Abstract
Introduction
Bisphosphonate therapy (BT) is used commonly in the management of osteoporosis. A systematic review was conducted investigating delayed union of lower limb, long bone fractures in patients on BT. We specifically assessed whether BT increases the risk of delayed union or non-union in lower limb, long bone fractures.
Methods
A literature search was conducted in the PubMed and Embase™ on 4 November 2014. Articles that investigated lower limb fractures, history of BT and fracture union were included in the review.
Results
A total of 9,809 papers were retrieved and 14 were deemed suitable for this review. The mean time to union in patients on BT was 8.5 months. A longer time to union was reported in a study investigating BT users versus controls (6.5 vs 4.8 months respectively). The mean rate of delayed or non-union for BT associated atypical fractures was 20% per fracture. Specifically in one study, delayed union was more common in the cohort with more than three years of BT (67%) than in the group with less than three years of BT (26%). Surgical fixation was associated with improved outcomes compared with non-operative management.
Conclusions
BT has been described to be associated with multiple adverse outcomes related to atypical fractures. Current evidence recommends operative management for this patient group. Further investigation is required to evaluate the exact effects of BT on lower limb fractures, in particular typical femoral fractures.
Keywords: Bisphosphonate, Delayed union, Non-union, Bone suppression
Bisphosphonates or diphosphonates are the most commonly prescribed medication in the management of osteoporosis.1 Placebo controlled randomised trials of bisphosphonate therapy (BT) have demonstrated evidence of this medication in preventing bone loss and osteoporotic fractures.2–5
The mechanism of action of bisphosphonates involves inhibition of osteoclast activity and reduction in the size of resorption cavities that form, with a resulting increase in bone mineral density.6 However, there have been concerns that BT may lead to oversuppression of bone turnover and impairment of bone healing; bone histomorphometric analysis in patients receiving long-term alendronate therapy showed changes consistent with severely suppressed bone turnover similar to adynamic bone disorder.7 There have been case reports of atypical femoral fractures associated with BT.8,9
A systematic review was conducted on all existing literature that described delayed or non-union of lower limb, long bone fractures among human adults on BT. The aim of this review was to investigate whether BT increases the risk of delayed or non-union in lower limb, long bone fractures.
Methods
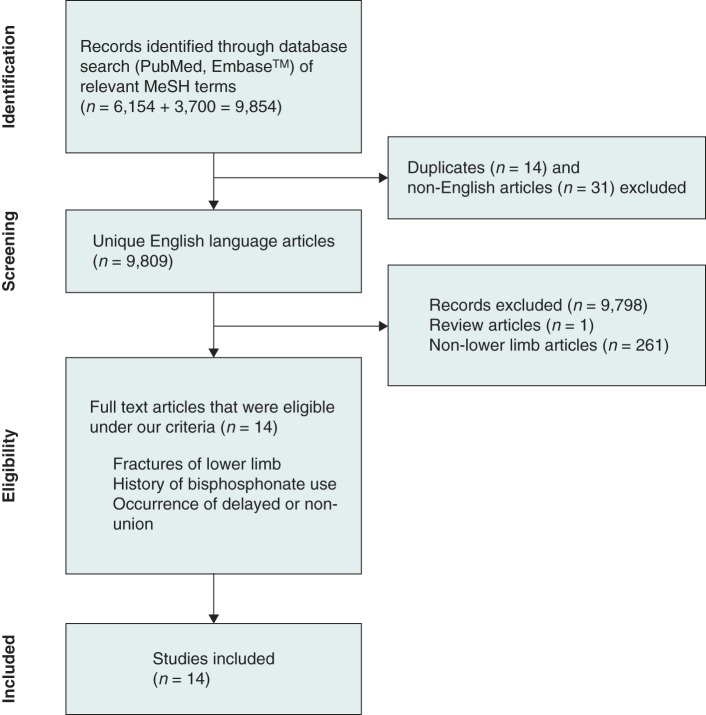
Our screening and bias assessment strategy, illustrated in Figure 1, was based on the PRSIMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) standards and checklist. A literature search was performed in PubMed (1950 – present) and Embase™ (1947 – present) on 4 November 2014 with the following search criteria: “fractures, bone OR fracture healing OR osteoporotic fractures AND diphosphonates OR alendronate OR pamidronate” for PubMed and “fracture OR non-union OR delayed union OR bone healing OR bone union AND bisphosphonate OR bisphosphonate acid derivative” for Embase™. Search terminology was based on the MeSH (Medical Subject Headings) database provided. Our search was limited to studies carried out in humans and reported in the English language. Print journals, online journals and meeting or conference abstracts were considered for inclusion. Review articles were excluded. This initial search strategy identified 9,809 articles of interest.
