Abstract
Background and Purpose
Decreased physical activity levels are an increasing concern, specifically for the aging population. Older adults (>65 years) are able to achieve health benefits from participating in a regular exercise program based on studies done in younger community-dwelling older adults. There is less research investigating the efficacy of exercise for improving physical function among the older adult population in assisted living settings. This study investigated using a treadmill with a harness system, to engage older adults in aerobic exercise. The primary objective of the study was to assess the feasibility of a large trial by evaluating the recruitment and short-term retention rate of older adults with limited mobility. Secondary objectives were to determine whether older adults could achieve the frequency, intensity, and duration of aerobic exercise recommended by the American College of Sports Medicine.
Methods
A feasibility study of residents of an assisted living facility who had care needs ranging from retirement home to palliative care. The feasibility of recruitment and retention was determined by recording the number of older adults who consented to participate in treadmill walking for 3 weeks, declined treadmill participation including reasons why, and completed the 6 treadmill sessions. All participating residents completed a baseline assessment, including a medical chart review, and had the choice to walk on the treadmill or not. To determine whether participants could achieve what is recommended in physical activity guidelines, exercise, frequency, intensity, and duration achieved after the final treadmill sessions were reported.
Results
Among eligible residents, 30% consented to participate in the study. There were no significant differences between treadmill participants and those who chose not to walk on the treadmill. The average compliance to treadmill sessions was 94.4% ± 10.8%. Treadmill participants achieved an average intensity of 50.3% heart rate reserve (SD = 30.2%) and an average frequency of 3 sessions in 1 week. Average duration of the final session was 14 minutes 53 seconds ± 6 minutes 43 seconds.
Conclusion
This study provides preliminary evidence that it is feasible to recruit and retain older adults in assisted living facilities to participate in a short-term treadmill walking study; however, it may be difficult to recruit a large number of individuals. Treadmill participants were able to achieve the American College of Sports Medicine’s recommended intensity and frequency for aerobic exercise. For older adults in assisted living settings to achieve 20 minutes a day, they may need more than 3 weeks of progression or multiple sessions per day.
Keywords: assisted living, exercise, older adults, treadmill, walking
BACKGROUND
Inactivity among older adults contributes to an increase in the prevalence of chronic diseases, functional limitations, and the risk of falling.1–4 Interventions such as exercise have the potential to help maintain physical function and independence in older adults.5–7 Research evaluating the efficacy of exercise among older adults has primarily been conducted in relatively healthy community-dwelling individuals and may not be applicable to older adults in assisted living settings.8–11 There are trials conducted in residents of assisted living settings that demonstrate that interventions such as tai chi, aerobic exercise, and seated resistance training can improve health-related outcomes and reduce falls.12–15 Furthermore, a scoping review of trials conducted in long-term care homes revealed that including exercise in a multifaceted intervention may be able to reduce the risk of falling in older adults.15
Although some trials have examined the efficacy of exercise programs in assisted living settings, there are a number of limitations that create barriers in the translation of knowledge to practice. There is inconsistent reporting of exercise program details2,16–20 and adverse events in randomized trials of exercise in older adults.21–25 Although Canada’s Physical Activity Guide for Older Adults provides recommendations for exercise frequency, intensity, and duration (4–7 days per week, 30–60 minutes per day at a “moderate” intensity),18 more specific recommendations may be needed to guide therapeutic exercise prescription. The American College of Sports Medicine (ACSM) recommendations for older adults may not be realistic for frail older adults but are more specific; frequency at least 3 days per week, duration of at least 20 minutes, and intensity of 40% to 60% of heart rate reserve (HRR).16 It is unknown whether either set of recommendations is appropriate for older adults in assisted living settings.16,26 Furthermore, the exclusion criteria often applied in exercise clinical trials in assisted living settings (eg, mild to severe cognitive impairment, joint replacement) reduce the generalizability of the results.12,27–30 Trials that have relatively rigorous exercise regimens may cause self-selection of the fittest participants, and the findings and exercise programs may not be realistic for a large proportion of frail individuals in assisted living settings.21,24,31 The exercise capacity of the typical resident in assisted living settings may not be sufficient to tolerate the level of training used in clinical trials.
