Question
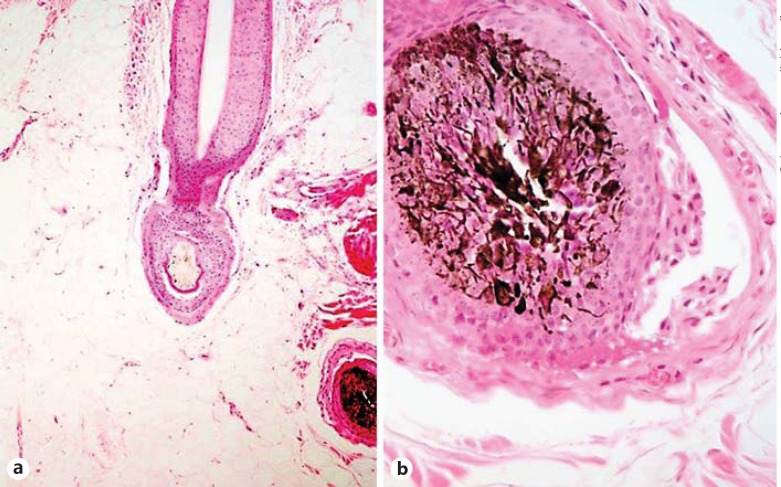
A 45-year-old healthy female presented to the dermatologic clinic with a 6-month history of diffuse hair loss and thinning but no relevant medical or pharmacological history. Scalp examination showed low-density hair in a diffuse pattern, which was more pronounced in the parietal and frontal areas (fig. 1a). The pull test was positive. Scalp dermoscopy revealed hair-shaft thinning and a lot of yellow dots (fig. 1b). Two 4-mm skin punch biopsies were performed in the parietal scalp and showed a nonscarring alopecia with an increased number of catagen/telogen miniaturized follicles (fig. 2a) and some follicular bulbs with melanin pigment casts and mild peribulbar lymphocytic inflammatory infiltrate (fig. 2b).
Fig. 1.
a Clinical picture of female-pattern hair loss. b Dermoscopy showing hair shaft thinning and multiple yellow dots (red circles; color refers to online version only).
Fig. 2.
a Catagen hair with miniaturization ×40. b Follicular bulb with melanic pigment casts and a peribulbar lymphocytic inflammatory infiltrate. Original magnification ×60.
Answer
Differential diagnosis of a diffuse alopecia with the female-pattern loss includes (1) androgenetic alopecia; (2) telogen effluvium; (3) cicatricial alopecia in pattern distribution, and (4) alopecia areata (AA; diffuse or incognita). Dermoscopy is a very useful complementary method that helps the dermatologists in the diagnosis of scalp disorders. In the patient presented here, dermoscopy showed multiple yellow dots, thinning of the hair shafts and absence of cicatricial areas, broken and exclamation mark hairs. These findings suggested alopecia areata incognita (AAI) that corroborated histopathology. We suggested treatment with systemic and topic corticosteroids, but the patient rejected it and was lost to follow-up.
Alopecia areata incognita
AAI was first described by Rebora in 1987 [1]. It is a variant of AA that most commonly affects females between 30 and 40 years of age [2,3]. AAI is characterized by the presence of acute and diffuse hair loss that mimics telogen effluvium and, in some cases, androgenetic alopecia. Dermoscopy and histology findings point out the difference between these entities.
Clinical examination shows diffuse alopecia with hair thinning that may predominate on the androgen-dependent scalp [3]. Characteristically, AAI lacks the presence of the typical patches of AA. Patients report an acute onset of diffuse hair loss with an evolution over a few months. Usually, the history is negative for possible causes of telogen effluvium [2].
The pathophysiology of AAI is still unknown. Rebora [1,4] suggested that if AA occurs in a scalp affected by androgenetic alopecia in which the hair cycle is shortened, causing a reduced number of follicles with high mitotic activity and an increased number of follicles with low mitotic activity, hairs can escape to telogen instead of becoming dystrophic. Therefore, the shedding in AAI is telogen, in contrast to diffuse AA where the hair is shed in a telogen and dystrophic anagen fashion.
The pull test is positive and shows different degrees of maturation of telogen roots [3]. Tosti et al. [2] analyzed the dermatoscopic findings in 70 patients with AAI and found that the presence of yellow dots is a constant finding helpful for the diagnosis. These yellow dots affect 70% of the follicles and are distributed in a uniform pattern. They correspond to the dilated ostium of miniaturized hair follicles filled with degenerated follicular keratinocytes and sebum.
The histopathologic features present in AAI include (1) a nonscarring pattern with a preserved number of follicular units but a decreased number of terminal follicles with an increased number of telogen follicles and vellus/miniaturized follicles; (2) dilated infundibular openings plugged with keratin and sebum (91.3%), and (3) in most cases, an inflammatory infiltrate around the miniaturized follicles in the upper dermis (50%) [2,3]. Miteva et al. [3], in connection with their analysis of 46 patients, proposed some histopathologic criteria for the diagnosis of AAI.
Many authors consider AAI the same entity as diffuse AA. Tosti et. al. [2] and Rebora [4] consider that these are different entities that differ in the presence of exclamation mark and dystrophic hairs. Exclamation mark and dystrophic hairs are exceptionally seen in AAI but are a common finding in diffuse AA [5].
AAI is usually treated with topic or systemic steroids, showing a good response in most cases [2,3]. Miteva et al. [3] found that only 6 out of 46 patients with AAI developed the typical patches of AA during the follow-up.
Dermoscopy and histopathology are fundamental methods in female-pattern hair loss to confirm the diagnosis and prescribe the appropriate treatment.
Statement of Ethics
The patient's consent was obtained. The authors have no ethical conflicts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Rebora A. Alopecia areata incognita: a hypothesis. Dermatologica. 1987;174:214–218. doi: 10.1159/000249182. [DOI] [PubMed] [Google Scholar]
- 2.Tosti A, Whiting D, Lorizzo M, Pazzaglia M, Misciali C, Vincenzi C, Micali G. The role of scalp dermoscopy in the diagnosis of alopecia areata incognita. J Am Acad Dermatol. 2008;59:64–67. doi: 10.1016/j.jaad.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 3.Miteva M, Misciali C, Fanti PA, Tosti A. Histopathologic features of alopecia areata incognito: a review of 46 cases. J Cutan Pathol. 2012;39:596–602. doi: 10.1111/j.1600-0560.2012.01896.x. [DOI] [PubMed] [Google Scholar]
- 4.Rebora A. Alopecia areata incognita: a comment. Clinics (Sao Paulo) 2011;66:1481–1482. doi: 10.1590/S1807-59322011000800028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inui S, Nakajima T, Nakagawa K, Itami S. Clinical significance of dermoscopy in alopecia areata: analysis of 300 cases. Int J Dermatol. 2008;47:688–693. doi: 10.1111/j.1365-4632.2008.03692.x. [DOI] [PubMed] [Google Scholar]