Abstract
Background:
Angelica sinensis and Aurantii fructu used in a pair, named Danggui-Zhiqiao herb-pair (DZHP), which was rich in essential oil and has been adopted to promote blood circulation, dispel blood stasis, and relieve pain in traditional Chinese medicine (TCM)
Objective:
To analyze the composition and pharmacological effects of essential oil from DZHP
Materials and Methods:
The composition of the essential oil from DZHP was analyzed by gas chromatography/mass spectrometry (GC/MS). Its analgesic activity was evaluated by acetic acid-induced writhing test and hot plate test. The hemorheology test was carried out to evaluate the effect on hemorheology in rats with blood stasis syndrome
Results:
Twenty-eight components were identified and the main components were α-pinene (3.07%), β-pinene (2.0%), β-myrcene (3.71%), D-limonene (49.28%), γ-terpinen (9.53%), α-terpinolene (1.80%), α-terpineol (2.02%), β-bisabolene (1.13%), butylidenephthalide (1.43%), and Z-ligustilide (16.08%). The pharmacology test showed that the essential oil significantly inhibited the number of writhes induced by acetic acid with inhibition rate of 44.64% and significantly increased hot-plate latency compared with control group from 30 to 90 min after oral administration of drugs in mice. It could significantly decrease plasma viscosity, whole blood relative index at high and low shear rate, whole blood reduced viscosity at high and low shear rate, and erythrocyte rigidity index in hemorheology test
Conclusion:
The composition of the essential oil of DZHP was determined successfully and it had analgesic and promoting blood circulation activities.
SUMMARY
Angelica sinensis and Aurantii fructu used in a pair, named Danggui-Zhiqiao herb-pair (DZHP), which was rich in Essential oil and has been adopted to promote blood circulation, dispel blood stasis and relieve pain in traditional Chinese medicine (TCM).
Twenty-eight components were identified and the main components were α-pinene (3.07%), β-pinene (2.0%), β-myrcene (3.71%), D-limonene (49.28%), γ-terpinen (9.53%), α-terpinolene (1.80%), α-terpineol (2.02%), β-bisabolene (1.13%), butylidenephthalide (1.43%), and Z-ligustilide (16.08%).
The essential oil significantly inhibited the number of writhes induced by acetic acid and increased hot-plate latency compared with control group from 30 min to 90 min after oral administration of drugs in mice.
The essential oil could significantly decrease plasma viscosity (PV), whole blood relative index (WBRI) at high and low shear rate, whole blood reduced viscosity (WBRV) at high and low shear rate, and erythrocyte rigidity index (ERI) in hemorheology test.
Abbreviations used: DZHP: Danggui-Zhiqiao herb-pair; TCM: traditional Chinese medicine; GC/MS: gas chromatography /mass spectrometry; PV: plasma viscosity; WBRI: whole blood relative index; WBRV: whole blood reduced viscosity; ERI: erythrocyte rigidity index
Keywords: Danggui-Zhiqiao herb-pair, essential oil, composition, analgesic activity, hemorheology
INTRODUCTION
Chinese herbal formulas, referring to the combination of two or more herbs, are the main form of clinical application in traditional Chinese medicine (TCM) and have been adopted to treat and prevent disease for thousands of years in China. More and more people from all over the world have recognized and accepted TCM formulas due to their remarkable efficacies and less adverse reactions. Herb pairs, mixture of two herbs, as the basic and the simplest composition units of Chinese herbal formulas, have special clinical significance without altering their basic therapeutic features in TCM.[1,2] So herb pairs were interested by many research workers and the composition, pharmacological effects, pharmacokinetics of herb pairs were widely studied in recent years.[3,4]
Danggui-Zhiqiao herb-pair (DZHP) is comprised of Radix Angelica sinensis and Fructus Aurantii (named as Danggui and Zhiqiao in Chinese, respectively). Angelica sinensis has been widely used to treat female menstrual disorders via nourishing the blood and activating blood circulation in TCM.[5] Fructus Aurantii is one of well known traditional herbal medicines to treat cardiovascular symptoms in China.[6] DZHP exists in many famous Chinese herbal formulas, such as Wu Ji san, Xuefu-Zhuyu decoction, Shujin Huoxue decoction, Gexia Zhuyu decoction, Danggui-Zhiqiao decoction, which are all used to promote blood circulation, remove blood stasis, and relieve pain for long history.[7] Clinically, pain is one of the characteristics of blood stasis.[8] Essential oil is the DZHP's active ingredient. For example, Z-ligustilide, presented in the essential oil of Angelica sinensis, can inhibit platelet aggregation, resist oxidation, reduce ischemic brain injury, and blood pressure, and so on,[9,10,11] d-Limonene, an active component of essential oil of Fructus Aurantii, has been reported possessing anti-inflammatory, anti-oxidative, lipid-lowering, and decreasing blood pressure activities.[12,13,14] Previous studies mostly have been focused separately on the essential oil from Angelica sinensis or Fructus Aurantii,[15,16] respectively. So far, to the best of our knowledge, none of the study on the composition and pharmacological effects of essential oil from DZHP has been reported.