To develop exercise recommendations specific to frail older adults with multiple comorbidities, there is a need to determine realistic goals and to design trials to evaluate their efficacy that are generalizable to a broader spectrum of older adults. To start, it would be useful to determine whether it is feasible to recruit older adults to participate in exercise clinical trials and evaluate exercise capacity among individuals in assisted living settings. Therefore, the primary objective of this study was to assess the feasibility of a large trial by evaluating the recruitment and short-term retention rate of older adults residing in an assisted living setting who would not be considered community ambulators. Secondary objectives were to determine whether the residents could achieve the frequency, intensity, and duration of aerobic exercise recommended by the ACSM and to compare residents who do and do not agree to participate in a study of treadmill walking exercise.
METHODS
Research Design
The research design was a pilot, feasibility study.32 The ACSM guidelines for older adults (3–5 times a week, 40% HRR, duration of 20–60 minutes)16 were used to determine whether the residents could achieve a frequency, intensity, and duration associated with achieving health benefits from exercising. The ACSM guidelines were chosen because they include specific exercise volume, and because the frequency and duration requirements are more conservative than the Canadian guidelines.
Participants
Residents living in a local assisted living setting from September 2008 to February 2009 were considered for participation. All residents (n = 263) were screened and the kinesiologist identified residents who were considered eligible for inclusion if they could safely walk 2 m independently (with or without assistive devices), were older than 65 years, could follow 2-step verbal commands, and received their physicians’ approval to participate in aerobic exercise. Residents were excluded if they were under palliative care, considered community ambulator (gait speed > 0.8 m/s), or had Parkinson’s disease, history of stroke affecting gait, multiple sclerosis, peripheral neuropathy, or other neurological conditions severely affecting physical function. Individuals with neurological conditions were excluded primarily because it was hypothesized that exercise capacity would be very different for this subset of older adults, and should be studied in a separate trial. The aim was to recruit individuals who were a frailer group, are not considered to be community ambulators, and are often excluded from exercise trials. Participating residents had 2 options to select from (1) to complete baseline testing, provide medical history, and walk on the treadmill (Treadmill Participants), or (2) to complete baseline testing and/or provide medical history only (nontreadmill participants). Consent was obtained by the resident and/or his or her legal representative. This study received ethics approval by the Office of Research Ethics at University of Waterloo.
Walking Protocol
A treadmill and harness (RTM 600 and Unweighting System, Biodex Medical Systems, New York) located within the assisted living setting were used. We used 6 sessions over 3 weeks to allow participants to become accustomed to treadmill walking. Session 1 was used for familiarization and participants self-selected their walking speed. The goals for session 2 were for the participant to achieve the walking speed obtained in session 1 within the first 2 minutes and to progressively increase speed until their fastest most comfortable walking speed was reached. For the remaining sessions, the goals were to achieve their fastest most comfortable walking speed within the first 2 minutes and maintain that speed, while increasing duration each session. Speed was adjusted upon request from the participant. Heart rate was monitored using a Polar heart rate monitor (Polar Electro Inc, Lake Success, NY) throughout each session and compared with a predetermined target (40% HRR) intensity, calculated using the Karvonen method. For participants on β-blockers, the age-predicted maximum heart rate was adjusted by 85%.33 During each session, the participants were asked whether they were willing to increase walking speed if they had not yet achieved 40% HRR. Walking speed was decreased if HRR exceeded 60%. Participants were encouraged to walk for as long as they could, and each walking session was stopped upon request from the participant.
