Abstract
Background:
To compare the margin reflex distance of the upper (MRD-1) and lower (MRD-2) eyelids and the eyebrow height (EBH) in patients with involutional and hard contact lens wear--induced blepharoptosis before and after ptosis surgery.
Methods:
Sixty patients with acquired blepharoptosis were studied. Group 1 consisted of 30 patients with involutional ptosis (age, 75.8 ± 6.4 years), and group 2 consisted of 30 patients with hard contact lens wear–induced ptosis (age, 50.2 ± 7.1 years). All patients underwent bilateral, CO2 laser–assisted levator aponeurosis advancement surgery. A digital image was taken in the primary position before and 2 months after the surgery. The image was analyzed by the ImageJ (NIH, Bethesda, Md.) software. Parameters included MRD-1, MRD-2, EBH, and ocular surface area (OSA).
Results:
After surgery, all patients had a significant increase in the MRD-1 and OSA and a decrease in the EBH (all P < 0.001). The increase in MRD-1 was significantly larger in group 1 than in group 2 (P = 0.028). The decrease of EBH was significantly greater in group 1 than in group 2 (P = 0.007). Group 1 had a slight decrease in the MRD-2, but group 2 had a significant increase after surgery (P = 0.026). The change in the OSA was not significantly different between the 2 groups.
Conclusions:
Digital image analyses can be used for precise measurements of the eyelid features. The disparity in the changes of eyelid and eyebrow features between the 2 groups may suggest different responses of the external eyelid muscles to surgery between cases of different etiology.
Blepharoptosis is an abnormal drooping of the upper eyelid that is observed when the eye is at primary position. Levator advancement surgery is a commonly used method to effectively treat this disorder.1–4 A restoration of the upper visual field and an improvement and rejuvenation of the facial appearance after levator advancement surgery are true and precious clinical targets and the outcomes are greatly appreciated by our patients.
At present, studies on the effectiveness of ptosis repair surgery typically use the height of the palpebral aperture in the midpupillary line as a measure of success. The conventional measure used to quantify the palpebral aperture is the margin reflex distance (MRD) which is defined as the vertical distance between the corneal light reflex and the upper (MRD-1) and lower (MRD-2) eyelid margins. However, this parameter is 1-dimensional, and the measurement of the MRD relies on the examiner’s experience. Detailed analyses of the eyelid contour including the ocular surface area (OSA) and eyebrow position, which are known to change after eyelid surgery, are important for the characterization of not only the features of the eyelid and ocular surface but also the facial appearance.5–7 Information of these parameters is necessary for both patients and surgeons to evaluate the outcome of ptosis repair surgery.
With the development of digital imaging technology and the analyzing software, the eyelid features can be assessed more accurately and quantitatively. There have been several studies using digital analyses of external photographs of the eye for the evaluation of the preoperative and postoperative eyelid and eyebrow features.5, 6, 8–10 Koushan et al5 reported using the Photoshop software to analyze the OSA of patients who had undergone ptosis repair surgery. They concluded that this simple method can quantify the OSA and was a good method to evaluate the postoperative changes. Prado et al8 used the ImageJ software to measure the angle of the eyebrow before and after blepharoplasty, and reported that the eyebrow tended to move down after surgery. To the best of our knowledge, there have been no reports in a single study documenting the changes of OSA, MRD, and eyebrow position, and no comparative studies focused on these changes between involutional and contact lens wear--induced ptosis.
Thus, the purpose of this study was to analyze the upper eyelid position, MRD-1, the lower eyelid position, MRD-2, the OSA, and the eyebrow height (EBH) before and after ptosis repair surgery. To accomplish this, we studied 2 groups of patients: the first group consisted of 30 patients with involutional ptosis, and the second group consisted of 30 patients with contact lens wear--induced ptosis. All the subjects underwent bilateral, CO2 laser–assisted levator aponeurosis advancement surgery.