Therefore, this article aimed to analyze the composition of the essential oil from DZHP and evaluate its analgesic activity and effect on promoting blood circulation. The analgesic activity was determined by two mice experimental models: acetic acid-induced writhing response test[17,18] and hot-plate latent pain response test.[19,20] The effect on activating blood circulation was evaluated by determining hemorheological parameters in rats with blood stasis syndrome.[21] Our result might provide scientific information to further understand the main components of the essential oil from DZHP, as well as its mechanism in relieving pain and activating blood circulation to dissipate blood stasis. It would be helpful for the clinical application of the essential oil from DZHP on blood stasis syndrome.
MATERIALS AND METHODS
Materials and reagents
Radix Angelica sinensis was purchased from Dong Tang Pharmacy (Lot number 101218, Changsha, China), Fructus Aurantii was provided by Hunan Hansen Pharmaceutical Co. Ltd. (Lot number 101102, Yiyang, China). The two herbs were authenticated by Professor Ta-si Liu from the Hunan University of Chinese Medicine. Adrenaline hydrochloride injection was obtained from Wuhan Grand Pharmaceutical Group Co. Ltd. (Lot number 110307, Wuhan, China); TW-80 was supplied by Hunan Er Kang Pharmaceutical Co. Ltd. (Lot number 100608, Changsha, China). Acetic acid (analytical grade) was obtained from Changsha Reagent Company (Changsha, China).
Instrument and analytical conditions
The gas chromatography/mass spectrometry (GC/MS) analyses were performed on QP 2010 GC/MS instrument (Shimadzu, Japan) equipped with a flame ionization detector (FID), mass selective detector (MSD), and a Rtx-5ms capillary column (30 m × 0.25 mm, 0.25 μm). The initial oven temperature was held at 60°C for 2 min, and raised from 60 to 140°C at 10°/min, and then heated to 200°C at 4°C/min, and held for 8 min; injector temperature, 250°C; FID temperature, 300°C; ion-source temperature, 200°C; transfer line temperature was scanned over 40-500 amu with an ionizing voltage of 70 eV and ionization current 150 mA. Samples (1.0 μL) were automatically injected into the GC/MS and Helium was used as the carrier gas (1.0 mL/min) with split mode (1:50).
Compound identification
Most constituents were identified by comparing their mass spectra with those in either a computer library or with the authentic compounds and were confirmed by comparing the Kovats retention indices with those of authentic samples or from the literature.[16,22]
Preparation of the essential oil sample
The essential oil from DZHP was obtained by hydrodistillation. A 480 g amount of herb pair, that is, Radix Angelica sinensis and Fructus Aurantii in the weight ratio of 1 : 2, was crushed to coarse powder. The mixture was then steam distilled for 6 h and the yield of essential oil was 2.27% (w/w). The essential oil samples administrated to animals were prepared by dissolving the essential oil in 1% (w/v) Polysorbate 80 (TW-80), and the essential oil concentration reached to 0.035 and 0.092 g/mL for mice and rats, respectively.