Figure 1.
Study flow diagram
The included articles were assessed for quantitative estimates of our key parameters of interest, namely time to fracture union and rate of delayed or non-union per fracture, specifically comparing between BT and non-BT cases. Outcomes following operative versus non-operative management of fractures were also assessed. Articles that described patients with fractures of the lower limb and a history of bisphosphonate use were included. Case reports were excluded. The following information was identified: author, study design, sample size, sex distribution, age, duration of BT, type of BT, fracture site, type of fractures described (assessed specifically using American Society for Bone and Mineral Research [ASBMR] definition of atypical femoral fractures),10,11 definitions of union, time to union, type of fracture management and other factors that may modify healing outcomes.
Results
Fourteen papers were included in this review.7,12–24 A summary of the design characteristics of each paper is provided in Table 1. A detailed meta-analysis of the articles was not possible owing to heterogeneity with regard to parameters of interest and types of populations sampled. Rough cumulative estimates, weighted by sample sizes, were calculated for all key parameters of interest.
Table 1.
Characteristics of papers reviewed
| Study | Study design | Number of patients (fractures) | Sex | Mean age of patients in years (range) | Median duration of BT in years (range) | Timing of follow-up in months (range) | Type of bisphosphonate | Fracture site |
|---|---|---|---|---|---|---|---|---|
| BT = bisphosphonate therapy; NA = not available; SD = standard deviation | ||||||||
| Armamento-Villareal, 20097 | Retrospective review | 8 (NA) | 7 female 1 male |
55.6 (43–75) | 5.6 (2–10) | NA (NA) | 7 alendronate, 1 risedronate | Femoral shaft, fibula |
| Odvina, 201012 | Retrospective review | 13 (16) | 13 female | 64.2 (38–77) | 7.1 (2–11) | NA (NA) | 10 alendronate, 3 risedronate | Subtrochanteric, femoral shaft, tibia |
| Das De, 201013 | Cohort study | 20 (26); case 12 (18); control 8 (8) | 19 female 1 male |
62 (51–75) case, 64.8 (44–88) control | 4.5 (3–8) | NA (NA) | 20 alendronate | Subtrochanteric, femoral shaft |
| Ha, 201014 | Retrospective review | 11 (14) | 11 female | 68 (57–82) | 4.5 (3–10) | Mean 27 (12–60) | 9 alendronate, 2 pamidronate | Subtrochanteric, femoral shaft |
| Banffy, 201115 | Retrospective review | 34 (40) | 34 female | 68.5 (53–87) | 6.4 (3–10) | Mean 36.5 (12–72) | 29 alendronate, 3 zoledronate, 2 pamidronate | Subtrochanteric, femoral shaft |
| Weil, 201116 | Retrospective review | 15 (17) | 14 female 1 male |
73 (51–85) | 7.8 (4–13) | 1.5, 3, 6, 12 (NA) | Alendronate (most frequent), etidronate, pamidronate, risedronate, zoledronate; proportions NA | Subtrochanteric, femoral shaft |
| Prasarn, 201217 | Cohort study | 45 (45); case 25 (25); control 20 (20) | 45 female | 72.3 (SD: 11) | 7.6 (1–12) | Mean 29 (5–60) | NA | Femoral |
| Schneider, 201218 | Retrospective review | 81 (NA) | 78 female 3 male |
64.9 (43.5–89) | 9.5 (1.5–15) | NA (NA) | 76 alendronate, 4 risedronate, 1 zoledronate | Femoral shaft |
| Thompson, 201219 | Cohort study | 27 (29); case 22 (24), control 5 (5) | 23 female 4 male |
75.6 (52–91) | 4.6 (0.04–12.1) | NA (NA) | 17 alendronate, 10 other (NA) | Subtrochanteric, femoral shaft |
| Ward, 201220 | Retrospective review | 16 (24) | 15 female 1 male |
69.1 (51–90) | 6.3 (3–10) | Median 31 (9–112) | 10 alendronate, 4 zoledronate, 3 risedronate, 1 ibandronate, 1 pamidronate; proportions NA | Subtrochanteric, femoral shaft |
| Sasaki, 201221 | Retrospective review | 8 (11) | 8 female | 77.1 (71–86) | 3.8 (1–6) | 3 (NA) | 6 alendronate, 2 risedronate | Femoral shaft |
