Abstract
Background:
Sensation is decreased or absent after breast reconstruction. This leaves reconstructed breasts vulnerable to injury from common household thermal sources such as heating pads and hot water bottles. We sought to categorize these injuries, provide a treatment plan, and prevent these injuries in the future.
Methods:
A retrospective review of patients who had sustained burns to reconstructed breasts with household devices was performed at a single institution. A PubMed search was performed to identify and summarize articles cataloguing patients who had suffered burns to breast reconstructions.
Results:
Five patients in our practice were affected. Fifteen articles were identified in the literature search. A total of 40 patients had sustained thermal injury to reconstructed breasts, with the majority being full thickness burns (67.5%). Patients who sustained full thickness burns to reconstructed breasts were more likely to require an operative procedure compared with patients who sustained partial thickness burns (P = 0.0076).
Conclusions:
Reconstructed breasts are at risk for injury from commonly used household warming devices and ambient heat from the sun. As a result, patients should be counseled about these risks accordingly, to avoid injury or loss of reconstruction. These injuries require immediate vigilant treatment.
Sensibility of the skin to touch and temperature (cold and warmth) after immediate breast reconstruction with implants is decreased or absent postoperatively.1 This finding has also been noted in patients who have undergone autologous breast reconstruction.2 Decreased sensation after breast reconstruction has been shown to be relatively permanent.3 As a result, reconstructed breasts are vulnerable to thermal injury. In addition, patients with implants may experience a cold sensation in their reconstructed breasts in cooler ambient temperatures, which may prompt patients to use warming devices on their breasts.4
During the previous winter season in New England, multiple plastic surgeons in our division treated patients that had sustained injury to their reconstructed breasts as a result of the use of common household warming devices. The goals of this study are to characterize thermal injuries to reconstructed breasts, review the various methods of treatment, and prevent this type of injury in the future.
METHODS
A retrospective review was performed of patients in our division that underwent breast reconstruction of any modality in addition to having sustained a burn from a commonly used warming device or household device within the past year. We collected demographic information, method of reconstruction, degree of thermal injury, and outcome for each patient.
Additionally, a PubMed search was performed to identify peer-reviewed studies, case reports, or letters to the editor cataloguing thermal injuries to reconstructed breasts. Articles were culled for information about each patient, including method of reconstruction, degree of thermal injury, and outcome. Stata/IC version 13.1 was used for statistical analysis.
RESULTS
A summary of the affected patients (n = 5) from our practice is shown in Table 1. The mean age at surgery was 46 years (range, 41.3–51.5 years). One patient had diabetes mellitus. All patients had bilateral mastectomies (1 skin-sparing, 4 nipple-sparing). Three patients received radiation (2 preoperatively, 1 postoperatively). All patients had chemotherapy preoperatively, or postoperatively, or both. All patients had an implant or expander in place. One patient sustained a superficial partial thickness burn, which resolved completely (Fig. 1). The remaining 4 patients (80%) sustained full thickness burns (Fig. 2). Two patients had the implant/expander removed without further reconstruction. One patient required a latissimus dorsi flap with implant exchange (Fig. 3).
Table 1.
Massachusetts General Hospital Patients
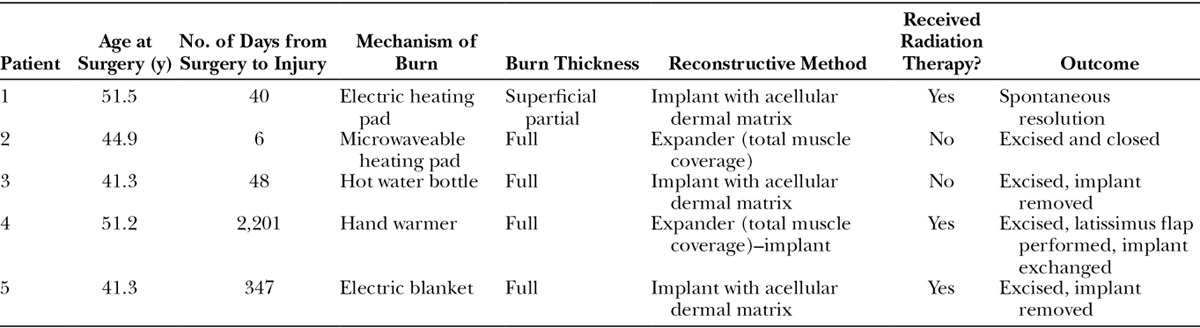
Fig. 1.