Animals
Sprague–Dawley rats (220 ± 20 g) and Imprinting Control Region (ICR) mice (20 ± 2 g) were purchased from the Animal Center of Hunan University of Chinese Medicine [Certificate No. SCXK (Xiang) 2009-0004]. They were individually housed in plastic bottom cages with food and water provided ad libitum, and maintained at temperature 24 ± 2° with 55 ± 5% relative humidity and a 12 h light/dark cycle. The animal experiments were approved by Animal Ethics Committee of Hunan University of Chinese Medicine.
Acetic acid-induced writhing response
The acetic acid-induced writhing test was carried out according to the report.[17,18] 30 ICR mice, half male and half female, were divided into three groups of 10 mice each: control group (vehicle, 1% TW-80), positive group (aspirin, 0.12 g/kg), and the test drug group (essential oil of DZHP, 0.35 g/kg). They were administered vehicle or drugs for five days. Until half hour after the final administration, 0.6% acetic acid (0.1 mL/10 g) was intraperitoneally injected to them. The number of writhes was counted for 15 min after the acetic acid administration. The inhibition rate of writhes was calculated as follows: inhibition rate = [(control mean-test mean)/control mean] × 100.
Hot plate test
The hot plate test was performed according to the method previously reported.[19,20] The female ICR mice were divided into three groups (n = 10): control group (vehicle, 1% TW-80), positive group (aspirin, 0.12 g/kg), and the test drug group (essential oil of DZHP, 0.35 g/kg). Each female mouse was placed on the hot plate with a fixed temperature of 55 ± 0.5°C to observe the pain responses (hind-paw-licking or jumping). Before test each mouse was habituated twice to the hot plate. The response latency was defined as the recorded time in seconds between the platform and reaction. The mice were excluded when they exhibited latency time greater than 30 s or less than 5 s. They received continuous dosing for five days. After the final administration, the latency time was determined at 30, 60, and 90 min. A cut-off time of 60 s was fixed to prevent damage to the mice.
Experiment on hemorheology in rats with blood stasis syndrome
The Sprague–Dawley rats, composed of male and female in half, were randomly divided into four groups with eight rats per group, control group, model group, positive medicine group (aspirin, 0.1 g/kg), and essential oil group (0.92 g/kg). The animals received continuous dosing for six days. Until 1 h after the final administration, except for the control group, the acute blood stasis models in the other three groups were established according to the report:[2] animals were subcutaneously injected at the intraperitoneal area with the adrenaline hydrochloride injection (0.8 mg/kg). The injection was administered twice, each separated by 4 h. Two hours before the second injection, animals were soaked in ice water for 5 min with their heads above the water. Rats were fasted overnight and administration continued after performing the model. Blood samples were collected 0.5 h after the last administration at the second day. The blood collection was carried out by carotid artery intubation and was collected into tubes at the ratio of 1 : 9 with 3.8% sodium citrate. The hemorheological parameters including whole blood relative index (WBRI) at high and low shear rate, whole blood reduced viscosity (WBRV) at high and low shear rate, and erythrocyte rigidity index (ERI) were detected by SA6000 automatic hemarheology meter. The plasma was separated from blood by centrifugation at 4000 rpm for 10 min and detected for plasma viscosity.
Statistical analysis
The results were analyzed by nonparametric Mann–Whitney U-test or one-way analysis of variance based on Dunnett's multiple comparisons test. The differences were considered significant at P value less than 0.05.
RESULTS AND DISCUSSION
Composition of essential oil
The essential oil was yellow and fragrant liquid. The GC/MS chromatogram of the essential oil from DZHP is shown in Figure 1 and the main components in the mixtures are presented in Table 1. The presence of 28 compounds, accounting for 96.22% of the total oil composition, was detected by GC/MS, a main analytical technique adopted to quantification and quality control for the essential active substances of Chinese herb plants.[23]
Figure 1.