Outcome Measures
The primary feasibility outcomes included the number of residents agreeing to participate in treadmill walking; the number of residents who agreed to participate, but not walk on the treadmill; the number of treadmill sessions completed compared with the number of potential sessions; and the number of residents who did not agree to participate and reasons why (if provided). Health-related and demographic characteristics were obtained from medical charts at the home. Secondary outcomes including cognition and walking endurance (assistive aids were allowed) were assessed by a research assistant using the Modified Mini-Mental State Examination (3MS)34 and the 6-minute walk test (6MWT),35 respectively. Participants were asked to walk as far as possible for 6 minutes over a marked course in the hallway of the facility. The distance completed in 6 minutes was recorded. For residents who consented to provide a medical history only, 3MS scores were obtained from their chart if possible. To determine the participants’ concern with falling, they completed the Activities-Specific Fall Concern (AFC) Scale at the baseline visit.36 The AFC is a valid and reliable measure of falls self-efficacy designed specifically for individuals living in residential and assisted living facilities.36 Furthermore, the rating scale uses a traffic light and simple language so that it can be applied in individuals with mild cognitive impairment.36 Treadmill walking capacity was quantified by recording walking speed, cumulative distance, duration, intensity (% HRR), and rate of perceived exertion using the BORG CR10 scale.37
Statistical Analysis
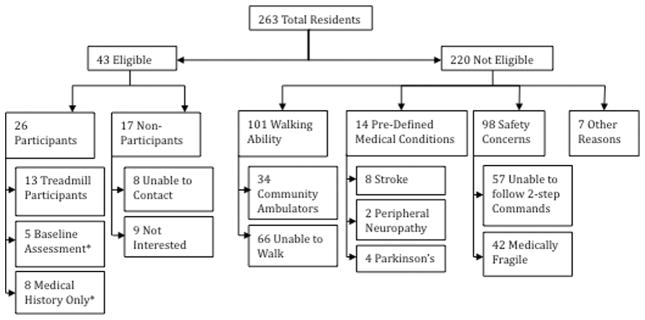
To determine feasibility of recruitment, the a priori criteria for success of this pilot trial were as follows: (a) 30% of the eligible residents will consent to participate and (b) participants will comply with at least 70% of the required sessions on the treadmill. The sample size was based primarily on feasibility considerations. Recruitment was calculated by the number of treadmill walking participants over the number of potentially eligible residents. Compliance was determined by the number of completed sessions divided by 6 possible treadmill sessions. A flow chart was used to track the flow of residents through the study (Figure 1).
Figure 1.
Flow diagram of participant recruitment and resident exclusion. *denotes non-treadmill participants.
To determine whether participants were able to achieve the recommended dose of exercise according to the ACSM for older adults, the frequency, intensity, and duration achieved by participants in the last completed treadmill session were compared with ACSM recommendations. Intensity recommended by the ACSM is 40% to 60% HRR; peak % HRR reached in the last session was used for comparison. Total cumulative duration obtained in the last session was compared with the ACSM-recommended duration of at least 20 minutes. Participants were considered to have achieved the frequency (3–5 times per week) if they attended 3 sessions in 1 week.
Data are presented as mean (standard deviation [SD]) for continuous variables and count (percent) for categorical variables. We used t tests to explore differences between treadmill participants and nontreadmill participants on secondary outcomes (6MWT, 3MS score, AFC score). The results are reported as estimate of differences (corresponding 95% confidence intervals and associated P values). We did not adjust the overall level of significance (set α = .05) for multiple comparisons as these analyses were mainly exploratory. All analyses were performed using SPSS (version 14, Armonk, New York).
RESULTS
Twenty-six residents agreed to participate in the pilot study (Table 1). Thirteen of 43 potentially eligible residents (30%) agreed to participate in treadmill walking, and 13 (30%) declined participation in treadmill walking but agreed to either the full assessment and chart abstraction or the chart abstraction only (Figure 2). There were no statistical significant differences between treadmill participants and nontreadmill participants for age, 3MS and AFC score, the number of comorbidities, and the 6MWT distance (Table 2). However, the mean difference and confidence intervals for age and cognition suggest that treadmill participants may have been younger and had higher cognitive function, but the sample size was too small to detect a true difference.
Table 1.