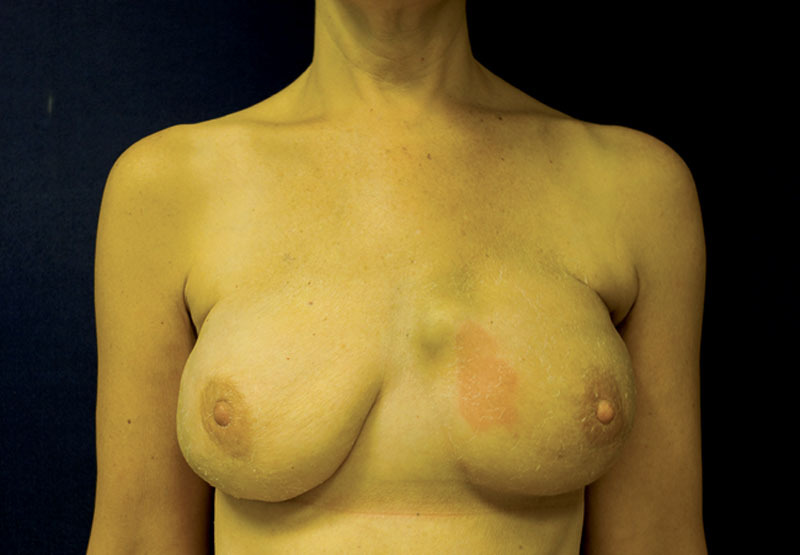
Superficial burn to left breast reconstructed with implant.
Fig. 2.
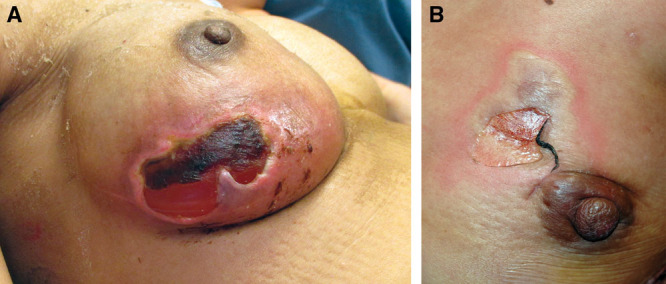
Full-thickness burns to breasts reconstructed with implants, one with implant exposure (A).
Fig. 3.
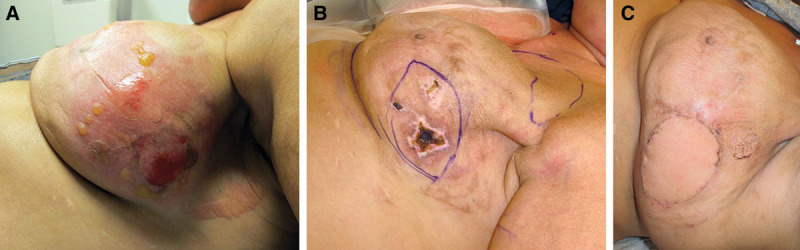
Full thickness burn, salvaged with latissimus flap and implant exchange. A, 1 week postburn. B, 4 weeks postburn. C, 6 weeks after latissimus dorsi flap.
Patient 1 was 51 years old, and had prior left breast lumpectomy and radiation therapy. She developed a recurrent cancer in the left breast, and underwent bilateral nipple-sparing mastectomies and immediate reconstruction with implants and acellular dermal matrix. She developed a focal hematoma on the left after drain removal, and the patient used a heating pad for discomfort. She developed a superficial partial thickness burn of the left breast which resolved spontaneously, as did the hematoma.
Patient 2 was 45 years old and was diagnosed with left breast cancer, which was node positive. She underwent neoadjuvant chemotherapy. She underwent bilateral nipple-sparing mastectomies and immediate reconstruction with tissue expanders using total muscle coverage. About 1 week after surgery, she had used a heating pad on the left breast for discomfort, and sustained a full thickness burn. This was treated with Silvadene for 1 week, and then without significant improvement, she was taken to the operating room and the burn was excised and closed primarily. The expander was not exposed. Two months later, the patient successfully underwent exchange of tissue expanders for implants.