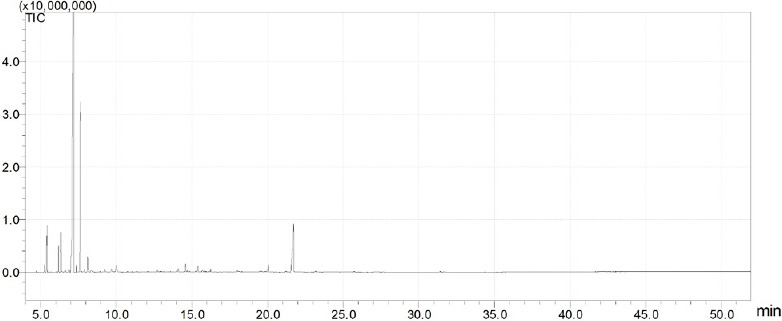
The gas chromatography/mass spectrometry chromatogram of the essential oil from Danggui-Zhiqiao herb-pair.
Table 1.
Chemical composition of essential oil from Danggui-Zhiqiao herb-pair
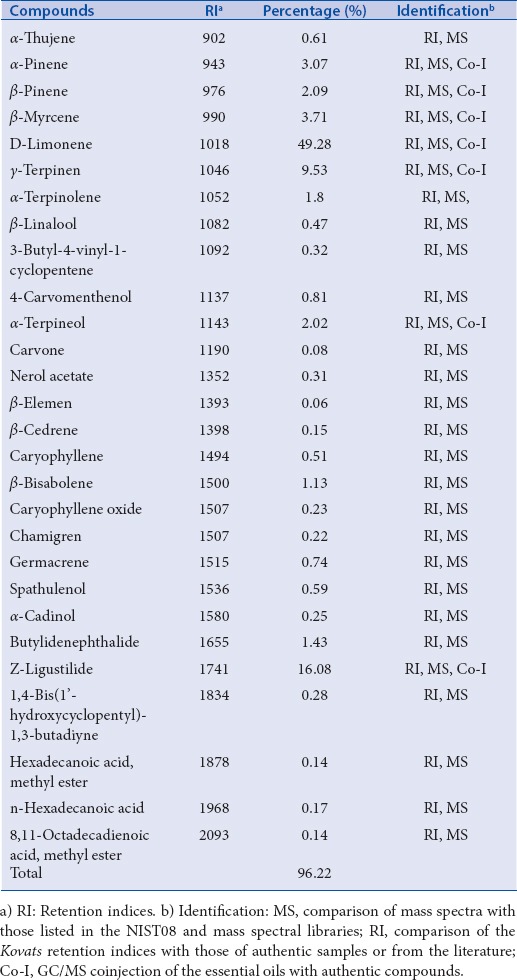
The constituents were identified by comparing their mass spectra with those in either a computer library or with the authentic compounds and were confirmed by comparing the Kovats retention indices with those of authentic samples or from the literature.[16,22] As shown in Table 1, the main components were α-pinene (3.07%), β-pinene (2.09%), β-myrcene (3.71%), D-limonene (49.28%), γ-terpinen (9.53%), α-terpinolene (1.80%), α-terpineol (2.02%), β-bisabolene (1.13%), butylidenephthalide (1.43%), and Z-ligustilide (16.08%). The oil was dominated by D-limonene, γ-terpinen, and Z-ligustilide, which made up 74.89 % of the identified oil composition.
To our knowledge, there are reports on the chemical composition of the essential oil of Angelica sinensis and Fructus Aurantii, respectively. The main compounds in Angelica sinensis were ligustilide, β-pinene, and butylidenephthalide and so on.[22] Limonene, α-pinene, γ-terpinen, carveol, terpineol, and linalool were the main compounds in Fructus Aurantii and the percentage of limonene was over 50%.[16] In previous reports, little is known about the essential oil of the herb pair, which was obtained by extracting the two herbs commonly. In our present study, the essential oil of the herb pair was dominated by the presence of D-limonene at 49.28% and Z-ligustilide at 16.08%. It was consistent with the results of the previous study that the major constituents of the two herbs were Z-ligustilide and D-limonene, respectively. The γ-terpinen, β-pinene, α-pinene, β-myrcene, α-terpinolene, α-terpineol, β-bisabolene, and butylidenephthalide were the other important products in the essential oil.