| Egol, 201322 | Retrospective review | 33 (41) | 31 female 2 male |
64.7 (46–83) | 8.8 (5–20) | 1, 3, 6, 12 (NA) | NA | Subtrochanteric, femoral shaft |
| Kang, 201423 | Retrospective review | 76 (99) | 73 female 3 male |
71.4 (43–89) | 3.1 (0.1–17) | Mean 24.5 (12–79) | 41 alendronate, 18 risedronate, 10 ibandronate, 1 pamidronate, 1 zoledronate, 5 mixed | Subtrochanteric, femoral shaft |
| Teo, 201424 | Retrospective review | 33 (33) | 33 female | 67.5 (47–91) | 4.9 (2–10) | Mean 21.7 (0–53) | NA, includes alendronate | Subtrochanteric |
Fractures investigated were described primarily as atypical femoral fractures associated with BT, with two exceptions: Armamento-Villareal et al included a patient with a fibular fracture7 and Odvina et al included a case of a tibial fracture that experienced delayed union.12 The included studies investigated a total of 420 patients: 387 patients on BT and 33 controls (401 female and 16 male). The cumulative mean age of the patients was 68.5 years (±5.6 years, range: 38–91 years).
The mean duration of BT in all the studies was 6.3 years (±1.9 years, range: 0.04–20 years). Alendronate was the most common type of BT prescribed but use of other BT (risedronate, zoledronate, etidronate, pamidronate and ibandronate) was also included.
Three studies employed non-BT controls. A retrospective review conducted by Das De et al examined 20 patients with subtrochanteric femur fractures, of whom 12 were receiving long-term alendronate, and 8 served as a control group.13 Prasarn et al conducted a retrospective review of patients who had sustained femoral shaft fractures, who had been on BT for at least one year; a control population was created retrospectively with similar preoperative parameters as the BT cohort.17 Finally, a retrospective review by Thompson et al looked at 27 insufficiency fractures of the subtrochanteric femoral shaft, from which patients on BT were identified retrospectively.19 Two studies performed comparisons that showed no significant differences between BT and control groups with regard to preoperative and patient characteristics.13,17
Important findings for each reviewed paper, pertaining to the questions posed in this review, are shown in Table 2.
Does BT increase the risk of delayed or non-union in lower limb, long bone fractures?
Our literature review demonstrates that BT is associated with poor healing of lower limb, long bone fractures. Four studies measured time to union in patients on BT.17,19,23,24 The mean time to union for BT users was 8.5 months across all four studies. In particular, Prasarn et al reported that the BT group had a longer time to union than the control group (6.5 vs 4.8 months).17 The mean rate of delayed or non-union for BT associated atypical fractures was 20% per fracture, with a range of 2–63%.7,12–16,18–22 Notably, there were comparisons between BT and non-BT groups with regard to rate of delayed or non-union; Das De et al stated that, compared with controls, the BT group had a higher proportion of patients experiencing non-union that necessitated further surgery (25% vs 13%).13
Kang et al investigated the correlation between duration of BT and delayed union, demonstrating that delayed union was more common in the cohort with more than three years of BT (67%) than in the group with less than three years of BT (26%).23 Furthermore, Schneider et al found that 43% of patients who continued BT after the first fracture went on to develop a second fracture more than 12 months later, compared with 17% of those who stopped BT after the first fracture.18
Does operative management improve the outcomes of these fractures?