Patient 3 was 41 years old, and had right breast cancer, which was node positive. She underwent neoadjuvant chemotherapy, followed by bilateral nipple-sparing mastectomies and immediate reconstruction directly with implants and acellular dermal matrix. One and a half months later, she had used a hot water bottle on the right breast for discomfort, and sustained a full thickness burn. She was taken to the operating room for removal of the right breast implant and primary closure. This sequence of events relating to the burn delayed the patient’s receipt of chemotherapy postoperatively.
Patient 4 was 51 years old, and had diabetes (type 2). She had prior left breast cancer and lumpectomy with radiation. She developed a recurrent cancer on the left, and underwent bilateral skin-sparing mastectomies and immediate reconstruction with tissue expanders with total muscle coverage. She subsequently had exchange of the tissue expanders for implants. Four years afterward, the patient placed hand warmers into her bra for a cold sensation in the implants, and she sustained a full thickness burn to the left breast. She was taken to the operating room for a latissimus flap and implant exchange.
Patient 5 was 41 years old, and was diagnosed with right breast cancer, node positive. She underwent neoadjuvant chemotherapy, followed by bilateral nipple-sparing mastectomies and immediate reconstruction with implants and acellular dermal matrix. She was diagnosed with metastatic cancer and underwent postoperative chemotherapy and radiation therapy to the right breast and multiple other sites. One year later, she used a heating blanket, and sustained a full thickness burn to the right breast with implant exposure. The implant was removed and the wound was closed primarily. One month later, the patient died of metastatic breast cancer.
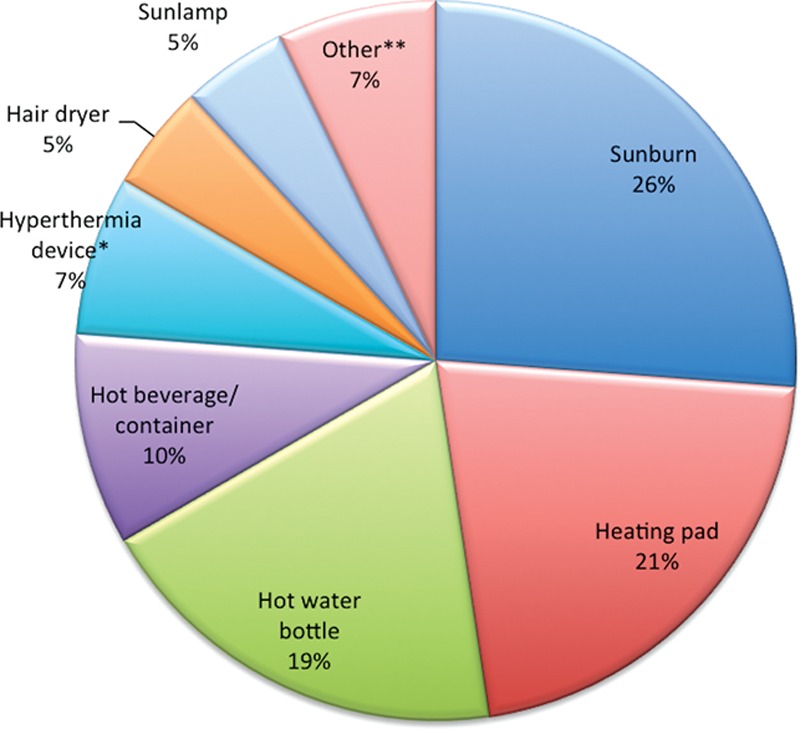
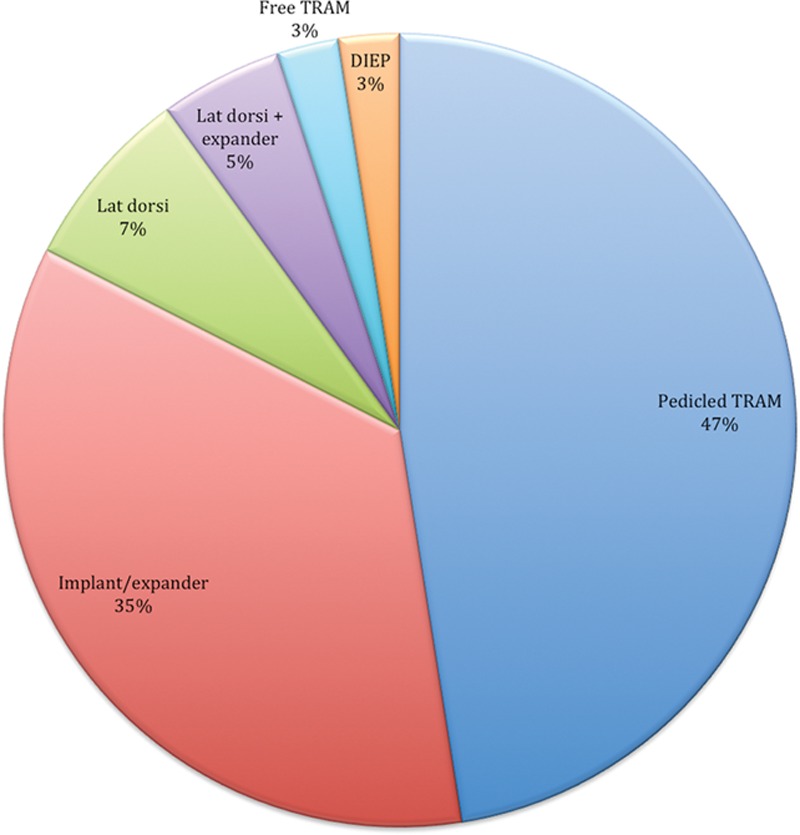
A summary of the 15 articles of the PubMed search is shown in Table 2. Combining our patients with the patients from the review, a total of 40 patients sustained thermal injury to reconstructed breasts. The top 3 most common causes of thermal injury to reconstructed breasts were sunburn (26%), heating pad (21%), and hot water bottle (19%). The frequency of burn sources responsible for injury in the 39 patients is represented in Figure 4.
Table 2.
Summary of Peer-reviewed Literature
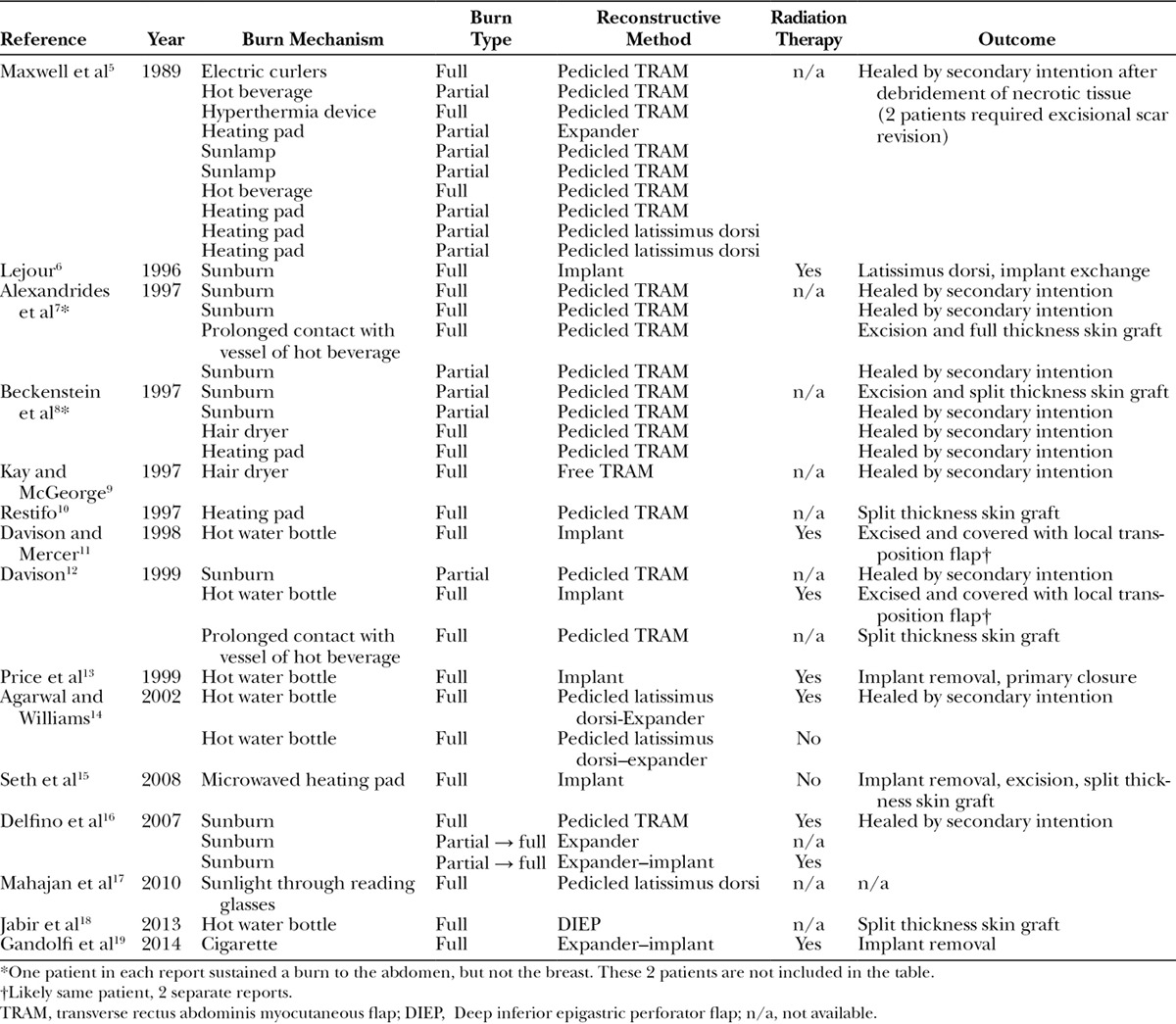
Fig. 4.
