Abstract
Introduction
Afferent loop syndrome (ALS) is a recognised complication of foregut surgery caused by mechanical obstruction at the gastrojejunostomy anastomosis itself or at a point nearby. Acute ALS has only been reported following pancreaticoduodenectomy (PD) after several years due to recurrence of malignancy at the anastomotic site. We report five cases of acute ALS in the first postoperative week.
Methods
The presentation, clinical findings and successful management of the 5 patients with ALS were obtained from a prospectively collected database of 300 PDs. All five patients with early acute ALS presented with signs and symptoms of a bile leak. Since the fifth patient, the surgical technique has been modified with the creation of a larger window in the transverse mesocolon and a Braun enteroenterostomy.
Results
There have been no further incidents of ALS since the adoption of these modifications to the standard technique of PD and there has also been a reduction in postoperative bile leaks (6.4% vs 3.6%, p=0.416).
Conclusions
Acute ALS is a rare but important complication in the immediate postoperative period following PD and causes disruption to adjacent anastomoses, resulting in a bile leak. A prophylactic Braun anastomosis and wide mesocolic window may prevent this complication and subsequent deterioration.
Keywords: Pancreaticoduodenectomy, Afferent loop syndrome, Braun anastomosis, Pancreaticojejunostomy, Roux-en-Y anastomosis, Postoperative complications
Afferent loop syndrome (ALS) is caused by distension and accumulation of digestive juices in the afferent limb of the jejunum following creation of a gastrojejunostomy. It results from mechanical obstruction at the anastomosis itself or at a point near the anastomosis. The presentation of ALS may be acute if there is complete obstruction and chronic when there is partial obstruction. In the acute presentation, there is continuous upper abdominal pain, nausea and vomiting due to build up of secretions in the completely obstructed length of small bowel. Patients with chronic ALS classically experience recurrent episodes of postprandial fullness and transient epigastric pain that is relieved by bilious vomiting as a partially obstructed afferent limb empties into the stomach.1–3
The Braun anastomosis has been used effectively to treat ALS following gastrectomy.4–6 This consists of an enteroenterostomy between the afferent and efferent limbs of a gastroenterostomy, and allows digestive juices in the afferent limb to flow into the efferent limb, thereby bypassing any obstruction at the gastrojejunostomy (Figs 1 and 2).
Figure 1.
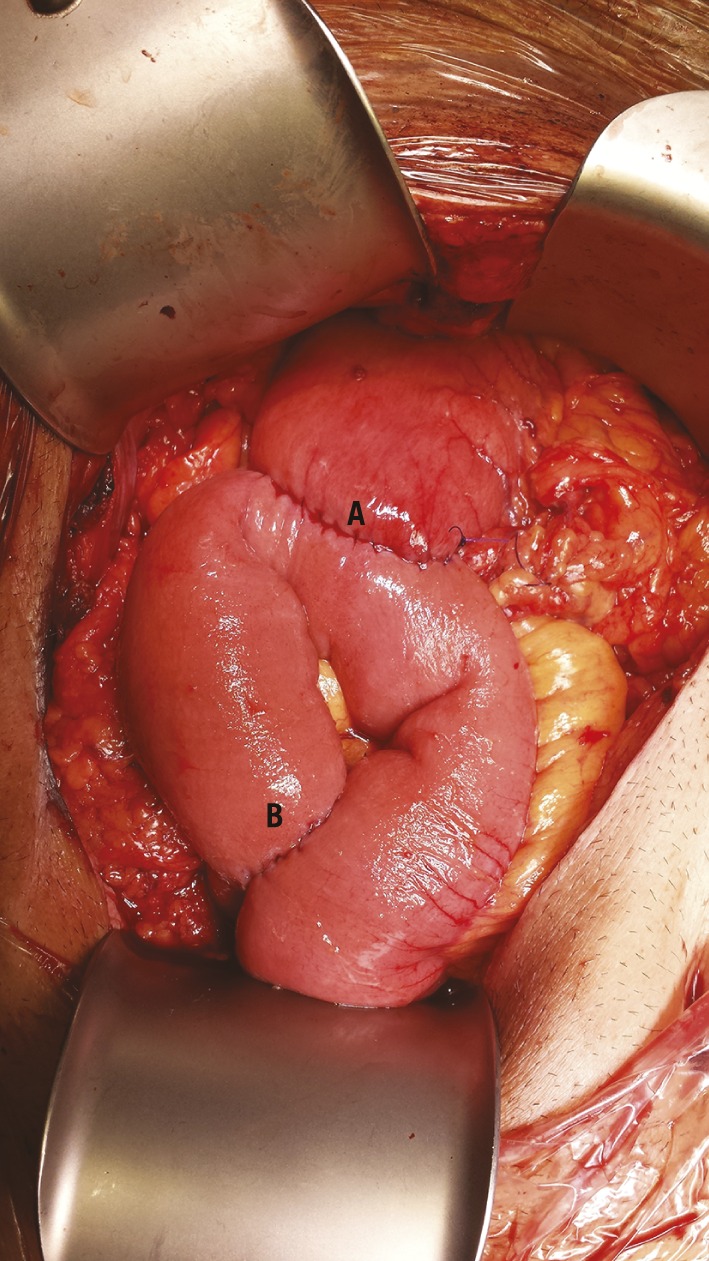
A Braun loop anastomosis created prophylactically during a pylorus preserving pancreaticoduodenectomy: pylorojejunostomy anstomosis (A) and jejunojejunostomy (Braun) anastomosis (B)
Figure 2.