PATIENTS AND METHODS
Subjects
Patients who were examined at the Department of Ophthalmology, Ehime University Hospital or Hanamizuki Eye Clinic with bilateral involutional or contact lens wear–induced blepharoptosis between December 2014 and June 2016 were studied. Patients with an MRD-1 <2.5 mm were included. The exclusion criteria were corneal changes precluding accurate measurements, use of sympathomimetic drugs or eye drops, prior eyelid surgery, other types of ptosis, for example, congenital, traumatic, or mechanical, and myopathies.
All subjects were informed on the procedures to be used and the possible complications, and a signed informed consent was obtained. This study was approved by the Ethics Committee of Ehime University Hospital and Hanamizuki Eye Clinic.
The patients were separated into 2 groups according to the etiology of blepharoptosis. Group 1 consisted of 30 patients with involutional ptosis (mean age, 75.8 ± 6.4 years), and group 2 consisted of 30 patients with contact lens wear–induced ptosis (mean age, 50.2 ± 7.1 years).
Surgical Procedures
All patients underwent standard bilateral, CO2 laser–assisted levator aponeurosis advancement surgery by the same surgeon (X.Z.). In brief, an incision was made at about 5 mm above the upper eyelid margin. Redundant skin was resected for 5–10 mm in width if necessary. The subcutaneous tissue was dissected, and the levator aponeurosis was isolated and advanced by 8–10 mm using 6-0 Asflex suture (polyvinylidene fluoride, CROWNJUN KONO CO., LTD, Chiba, Japan). The upper eyelid margin was fixed at approximately 1 mm lower from the upper corneal limbus and the proper eyelid position was confirmed while the patient was in a sitting position. Finally, interrupted sutures using 6-0 nylon were made to close the skin (Fig. 1). All subjects were examined on the first day after the surgery and again 1 week later, and the sutures were removed at 7–10 days after the surgery. Ofloxacin ophthalmic ointment (0.3%; Tarivit, Santen Co., Osaka, Japan) was applied twice a day onto the wound for 2 weeks.
Fig. 1.
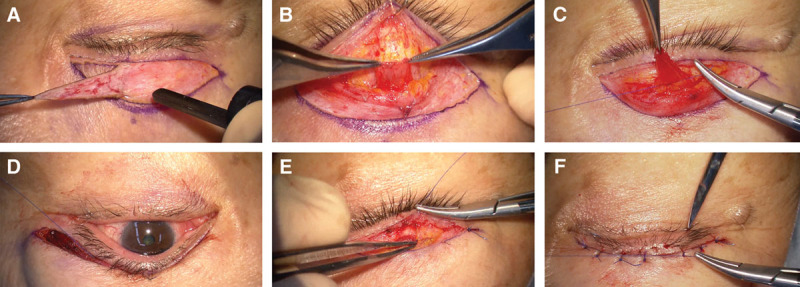
Surgical procedure for blepharoptosis repair with CO2 laser. Redundant skin was removed (A), the levator muscle and tarsus were exposed (B), and levator muscle was advanced for about 8–10 mm and sutured to the center of tarsus (C). The upper eyelid margin was positioned at about 1 mm lower from the corneal limbus (D). Subcutaneous tissue was sutured to tarsus at 2–3 points for double layer formation (E) and interrupted sutures were made to close the skin (F).
Image Processing and Measurements
Frontal photographs were taken preoperatively and at 2 months postoperatively with the eyes in the primary position. A Nikon 5500 digital camera (Nikon, Osaka, Japan) with strobe light was used. The digital images were analyzed with the ImageJ software (version 1.45, NIH, Bethesda, Md.), with the Java platform version 1.6.
The following parameters were measured and evaluated: MRD-1, the vertical distance between upper eyelid margin and corneal light reflex; MRD-2, the distance between lower eyelid margin and corneal light reflex; EBH, the distance between the center of eyebrow and the corneal light reflex; and OSA, the area surrounded by the upper and lower margins of the eyelid which was manually traced, and the area was automatically calculated by the software (Fig. 2). If the upper eyelid covered the corneal light reflex, the putative center of a circle overlapping the corneal limbus was deemed as the corneal light reflex. Then, the MRD-1 was measured and expressed as a negative value. The measurements were made by 2 of the authors (X.Z. and T.G.), and the average was used for statistical analyses.