Sources of thermal injuries to reconstructed breasts. *Hyperthermia device includes electric blanket and personal warming device. **Other: 1 patient each with burns from electric curlers, cigarette, and sunlight through reading glasses.
Most patients sustained full thickness burn injury (n = 27; 67.5%). The top 3 methods of reconstruction overall were pedicled TRAM (47%), implant or expander (35%), and pedicled latissimus dorsi flap (7%; Fig. 5). Fifteen patients (5 in our group and 10 in the peer-reviewed papers) had information regarding the receipt of radiation; of those, 11 patients had received radiation. Most burns healed by secondary intention (n = 24, 60%), 11 of whom had sustained partial thickness burns (45.8%). The proportion of patients requiring treatment with a surgical procedure was significantly higher in the group that sustained full thickness burns in comparison with partial thickness burns [n = 14, 51.9% (full) versus n = 1, 8.3% (partial); P = 0.0076). Five patients had full or split thickness skin grafts, 6 had removal of the implant or expander (one required a split thickness skin graft in addition), 2 patients required salvage with latissimus dorsi flaps, and 2 had local flaps (local tissue rearrangement).
Fig. 5.
Method of reconstruction in patients sustaining thermal injury to reconstructed breasts.
CONCLUSIONS
After breast reconstruction using any available method, patients are vulnerable to thermal injury to their reconstructed breasts, because of loss of sensation.1, 20 Although a subset of patients may have partial return of sensation after breast reconstruction, there is still insufficient sensation to provide protection from exposure to commonly utilized household thermal devices such as heating pads and hot water bottles. In addition, patients are not routinely made aware of the perils of these devices on their reconstructed breasts, and it may be helpful to furnish patients with a list of such devices to avoid.
Once a patient has sustained a thermal injury to a reconstructed breast, immediate evaluation and treatment is necessary. Partial thickness burns can often be treated with local wound care and close observation. Full thickness burns are likely to require surgery (either immediately or in a delayed fashion) to remove an exposed implant or expander, and excise a full thickness burn. These patients may require split or full thickness skin grafts or a myocutaneous flap for salvage.