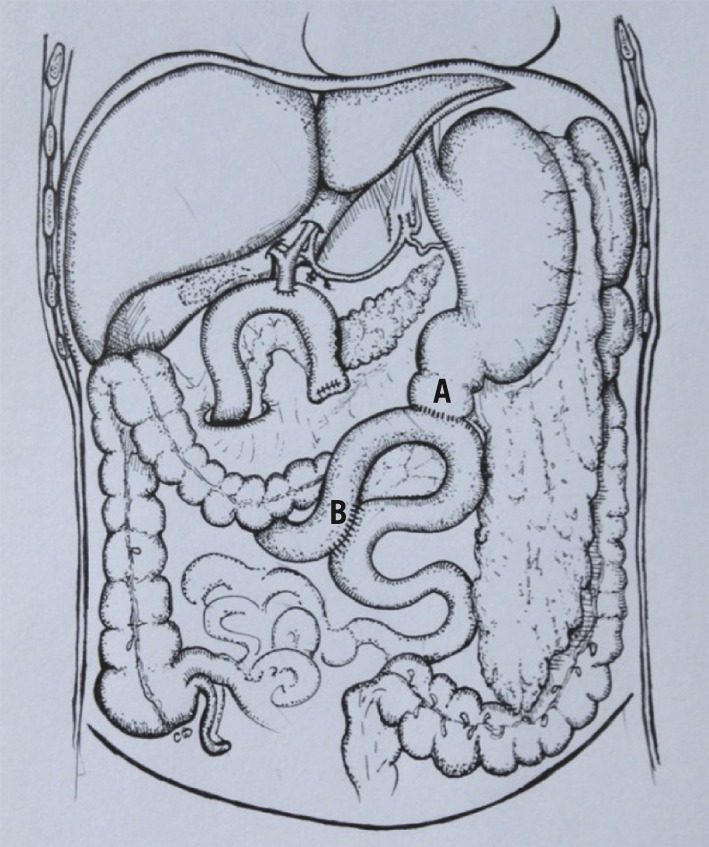
Diagram of the Braun loop anastomosis during pylorus preserving pancreaticoduodenectomy: pylorojejunostomy anstomosis (A) and jejunojejunostomy (Braun) anastomosis (B)
While ALS is most commonly recognised following distal gastrectomy with Billroth II reconstruction, it has also been reported after other procedures of the foregut including pancreaticoduodenectomy (PD). Most cases of ALS after PD, however, present with chronic symptoms7–10 and although reports of acute ALS exist, these have occurred several years after the initial operation due to recurrence of malignancy at the anastomotic site.7,8 To our knowledge, there are no reports of early acute ALS in the immediate postoperative period following PD.
We present five patients who were found to have acute ALS in the first postoperative week. Four of the five original resections were performed at the Royal Surrey County Hospital (RSCH) and the other in the private sector. Three different hepatopancreatobiliary (HPB) surgeons performed the original cases. Since the fifth case, HPB surgeons at RSCH have modified their surgical technique to include a wider mesocolic window at the transverse mesocolon and creation of a Braun enteroenterostomy. In this paper, we discuss the impact of these prophylactic measures in patients undergoing PD.
Methods
Clinical information on the five reported patients was collected from hospital records. A database of 300 PD cases was analysed to compare the demographics, intraoperative findings and postoperative outcomes before and after the introduction of a prophylactic Braun anastomosis and wide mesocolic window as part of the operative technique.
Statistical comparisons were carried out using SPSS® version 21 (IBM, New York, US). Continuous variables were analysed using the Student’s t-test and categorical data with Fisher’s exact test. A p-value of <0.05 was considered statistically significant.