Compared with non-operative management, intramedullary nailing of atypical BT related fractures was associated with a lower risk of non-union than for non-operative management.14,15,20 Banffy et al reported that 5 of 6 fractures (83%) managed initially non-operatively resulted in non-union (completion and displacement of fracture) by 18 months.15 In addition, Teo et al described a high rate of implant failure (7/30, 23%) in the BT group.24 In contrast, 0 of 6 fractures managed initially with prophylactic nailing in the study by Banffy et al resulted in non-union at 12 months (ie all fractures demonstrated radiological union) and overall, only 1 of 34 fractures (2%) that were managed operatively (whether initially or after failure of conservative management) experienced delayed union.15
Ha et al found that 4 of 4 patients who refused operative management continued to have radiological non-union during their follow-up period.14 By comparison, 0 of 10 patients whose fractures were managed operatively had continued non-union; instead, all of these cases had achieved bony union by the end of their follow-up period. Both operative and non-operative groups had similar follow-up periods except for a single outlier in the operative group (60 months).
Discussion
Risk of poor healing in lower limb, long bone fractures
There is evidence supporting prolonged bone healing in patients with atypical fractures after BT (Australian National Health and Medical Research Council level of evidence III-2 and III-3). Our systematic review identified clinically significant rates of delayed or non-union associated with BT. Two studies specifically measured time to union in patients on BT; the mean time to union in the BT group was quoted as 6–6.5 months.17,19 This falls into the time range for delayed union.14,21 Furthermore, Prasarn et al suggested that BT was associated with longer healing times (1.7 months) compared with non-BT.17 Overall in our review, approximately a third of all BT related fractures resulted in delayed or non-union.
A number of case reports and case series in the literature suggest a similar trend to that seen in our review. Sayed-Noor and Sjödén reported two patients with femoral insufficiency fractures after long-term alendronate therapy and one of these had delayed union after internal fixation.8 Visekruna et al reported three patients with subtrochanteric insufficiency fractures, one of whom had no radiographic evidence of union at 22 months.25
In particular, Kang et al identified that a high rate (56.5%) of patients on long-term BT who developed delayed union.23 In addition, there was a significantly higher incidence of delayed union in the group with long-term therapy.
From a pathological perspective, the prolonged times to fracture union and the greater rates of failed union observed in our review are consistent with existing claims of aberrant bone growth with BT.7,12 Armamento-Villareal et al conducted histomorphometric analyses in 14 bisphosphonate users and reported that the number of trabecular osteoclasts was reduced in all patients regardless of the bone turnover rate.7 They hypothesised that decreased osteoclast function translates to dampening of remodelling. Allen and Burr also noted that initiation of osteoclast activity is suppressed by BT, which reduces the number of active bone remodelling sites and the size of resorption cavities that form.6
Odvina et al performed transiliac bone biopsy with double tetracycline labelling in six bisphosphonate users and identified low bone turnover in all six; five of these were severely suppressed.12 They suggested that low bone turnover could impair the bone’s ability to repair strain related microdamage, leading to accumulation of microcracks.