Fig. 2.

Measurements of the eyelid and eyebrow parameters by the ImageJ (NIH, Bethesda, Md.) software. The radius of the cornea was used as a standard scale of 5.5 mm (A). The following parameters were measured and analyzed: (1) the eyelid MRD of the upper (MRD-1) and lower (MRD-2) eyelids; (2) EBH, measured as the vertical distance from the center of the eyebrow to the pupil center (B); (3) OSA, calculated automatically by the software following the delineation of the eyelid margins manually (C). If the upper eyelid covered the corneal light reflex, the putative center of a circle overlapping the corneal limbus was deemed as the corneal light reflex. Then the MRD-1 was measured and expressed as a negative value.
Statistical Analysis
All data were analyzed by JMP, version 9.1 (Japan). Data are expressed as the means ± SD. The significance of the difference in the sex distribution in group 1 and group 2 was analyzed by Tukey’s test. For all other parameters, significance of the differences between the preoperative and postoperative values for the 2 groups was determined by Student’s t tests. A P <0.05 was taken to be statistically significant.
RESULTS
Outcome of Levator Aponeurosis Advancement Surgery
Both groups had 30 subjects (60 eyes), and the sex distribution between the 2 groups was not significantly different (P = 0.732, Tukey’s test). The patients in group 1 with involutional ptosis were significantly older than the patients in group 2 (P < 0.0001, Student’s t test). None of the patients had any complications during and after the surgery. The average operating time was 51.5 ± 13.8 minutes for group 1 and 48.2 ± 10.6 minutes for group 2 (P = 0.376, Student’s t test). The time of suture removal was also not significantly different between the 2 groups (P = 0.884, Student’s t test). There was no difference of sex in all the parameters (MRD, OSA, and EBH) analyzed for each group. A reoperation was not needed for all subjects during the observation period. Photographs of representative cases are shown in Figure 3.
Fig. 3.
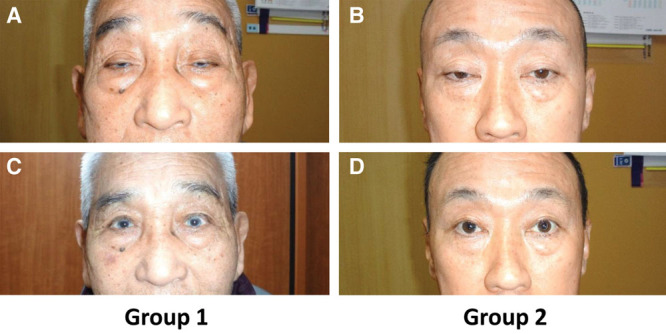
Representative photographs of patients from group 1 and group 2 before (A, B) and after (C, D) blepharoptosis surgery.
Changes in Eyelid Features and Eyebrow Position
Before the surgery, MRD-1 was −0.56 ± 1.82 mm in group 1, which was significantly smaller than 0.64 ± 1.71 mm in group 2 (P = 0.016, Student’s t test). After surgery, MRD-1 was 3.14 ± 0.67 mm in group 1 and 3.66 ± 0.54 mm in group 2. Both values were significantly larger than the preoperative values (both P < 0.001, paired t tests). There was no significant difference in MRD-1 between the 2 groups after surgery (P = 0.742, Student’s t tests).
MRD-2 was 4.48 ± 1.26 mm in group 1 and 4.36 ± 0.75 mm in group 2 before surgery, and it was 4.15 ± 0.68 mm in group 1 and 4.68 ± 0.67 mm in group 2 after the surgery. The difference in MRD-2 between the 2 groups before surgery was not significant (P = 0.692, Student’s t test); however, MRD-2 was significantly larger in group 2 than group 1 after the surgery (P = 0.008, Student’s t test). In addition, MRD-2 after the surgery in group 2 was significantly larger than that before surgery (P = 0.026, paired t test).