Results
Patient 1
A 32-year-old man underwent an uneventful pylorus preserving pancreaticoduodenectomy (PPPD) for a mucinous cyst in the head of the pancreas. On day 3, raised inflammatory markers were noted and despite computed tomography (CT) reported as showing only postsurgical changes and the patient being started on antibiotics for a lower respiratory tract infection, they continued to increase. On day 6, the patient underwent repeat CT, which showed a larger volume of fluid in the right upper quadrant, suspicious for an anastomotic leak (Fig 3).
Figure 3.

Computed tomography showing collection of fluid (arrow) arising from the hepaticojejunostomy anastomosis
At laparotomy, a bile leak was identified at the hepaticojejunostomy. The cause was obstruction at the pylorojejunostomy secondary to kinking of the afferent limb of the small bowel. The pylorojejunostomy was refashioned with relief of afferent limb obstruction. The patient made a slow recovery and was discharged 18 days later.
Patient 2
A 76-year-old man with a neuroendocrine tumour of the duodenum and uncinate process underwent a PPPD. The following morning, 500ml of bile was noted in the abdominal drain. He was taken back to theatre and a leak was found at the hepaticojejunostomy with distension of the afferent loop due to constriction at the transverse mesocolon window. A single suture was placed to reinforce the hepaticojejunostomy, the constriction at the mesocolon relieved and a side-to-side jejunojejunostomy (Braun anastomosis) created. The patient made an uneventful recovery and was discharged on day 16.
Patient 3
A 63-year-old woman underwent a PPPD for an adenoma on the medial wall of the second part of the duodenum. The following day, she complained of increasing abdominal pain and bile was noted in her abdominal drain, totaling 135ml on day 1 and 600ml on day 2. She was taken back to theatre where the afferent loop was found to be distended owing to kinking at the pylorojejunostomy and causing anastamotic disruption at the pancreaticojejunostomy. A single suture was placed over the leak at the pancreaticojejunostomy and a side-to-side jejunojejunostomy (Braun anastomosis) created. The patient made a full recovery and was discharged on day 15.
Patient 4
A 78-year-old man underwent a PD for a tumour involving the first part of the duodenum. On day 7, his abdomen became distended and tympanic with absent bowel sounds. At laparotomy, afferent limb distension was noted with constriction at the transverse mesocolon and bile leak at the pancreaticojejunostomy. The opening in the transverse mesocolon was widened and the pancreaticojejunostomy refashioned. The patient recovered uneventfully and was discharged 18 days later.
Patient 5
A 73-year-old woman underwent a PPPD procedure for a neuroendocrine tumour of the head of the pancreas. On day 2, there was 300ml of bile in the abdominal drains and she was returned to theatre. A leak was found at the pancreaticojejunostomy secondary to constriction at the transverse mesocolon window. The constriction was relieved and a single suture placed at the site of the leak. Two days later, a small volume of bile was again noted in the drains but this was managed conservatively. She recovered slowly and was discharged 23 days after the initial operation.
The findings from these five patients are summarised in Table 1.
Table 1.
Patient characteristics and operative findings for the five patients found to have early acute afferent loop syndrome following pancreaticoduodenectomy
| Patient | Age | Diagnosis | Comorbidities | Site of bile leak | Cause of obstruction | Hospital stay |
|---|---|---|---|---|---|---|
| HJ = hepaticojejunostomy; PyJ = pylorojejunostomy; GORD = gastro-oesophageal reflux disease; PJ = pancreaticojejunostomy; NIDDM = non-insulin dependent diabetes mellitus | ||||||
| 1 | 32 | Benign mucinous cyst | Nil | HJ anastomosis | Kinking at PyJ anastomosis | 18 days |
| 2 | 76 | Neuroendocrine tumour of pancreatic origin | Nil | HJ anastomosis | Constriction at mesocolon | 16 days |
| 3 | 63 | Adenoma at D2 with high grade dysplasis | Asthma, GORD, smoker | PJ anastomosis | Kinking at PyJ anastomosis | 15 days |
| 4 | 78 | Pancreatic head tumour | Hypertension, NIDDM | PJ anastomosis | Constriction at mesocolon | 25 days |
| 5 | 73 | Neuroendocrine tumour of pancreatic origin | Nil | PJ anastomosis | Constriction at mesocolon | 23 days |
Series analysis
Since the last patient with ALS, this complication has been avoided by modifying our standard surgical technique for PD with the creation of a larger mesocolic window in the transverse mesocolon and a prophylactic Braun enteroenterostomy. The last 300 consecutive PD cases were analysed and the patients divided into those prior to the introduction of the prophylactic measures (n=217) and those since (n=83). The incidence of ALS in the earlier cohort was 2.3% compared with none in the latter (p=0.327). We also found a reduction in the number of patients returning to theatre (11.5% vs 3.6%, p=0.044) and in the rate of bile leak (6.4% vs 3.6%, p=0.416) (Table 2).