Participant Characteristics
| Characteristic | Treadmill Participants (n = 13a) | Nontreadmill Participants (n = 13) |
|---|---|---|
| Age, mean (SD), y | 84.9 (7.3) | 88.6 (4.3) |
| Number of women, n | 8 | 5 |
| Length of stay, mean (SD), y | 3 (2.7) | 3.42 (1.91) |
| Cognitive function (3MS score/100), mean (SD) | 81.8 (15.0) | 74.2 (15.3)b |
| Fall Concern (Activities-Specific Fall Concern Score/40), mean (SD) | 19.2 (8.3) | 17.3 (8.6)b |
| 6MWT, mean (SD) | ||
| Distance, m | 237.6 (82.9) | 243.6 (26.0)b |
| Velocity, m/s | 0.81 (0.25) | 0.81 (0.11)b |
| Use of assistive device | 9 (69%) | 11 (85%)b |
| No. of comorbid conditions | ||
| 0–2 | 0 | 1 |
| 3–5 | 6 | 5 |
| 6+ | 7 | 7 |
| Average number of medications, mean (SD) | 7.8 (3.8) | 9.15 (3.21) |
| On 10 or more medications, n | 3 | 5 |
| Number on β-blockers | 5 | 5 |
Abbreviations: 6MWT, 6-minute walk test; 3MS, Modified Mini-Mental State Examination.
Characteristics include the 1 resident who dropped out after 3 treadmill sessions.
(n = 5) Only 5 nontreadmill participants completed Modified Mini-Mental State Examination, Fall Concern, 6-minute walk test assessment.
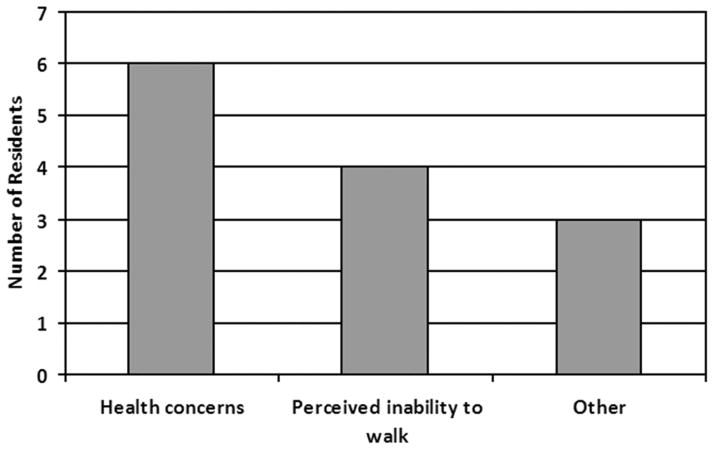
Figure 2.
Reasons why resident nontreadmill participants did not want to walk on the treadmill.
Table 2.
Differences Between Treadmill Participant Group and Nontreadmill Participant Group
| Characteristic | Mean Difference (95% Confidence Interval) | P Value (t Test) |
|---|---|---|
| Age, y | 3.7 (−8.5, 1.2) | .13 |
| Cognitive function (3MS score) | 7.6 (−9.2, 24.5) | .35 |
| Fall concern (Activities-Specific Fall Concern score) | 1.6 (−7.4, 10.7) | .71 |
| No. of comorbidities | 0.5 (−1.7, 2.6) | .66 |
| 6MWT distance | 6.0 (−87.5, 75.5) | .88 |
Abbreviations: 6MWT, 6-minute walk test; 3MS, Modified Mini-Mental State Examination.
Treadmill walking capacity parameters for residents who agreed to walk on the treadmill are presented in Table 3. Ten participants achieved the ACSM-recommended intensity of 40% HRR, mean (SD) = 64% (20%); only 2 residents (both on β-blockers) were unable to reach 40% HRR in the final session, mean (SD) = 26% (1%), despite the fact that the target heart rates had been adjusted to account for β-blocker use. The number of treadmill participants achieving a cumulative duration of each 5-minute interval in the last treadmill session is presented in Figure 3, with a minimum walking duration of 5 minutes to a maximum walking duration of 24 minutes.
Table 3.