Operative management of atypical fractures
There is a consensus among three publications in this review that operative management of atypical fractures offers superior outcomes compared with conservative non-operative management. Specifically, internal fixation has a higher likelihood of achieving bone union than non-operative management.14,15 Other clinical outcomes such as length of hospital stay and pain relief are also improved with operative management. Furthermore, prophylactic operative management in the contralateral femur (or in any femur that demonstrates a stress pattern on radiography) is associated with lower risk of subsequent fracture and healing complications.15,20
Interestingly, Prasarn et al identified that BT was associated with a higher complication rate from operative management (71% vs 10%) despite the use of additional medical and surgical adjuvants.17 Moreover, there is an increased rate of bilateral and secondary contralateral fractures.13,18 It is postulated that the higher incidence of bilateral fractures in BT groups may be secondary to generalised aberrant bone growth with BT.13
Other factors involved in operative management including bone grafting, revision plate fixation and renailing have been described in very few cases in papers reviewed in this study but there has been no long-term follow-up of these rare cases. In one article, these were excluded from statistical analysis.22
In the wider literature, there has been medical and non-operative management of BT related lower limb fractures. Of note, patients who sustained bisphosphonate related lower limb fractures that were managed non-operatively had a higher incidence of teriparatide use (64% vs 5%).20 Moreover, recent evidence suggests that teriparatide use accelerates healing in the postoperative setting in BP related atypical femoral fractures.26 Despite this, there has been no identified benefit of teriparatide use on rates of healing found in papers included in this review.20
Limitations
Assessing for delayed and non-union was complicated by variability in existing definitions of fracture union. For example, Ha et al and Weil et al defined delayed union as longer than twice the expected healing time for specific regions of bones (ie longer than 12 weeks for fractures in the upper limb and feet, and 6 months in the femur or tibia).14,16 Failure of union was defined by Thompson et al as 1.5 times the expected duration for fracture union.19
The most accepted criteria for atypical subtrochanteric and diaphyseal femoral fractures were described in ASBMR report.10,11 However, these criteria were used in only three papers reviewed in this study to define atypical femoral fractures.18,23,24
Patients on BT may have existing risk factors that predispose to delayed bone healing, such as age, steroid use and osteoporosis. This potential source of bias was addressed by three of the reviewed studies, which identified no significant difference between BT and control groups in terms of existing risk factors.13,17,23
While BT is often used in patients with both typical and atypical fractures,27 most studies in the literature described atypical fractures. Our analysis may therefore not necessarily reflect bone healing in bisphosphonate users who sustain typical traumatic fractures.
Notably, the role of operative management in bisphosphonate users discussed in this review is an incidental finding of the initial literature review. Consequently, papers included in the current study may not be a comprehensive review of current evidence of operative management of fractures in bisphosphonate users.
For these reasons, it is suggested that further investigations to evaluate the exact effects of BT on lower limb fractures are carried out.
Conclusions
Overall, BT appears to be associated with poor healing of atypical fractures, including longer duration to complete union and higher incidence of non-union. Operative management of atypical fractures and prophylactic treatment of incomplete stress fractures may help ameliorate some of these risks. Further high level studies are required to clarify the fracture risks associated with BT, in particular typical femoral fractures.
References
- 1.Stafford RS, Drieling RL, Hersh AL. National trends in osteoporosis visits and osteoporosis treatment, 1988–2003. Arch Intern Med 2004; : 1,525–1,530. [DOI] [PubMed] [Google Scholar]
- 2.Harris ST, Watts NB, Genant HK et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. JAMA 1999; : 1,344–1,352. [DOI] [PubMed] [Google Scholar]
- 3.Black DM, Thompson DE, Bauer DC et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. J Clin Endocrinol Metab 2000; : 1,118–4,124. [DOI] [PubMed] [Google Scholar]