Table 2.
Comparison of patient demographics, intraoperative data and postoperative outcomes in patients who underwent pancreaticoduodenectomy prior to and after the introduction of a prophylactic Braun anastomosis and wide mesocolic window
| PD without prophylactic measures (n=217) | PD with prophylactic measures (n=83) | p-value | |
|---|---|---|---|
| PD = pancreaticoduodenectomy; PPPD = pylorus preserving pancreaticoduodenectomy; EBL = estimated blood loss; ALS = afferent loop syndrome | |||
| Demographics | |||
| Median age (range) | 70 yrs (23–97 yrs) | 67 yrs (31–82 yrs) | 0.269 |
| Male | 122 (56%) | 47 (57%) | 1.000 |
| Diabetic | 26 (12%) | 14 (17%) | 0.261 |
| Current/former smoker | 96 (44%) | 42 (51%) | 0.365 |
| Intraoperative data | |||
| PPPD | 121 (56%) | 66 (80%) | 0.0002 |
| Median duration (range) | 330 mins (150–660 mins) | 350 mins (180–620 mins) | 0.453 |
| Median EBL (range) | 600ml (40–4,200ml) | 600ml (100–2,600ml) | 0.577 |
| Postoperative outcomes | |||
| ALS | 5 (2.3%) | 0 (0%) | 0.327 |
| Bile leak | 14 (6.4%) | 3 (3.6%) | 0.416 |
| Return to theatre | 25 (11.5%) | 3 (3.6%) | 0.044 |
| Morbidity | 79 (36.4%) | 24 (28.9%) | 0.277 |
| 30-day mortality | 6 (2.8%) | 0 (0%) | 0.192 |
Discussion
We have identified five patients with acute ALS occurring in the first postoperative week following PD. All five cases occurred prior to modification of the surgical technique with the creation of a wider mesocolic window in the transverse mesocolon and the addition of a Braun anastomosis. The incidence of early acute ALS prior to these prophylactic measures was 2.3% (5/217) and there has not been a recognised case since (0/83). There has also been a reduction in the incidence of confirmed bile leaks and in the number of patients returning to theatre but these changes in outcome cannot be attributed purely to these measures as other elements of surgical technique, medical practice and overall patient care has changed significantly over the years.
In two patients, obstruction to the afferent limb was caused by stricturing or kinking at the pylorojejunostomy itself and in the other three cases, ALS was caused by constriction at the transverse mesocolic window. In previous reports of ALS occurring after gastrectomies, obstruction has been reported due to adhesions, internal hernias, intussusception, volvulus, gallstones and enteroliths.10–14 Following resections for malignancy, obstruction from recurrence at the anastomosis has also been described.7,8
Acute ALS occurring in the first week postoperatively has been reported following gastrectomy although presentation after 30–40 years following surgery has also been described.15 Our patients presented with features similar to those of a bile leak with bile in the abdominal drain (in 3 patients), leucocytosis (in 4), change in abdominal examination findings (in 3) and fever.16 In the two patients who did not have bile in their drains, at the time of deterioration, a drain was either not inserted intraoperatively (Patient 1) or was removed early following an initial good recovery (Patient 4). An analysis of postoperative liver function tests did not reveal any consistent derangement in these patients. Alanine transferase was the most commonly increased, in four of the five patients.
Despite two patients having had CT, distension of the afferent limb was not reported initially on these images although on retrospective examination, this finding was present. This illustrates the difficulty in distinguishing between abnormal findings and expected early postoperative changes following complex anatomical rearrangement as occurs during PD and the high index of suspicion required to detect ALS.
These patients underwent operative management as they had evidence of a significant bile leak or deterioration requiring active intervention. Two patients with obstruction caused by constriction at the mesocolon only required widening of the constriction and placement of a reinforcing suture at the site of the bile leak. One patient required refashioning of the pancreaticojejunostomy. With the other two patients, whose obstruction was caused by kinking at the pylorojejunostomy, one required refashioning of that anastomosis but the other did not. The overriding principles for definitive management were the same in all patients: correct any anastomotic disruption and resolve the cause of mechanical obstruction. In two of the patients described, a Braun anastomosis was carried out in case of recurrent obstruction.
