To the Editor,
Ungual changes can be helpful in the diagnosis of psoriasis, especially when the clinical features of the skin lesions are not typical. Onycholysis, dilated and tortuous capillaries in the hyponychium, crumbling of the nail plate, dilated blood vessels, and hemorrhages in the nail bed have been observed in patients with nail psoriasis [1,2].
We report on the presence of mottled lunulae in 3 patients with psoriasis. Nail biopsy studies showed that the red spots are consistent with dilated blood vessels in the lunulae. In the skin, these would be the dilated dermal capillaries under thin suprapapillary plates, which produce the Auspitz sign when bleeding.
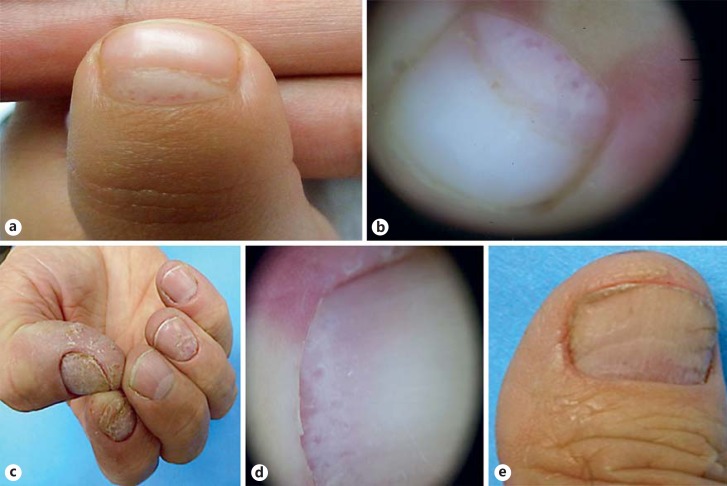
Case 1 is a 4-year-old girl with a 1-year history of red plaques on the tongue, neck, and buttocks, some of these were covered with a thick scale. The nail beds of both thumbs had multiple red spots with mild peripheral whitening (fig. 1a, b). She was diagnosed with psoriasis based on the clinical findings. Topical treatment with calcipotriol/betamethasone ointment was started in the skin and nail lesions with good response after 6 months of treatment.
Fig. 1.
Clinical and dermatoscopic findings: mottled lunulae. a, b Patient 1. c, d Patient 2. e Clinical response after topical and intralesional treatment in patient 2.
Case 2 is a 65-year-old man who reported a 5-month history of nail plate surface abnormalities on the fingernails. Dermoscopy showed puntiform red spots on the distal matrix (fig. 1c, d). The patient refused a nail biopsy, and topical treatment with calcipotriol/betamethasone was started with good response after 16 weeks (fig. 1e).
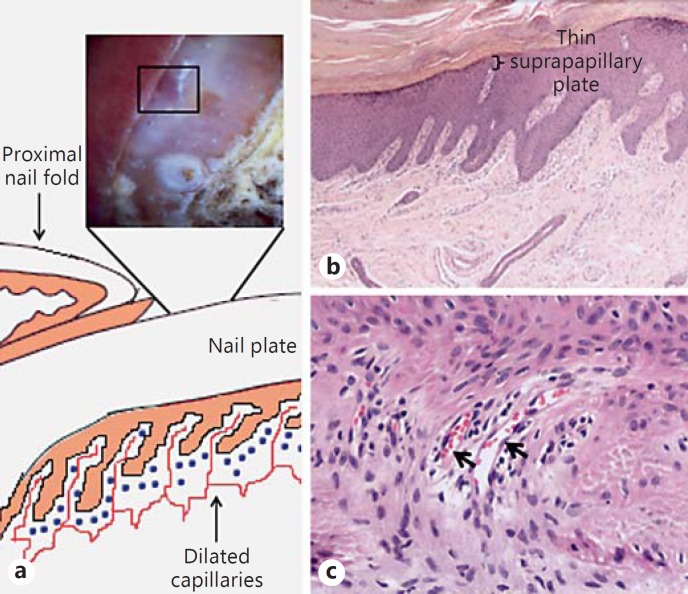
Case 3 is a 63-year-old man who presented with a 1-year history of nail plate surface abnormalities of the right thumb. No other lesions were found in the skin. Dermoscopy showed puntiform red spots with a perilesional white halo on the nail bed (fig. 2a). Nail biopsy revealed a dystrophic nail plate with mounds of parakeratosis with neutrophils, acanthosis, and spongiosis of the nail bed epithelium and perpendicular dilated capillaries in the onychodermis and a mild-to-moderate perivascular lymphocytic infiltrate (fig. 2b, c). The patient received one dose of intralesional triamcinolone and topical treatment with calcipotriol/betamethasone under occlusion showing good response after 6 weeks.
