Abstract
Background
Rosacea is a chronic inflammatory skin condition associated with four distinct subtypes: erythematotelangiectatic, papulopustular, phymatous, and ocular.
Purpose
To review the different kinds of management for all subtypes.
Methods
We divided rosacea management into three main categories: patient education, skin care, and pharmacological/procedural interventions.
Results
Flushing is better prevented rather than treated, by avoiding specific triggers, decreasing transepidermal water loss by moisturizers, and blocking ultraviolet light. Nonselective β-blockers and α2-adrenergic agonists decrease erythema and flushing. The topical α-adrenergic receptor agonist brimonidine tartrate 0.5% reduces persistent facial erythema. Intradermal botulinum toxin injection is almost safe and effective for the erythema and flushing. Flashlamp-pumped dye, potassium-titanyl-phosphate and pulsed-dye laser, and intense pulsed light are used for telangiectasias. Metronidazole 1% and azelaic acid 15% cream reduce the severity of erythema. Both systemic and topical remedies treat papulopustules. Systemic remedies include metronidazole, doxycycline, minocycline, clarithromycin and isotretinoin, while topical remedies are based on metronidazole 0.75%, azelaic acid 15 or 20%, sodium sulfacetamide, ivermectin 1%, permethrin 5%, and retinoid. Ocular involvement can be treated with oral or topical antibacterial. Rhinophyma can be corrected by dermatosurgical procedures, decortication, and various types of lasers.
Conclusion
There are many options for rosacea management. Patients may have multiple subtypes, and each phase has its own treatment.
Key Words: Inflammatory lesion, Ocular rosacea, Laser, Ivermectin, Azelaic acid, Demodex, Rosacea, Isotretinoin
Introduction
Rosacea is a chronic inflammatory disorder that affects 10% of the population. The prevalence of rosacea is highest among fair-skinned individuals. The consensus committee and review panel of 17 medical experts worldwide identified four subtypes of rosacea, defined as common patterns or groupings of signs and symptoms. These include:
subtype 1 - erythematotelangiectatic rosacea: characterized by flushing and persistent redness; it may also include visible blood vessels;
subtype 2 - papulopustular rosacea: characterized by persistent redness with transient papules and pastules (bumps and pimples);
subtype 3 - phymatous rosacea: characterized by skin thickening, often resulting in an enlargement of the nose from excess tissue;
subtype 4 - ocular rosacea: characterized by ocular manifestations such as dry eye, tearing and burning, swollen eyelids, recurrent hordeolum (styes) and potential vision loss from corneal damage.
Many patients experience characteristics of more than one subtype at the same time, and those may often develop in succession. While rosacea may or may not evolve from one subtype to another, each individual sign or symptom may progress from mild to moderate to severe. Early diagnosis and treatment are therefore recommended. Treatment is guided based on what subtypes patients have. Patients who find that they blush and flush frequently, or have a family history of rosacea, are advised to avoid the physiological and environmental stimuli that can cause increased facial redness. Topical agents such as metronidazole, azelaic acid, ivermectin, or sulfur preparations are effective in managing rosacea [1]. Patients who have progressed to erythematotelangiectatic and papulopustular rosacea may benefit from the use of an oral antibiotic, such as tetracycline, and in severe or recalcitrant cases, isotretinoin, to bring the rosacea flare-up under control. Patients with ocular involvement may benefit from a long-term course of an antibiotic and the use of metronidazole gel. A surgical alternative, i.e. laser therapy, is recommended for the treatment of telangiectasias and rhinophyma. Topical α-adrenergic receptor agonists and cosmetic camouflage may be considered to cover the signs of rosacea [2]. The facial skin manifestations of rosacea have significant implications on patients' well-being and social and emotional health. Patients with rosacea have reported a negative burden of their disease, such as low self-esteem, low self-confidence, and decreased social interactions. Improvement of the clinical symptoms of rosacea improves the patient's emotional well-being and quality of life. Since a cure for rosacea does not yet exist, management and treatment regimens are designed to suppress the inflammatory lesions, erythema, and to a lesser extent, the telangiectasia involved with rosacea. With the wide variety of oral and topical agents available for the effective management of rosacea, patients no longer need to feel self-conscious because of their disorder. This paper includes a brief overview of the treatment modalities for rosacea and its management, and it focuses on three main categories: patient education, skin care, and pharmacological/procedural interventions for each phase, which has its own treatment.
Results
Each phase of rosacea has its own management and treatment.
