Summary:
Upper extremity reconstruction is most often encountered in trauma patients. Although the rate of complications from elective orthopedic procedures remains relatively low, these complications are oftentimes in the form of open joints or joint infections that can be devastating. Classically, wounds of the shoulder girdle have been treated with large muscles such as the pectoralis major, pectoralis minor, and latissimus dorsi. Flaps more local to the area including the deltoid muscle flap have been overlooked due to their small size. Despite its size, the anterior deltoid can be used for shoulder girdle reconstruction with minimal functional deficit and allows for reconstruction of the glenohumeral joint without sacrifice of the larger muscles of the upper trunk. This study reports a case of a chronic shoulder girdle wound and successful management with the use of an anterior deltoid muscle flap.
TECHNIQUE
The patient is a 66-year-old female with a nonhealing wound of the right anterior shoulder after a mini-rotator cuff procedure with resulting infection and draining wound of the glenohumeral joint. She was found to have methicillin-sensitive Staphylococcus aureus infection. The patient underwent multiple washouts and debridements of the wound and was placed on an 8-week course of intravenous antibiotics and vacuum-assisted closure therapy. Despite vacuum-assisted closure therapy and intravenous antibiotics, the open wound persisted.
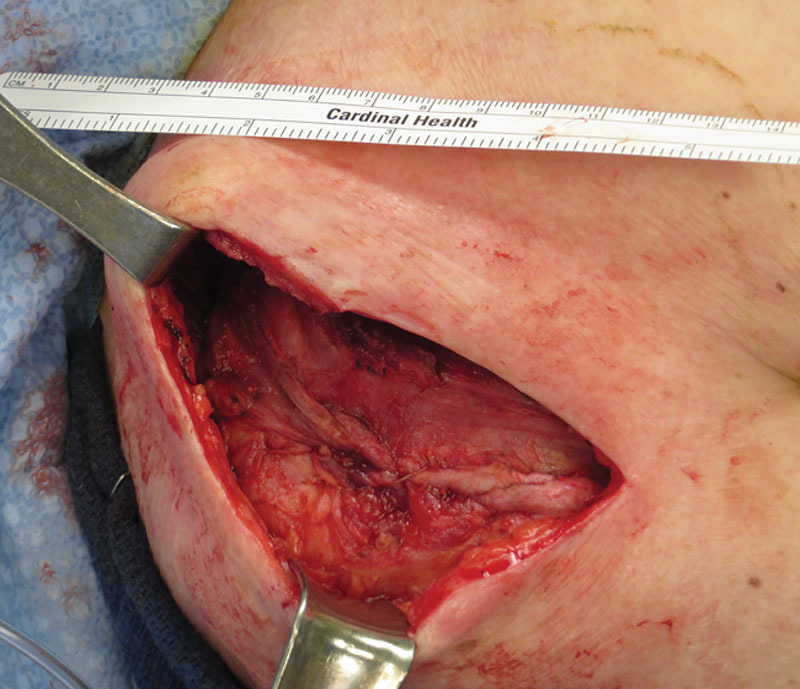
The patient was taken for muscle flap closure in an attempt to close the wound. The open wound was debrided and the surgical site extended superiorly and inferiorly along the resting skin tension lines of the shoulder (Fig. 1). The glenohumeral joint was debrided and thoroughly irrigated. The anterior deltoid muscle was then isolated and dissected free of the lateral head of the deltoid. The anterior deltoid was freed posteriorly while protecting the vascular perforators. Once completely mobilized in the deep plane, the anterior investing fascia was incised to allow for greater muscle mobility (Fig. 2). The anterior deltoid was transposed laterally and sutured to the lateral deltoid with 0-Vicryl sutures over a Hemovac drain placed in the joint (Fig. 3). The skin was then closed in a layered fashion over a Jackson–Pratt drain. The patient was immobilized for 2 weeks and then allowed to start physical therapy under the care of her orthopedic surgeon.
Fig. 1.

Debrided open wound with extension of the wound to access deltoid.