Fig. 2.
Dermatoscopic and histopathological findings in patient 3. a Dermatoscopic features with red dots in the lunula. b 4×; c 40×. Hematoxylin and eosin staining. Dilated capillaries in the superficial papillary dermis (arrows) and thinning of the suprapapillary plate.
Nail involvement is common in patients with psoriasis, between 10 and 78% of these patients have nail changes and up to 5% have only isolated nail psoriasis without skin manifestations. Frequently, more than one nail is involved and the fingernails are affected more often than the toenails [3,4]. These findings can be helpful for the diagnosis and some of them, for example hyponychial dilated capillaries, can correlate with disease severity and with response to treatment [2]. Red spots in the lunulae, so-called mottled lunulae, have been reported in psoriasis, alopecia areata, lichen planus, and rheumatoid arthritis. It reflects an acute inflammatory disorder [5,6,7].
It is well known that psoriasis can involve any structure of the nail apparatus, and according to the affected site, there are different clinical manifestations [3]. In skin biopsies of patients with psoriasis, there are tortuous and dilated capillaries in the superficial papillary dermis and the suprapapillary plate is typically thinned [8]. In this series, 2 patients underwent nail biopsy and all of them showed areas with thin suprapapillary plates and dilated onychodermal capillaries with a lymphocytic inflammatory infiltrate surrounding them. These findings could correspond to the red dots in the lunulae seen clinically (fig. 2).
In most cases, the diagnosis of nail psoriasis can be established according to clinical manifestations, but in some cases, it is necessary to perform a matrix or nail bed biopsy in order to confirm the suspected disease [3].
There are several topical and systemic treatments for nail psoriasis. Topical modalities include corticosteroids under occlusion with or without keratolytics, intralesional corticosteroids, vitamin D derivatives under occlusion, or topical PUVA. Systemic treatments proven useful are acitretin, methotrexate, cyclosporine, and biologic agents [3,4,9]. Our 3 patients were treated with topical calcipotriol/betamethasone under occlusion and 1 of them received one intralesional corticosteroid injection with improvement of the nail dystrophy and reduction of the red points.
In conclusion, mottled lunulae may correspond to onychodermal elongated and dilated capillaries. When this finding is present, it can be helpful in the diagnosis of psoriasis, especially in patients with isolated nail psoriasis.
Statement of Ethics
Although the study subjects are not identifiable in the pictures, they have given their informed consent to use the clinical photographs included in this article.
Disclosure Statement
The authors have no conflicts of interest to disclose. There was no funding for this work.
References
- 1.Piraccini BM, Bruni F, Starace M. Dermoscopy of non-skin cancer nail disorders. Dermatol Ther. 2012;25:594–602. doi: 10.1111/j.1529-8019.2012.01521.x. [DOI] [PubMed] [Google Scholar]
- 2.Iorizzo M, Dahdah M, Vincenzi C, Tosti A. Videodermoscopy of the hyponychium in nail bed psoriasis. J Am Acad Dermatol. 2008;58:714–715. doi: 10.1016/j.jaad.2007.11.026. [DOI] [PubMed] [Google Scholar]
- 3.Sánchez-Regaña M, Umbert P. Diagnosis and management of nail psoriasis. Actas Dermosifiliogr. 2008;99:34–43. [PubMed] [Google Scholar]
- 4.Tan ES, Chong WS, Tey HL. Nail psoriasis: a review. Am J Clin Dermatol. 2012;13:375–388. doi: 10.2165/11597000-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 5.Tosti A, Daniel R, Piraccini BM, Iorizzo M. in Color Atlas of Nails. Berlin Heidelberg: Springer-Verlag; 2010. Nail thinning; pp. 23–25. [Google Scholar]
- 6.Tosti A. Erythronychia. In: Tosti A, Thiers BH, editors. Nail Disorders Practical Tips for Diagnosis and Treatment. Philadelphia: Elsevier; 2015. p. 252. [Google Scholar]
- 7.Chang P, Vásquez-Acajabón MV. Red Lunula. Our Dermatol Online. 2013;4:555–556. [Google Scholar]
- 8.Calonje JE, Brenn T, Lazar AJ, McKee PH. McKee's Pathology of the Skin. 4th ed. Elsevier; 2012. [Google Scholar]
- 9.de Vries AC, Bogaards NA, Hooft L, Velema M, Pasch M, Lebwohl M, et al. Interventions for nail psoriasis. Cochrane Database Syst Rev. 2013;31:1. doi: 10.1002/14651858.CD007633.pub2. CD007633. [DOI] [PMC free article] [PubMed] [Google Scholar]