Erythematotelangiectatic Rosacea
Erythematotelangiectatic rosacea is characterized by a transient episode of flushing and persistent central facial erythema. Diffuse facial erythema is a common finding in rosacea patients and can lead to persistent erythema. Redness may also involve the peripheral face, ears, and upper aspect of the chest, but periocular skin is typically spared; telangiectasias are also common.
Stimuli Avoidance
Flushingis better prevented rather than treated, in addition to patient education and skin care. Patients who find that they flush frequently, or have a family history of rosacea, are advised to avoid the physiological and environmental stimuli that can cause increased facial redness, such as the following:
environmental stimuli: exposure to temperature extremes, hot or cold, moving to a warm or hot environment from a cold one, cold wind, and heat from sunlight and severe sunburn;
emotional stimuli: stress and anxiety;
physiological stimuli: some foods and drinks, including alcohol, caffeine, spicy foods, and strenuous exercise;
exogenous stimuli: microdermabrasion, chemical peels, and products containing alcohol, menthol, peppermint, eucalyptus, clove oils, and other irritants [2].
Nonpharmacologic Treatment/Skin Care
Proper skin care plays a pivotal role in maintaining remission and alleviating the symptoms of rosacea. Moisturizers are an important aspect of treating rosacea - especially the flushing and erythema - because rosacea skin has increased transepidermal water loss. Blocking ultraviolet light is very important; sunscreens decrease LL-37 production and the subsequent production of reactive oxygen species that can trigger rosacea (table 1) [3].
Table 1.
Subtypes of rosacea and different kinds of management
| Kinds of management | Subtypes of rosaceaa | Advantage | Disadvantage |
|---|---|---|---|
| Avoidance of environmental stimuli (sun, cold, hot), emotional stimuli (stress and anxiety), physiological stimuli (alcohol, caffeine, spicy foods, strenuous exercise) | 1, 2, 4 | Prevent flare and decrease symptoms | No research study, poor patient compliance |
| Skin care (blocking ultraviolet light, moisturizers) | 1–4 | Prevent flare and decrease symptoms | No research study, poor patient compliance |
| Topical treatment | |||
| Topical a-adrenergic receptor agonists 0.5% | 1 | Significantly reduce baseline erythema, cosmetic benefit | Lasts up to 10 h, does not work for all, and rebound erythema in some |
| Topical metronidazole, 1 and 0.75% | 1, 2, 4 | Effective in reducing erythema, papules, and pustules in moderate to severe rosacea | Irritation and dermatitis |
| Topical erythromycin eyedrops 1%, topical cyclosporine, clarithromycin, metronidazole | 4 | Effective treatment for severe ocular symptoms | Just for ocular rosacea |
| Topical sodium sulfacetamide, 10% sodium sulfacetamide with 5% sulfur | 1, 2 | Good for rosacea with concomitant seborrheic dermatitis, decrease inflammatory lesions and facial erythema | Dryness, erythema, or irritation |
| Topical azelaic acid, 15% gel and 20% cream | 1, 2 | Complete remission or marked improvement of erythema and inflammatory lesion counts | Irritation, dryness, and transient stinging and burning |
| Topical ivermectin 1% cream | 2 | Significant reduction in inflammatory lesion counts | Irritation, xerosis, and burning |
| Topical retinoids | 1, 2 | Reduce erythema, papules and pustules, and telangiectasias | Irritation, xerosis |
| Topical praziquantel ointment 3% b.i.d., topical permethrin cream 5% | 2 | Significantly reduces the papules and pustules, treat cutaneous demodicosis | Irritation, xerosis, and burning |
| Topical calcineurin inhibitors | 1, 2 | Treat papulopustules, significant improvement in erythema | Irritation, burning |
| Emerging topical treatments: topical serine protease inhibitors, topical cromolyn sodium 4% solution | 1, 2 | Play a role in the pathogenesis of rosacea, potential therapeutic target in rosacea | More clinical trials needed |
| Oral treatments | |||
| Oral antibiotic: tetracyclines of doxycycline <50 mg daily, erythromycin at a dose of 250 mg/ day; oral metronidazole at doses of 200 mg b.i.d. | 2, 4 | Anti-inflammatory effects of tetracyclines are the main mechanism of action in reducing rosacea symptoms; erythromycin in pregnancy | Gastrointestinal distress; metronidazole; neuropathy and seizures |
| Isotretinoin 0.5 - 1.0 mg/kg daily | 2, 3 | Effective treatment for severe papulopustular rosacea, refractory rosacea | Increase triglycerides, dryness, and joint pain. |
| Nonselective ß-blockers, a2-adrenergic agonist 0.05 mg b.i.d. | 1 | Decrease erythema and flushing | Reduction in blood pressure, responders are not clinically identifiable |
| Procedural treatments | |||
| Laser (long pulse-duration pulsed-dye laser, Nd:YAG) | 1, 2 | Treatment of facial telangiectasia, inflammatory lesions, reduce the purpura, treat the broken blood vessels | Pigmentation in dark skin, purpura |
| Nonlaser intense pulsed light | 1, 2 | Noninvasive and nonablative, effective for vascular form | Just the perilesional erythema |
| Botulinum toxin injection | 1 | Symptomatic relief for severe refractory facial erythema and flushing | Rarely may cause headache |
| CO2 laser | 3 | Treating thickening, powerful - shave down the bumps; less bleeding, seals blood vessels | Permanent hypopigmentation, hyperpigmentation in dark skin |
| Surgical procedures, dermabrasion, electrocautery | 3 | Scrape off unwanted skin | Bleeding and cutting too deep, may cause scarring and permanent color changes |
Subtypes of rosacea: 1 = erythematotelangiectatic rosacea; 2 = papulopustular rosacea; 3 = phymatous rosacea; 4 = ocular rosacea.