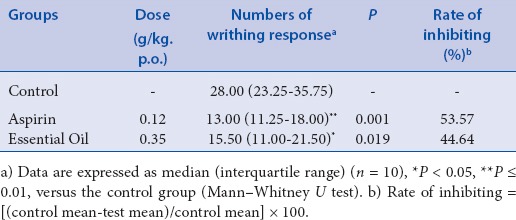
Acetic acid-induced writhing response
In analgesic study mice are widely used because of short reproduction period, cheaper to purchase and maintain. Moreover, mice models showed advantages of smaller quantity of agents required to induce and/or treat disease. Therefore, analgesic studies were carried out in mice in our research. The acetic acid-induced writhing test model is a highly sensitive and useful test for screening analgesic drug and has been widely regarded as a classical peripheral analgesic animal model.[24] The results of the acetic acid-induced writhing response are shown in Table 2. The essential oil, at the dose of 0.35 g/kg, showed remarkable inhibition on the number of writhes induced by acetic acid with inhibition rate of 44.64%. The positive control aspirin (0.12 g/kg) also very significantly inhibited the writhing response with inhibition rate of 53.57%. Compared with the blank control group, the results of the positive control aspirin and the tested essential oil were statistically significant (P < 0.01 and P < 0.05). Several studies suggested that acetic acid could result in an increase in peritoneal fluid levels of prostaglandins (PGE2 and PGF2) involving in part peritoneal receptors and inflammatory pain by inducing capillary permeability.[25] The effect of the essential oil of DZHP might inhibit the synthesis and/or the release of the prostaglandins and may be mediated through inhibition of cyclooxygenases and/or lipoxygenases.[25,26]
Table 2.
Effect of the essential oil from Danggui-Zhiqiao herb-pair on acetic acid-induced writhing response in mice
Hot plate latent pain response test in mice
The hot plate test, using thermal stimulus to induce pain, was proposed by Eddy and Leimbach[19] and is commonly applied to evaluate its centrally mediated antinociceptive activity. Significant analgesic efficacy of the essential oil of DZHP was observed by the hot plate test and is shown in Figure 2. Aspirin and the essential oil of DZHP significantly increased pain threshold of mice compared with preadministration (0 min) and a significant increase in hot plate latency occurred from 30 to 90 min after oral administration of drugs in mice compared with control group (P < 0.01). In our study, the essential oil of DZHP could significantly increase hot plate latency and this good analgesic activity may be mediated through inhibiting central pain receptors.
Figure 2.
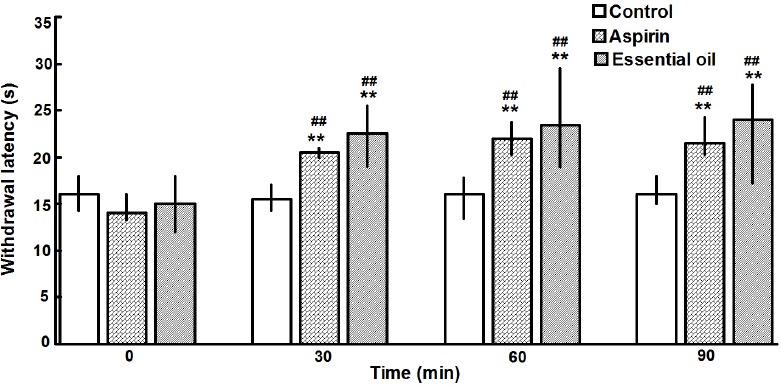
Effect of essential oil on hot plate test in mice. Each mouse was given a single dose of aspirin or essential oil or vehicle and then the hot plate latent response time of each animal was recorded at 0 (preadministration), 30, 60, and 90 min. The columns represent the median values and the vertical bars show the interquartile ranges. Mann–Whitney U test was used for statistical analysis. **P value less than 0.01 versus the control group and ##P value less than 0.01 versus preadministration (0 min)
Effect on hemorheology
According to report,[2] rats were selected to take part in hemorheology test. Effect on hemorheology was observed and the results are presented in Table 3. Compared with the control group, the model group had conspicuous plasma viscosity, WBRI at high and low shear rate, WBRV at high shear rate, and ERI, which indicated that the blood stasis model was built successfully. After administration, these hemorheological parameters significantly decreased in aspirin group and essential oil group compared with the model group. Obviously, the essential oil from DZHP can activate blood circulation to remove blood stasis.