Mean (SD) Exercise Parameters for Treadmill Participants
| Parameter | Session 1 | Session 2 | Session 6 |
|---|---|---|---|
| Speed, km/h | 1.55 (1.0) | 2.16 (1.33) | 2.48 (1.36) |
| Distance, km | 0.13 (0.08) | 0.30 (0.22) | 0.67 (0.57) |
| Intensity (% HRR) | 44.5 (19.9) | 53.1 (21.6) | 57.6 (23.4) |
| Rate of perceived exertion (1–10) | 4.1 (1.6) | 4.6 (1.2) | 4.58 (1.16) |
| Duration (min:s)a | 5:48 (2:00) | 9:13 (3:44) | 14:53 (6:43) |
Abbreviation: HRR, heart rate reserve.
Duration in session 1 was limited to 6 minutes to match baseline assessment of the 6-minute walk test.
Figure 3.
Cumulative duration achieved by treadmill participants in final treadmill session.
Eleven of 12 participants (92%) attended 3 treadmill sessions in 1 week. Three participants missed 1 session each because of scheduling conflicts and therefore completed only 5 of 6 treadmill sessions. The average compliance was 94.4% ± 10.8% of the 13 participants participating in treadmill walking, and 12 (92%) met the feasibility requirement of attending at least 4 of the 6 sessions scheduled. The 1 participant who did not meet the expected compliance had declining health.
DISCUSSION
A key finding of this report is that even those individuals living in assisted living settings who have limited mobility are capable of short (15 minutes or less) bouts of treadmill walking at 40% of HRR or greater and were agreeable to complete 3 sessions in 1 week. Although we achieved our recruitment target, the screening to recruitment ratio for the exercise portion of the study was greater than 3:1. The implications of this study are 2-fold: (1) exercise guidelines specific to frail older adults in assisted living settings may need to reduce the duration of exercise to achieve broader acceptance and (2) future clinical trials of exercise in assisted living settings may need a multicenter trial design to achieve the sample size needed to evaluate efficacy.
A consistent finding in this study was that residents were unable to achieve the ACSM-recommended duration of 20 minutes. Canada’s Physical Activity Guide18 is less specific to older adults and recommends a much longer duration. Sattelmair et al4 report that it could take months for the deconditioned frail older adult to achieve exercise recommendations. Interventions may need to last a minimum of 6 weeks, as one treadmill study saw no training effects until week 6 of 12.38 Participants in the current study may have been able to reach 20 minutes’ duration if their room was located closer to the treadmill, the protocol lasted longer than 3 weeks, or more than 1 session per day was offered. For older adults, it has been recommended to increase duration first and then adjust speed (intensity) as necessary.16,26,38 However, it remains to be determined whether a short bout of activity at the target intensity would be more effective than a longer duration bout with an intensity lower than currently recommended for health benefits. Shorter exercise bouts would be easier to implement and possibly more desirable to the participant. In adults with coronary artery disease, interval training has been shown to be effective and safe; however, the dose-response relationship is still to be determined.39 Although near-maximal exercise intensities would not be advisable in frail older adults, an exercise program emphasizing shorter-duration interval training may be an interesting paradigm to test in a clinical trial of exercise in this population. Studies to date of residents in assisted living settings have reported durations of 20 minutes or longer, suggesting that their populations are not representative of the general population in these settings.21,24,40,41 The current study reveals that it may not be realistic to expect frail older adults to achieve a minimum of 20 minutes of physical activity in one bout at the target intensity.
Although most participants achieved the recommended frequency (92%) and intensity (83%) of exercise, there is clearly a need for individualization of exercise testing and exercise prescription protocols. We used the Karvonen formula to determine each participant’s target heart rate zone and the crude formula of 220 minus age to predict maximum heart rate. A maximal exercise test would not have been practical in the frail older adult population, but a submaximal test may have been feasible and provided a more accurate assessment of exercise capacity. Given the difficulties we expected recruiting individuals to simply walk on the treadmill at self-selected speeds, we chose not to implement formal exercise testing. Increasing speed is often used as a means to increase intensity during walking but may limit exercise progression for individuals with motor control difficulties or those who do not wish to move past a “comfortable” walking speed. The use of an incline was not implemented in this study but may be a means to increase intensity gradually without increasing speed. Finally, despite adjustment for β-blocker use, the 2 participants on β-blockers were not able to achieve our target intensity, which may be due to compromised exercise capacity or to inaccuracies in the methods used to estimate exercise intensity.