Pharmacologic Treatment
Topical α-adrenergic receptor agonists have been shown to reduce persistent facial erythema in rosacea by vasoconstricting dermal blood vessels. Brimonidin tartrate 0.5% is approved by the US Food and Drug Administration for the treatment of rosacea-associated erythema. Oxymetazoline has also been shown to significantly reduce baseline erythema in patients with rosacea (table 1) [3].
Nonselective β-blockers, atenolol in particular, are thought to decrease erythema and flushing, as well as α2-adrenergic agonist clonidine. β-Blockers are used to treat a variety of cardiovascular conditions. By vasoconstricting dermal blood vessels, they have been shown to decrease erythema and flushing in some rosacea patients. Several case reports have suggested a role for β-blockers in the treatment of rosacea. Nonselective β-blockers are thought to decrease erythema and flushing in rosacea by inhibiting β-adrenergic receptors on the smooth muscles surrounding blood vessels, leading to vasoconstriction of these vessels [3,4].
The α2-adrenergic agonist clonidine has also been reported to improve flushing and blushing reactions at doses of 0.05 mg twice a day. At this dose, there was no reduction in blood pressure, but lower baseline malar temperature may have been reduced by peripheral vasoconstriction. Although some patients do remarkably well on clonidine, responders are not clinically identifiable before treatment. Since control of this feature of rosacea is so difficult, a trial course may be indicated [4].
Procedures: Laser, Intense Pulsed Light, and Intradermal Botulinum Toxin Injection
A variety of lasers have been used for the treatment of rosacea. Both the flashlamp-pumped long-pulse dye laser (1,064 nm long) and the potassium-titanyl-phosphate laser are used in the treatment of facial telangiectasia [4]. Rosacea treatment using the new-generation, high-energy, 595-nm-long pulse-duration pulsed-dye laser improves rosacea with a very favorable safety profile, and less purpura than resulted from earlier-generation pulsed-dye laser. The new V-beam features provide ultra-long pulse duration at the target blood vessels. This reduces the purpura and can also treat the broken blood vessels associated with rosacea, which is more comfortable for patients [5]. The long-pulsed neodymium-doped yttrium aluminium garnet (Nd:YAG) laser is a safe and effective treatment for vascular and inflammatory lesions of rosacea [6].
Nonlaser intense pulsed light is safe and effective for the treatment of a vascular form of rosacea [7]. It is a noninvasive and nonablative treatment that uses high-intensity pulses of visible light to improve the appearance of the vascular lesions of rosacea. Intense pulsed light is a light pulse targeted at the red pigment in the blood which heats and destroys the pigment without affecting the skin or other tissues. Intense pulsed light (540-950 nm) is a safe and effective treatment for rosacea-associated erythema, especially for perilesional erythema [8].
Several recent reports demonstrate the possible action of botulinum toxin for facial erythema and flushing. Botulinum toxin works as a neuromodulator at the neuromuscular junction. Chemical denervation by botulinum toxin appears to interfere with normal acetylcholine signaling pathways and can provide symptomatic relief to patients with severe facial flushing. Intradermal botulinum toxin injection seems effective and almost a safe therapy for patients with refractory erythema (it may rarely cause headache) and may be considered a reasonable addition to the therapeutic options, especially when other established therapies have failed [9].