Table 3.
Effect of essential oil from Danggui-Zhiqiao herb-pair on the hemorheology in rats with acute blood stasis syndrome
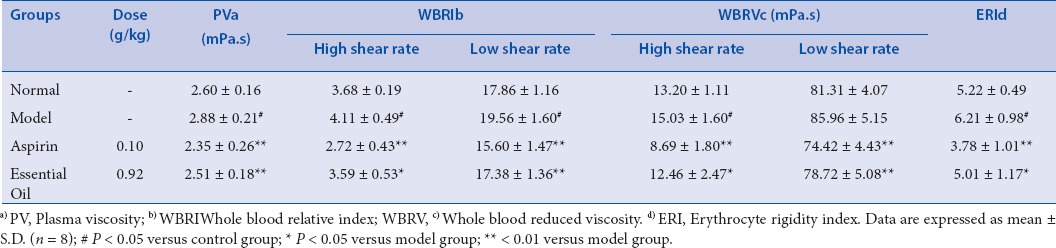
Hemorheology is the study on the relation of blood flow to pressure, flow volume, and resistance of blood vessels.[2] Once blood stasis develops, hemorheology and microcirculation will be further affected. It will lead to the elevation of blood viscosity, deterioration of erythrocyte deformability, acceleration of erythrocyte aggregation, and platelet aggregation, as well as microcirculatory dysfunction.[27] The hemorheological parameters will display abnormal when blood stasis occurs. In our study, hemorheological indexes were determined to evaluate whether the essential oil of DZHP had the effect on promoting blood circulation. The results demonstrated that the essential oil of DZHP could significantly decrease hemorheological parameters including plasma viscosity, WBRI, WBRV, and ERI compared with the model group and had strong effect on activating blood circulation.
CONCLUSION
The composition of the essential oil of DZHP and its analgesic, promoting blood circulation activity are reported for the first time. The essential oil of DZHP was analyzed successfully by GC/MS, and D-limonene (49.28%), Z-ligustilide (16.08%), and γ-terpinen (9.53%) were rich in the oil. It had good analgesic and promoting blood circulation activities, which may give evidences contributing to explain clinical application of essential oil of DZHP on blood stasis syndrome and provide foundation for clarifying the nature of the effect in the further study.
Financial support and sponsorship
Nil.
Conflict of interest
There are no conflicts of interest.
ABOUT AUTHOR

LI Shun-Xiang
Prof. LI Shun-Xiang, is a Professor at School of Pharmacy, Hunan University of Chinese Medicine, and Director of Hunan Province Engineering Research Center of Bioactive Substance Discovery of Chinese Medicine, China. His research interests are in the area of Natural product chemistry (Phytochemistry) and Active component of Chinese materia medica and their mechanism.
Acknowledgement
This work was supported by the Science and Technology Innovative Research Team in Higher Educational Institutions of Hunan Province for Innovation of Chinese Medicine and Resources sustained utilization (2010212), Construct program of the key discipline of Chinese Pharmacy in Hunan Province (201176), Research Fundation of the talent introduction project of Central South University of Forestry & Technology (2013RJ026).