The OSA was 58.26 ± 19.04 mm2 for group 1 and 63.71 ± 17.25 mm2 for group 2. The OSA increased to 100.17 ± 20.63 mm2 in group 1 and 103.15 ± 19.69 mm2 in group 2 after the surgery. The increase in the OSA was statistically significant for both groups (both P < 0.001, paired t test), and the differences between the 2 groups before and after the surgery were not significant.
The EBH was 30.16 ± 8.25 mm for group 1 and 22.09 ± 3.88 mm for group 2 before the surgery. The EBH was 25.71 ± 7.33 mm in group 1 and 19.64 ± 3.82 mm in group 2 after the surgery. The EBH was significantly larger in group 1 than in group 2 before and after surgery (all P < 0.001, Student’s t test). Both groups had a significant decrease in the EBH after the surgery (all P <0.001, paired t test). Also, the decrease of the EBH was significantly greater in group 1 than in group 2 (P = 0.007, Student’s t test).
Correlation of EBH and MRD-1 Corrected
To eliminate the effect of the difference in the corrected volume between the 2 groups, we also evaluated the ratio of the EBH to the MRD-1 (EBH/MRD-1) of both groups. The EBH/MRD-1 was 1.17 ± 1.09 for group 1 and 1.12 ± 0.84 for group 2. The difference between the 2 groups was not significant (P = 0.863, Student’s t test).
The correlation between the MRD-1 corrected and EBH change was analyzed in all subjects. The EBH change was significantly and positively correlated with the MRD-1 corrected (P = 0.0003; r = 0.4528, Spearman correlation coefficient; Fig. 4). The correlation between the EBH change and MRD-1 corrected volume is
Fig. 4.
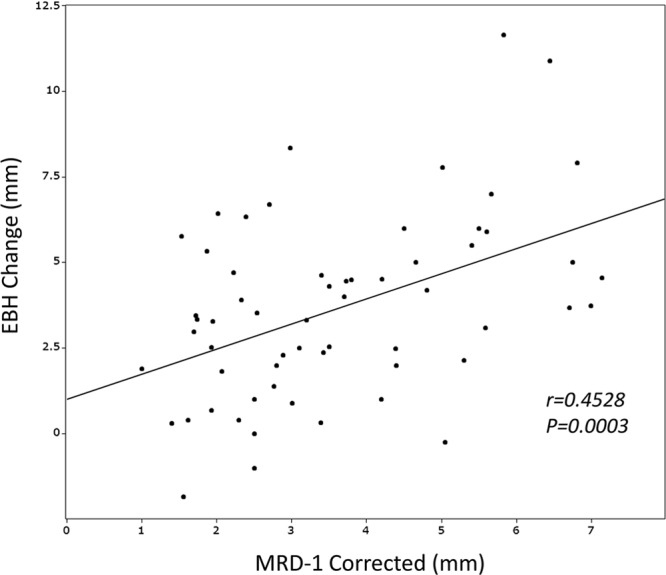
Correlation of the change in the EBH and MRD-1 corrected. EBH changes are significantly and positively correlated to the MRD-1 corrected (P = 0.0003; r = 0.4528, Spearman correlation coefficient).
where R = MRD-1 corrected.
DISCUSSION
Blepharoptosis not only reduces the extent of the superior visual field but can impair reading and other close-work activities.11, 12 Also, the asymmetry and aging appearance can compromise the quality of vision and quality of life of the patients. The advancement of levator aponeurosis is an effective surgical approach to restore the levator palpebral function and rejuvenate the facial appearance.1–4
Our results showed that computerized image analyses can be used to determine the outcome of ptosis surgery quantitatively. The analysis is simple and precise, and images of the 2 eyes can be analyzed in less than 5 minutes. The interobserver correlation coefficient of the parameters measured varies between 0.91 and 0.95 (data not shown).
Another advantage of using the ImageJ software to analyze the image is that the digital photographs and data can be permanently stored in a computer and recalled when consulting with a patient on the outcome of the surgery, and for following the postoperative course of recovery or planning a repeated surgery.