Papulopustular Rosacea
The papulopustular subtype of rosacea is characterized by the persistent central facial erythema, in addition to inflammatory papules and pustules which are transient in nature.
Skin Care/Patient Education
In addition to skin care and avoiding specific triggers or exacerbating factors, such as wind, spicy foods, alcohol, hot drinks, ultraviolet light, and physical or psychological stress, medication reconciliation also plays an important role in the treatment of papulopustular rosacea.
Pharmacologic Treatment
Topical Medication
Topical sodium sulfacetamide, 10% sodium sulfacetamide with 5% sulfur, is useful in treating patients with rosacea, especially those who have concomitant seborrheic dermatitis. Efficacy of sodium sulfacetamide has been reported in papulopustular rosacea. It helps decrease inflammatory lesions and facial erythema. The most common adverse reactions include dryness, erythema, or irritation at the application site, which decrease in frequency over time [3.]
Topical metronidazole, 1 and 0.75%, is thought to be beneficial in treating rosacea because of its ability to decrease the reactive oxygen species generation and inactive existing reactive oxygen species production. It has been used as a topical treatment for rosacea for decades. Metronidazole has been effective in reducing erythema, papules, and pustules in multiple trials of patients with moderate to severe rosacea. The 0.75 and 1% creams have proven equally efficacious at reducing erythema, papules, and pustules when applied once daily, and have also been shown to maintain remission after discontinuation of treatment. Overall, topical application of metronidazole appears to be safe and well tolerated. Irritation and dermatitis are the most observed adverse reactions [10].
Topical azelaic acid, 15% gel and 20% cream, has been shown to decrease the expression of kallikrein 5 and cathelicidin, two important components of the inflammatory cascade in rosacea. Studies showed that 70-80% of patients using azelaic acid reported complete remission or marked improvement in their rosacea symptoms, in both erythema and inflammatory lesion counts. Once daily application of azeliac acid is effective and generally well tolerated. Irritation, dryness, and transient stinging and burning are the most observed adverse reactions [10].
Topical ivermectin 1% cream is an emerging treatment for papulopustular rosacea. It kills the Demodex mites that reside in the pilosebaceous units of patients with papulopustular rosacea. Its mechanism of action in rosacea is unknown, but it has anti-inflammatory effects, decreasing cellular and humoral immune responses, including neutrophil phagocytosis and chemotaxis, and regulates tumor necrosis factor α, interleukin IL-1b and IL-10. Inflammatory mechanisms appear to play a dominant role in the development of rosacea papules and pustules [11,12]. Ivermectin 1% cream revealed a significant reduction in inflammatory lesion counts. The most common adverse effects are irritation, xerosis, and burning.
Topical retinoids have been shown to repair photo-damaged skin by promoting connective tissue remodeling and downregulation of Toll-like receptor 2 expression. It has been theorized that topical retinoids may be effective in decreasing rosacea symptoms by reversing the contribution of ultraviolet radiation to rosacea's manifestations, and downregulation of Toll-like receptor 2 [13]. It has been reported in multiple studies to clinically reduce erythema, papules and pustules, and telangiectasias, but with potential for irritation [13,14].
Topical calcineurin inhibitors are hypothesized to be beneficial in reducing rosacea symptoms because of their ability to inhibit T-cell activation, thereby preventing the release of proinflammatory cytokines. Calcineurin inhibitors have been used to treat papulopustular rosacea and erythema, and have led to significant improvement in erythema in open-label studies with potential for irritation [15].
Topical permethrin cream 5% has been shown to treat cutaneous demodicosis and reducing erythema and papules, but not pustule count and telangiectasias [16].
Topical praziquantel ointment 3% twice daily significantly reduces the papules and pustules in rosacea patients. This agent has the ability to treat cutaneous demodicosis as antiparasitic agent, and may have anti-inflammatory activity [17].
Systemic Medications
Tetracyclines have been the foundation of systemic rosacea therapy for decades. Anti-inflammatory dosing of doxycycline <50 mg daily improves the manifestation of rosacea by decreasing matrix metalloproteinase expression, downregulating inflammatory cytokines, reducing reactive oxygen species levels, and inhibiting nitric oxide-mediating vasodilation. It has been proposed that the anti-inflammatory effects of tetracyclines are the main mechanism of action in reducing rosacea symptoms [3,18.]