The Braun enteroenterostomy was first described in 1892 by Heinrich Braun as a way to prevent bilious vomiting after the creation of a gastrojejunostomy. It has since been used successfully to treat both acute and chronic forms of ALS.4–6,10 He initially described a side-to-side jejunojejunostomy although the eponym has been applied to subsequent modifications, including end-to-side and double side-to-side anastomoses.5,6 Following PDs, the extra anastomosis ensures that an obstructed afferent limb can decompress into the efferent limb, preventing a rise in intraluminal pressure, distension and mechanical disruption to other anastomoses.
Conclusions
Acute ALS is a rare but important complication in the early postoperative period following PD. It presents with associated features of a bile leak due to disruption of anastomoses from raised intraluminal pressure. Early operative management with relief of the obstruction and correction of anastomotic disruption is an effective treatment strategy. In our opinion, creation of a wide window in the transverse mesocolon and a prophylactic Braun anastomosis may prevent this complication and reduce the incidence of bile leak following PD. Furthermore, the results of this study highlight the need to pay sufficient attention to minor technical details in order to prevent complications and obtain the best outcomes for our patients.
Acknowledgement
The authors would like to thank Cara Baker (Consultant Surgeon at Frimley Health NHS Foundation Trust) for the artwork in Figure 2.
References
- 1.Herrington JL. Experiences with the surgical management of the afferent loop syndrome. Ann Surg 1966; : 797–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woodfield CA, Levine MS. The postoperative stomach. Eur J Radiol 2005; : 341–352. [DOI] [PubMed] [Google Scholar]
- 3.Pannala R, Brandabur JJ, Gan SI et al. Afferent limb syndrome and delayed GI problems after pancreaticoduodenectomy for pancreatic cancer: single-center, 14-year experience. Gastrointest Endosc 2011; : 295–302. [DOI] [PubMed] [Google Scholar]
- 4.Braun H. Über Gastro-enterostomie und gleichzeitig ausgeführte Entero-anastomose. Arch Klin Chir 1893; : 361. [Google Scholar]
- 5.Fischer JE. Master of Surgery. Volume 1. Philadelphia: Lippincott Williams & Wilkins; 2006. pp856–857. [Google Scholar]
- 6.Kim DJ, Lee JH, Kim W. Afferent loop obstruction following laparoscopic distal gastrectomy with Billroth-II gastrojejunostomy. J Korean Surg Soc 2013; : 281–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Burdick JS, Garza AA, Magee DJ et al. Endoscopic management of afferent loop syndrome of malignant etiology. Gastrointest Endosc 2002; : 602–605. [DOI] [PubMed] [Google Scholar]
- 8.Aimoto T, Uchida E, Nakamura Y et al. Malignant afferent loop obstruction following pancreaticoduodenectomy: report of two cases. J Nippon Med Sch 2006; : 226–230. [DOI] [PubMed] [Google Scholar]
- 9.Spiliotis J, Karnabatidis D, Vaxevanidou A et al. Acute cholangitis due to afferent loop syndrome after a Whipple procedure: a case report. Cases J 2009; : 6,339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim JK, Park CH, Huh JH et al. Endoscopic management of afferent loop syndrome after a pylorus preserving pancreatoduodenctomy presenting with obstructive jaundice and ascending cholangitis. Clin Endosc 2011; : 59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pfahler GE, Stamm CS. Diagnosis of enteroliths by means of roentgen rays. Surg Gynecol Obstet 1915; : 14–17. [Google Scholar]
- 12.Locke GR, Alexander GL, Sarr MG. Obstructive jaundice: an unusual presentation of afferent loop obstruction. Am J Gastroenterol 1994; : 942–944. [PubMed] [Google Scholar]
- 13.Dias AR, Lopes RI. Biliary stone causing afferent loop syndrome and pancreatitis. World J Gastroenterol 2006; : 1,229–6,231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee MC, Bui JT, Knuttinen MG et al. Enterolith causing afferent loop obstruction: a case report and literature review. Cardiovasc Intervent Radiol 2009; : 1,091–1,096. [DOI] [PubMed] [Google Scholar]
- 15.Delcore R, Cheung LY. Surgical options in postgastrectomy syndromes. Surg Clin North Am 1991; : 57–75. [DOI] [PubMed] [Google Scholar]
- 16.Burkhart RA, Relles D, Pineda DM et al. Defining treatment and outcomes of hepaticojejunostomy failure following pancreaticoduodenectomy. J Gastrointest Surg 2013; : 451–460. [DOI] [PubMed] [Google Scholar]