The involutional ptosis (group 1) had a significantly lower MRD-1 than the contact lens wear–induced ptosis (group 2) preoperatively. This may be because the eyelids of patients with involutional ptosis were more sagged; hence, they required a larger resection of the eyelid skin. As a result, the position of the eyebrow, the EBH, decreased more in group 1 than in group 2. This change is reasonable because the decrease in the upper eyelid volume can reduce the need of the frontalis muscle contraction leading to a lowering of the eyebrow.
The changes in the lower eyelid height (MRD-2) were significantly different between the 2 groups. Group 1 had a slight and not significant decrease in the MRD-2, whereas in group 2 this parameter was significantly increased after surgery. Coupled with the MRD-1 alterations, the OSAs between the 2 groups were not significantly different before and after surgery.
One possible mechanism for the difference in the MRD-2 changes is that there is a reduction in the neural stimulation to the orbicularis oculi caused by the ptosis repair. Another reason for this phenomenon is aging, which causes an attenuation, dehiscence, or looseness of the lower eyelid retractors.13, 14 The lower eyelid may be elevated slightly in older patients (decreased MRD-2), whereas the younger patients had the effect of lower eyelid traction (increased MRD-2) after the surgery.
In contrast, Matsuo et al15 reported that there is an additional contraction of the inferior rectus muscle in eyes with blepharoptosis which pulls the inferior suspensory ligament of Lockwood and the capsulopalpebral fascia downward. This contraction retracts the lower eyelid resulting in inferior scleral show, which is a sign of a disinsertion of the levator aponeurosis from the tarsus.15
Although our findings of the decrease of MRD-2 in group 1 were consistent with the findings of Matsuo et al,15 the MRD-2 in the group 2 was significantly increased. This discrepancy may be due to the differences in the age, etiology of the cause, and the methodology of the measurements. The age difference may account for different responses of orbicularis oculi muscle and/or lower eyelid retractors after surgery. One of the etiological factors in contact lens ptosis has been reported to be due to the Müller’s muscle fibrosis.16 We evaluated the MRD with an imaging analysis software, whereas Matsuo et al15 measured the area enclosed by the lower eyelid margin and medial and lateral canthi.
There are some limitations in this study. Our measurements using the corneal light reflex could be influenced by a slight rotation of the eye. However, all photographs were taken under the same conditions, and the image analyses were conducted in the same manner for both groups preoperatively and postoperatively. Under these conditions, the differences found must be valid. Changes of the lower eyelid could be slight and variable according to the evaluation method applied; future studies using more accurate and objective techniques are needed. Furthermore, difference may also exist in other types of blepharoptosis and it is known that there is a considerable anatomical difference in the eyelid and surrounding tissue of Orientals and Westerners.17 This also warrants future studies on patients of different origin to determine the intrinsic changes of the eyelid features.
In conclusion, our results showed that digital image analysis is feasible and useful in quantifying the changes of the eyelid and eyebrow after ptosis surgery. The external eyelid muscles, including the orbicularis oculi muscle and lower eyelid retractor, may respond differently after surgery for blepharoptosis of different etiology.