Erythromycin is an effective antibiotic in the treatment of papulopustular rosacea, but its use is often limited by gastrointestinal distress. Erythromycin at a dose of 250 mg/day is generally used in patients who are intolerant to tetracyclines as well as in pregnant women in whom tetracyclines are contraindicated.
Oral metronidazole at a dose of 200 mg twice a day has been shown to be effective in treating papulopustular rosacea, but has been associated with rare potential side effects such as neuropathy and seizures [19,20].
Isotretinoin may be useful in treating patients with severe, recalcitrant papulopustular rosacea by downregulating Toll-like receptor 2 expression. Although it has not been approved by the Food and Drug Administration for the treatment of rosacea, several studies have shown that oral isotretinoin dose ranges from 0.5 to 1.0 mg/kg daily is an effective treatment for severe papulopustular rosacea [21]; however, studies have also shown that low-dose isotretinoin (10 mg daily) is effective in treating refractory rosacea with evidence of less adverse effects [22].
Emerging Therapies
Topical serine protease inhibitors may be useful in treating papulopustular rosacea because they inhibit the cleavage of the cathelicidin precursor into LL-37, the molecule's active form that plays a role in the pathogenesis of rosacea [23,24].
Topical cromolyn sodium (4% solution), the mast cell stabilizer, may be beneficial in treating rosacea, because mast cells release known rosacea triggers such as LL-37, matrix metalloproteinases, and inflammatory cytokines. Blocking mast cell degranulation was therefore hypothesized to be a potential therapeutic target in rosacea [3,25].
Ocular Rosacea
Ocular rosacea is an inflammation that causes redness, burning, photophobia, and itching of the eyes. It develops in people who have rosacea. Sometimes ocular rosacea is the first sign that may later develop into the facial type. Medication and a good eye care routine can help control the signs and symptoms.
Eye Care/Patient Education
A good eye care routine is very important, such as washing the eyes at least twice a day with warm water and using artificial tears to relieve dryness. Avoiding makeup or using a noncomedogenic and free-fragrance products is recommended, in addition to avoiding triggers including hot and spicy foods, alcoholic beverages, and sunlight.
Pharmacologic Treatment/Antibiotic
Tetracyclines (Doxycycline, Minocycline) Anti-Inflammatory Dose Once a Day (50 mg)
Tetracyclines are most common and effective, not primarily as antibiotics, but rather through a secondary effect that they exert on meibomian glands. Tetracyclines decrease bacterial lipase; therefore, they are effective in protecting the cornea from impending perforation secondary to inflammatory responses [26].
Topical Antibiotic
Topical erythromycin eyedrops 1% have also gained popularity in the treatment of ocular rosacea, because it often results in severe recalcitrant blepharitis and meibomian gland dysfunction.
Topical cyclosporine is more effective than oral doxycycline. Cyclosporine was more effective in symptomatic relief and in the treatment of eyelid signs (p = 0.01). There was a statistically significant increase in the mean Schirmer score with anesthesia and tear break-up time scores in the cyclosporine treatment group compared to the doxycycline treatment group (p < 0.05) [27].
Clarithromycin and metronidazole have also shown efficacy in treating ocular rosacea. A pilot study found the topical compound to be safe and effective in treating eyelid involvement in ocular rosacea [28].
Phymatous Rosacea
Phymatous rosacea is characterized by skin thickening, often resulting in an enlargement of the nose from excess tissue and overgrowth of sebaceous glands. It can also affect the chin or cheek as well as the forehead. Ignoring the signs of rosacea may lead to phymatous rosacea with a puffy look. This type of rosacea is very rare today, because many patients are more likely to have their rosacea treated early on.
Oral Isotretinoin
Oral isotretinoin (0.3 mg/kg/day) may be effective in treating phymatous rosacea. It appears to be an efficacious and well-tolerated option for the treatment of phymatous rosacea by significantly reducing facial cutaneous blood flow and the growth of sebaceous glands [29].
Surgical and Other Procedures for Treating Thick Skin
Fortunately surgical procedures can help reshape the nose and bring the skin back to normal size by shaving off the extra layers of skin. It takes about a week to heal from the surgery, and about 6 weeks after the procedures, the skin will look smoother and healthier (table 1).
CO2 Laser
CO2 laser is the preferred and most common method of treating thickening skin - a powerful laser to shave down the bumps induced by thickening skin. This procedure causes the least amount of bleeding because the laser seals blood vessels as it works; however, by using the traditional fully ablative CO2 lasers, there is a risk of hypopigmentation and hyperpigmentation [30].
