa Belgica. 2005;71(3):303-8. [PubMed] [Google Scholar]
- 44.Csintalan RP Latt LD Fornalski S Raiszadeh K Inacio MC Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27(2):139-46. [DOI] [PubMed] [Google Scholar]
- 45.Nomura E Inoue M. Hybrid medial patellofemoral ligament reconstruction using the semitendinous tendon for recurrent patellar dislocation: minimum 3 years' follow-up. Arthroscopy. 2006;22(7):787-93. [DOI] [PubMed] [Google Scholar]
- 46.Mikashima Y Kimura M Kobayashi Y Miyawaki M Tomatsu T. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belgica. 2006;72(1):65-71. [PubMed] [Google Scholar]
- 47.Panagopoulos A van Niekerk L Triantafillopoulos IK. MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med. 2008;29(5):359-65. [DOI] [PubMed] [Google Scholar]
- 48.Enderlein D Nielsen T Christiansen SE Fauno P Lind M. Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthroscopy. 2014;22(10):2458-64. [DOI] [PubMed] [Google Scholar]
- 49.Watanabe T Muneta T Ikeda H Tateishi T Sekiya I. Visual analog scale assessment after medial patellofemoral ligament reconstruction: with or without tibial tubercle transfer. J Orthop Sci. 2008;13(1):32-8. [DOI] [PubMed] [Google Scholar]
- 50.Ronga M Oliva F Longo UG Testa V Capasso G Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37(9):1735-42. [DOI] [PubMed] [Google Scholar]
- 51.Fulkerson JP. Complications of patellofemoral instability surgery: A practical guide. Op Tech Sports Med . 2015; 23(2):84-6. [Google Scholar]
- 52.Caton JH Dejour D. Tibial tubercle osteotomy in patello-femoral instability and in patellar height abnormality. Int Orthop. 2010;34(2):305-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Koh JL Stewart C. Patellar instability. Clin Sports Med. 2014;33(3):461-76. [DOI] [PubMed] [Google Scholar]
- 54.Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Rel Res. 1983(177):176-81. [PubMed] [Google Scholar]
- 55.Ward SR Terk MR Powers CM. Influence of patella alta on knee extensor mechanics. J Biomech. 2005;38(12):2415-22. [DOI] [PubMed] [Google Scholar]
- 56.Servien E Verdonk PC Neyret P. Tibial tuberosity transfer for episodic patellar dislocation. Sports Med Arthroscopy Rev. 2007;15(2):61-7. [DOI] [PubMed] [Google Scholar]
- 57.Trillat A Dejour H Couette A. [DIAGNOSIS AND TREATMENT OF RECURRENT DISLOCATIONS OF THE PATELLA]. Revue de Chirurgie Orthop et reparatrice de l'appareil Moteur. 1964;50:813-24. [PubMed] [Google Scholar]
- 58.Cohen ZA Henry JH McCarthy DM Mow VC Ateshian GA. Computer simulations of patellofemoral joint surgery. Patient-specific models for tuberosity transfer. Am J Sports Med. 2003;31(1):87-98. [DOI] [PubMed] [Google Scholar]
- 59.Pidoriano AJ Weinstein RN Buuck DA Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med. 1997;25(4):533-7. [DOI] [PubMed] [Google Scholar]
- 60.Colvin AC West RV. Patellar instability. J Bone Joint Surg Am. 2008;90(12):2751-62. [DOI] [PubMed] [Google Scholar]
- 61.Longo UG Rizzello G Ciuffreda M, et al. Elmslie-Trillat, Maquet, Fulkerson, Roux Goldthwait, and other distal realignment procedures for the management of patellar dislocation: Systematic review and quantitative synthesis of the literature. Arthroscopy. 2016;32(5):929-43. [DOI] [PubMed] [Google Scholar]
- 62.Sherman SL Erickson BJ Cvetanovich GL, et al. Tibial tuberosity osteotomy: Indications, techniques, and outcomes. Am J Sports Med. 2014;42(8):2006-17. [DOI] [PubMed] [Google Scholar]
- 63.Tanaka MJ. Complications in patellofemoral instability surgery. Op Tech Sports Med. 2015; 23(2):77-83. [Google Scholar]
- 64.Weber AE Nathani A Dines JS, et al. An algorithmic approach to the management of recurrent lateral patellar dislocation. J Bone Joint Surg Am. 2016;98(5):417-27. [DOI] [PubMed] [Google Scholar]
- 65.Stetson WB Friedman MJ Fulkerson JP Cheng M Buuck D. Fracture of the proximal tibia with immediate weightbearing after a Fulkerson osteotomy. Am J Sports Med. 1997;25(4):570-4. [DOI] [PubMed] [Google Scholar]
- 66.Bollier M Fulkerson JP. The role of trochlear dysplasia in patellofemoral instability. J Am Acad Orthop Surg. 2011;19(1):8-16. [DOI] [PubMed] [Google Scholar]
- 67.Duncan ST Noehren BS Lattermann C. The role of trochleoplasty in patellofemoral instability. Sports Med Arthroscopy Rev. 2012;20(3):171-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.LaPrade RF Cram TR James EW Rasmussen MT. Trochlear dysplasia and the role of trochleoplasty. Clin Sports Med. 2014;33(3):531-45. [DOI] [PubMed] [Google Scholar]
- 69.Hinckel BB Arendt EA Ntagiopoulos PG Dejour D. Trochleoplasty: Historical overview and Dejour Technique. Op Tech Sports Med. 2015;23(2):114-22. [Google Scholar]
- 70.Peterson L Vasiliadis HS. Proximal Open Trochleoplasty (Grooveplasty). In: Zaffagnini S Dejour D Arendt AE, editors. Patellofemoral Pain, Instability, and Arthritis: Clinical Presentation, Imaging, and Treatment. Berlin, Heidelberg: Springer Berlin Heidelberg; 2010. p. 217-24. [Google Scholar]
- 71.Dejour D Saggin P. The sulcus deepening trochleoplasty-the Lyon's procedure. Int Orthop. 2010;34(2):311-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Biedert RM Albrecht S. The patellotrochlear index: a new index for assessing patellar height. Knee Surg Sports Traumatol Arthroscopy. 2006;14(8):707-12. [DOI] [PubMed] [Google Scholar]
- 73.von Knoch F Bohm T Burgi ML von Knoch M Bereiter H. Trochleaplasty for recurrent patellar dislocation in association with trochlear dysplasia. A 4- to 14-year follow-up study. J Bone Joint Surg Br. 2006;88(10):1331-5. [DOI] [PubMed] [Google Scholar]