ACKNOWLEDGMENTS
The authors thank Dr. Tomoyuki Kamao (Ehime University School of Medicine) and Dr. Eri Ishikawa (Ehime Prefecture Hospital) for their invaluable advice on this work.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Kakizaki H, Zako M, Mito H, et al. A guide to making a natural eyelid margin curvature in blepharoptosis surgery. Acta Ophthalmol Scand. 2004;82:240–241. doi: 10.1111/j.1600-0420.2004.00150b.x. [DOI] [PubMed] [Google Scholar]
- 2.Noma K, Takahashi Y, Leibovitch I, et al. Transcutaneous blepharoptosis surgery: simultaneous advancement of the levator aponeurosis and Müller’s muscle (levator resection). Open Ophthalmol J. 2010;4:71–75. doi: 10.2174/1874364101004010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wada Y, Hashimoto T, Kakizaki H, et al. What is the best way to handle the involutional blepharoptosis repair? J Craniofac Surg. 2015;26:e377–e380. doi: 10.1097/SCS.0000000000001840. [DOI] [PubMed] [Google Scholar]
- 4.Leclère FM, Alcolea J, Mordon S, et al. Long-term outcomes of laser assisted blepharoplasty for ptosis: about 104 procedures in 52 patients. J Cosmet Laser Ther. 2013;15:193–199. doi: 10.3109/14764172.2012.758385. [DOI] [PubMed] [Google Scholar]
- 5.Koushan K, Skibell BC, Harvey JT, et al. Digital photography as a novel technique of measuring ocular surface dimensions. Orbit. 2008;27:259–265. doi: 10.1080/01676830802222811. [DOI] [PubMed] [Google Scholar]
- 6.Tsai PY, Wu YC, Lai CH, et al. Ocular surface area changes after double eyelidplasty. J Plast Reconstr Aesthet Surg. 2012;65:e141–e145. doi: 10.1016/j.bjps.2012.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Cruz AA, Coelho RP, Baccega A, et al. Digital image processing measurement of the upper eyelid contour in Graves disease and congenital blepharoptosis. Ophthalmology. 1998;105:913–918. doi: 10.1016/S0161-6420(98)95037-0. [DOI] [PubMed] [Google Scholar]
- 8.Prado RB, Silva-Junior DE, Padovani CR, et al. Assessment of eyebrow position before and after upper eyelid blepharoplasty. Orbit. 2012;31:222–226. doi: 10.3109/01676830.2011.648801. [DOI] [PubMed] [Google Scholar]
- 9.Flynn TH, Rose GE, Shah-Desai SD. Digital image analysis to characterize the upper lid marginal peak after levator aponeurosis repair. Ophthal Plast Reconstr Surg. 2011;27:12–14. doi: 10.1097/IOP.0b013e3181eea2e3. [DOI] [PubMed] [Google Scholar]
- 10.Nishihira T, Ohjimi H, Eto A. A new digital image analysis system for measuring blepharoptosis patients’ upper eyelid and eyebrow positions. Ann Plast Surg. 2014;72:209–213. doi: 10.1097/SAP.0b013e31825b8fb7. [DOI] [PubMed] [Google Scholar]
- 11.Federici TJ, Meyer DR, Lininger LL. Correlation of the vision-related functional impairment associated with blepharoptosis and the impact of blepharoptosis surgery. Ophthalmology. 1999;106:1705–1712. doi: 10.1016/S0161-6420(99)90354-8. [DOI] [PubMed] [Google Scholar]
- 12.Cahill KV, Bradley EA, Meyer DR, et al. Functional indications for upper eyelid ptosis and blepharoplasty surgery: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118:2510–2517. doi: 10.1016/j.ophtha.2011.09.029. [DOI] [PubMed] [Google Scholar]
- 13.Cho WK, Paik JS, Han SH, et al. Microscopic characteristics of lower eyelid retractors in Koreans. Korean J Ophthalmol. 2011;25:344–348. doi: 10.3341/kjo.2011.25.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schaefer AJ. Variation in the pathophysiology of involutional entropion and its treatment. Ophthalmic Surg. 1983;14:653–655. [PubMed] [Google Scholar]
- 15.Matsuo K, Kondoh S, Kitazawa T, et al. Pathogenesis and surgical correction of dynamic lower scleral show as a sign of disinsertion of the levator aponeurosis from the tarsus. Br J Plast Surg. 2005;58:668–675. doi: 10.1016/j.bjps.2004.12.032. [DOI] [PubMed] [Google Scholar]
- 16.Watanabe A, Araki B, Noso K, et al. Histopathology of blepharoptosis induced by prolonged hard contact lens wear. Am J Ophthalmol. 2006;141:1092–1096. doi: 10.1016/j.ajo.2006.01.032. [DOI] [PubMed] [Google Scholar]
- 17.Watanabe K. Measurement method of upper blepharoplasty for orientals. Aesthetic Plast Surg. 1993;17:1–8. doi: 10.1007/BF00455042. [DOI] [PubMed] [Google Scholar]