Light-Based Therapy
Light-based therapy has had some good results, but it is not sufficient.
Dermabrasion
This technique involves using a wire brush to scrape off, or abrade, unwanted skin, but it can cause bleeding and there is the risk of cutting too deep, which can induce scarring and permanent color changes to the skin [30].
Electrocautery
This procedure involves using a heated electrode to warm and scrape off excess skin to give it a smoother look, but it may cause bleeding.
Care Plans
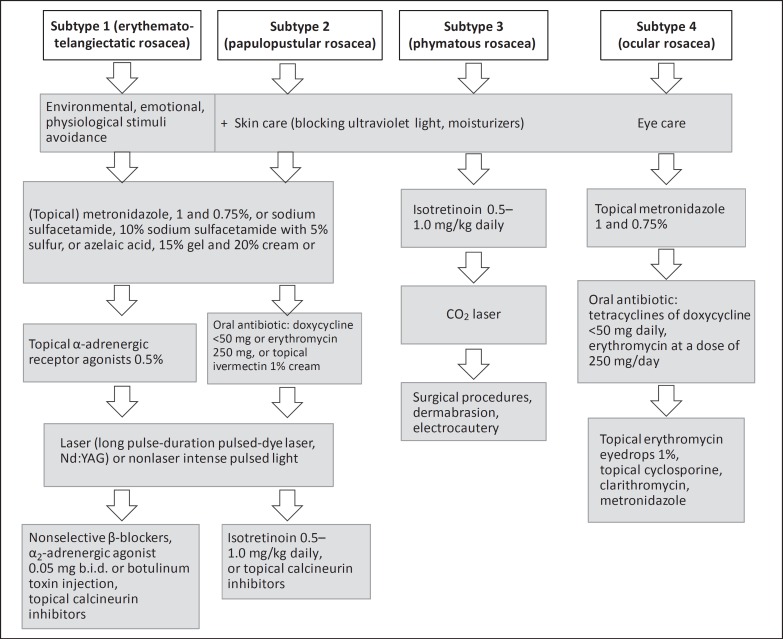
Each phase of rosacea has its own management; however, treatment of all subtypes involves the following (fig. 1):
Fig. 1.
Treatment algorithm of rosacea.
patient education: environmental stimuli avoidance (sun, cold, hot), emotional stimuli avoidance (stress and anxiety), and physiological stimuli avoidance (alcohol, caffeine, spicy foods, strenuous exercise);
skin care (blocking ultraviolet light, moisturizers) and eye care (artificial tears, eye washing);
subtype 1, erythematotelangiectatic rosacea: first step, topical treatment (metronidazole, calcineurin inhibitors, α-adrenergic receptor agonists 0.5%, retinoids); second step, procedures (laser, intense pulsed light, and intradermal botulinum toxin injection), and third step, oral medication (clonidine or atenolol);
subtype 2, papulopustular rosacea: first step, topical treatment (metronidazole 0.75%, azelaic acid 15%, ivermectin 1%, sodium sulfacetamide, retinoids, or calcineurin inhibitors); second step, oral antibiotic (doxycycline <50 mg daily, erythromycin 250 mg/day or oral metronidazole 200 mg); third step, oral isotretinoin 0.5-1.0 mg/kg daily, and fourth step, procedures (laser, intense pulsed light);
subtype 3, phymatous rosacea: first step, oral isotretinoin 0.5-1.0 mg/kg daily; second step, CO2 laser, and third step, surgical procedures (dermabrasion or electrocautery);
subtype 4, ocular rosacea: first step, topical metronidazole; second step, oral antibiotic (doxycycline <50 mg daily, erythromycin 250 mg/day, or oral metronidazole 200 mg twice a day), and third step, topical erythromycin eyedrops 1%, topical cyclosporine, or clarithromycin.
Conclusion
Rosacea management focuses on three main categories: patient education, skin care, and pharmacological/procedural interventions. Each phase has its own treatment. Patient education, skin care, and pharmacologic treatment are all pillars of effective and comprehensive management of treatment through both standard and novel pathways, while focusing on patient education and skin care can allow for better symptom control and improved quality of life for individuals with rosacea. Patients who find that they blush and flush frequently, or have a family history of rosacea, are advised to avoid the physiological and environmental stimuli that can cause increased facial redness. Topical agents such as metronidazole, azelaic acid, ivermectin, or sulfur preparations are effective in managing rosacea [1]. Patients who have progressed to erythematotelangiectatic and papulopustular rosacea may benefit from the use of an oral antibiotic, such as tetracycline, and in severe or recalcitrant cases, isotretinoin to bring the rosacea flare-up under control. Patients with ocular involvement may benefit from a long-term course of an antibiotic and the use of metronidazole gel. A surgical alternative, laser therapy, is recommended for the treatment of telangiectasias and rhinophyma. Topical α-adrenergic receptor agonists and cosmetic camouflage may be considered to cover the signs of rosacea [1]. As our knowledge of rosacea and its therapeutic options expand, a multifaceted approach to treatment is warranted.