REFERENCES
- 1.Han C, Guo J. Antibacterial and anti-inflammatory activity of traditional Chinese herb pairs, Angelica sinensis and Sophora flavescens. Inflammation. 2012;35:913–19. doi: 10.1007/s10753-011-9393-6. [DOI] [PubMed] [Google Scholar]
- 2.Liu L, Duan JA, Tang Y, Guo J, Yang N, Ma H. Taoren-Honghua herb pair and its main components promoting blood circulation through influencing on hemorheology, plasma coagulation and platelet aggregation. J Ethnopharmacol. 2012;139:381–87. doi: 10.1016/j.jep.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Ma C, Fan M, Tang Y, Li Z, Sun Z, Ye G, et al. Identification of major alkaloids and steroidal saponins in rat serum by HPLC-diode array detection-MS/MS following oral administration of Huangbai-Zhimu herb-pair Extract. Biomed Chromatogr. 2008;22:835–50. doi: 10.1002/bmc.1000. [DOI] [PubMed] [Google Scholar]
- 4.Liu Z, Dong X, Ding X, Chen X, Lv L, Li Y. Comparative pharmacokinetics of timosaponin B-II and timosaponin A-III after oral administration of Zhimu-Baihe herb-pair, Zhimu extract, free timosaponin B-II and free timosaponin A-III to rats. J Chromatogr B Analyt Technol Biomed Life Sci. 2013;926:28–35. doi: 10.1016/j.jchromb.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Mei QB, Tao JY, Cui B. Advances in the pharmacological studies of radix Angelica sinensis (Oliv) Diels (Chinese Danggui) Chin Med J. 1991;104:776–81. [PubMed] [Google Scholar]
- 6.Zhang B, Jin J, Jin ZG, Wu FH. Pharmacological effects and clinical application of Fructus Aurantii. Yi Yao Dao Bao. 2013;32:1462–64. [Google Scholar]
- 7.China Pharmacopoeia Committee. China: China Medical Science and Technology Press, Beijing; 2010. Chinese Pharmacopoeia (Chapter One) p. 693. [Google Scholar]
- 8.Chen KJ. Blood stasis syndrome and its treatment with activating blood circulation to remove blood stasis therapy. Chin J Integr Med. 2012;18:891–96. doi: 10.1007/s11655-012-1291-5. [DOI] [PubMed] [Google Scholar]
- 9.Zhang L, Du JR, Wang J, Yu DK, Chen YS, He Y. Z-ligustilide extracted from Radix Angelica Sinensis decreased platelet aggregation induced by ADP ex vivo and arterio-venous shunt thrombosis in vivo in rats. Yakugaku Zasshi. 2009;129:855–59. doi: 10.1248/yakushi.129.855. [DOI] [PubMed] [Google Scholar]
- 10.Kuang X, Du JR, Liu YX, Zhang GY, Peng HY. Postischemic administration of Z-ligustilide ameliorates cognitive dysfunction and brain damage induced by permanent forebrain ischemia in rats. Pharmacol Bio chem Behav. 2008;88:213–21. doi: 10.1016/j.pbb.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 11.Cao YX, Zhang W, He JY, He LC, Xu CB. Ligustilide induces vasodilatation via inhibiting voltage dependent calcium channel and receptor-mediated Ca2+ influx and release. Vascul Pharmacol. 2006;45:171–76. doi: 10.1016/j.vph.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Ruberto G, Baratha MT. Antioxidant activity of selected essential oil components in two lipid model systems. Food Chem. 2000;69:167–74. [Google Scholar]
- 13.d’Alessio PA, Ostan R, Bisson JF, Schulzke JD, Ursini MV, Béné MC. Oral administration of d-Limonene controls inflammation in rat colitis and displays anti-inflammatory properties as diet supplementation in humans. Life Sci. 2013;92:1151–56. doi: 10.1016/j.lfs.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Jesudoss VA, Jayaraman J, Madhavan S, Namasivayam N. d-limonene attenuates blood pressure and improves the lipid and antioxidant status in high fat diet and L-NAME treated rats. J Pharm Sci and Res. 2010;11:752–58. [Google Scholar]