- 4.Reginster J, Minne HW, Sorensen OH et al. Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Osteoporos Int 2000; : 83–91. [DOI] [PubMed] [Google Scholar]
- 5.Tonino RP, Meunier PJ, Emkey R et al. Skeletal benefits of alendronate: 7-year treatment of postmenopausal osteoporotic women. J Clin Endocrinol Metab 2000; : 1,109–3,115. [DOI] [PubMed] [Google Scholar]
- 6.Allen MR, Burr DB. Bisphosphonate effects on bone turnover, microdamage, and mechanical properties: what we think we know and what we know that we don’t know. Bone 2011; : 56–65. [DOI] [PubMed] [Google Scholar]
- 7.Armamento-Villareal R, Napoli N, Diemer K et al. Bone turnover in bone biopsies of patients with low-energy cortical fractures receiving bisphosphonates: a case series. Calcif Tissue Int 2009; : 37–44. [DOI] [PubMed] [Google Scholar]
- 8.Sayed-Noor AS, Sjödén GO. Two femoral insufficiency fractures after long-term alendronate therapy. Clin Orthop Relat Res 2009; : 1,921–1,926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Napoli N, Novack D, Armamento-Villareal R. Bisphosphonate-associated femoral fracture: implications for management in patients with malignancies. Osteoporos Int 2010; : 705–708. [DOI] [PubMed] [Google Scholar]
- 10.Shane E, Burr D, Ebeling PR et al. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2010; : 1,267–2,294. [DOI] [PubMed] [Google Scholar]
- 11.Shane E, Burr D, Abrahamsen B et al. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014; : 1–23. [DOI] [PubMed] [Google Scholar]
- 12.Odvina CV, Levy S, Rao S et al. Unusual mid-shaft fractures during long-term bisphosphonate therapy. Clin Endocrinol 2010; : 161–168. [DOI] [PubMed] [Google Scholar]
- 13.Das De S, Setiobudi T, Shen L, Das De S. A rational approach to management of alendronate-related subtrochanteric fractures. J Bone Joint Surg Br 2010; : 679–686. [DOI] [PubMed] [Google Scholar]
- 14.Ha YC, Cho MR, Park KH et al. Is surgery necessary for femoral insufficiency fractures after long-term bisphosphonate therapy? Clin Orthop Relat Res 2010; : 1,393–3,398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Banffy MB, Vrahas MS, Ready JE, Abraham JA. Nonoperative versus prophylactic treatment of bisphosphonate-associated femoral stress fractures. Clin Orthop Relat Res 2011; : 1,028–2,034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Weil YA, Rivkin G, Safran O et al. The outcome of surgically treated femur fractures associated with long-term bisphosphonate use. J Trauma 2011; : 186–190. [DOI] [PubMed] [Google Scholar]
- 17.Prasarn ML, Ahn J, Helfet DL et al. Bisphosphonate-associated femur fractures have high complication rates with operative fixation. Clin Orthop Relat Res 2012; : 1,295–2,301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schneider JP, Hinshaw WB, Su C, Solow P. Atypical femur fractures: 81 individual personal histories. J Clin Endocrinol Metab 2012; : 1,324–4,328. [DOI] [PubMed] [Google Scholar]
- 19.Thompson RN, Phillips JR, McCauley SH et al. Atypical femoral fractures and bisphosphonate treatment: experience in two large United Kingdom teaching hospitals. J Bone Joint Surg Br 2012; : 385–390. [DOI] [PubMed] [Google Scholar]
- 20.Ward WG, Carter CJ, Wilson SC, Emory CL. Femoral stress fractures associated with long-term bisphosphonate treatment. Clin Orthop Relat Res 2012; : 759–765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sasaki S, Miyakoshi N, Hongo M et al. Low-energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J Bone Miner Metab 2012; : 561–567. [DOI] [PubMed] [Google Scholar]
- 22.Egol KA, Park JH, Rosenberg ZS et al. Healing delayed but generally reliable after bisphosphonate-associated complete femur fractures treated with IM nails. Clin Orthop Relat Res 2014; : 1,728–2,734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kang JS, Won YY, Kim JO et al. Atypical femoral fractures after anti-osteoporotic medication: a Korean multicenter study. Int Orthop 2014; : 1,247–1,253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teo BJ, Koh JS, Goh SK et al. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. Bone Joint J 2014; : 658–664. [DOI] [PubMed] [Google Scholar]
- 25.Visekruna M, Wilson D, McKiernan FE. Severely suppressed bone turnover and atypical skeletal fragility. J Clin Endocrinol Metab 2008; : 1,948–2,952. [DOI] [PubMed] [Google Scholar]
- 26.Miyakoshi N, Aizawa T, Sasaki S et al. Healing of bisphosphonate-associated atypical femoral fractures in patients with osteoporosis: a comparison between treatment with and without teriparatide. J Bone Miner Metab 2014. September 17 [Epub ahead of print.] [DOI] [PubMed]
- 27.Agarwal S, Agarwal S, Gupta P et al. Risk of atypical femoral fracture with long-term use of alendronate (bisphosphonates): a systemic review of literature. Acta Orthop Belg 2010; : 567–571. [PubMed] [Google Scholar]