Disclosure Statement
Dr. Abokwidir does not have any potential conflicts of interest. Dr. Feldman is a consultant for Galderma, Janssen, Lilly, Merck, Novartis, Qurient, Caremark, Advance Medical, and Suncare Research. He receives grant/research support from Galderma, GSK/Stiefel, Leo Pharma, Celgene, Pfizer, Valeant, Abbvie, Anacor, Janssen, Novartis, Qurient, and the National Biological Corporation.
References
- 1.Gupta AK, Chaudhry MM. Rosacea and its management: an overview. J Eur Acad Dermatol Venereol. 2005;19:273–285. doi: 10.1111/j.1468-3083.2005.01216.x. [DOI] [PubMed] [Google Scholar]
- 2.National Rosacea Society http://www.rosacea.org/tags/rosacea-awareness-month. www.rosacea.org/patients/allaboutrosacea.php.
- 3.Two AM, Wu W, Gallo RL, Hata TR. Topical and systemic therapies in the treatment of rosacea. J Am Acad Dermatol. 2015;72:761–770. doi: 10.1016/j.jaad.2014.08.027. quiz 771-772. [DOI] [PubMed] [Google Scholar]
- 4.Rebora A. The management of rosacea. Am J Clin Dermatol. 2002;3:489–496. doi: 10.2165/00128071-200203070-00005. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein EF, Kligman A. Rosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laser. Lasers Surg Med. 2008;40:233–239. doi: 10.1002/lsm.20621. [DOI] [PubMed] [Google Scholar]
- 6.Say EM, Okan G, Gökdemir G. Treatment outcomes of long-pulsed Nd:YAG laser for two different subtypes of rosacea. J Clin Aesthet Dermatol. 2015;8:16–20. [PMC free article] [PubMed] [Google Scholar]
- 7.Svyatenko T, Starostina O. New opportunities of IPL-therapy in complex treatment of the rosacea vascular forms. Georgian Med News. 2015;243:62–66. [PubMed] [Google Scholar]
- 8.Liu J, Liu J, Ren Y, Li B, Lu S. Comparative efficacy of intense pulsed light for different erythema associated with rosacea. J Cosmet Laser Ther. 2014;16:324–327. doi: 10.3109/14764172.2014.957218. [DOI] [PubMed] [Google Scholar]
- 9.Park KY, Hyun MY, Jeong SY, Kim BJ, Kim MN, Hong CK. Botulinum toxin for the treatment of refractory erythema and flushing of rosacea. Dermatology. 2015;230:299–301. doi: 10.1159/000368773. [DOI] [PubMed] [Google Scholar]
- 10.van Zuuren EJ, Kramer SF, Carter BR, Graber MA, Fedorowicz Z. Effective and evidence-based management strategies for rosacea: summary of a Cochrane systematic review. Br J Dermatol. 2011;165:760–781. doi: 10.1111/j.1365-2133.2011.10473.x. [DOI] [PubMed] [Google Scholar]
- 11.Ci X, Li H, Yu Q, Zhang X, Yu L, Chen N, Song Y, Deng X. Avermectin exerts anti-inflammatory effect by downregulating the nuclear transcription factor kappa-B and mitogen-activated protein kinase activation pathway. Fundam Clin Pharmacol. 2009;23:449–455. doi: 10.1111/j.1472-8206.2009.00684.x. [DOI] [PubMed] [Google Scholar]
- 12.Abokwidir M, Fleischer AB. An emerging treatment: topical ivermectin for papulopustular rosacea. J Dermatolog Treat. 2015;26:379–380. doi: 10.3109/09546634.2014.991672. [DOI] [PubMed] [Google Scholar]
- 13.Yamasaki K, Gallo RL. The molecular pathology of rosacea. J Dermatol Sci. 2009;55:77–81. doi: 10.1016/j.jdermsci.2009.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ertl GA, Levine N, Kligman AM. A comparison of the efficacy of topical tretinoin and low-dose oral isotretinoin in rosacea. Arch Dermatol. 1994;130:319–324. [PubMed] [Google Scholar]
- 15.Kim MB, Kim GW, Park HJ, Kim HS, Chin HW, Kim SH, Kim BS, Ko HC. Pimecrolimus 1% cream for the treatment of rosacea. J Dermatol. 2011;38:1135–1139. doi: 10.1111/j.1346-8138.2011.01223.x. [DOI] [PubMed] [Google Scholar]