Burn injuries to reconstructed breasts may occur more frequently in colder climates. As such, we have added an item to our postoperative instructions for patients explicitly stating to avoid the use of warming or cooling devices on reconstructed breasts. We counsel patients to avoid direct sun exposure to reconstructed breasts in addition. We have extended these instructions to patients that have undergone free tissue transfer, as these types of injuries have been shown to also occur in patients who have undergone free tissue transfer for reconstruction of other body regions, such as the scalp or extremities.21 Patients should be notified that these risks are not just in the immediate postoperative period, and in fact do last for their lifetime.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Lagergren J, Wickman M, Hansson P. Sensation following immediate breast reconstruction with implants. Breast J. 2010;16:633–638. doi: 10.1111/j.1524-4741.2010.00984.x. [DOI] [PubMed] [Google Scholar]
- 2.Shridharani SM, Magarakis M, Stapleton SM, et al. Breast sensation after breast reconstruction: a systematic review. J Reconstr Microsurg. 2010;26:303–310. doi: 10.1055/s-0030-1249313. [DOI] [PubMed] [Google Scholar]
- 3.Unukovych D, Johansson H, Johansson E, et al. Physical therapy after prophylactic mastectomy with breast reconstruction: a prospective randomized study. Breast. 2014;23:357–363. doi: 10.1016/j.breast.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 4.Snell L, McCarthy C, Klassen A, et al. Clarifying the expectations of patients undergoing implant breast reconstruction: a qualitative study. Plast Reconstr Surg. 2010;126:1825–1830. doi: 10.1097/PRS.0b013e3181f44580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maxwell GP, Tornambe R. Second- and third-degree burns as a complication in breast reconstruction. Ann Plast Surg. 1989;22:386–390. doi: 10.1097/00000637-198905000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Lejour M. Burn of a reconstructed breast. Plast Reconstr Surg. 1996;97:1306–1307. doi: 10.1097/00006534-199605000-00041. [DOI] [PubMed] [Google Scholar]
- 7.Alexandrides IJ, Shestak KC, Noone RB. Thermal injuries following TRAM flap breast reconstruction. Ann Plast Surg. 1997;38:335–341. doi: 10.1097/00000637-199704000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Beckenstein MS, Beegle PH, Hartrampf CR., Jr Thermal injury to TRAM flaps: a report of five cases. Plast Reconstr Surg. 1997;99:1606–1609. [PubMed] [Google Scholar]
- 9.Kay AR, McGeorge D. Susceptibility of the insensate reconstructed breast to burn injury. Plast Reconstr Surg. 1997;99:927. doi: 10.1097/00006534-199703000-00068. [DOI] [PubMed] [Google Scholar]
- 10.Restifo RJ. Heating pad burn of a reconstructed breast. Plast Reconstr Surg. 1997;100:547–548. doi: 10.1097/00006534-199708000-00053. [DOI] [PubMed] [Google Scholar]
- 11.Davison JA, Mercer DM. Accidental burns following subcutaneous mastectomy and reconstruction with a prosthesis. Br J Plast Surg. 1998;51:486. doi: 10.1016/s0007-1226(98)80037-4. [DOI] [PubMed] [Google Scholar]
- 12.Davison JA. Burns to reconstructed breasts. Ann R Coll Surg Engl. 1999;81:19–22. [PMC free article] [PubMed] [Google Scholar]
- 13.Price RK, Mokbel K, Carpenter R. Hot-water bottle induced thermal injury of the skin overlying Becker’s mammary prosthesis. Breast. 1999;8:141–142. doi: 10.1054/brst.1999.0053. [DOI] [PubMed] [Google Scholar]
- 14.Agarwal SK, Williams MR. Burn injuries after latissimus dorsi breast reconstruction in a cold climate. Breast. 2002;11:270–272. doi: 10.1054/brst.2001.0413. [DOI] [PubMed] [Google Scholar]
- 15.Seth R, Lamyman MJ, Athanassopoulos A, et al. Too close for comfort: accidental burn following subcutaneous mastectomy and immediate implant reconstruction. J R Soc Med. 2008;101:39–40. doi: 10.1258/jrsm.2007.070032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Delfino S, Brunetti B, Toto V, et al. Burn after breast reconstruction. Burns. 2008;34:873–877. doi: 10.1016/j.burns.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Mahajan AL, Chapman TW, Mandalia MR, et al. Sun burn as a consequence of resting reading glasses on a reconstructed breast. J Plast Reconstr Aesthet Surg. 2010;63:e170. doi: 10.1016/j.bjps.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Jabir S, Frew Q, Griffiths M, et al. Burn injury to a reconstructed breast via a hot water bottle. J Plast Reconstr Aesthet Surg. 2013;66:e334–e335. doi: 10.1016/j.bjps.2013.06.031. [DOI] [PubMed] [Google Scholar]
- 19.Gandolfi S, Vaysse C, Garrido I, et al. Burn injury to a reconstructed breast via a cigarette causing implant exposure. The importance of the patient’s education. Breast J. 2014;20:543–544. doi: 10.1111/tbj.12314. [DOI] [PubMed] [Google Scholar]
- 20.Lagergren J, Edsander-Nord A, Wickman M, et al. Long-term sensibility following nonautologous, immediate breast reconstruction. Breast J. 2007;13:346–351. doi: 10.1111/j.1524-4741.2007.00441.x. [DOI] [PubMed] [Google Scholar]
- 21.Butler CE, Davidson CJ, Breuing K, et al. Thermal injuries to free flaps: better prevented than treated. Plast Reconstr Surg. 2001;107:809–812. doi: 10.1097/00006534-200103000-00023. [DOI] [PubMed] [Google Scholar]