Fig. 2.

Tension-free movement of the anterior deltoid.
Fig. 3.
Anterior head of the deltoid transposed laterally and reattached to the lateral head of the deltoid.
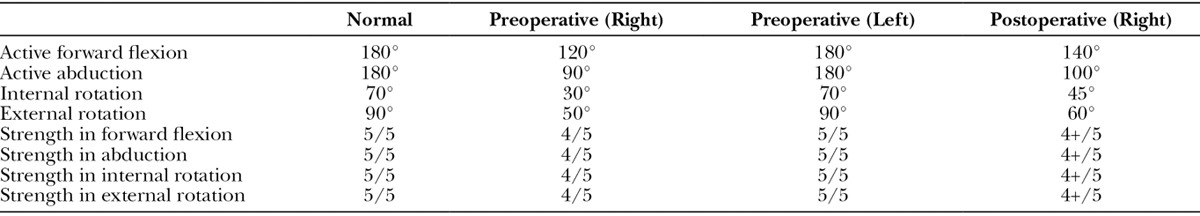
One year postoperatively, the patient maintains excellent motion in the shoulder with only mild difference in motion with the contralateral shoulder (Table 1).
Table 1.
Strength and Mobility Values Preoperatively and Postoperatively
DISCUSSION
The deltoid muscle has been used in reconstructive surgery, particularly in muscle transfers of the upper extremity due to nerve injuries.1 However, there are few reports of the use of the deltoid to reconstruct defects of the shoulder.2
The deltoid muscle is the largest and the most important muscle of the glenohumeral joint. The deltoid consists of 3 sections: the anterior deltoid, the lateral (middle) third of the deltoid, and the posterior deltoid.3 The origin of the deltoid is collagen poor, whereas the insertion is the confluence of the muscle fibers into a broad V-shaped tendon. Although considered the same muscle, the 3 sections of the deltoid differ in internal structure and function.4 The anterior deltoid and the posterior deltoid have a configuration of parallel fibers and a longer excursion compared with the lateral third. The lateral third is multipennate and stronger and has a shorter excursion. The middle third takes part in all motions that elevate the humerus.
Elevation in the scapular plane involves the anterior and lateral thirds of the deltoid, with increasing involvement of the posterior third above 90°. Abduction in the coronal plane has decreased contribution of the anterior third and increased contribution of the posterior third. Flexion is produced through the actions of the anterior and lateral thirds with contributions from the clavicular head of the pectoralis major, which shares many functions with the anterior third of the deltoid and the biceps. The actions of the pectoralis and the biceps are so small that, without the deltoid, the arm could not be held up against gravity.5
Innervation of the deltoid is supplied by the axillary nerve (C5–C6), which splits within the quadrilateral space and enters the posterior third of the muscle to travel along the medial and inferior borders of the posterior deltoid. The anterior two-thirds of the deltoid is innervated by a branch of the axillary nerve that ascends superiorly and anteriorly, approximately 6.5 cm inferior to the acromion.6
The vascular supply of the deltoid is largely derived from the posterior humeral circumflex artery that travels with the axillary nerve to the deep surface of the muscle. The deltoid is also supplied by the deltoid branch of the thoracoacromial artery that provides the blood supply to the majority of the anterior muscle.7
The general principles in the pathogenesis of shoulder sepsis are: hematogenous seeding, contiguous spread from adjacent metaphyseal osteomyelitis, and penetration of the joint by trauma or surgery. Shoulder sepsis is uncommon due to normal defense mechanisms, the use of antibiotics, and an excellent local blood supply. Most joint infections are caused by hematogenous spread. Infection rates after arthroscopy are low ranging between 0.4% and 3.4%.8 Systemic antibiotic therapy should begin immediately after diagnosis. Most orthopedic surgeons believe that the nature of shoulder sepsis demands surgical intervention.9 Surgical drainage allows for the debridement of necrotic bone and drainage of any abscesses, converting an infection with necrotic substrate to a region with well-vascularized tissue that is readily penetrated by bloodborne antibiotics.