- 16.Forstinger C, Kittler H, Binder M. Treatment of rosacea-like demodicidosis with oral ivermectin and topical permethrin cream. J Am Acad Dermatol. 1999;41(5 Pt 1):775–777. doi: 10.1016/s0190-9622(99)70022-8. [DOI] [PubMed] [Google Scholar]
- 17.Abokwidir M, Fleischer AB. Additional evidence that rosacea pathogenesis may involve demodex: new information from the topical efficacy of ivermectin and praziquantel. Dermatol Online J. 2015;21 pii:13030/qt13v249f5. [PubMed] [Google Scholar]
- 18.Del Rosso JQ, Schlessinger J, Werschler P. Comparison of anti-inflammatory dose doxycycline versus doxycycline 100 mg in the treatment of rosacea. Drugs Dermatol. 2008;7:573–576. [PubMed] [Google Scholar]
- 19.Wienbren MJ, Perinpanayagam RM, Camba L. Convulsions and encephalopathy in a patient with leukemia after treatment with metronidazole. J Clin Pathol. 1985;38:1076. doi: 10.1136/jcp.38.9.1076-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saihan EM, Burton JL. A double-blind trial of metronidazole versus oxytetracycline therapy for rosacea. Br J Dermatol. 1980;102:443–445. doi: 10.1111/j.1365-2133.1980.tb06558.x. [DOI] [PubMed] [Google Scholar]
- 21.Kennedy Carney C, Cantrell W, Elewski BE. Rosacea: a review of current topical, systemic and light-based therapies. G Ital Dermatol Venereol. 2009;144:673–688. [PubMed] [Google Scholar]
- 22.Park H, Del Rosso JQ. Use of oral isotretinoin in the management of rosacea. J Clin Aesthet Dermatol. 2011;4:54–61. [PMC free article] [PubMed] [Google Scholar]
- 23.Yamasaki K, Schauber J, Coda A, Lin H, Dorschner RA, Schechter NM, Bonnart C, Descargues P, Hovnanian A, Gallo RL. Kallikrein-mediated proteolysis regulates the antimicrobial effects of cathelicidins in skin. FASEB J. 2006;20:2068–2080. doi: 10.1096/fj.06-6075com. [DOI] [PubMed] [Google Scholar]
- 24.Two AM, Hata TR, Nakatsuji T, Coda AB, Kotol PF, Wu W, Shafiq F, Huang EY, Gallo RL. Reduction in serine protease activity correlates with improved rosacea severity in a small, randomized pilot study of a topical serine protease inhibitor. J Invest Dermatol. 2014;134:1143–1145. doi: 10.1038/jid.2013.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Di Nardo A, Vitiello A, Gallo RL. Cutting edge: mast cell antimicrobial activity is mediated by expression of cathelicidin antimicrobial peptide. J Immunol. 2003;170:2274–2278. doi: 10.4049/jimmunol.170.5.2274. [DOI] [PubMed] [Google Scholar]
- 26.Oge LK, Muncie HL, Phillips-Savoy AR. Rosacea: diagnosis and treatment. Am Fam Physician. 2015;92:187–196. [PubMed] [Google Scholar]
- 27.Arman A, Demirseren DD, Takmaz T. Treatment of ocular rosacea: comparative study of topical cyclosporine and oral doxycycline. Int J Ophthalmol. 2015;8:544–549. doi: 10.3980/j.issn.2222-3959.2015.03.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luchs J. Azithromycin in DuraSite for the treatment of blepharitis. J Clin Ophthalmol. 2010;4:681–688. doi: 10.2147/opth.s6370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Park H, Del Rosso JQ. Use of oral isotretinoin in the management of rosacea. Clin Aesthet Dermatol. 2011;4:54–61. [PMC free article] [PubMed] [Google Scholar]
- 30.Kassir R, Gilbreath J, Sajjadian A. Combination surgical excision and fractional carbon dioxide laser for treatment of rhinophyma. World J Plast Surg. 2012;1:36–40. [PMC free article] [PubMed] [Google Scholar]