- 15.Kim MR, Abd EI-Aty AM, Choi JH, Lee KB, Shim JH. Identification of volatile components in Angelica species using supercritical-CO2 fluid extraction and solid phase micro extraction coupled to gas chromatography-mass spectrometry. Biomed Chromatogr. 2006;20:1267–73. doi: 10.1002/bmc.696. [DOI] [PubMed] [Google Scholar]
- 16.Jiang YH, Yang XY, Zhang QH, Cao MM, Gong QF, Shi JL. Analysis of volatile oil in Fructus aurantii processed with Zhangband method by GC-MS. Zhong Yao Cai. 2010;33:1233–36. [PubMed] [Google Scholar]
- 17.Nakamura H, Shimoda A, Ishii K, Kadokawa T. Central and peripheral analgesic action of non-acidic non-steroidal anti-inflammatory drugs in mice and rats. Arch Int Pharmacodyn Ther. 1986;282:16–25. [PubMed] [Google Scholar]
- 18.Guo J, Pan W, Qian D, Duan JA, Shang E, Tang Y. Analgesic activity of DaChuan Xiong Fang after intranasal administration and its potential active components in vivo. J Ethnopharmacol. 2013;150:649–54. doi: 10.1016/j.jep.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 19.Eddy NB, Leimbach D. Synthetic analgesics: II Dithyienylbutenylamines and dithyienylbutylamines. J Pharmacol Exp Ther. 1953;107:385–93. [PubMed] [Google Scholar]
- 20.Su S, Wang T, Duan JA, Zhou W, Hua YQ, Tang YP. Anti-inflammatory and analgesic activity of different extracts of Commiphora myrrha. J Ethnopharmacol. 2011;134:251–58. doi: 10.1016/j.jep.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 21.Li HX, Han SY, Wang XW, Ma X, Zhang K, Wang L. Effect of the carthamins yellow from Carthamus tinctorius L on hemorheological disorders of blood stasis in rats [J] Food Chem Toxicol. 2009;47:1797–802. doi: 10.1016/j.fct.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 22.Wu MJ, Sun XJ, Dai YH, Guo FQ, Huang LF, Liang YZ. Determination of constituents of essential oil from Angelica sinensis by gas chromatography-mass spectrometry. J Cent South Univ. 2005;12:430–36. [Google Scholar]
- 23.Song L, Ding JY, Tang C, Yin CH. Compositions and biological activities of essential oils of Kadsura longepedunculata and Schisandra sphenanthera. Am J Chin Med. 2007;35:353–64. doi: 10.1142/S0192415X07004874. [DOI] [PubMed] [Google Scholar]
- 24.Negus SS, Vanderah TW, Brandt MR, Bilsky EJ, Becerra L, Borsook D. Preclinical assessment of candidate analgesic drugs: recent advances and future challenges. J Pharmacol Exp Ther. 2006;319:507–14. doi: 10.1124/jpet.106.106377. [DOI] [PubMed] [Google Scholar]
- 25.Deraedt R, Jouquey S, Delevallée F, Flahaut M. Release of prostaglandins E and F in an algogenic reaction and its inhibition. Eur J Pharmacol. 1980;61:17–24. doi: 10.1016/0014-2999(80)90377-5. [DOI] [PubMed] [Google Scholar]
- 26.Amann R, Peskar BA. Anti-inflammatory effects of aspirin and sodium salicylate. Eur J Pharmacol. 2002;447:1–9. doi: 10.1016/s0014-2999(02)01828-9. [DOI] [PubMed] [Google Scholar]
- 27.Wang T, Jia C, Chen Y, Li X, Cheng J. Analysis on establishment and affecting factors of qi stagnation and blood stasis rat model. Zhongguo Zhong Yao Za Zhi. 2012;37:1629–33. [PubMed] [Google Scholar]


