Dear Sir,
Sweet's syndrome (SS) is a neutrophilic dermatosis characterized by fever, peripheral neutrophil leucocytosis, and tender erythematous cutaneous lesions [1]. We describe a peculiar, never-reported, initial localization of SS involving a single phalanx.
A 54-year-old female presented with a 5-day history of a bluish swelling of the third right finger (fig. 1).
Fig. 1.

Single lesion of SS involving the distal phalanx of the third finger of the right hand.
At the time of our clinical consultation, we observed an erythematous, violaceous-based, hemorrhagic, vesicular lesion localized on the distal phalanx of the third digit of the right hand, characterized by the complete involvement of the nail bed. The patient complained of severe pain, fever, and arthralgia, which prompted her to seek medical advice.
The patient's medical history was remarkable for a 3-year history of essential thrombocythemia for which she received treatment with oncocarbide and anagrelide. She was also receiving anticoagulant therapy following an episode of pulmonary embolism secondary to deep vein thrombosis 2 years before.
Our initial differential diagnosis included an ischemic necrosis and an anticoagulant-induced hematoma.
Laboratory tests showed neutrophilia and an increased erythrocyte sedimentation rate. Other blood tests were within the normal value, including antinuclear antibody, extractable nuclear antibody, and anti-double-stranded DNA and coagulation factors.
One week later, the patient developed multiple tender, painful, red papules and nodules on the limbs, with a pseudovesicular appearance. Histologic examination of a skin lesion showed a spongiotic epidermis with a dense diffuse infiltrate of neutrophils in the upper dermis (fig. 2). Based on the clinical and histologic findings, we performed a final diagnosis of SS related to the underlying myeloproliferative disorder. The temporal relationship between the involvement of the third right digit and the onset of other skin lesions raised the hypothesis that the former represented the initial presentation of SS. This was confirmed by the prompt improvement of both cutaneous and nail lesions under steroid treatment.
Fig. 2.
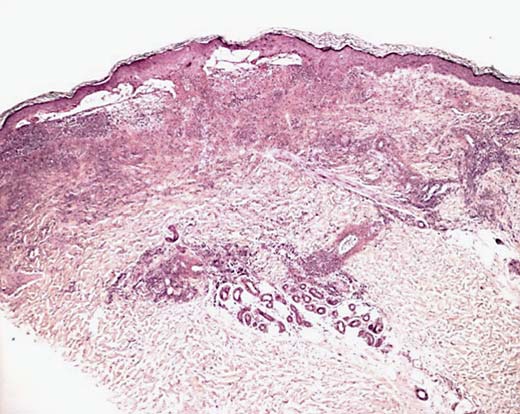
Low magnification of the histologic analysis from a popular lesion showing focal epidermal necrosis, subepidermal edema, and diffused neutrophils and lymphocytes in the reticular dermis. HE. ×10.
Initial lesions of SS appear as asymmetric, painful, red or purple-red papules or nodules. Later lesions of SS have a transparent, vesicle-like appearance because of the pronounced edema in the upper dermis. Differential diagnoses include systemic infections, other neutrophilic dermatoses, and vasculitis.
Typical SS usually starts after an upper respiratory tract infection; however, SS can also be related to drugs or associated with malignancy. In this latter form, it can occur as a paraneoplastic syndrome in patients with an established cancer or can be correlated with a hematologic dyscrasia [1].
Systemic corticosteroids are the therapeutic gold standard for SS, with a common response, consisting of a rapid improvement of both the skin lesions and the general symptoms after initiation of treatment. Topical application of high-potency corticosteroids or intralesional corticosteroids may be effective for treating localized lesions. Other second-line oral systemic agents are potassium iodide, colchicine, indomethacin, clofazimine, cyclosporine, and dapsone.
Although the initial lesions typically involve the upper extremities, face, and neck, a number of unusual different localizations have been reported, including wounds [2], scars [3], areas of lymphedema [4], and areas of radiotherapy [5]. Viseux et al. [6] described a case of SS and subungual erythema, but to the best of our knowledge, this is the first case describing an entire phalanx involvement as the initial sign of SS.
We would like to draw attention to a new possible site as the first localization of SS, an anticipatory event of a diffuse whole-skin manifestation of the disease.
Statement of Ethics
The authors have no ethical conficts to disclose.
Disclosure Statement
The authors have no conflicts of interest to disclose.
References
- 1.Cohen PR. Sweet's syndrome - a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;26:2–34. doi: 10.1186/1750-1172-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tavadia SMB, Smith G, Herd RM, Zuk RJ. Sweet's syndrome associated with oral squamous cell carcinoma and exhibiting the Koebner phenomenon. Br J Dermatol. 1999;141:169–170. doi: 10.1046/j.1365-2133.1999.02913.x. [DOI] [PubMed] [Google Scholar]
- 3.Atzori L, Ferreli C, Pinna AL, et al. P07.16. Sweet's syndrome lesions within pre-existing scars. J Eur Acad Dermatol Venereol. 2004;18((suppl)):363. [Google Scholar]
- 4.Petit T, Frances C, Marinho E, Herson S, Chosidow O. Lymphoedema-area-restricted Sweet syndrome during G-CSF treatment. Lancet. 1996;347:690. doi: 10.1016/s0140-6736(96)91241-6. [DOI] [PubMed] [Google Scholar]
- 5.Vergara G, Vargas-Machuca I, Pastor MA, Fariña MC, Martín L, Requena L. Localization of Sweet's syndrome in radiation-induced locus minoris resistentae. J Am Acad Dermatol. 2003;49:907–909. doi: 10.1016/s0190-9622(03)01832-2. [DOI] [PubMed] [Google Scholar]
- 6.Viseux V, Boulenger A, Jestin B, Plantin P. Transient subungual erythema in a patient with idiopathic Sweet's syndrome. J Am Acad Dermatol. 2003;49:554–555. doi: 10.1067/s0190-9622(03)00796-5. [DOI] [PubMed] [Google Scholar]