Classically, the larger muscles of the trunk have been described for reconstruction of the shoulder. The pectoralis muscle and the latissimus dorsi can both be turned over after disinsertion to cover defects of the glenohumeral joint.10 Whereas these muscles can be used to cover large defects that may involve both skin and soft tissue, the deltoid muscle can be used to provide coverage for smaller defects in the joint. There is minimal donor site morbidity because the muscle is localized to the area that requires coverage. Furthermore, because the anterior deltoid has functional redundancy with the pectoralis major and the biceps, there is very little detriment to movement of the anterior deltoid.
There was a decrease in the range of motion with muscle reconstruction; however, this decrease was not solely due to use of the deltoid. Internal derangement of the joint, as with arthritis and rotator cuff injury for which most shoulder surgery is performed, causes a decrease in motion before use of the muscle flap. In addition, with soft tissue coverage and the infection eradicated, salvage procedures such as total shoulder and reverse total shoulder arthroplasty are future possibilities for the involved glenohumeral joint.
CONCLUSIONS
The deltoid muscle is the largest and most important muscle of the shoulder girdle. Although small when compared with the “work-horse” muscles of the anterior and posterior trunk, the deltoid can provide excellent muscle coverage of anterior defects in the glenohumeral joint with little functional deficit after muscle movement.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge will be paid by the Long Island Plastic Surgical Group, PC.
REFERENCES
- 1.Chuang DC, Hattori Y, Ma And HS, et al. The reconstructive strategy for improving elbow function in late obstetric brachial plexus palsy. Plast Reconstr Surg. 2002;109:116–126; discussion 127. doi: 10.1097/00006534-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Munnoch DA, Herbert KJ, Morris AM, et al. The deltoid muscle flap: anatomical studies and case reports. Br J Plast Surg. 1996;49:310–314. doi: 10.1016/s0007-1226(96)90161-7. [DOI] [PubMed] [Google Scholar]
- 3.Klepps S, Auerbach J, Calhon O, et al. A cadaveric study on the anatomy of the deltoid insertion and its relationship to the deltopectoral approach to the proximal humerus. J Shoulder Elbow Surg. 2004;13:322–327. doi: 10.1016/j.jse.2003.12.014. [DOI] [PubMed] [Google Scholar]
- 4.Abbott LC, Lucas DB. The tripartite deltoid and its surgical significance in exposure of the scapulohumeral joint. Ann Surg. 1952;136:392–403. doi: 10.1097/00000658-195209000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colachis SC, Jr, Strohm BR, Brechner VL. Effects of axillary nerve block on muscle force in the upper extremity. Arch Phys Med Rehabil. 1969;50:647–654. [PubMed] [Google Scholar]
- 6.Ball CM, Steger T, Galatz LM, et al. The posterior branch of the axillary nerve: an anatomic study. J Bone Joint Surg Am. 2003;85-A:1497–1501. doi: 10.2106/00004623-200308000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Reid CD, Taylor GI. The vascular territory of the acromiothoracic axis. Br J Plast Surg. 1984;37:194–212. doi: 10.1016/0007-1226(84)90010-9. [DOI] [PubMed] [Google Scholar]
- 8.Bigliani LU, Flatow EL, Deliz ED. Complications of shoulder arthroscopy. Ortho Rev. 1991;20:743–751. [PubMed] [Google Scholar]
- 9.Mehta P, Schnall SB, Zalavras CG. Septic arthritis of the shoulder, elbow, and wrist. Clin Orthop Relat Res. 2006;451:42–45. doi: 10.1097/01.blo.0000229322.30169.29. [DOI] [PubMed] [Google Scholar]
- 10.Rosenberg L, Mahler D. Extended rotation-transposition of the pectoralis major myocutaneous flap in the repair of lesions over the shoulder. Br J Plast Surg. 1981;34:322–325. doi: 10.1016/0007-1226(81)90021-7. [DOI] [PubMed] [Google Scholar]