The current investigation revealed that future studies of walking or treadmill exercise should expect to screen at least 3 people for every one needed in the trial. Given that we were able to recruit an additional 30% of our potentially eligible residents to participate in the walking assessments and chart review, it is likely that it was the commitment to the exercise that deterred many individuals. It is possible that residents were not fearful of walking, but of the treadmill specifically. However, few cited the treadmill as the reason for their refusal. Only a few other studies that involved walking as part of an intervention reported the proportion of people who were screened, included, and consented; the proportions of eligible residents consenting in these studies were 17%,24 25%,31 and 29% respectively,23 suggesting that our screening-to-recruitment ratio of 3:1 is accurate. A few methodological recruitment barriers were encountered in the present study. Two staff kinesiologists evaluated eligibility, whereas nurses may have been more appropriate to confirm participant eligibility. A biweekly review would allow for identification of more new residents. Consent was not provided by some of the residents’ legal representatives; therefore, we were unable to approach residents themselves for study participation, which was an unexpected barrier to recruitment. We recommend that any future clinical trials in the assisted living setting screen 4 times the number of required participants (and many more if individuals with neurological impairment are to be excluded). The quality of reporting should be improved according to the CONSORT recommendations for clinical trials so that information about recruitment and retention is available to assist in the planning of future trials.42
Limitations
The sample size in this study was small, may have represented a select group of highly motivated individuals, and could have been increased by including the residents who were not eligible because they were considered to be community ambulators (gait speed > 0.8 m/s). It is not possible to determine whether it was exercise in general or treadmill walking in particular that was not appealing to those who did not agree. Barriers that affected compliance include events such as designated meal times and social activities and medical outbreaks that occur within the home. Future work should consider offering other modes of exercise such as the recumbent stepper, cycling, or even overground walking to provide the participants with options in the event that they are fearful or uncomfortable with treadmill walking.
CONCLUSIONS
Based on a priori criteria, it is feasible to recruit older adults in assisted living facilities to participate in a treadmill walking study. To make recruitment in the assisted living setting more efficient and effective, strategies such as having the eligibility list reviewed biweekly by a health care professional, broadening the inclusion criteria, and improving education to legal representatives and residents about the study should be implemented. This study provides preliminary evidence that residents in an assisted living setting can achieve ACSM’s recommended intensity and frequency for aerobic or endurance exercise while walking on a treadmill, but that it may not be realistic to expect residents to walk for a cumulative duration of 20 minutes. Further research evaluating the effectiveness of exercise for residents in assisted living settings should consider multicenter trials to increase sample size, utilize other modes of exercise, aim to improve reporting, and adopt consistent protocols for determining and progressing intensity, frequency, and duration.
Acknowledgments
We would like to express our gratitude to the Research Institute for Aging (RIA) and the Ontario Rehabilitation Research Advisory Network for financial support. We thank the RIA for providing the space and access to residents to conduct the project. We would also like to thank Susan Brown for assisting with the coordination of the project. Dr. Giangregorio has received infrastructure funding and other support from the Canada Foundation for Innovation, the Ontario Ministry of Research and Innovation, and the Canadian Institutes of Health Research.
Footnotes
The poster was presented at Canadian Geriatric Society (2009).
The authors declare no conflicts of interest.
References
- 1.Bruce DG, Devine A, Prince RL. Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc. 2002;50(1):84–89. doi: 10.1046/j.1532-5415.2002.50012.x. [DOI] [PubMed] [Google Scholar]
- 2.Paterson DH, Jones GR, Rice CL. Ageing and physical activity: evidence to develop exercise recommendations for older adults. Appl Physiol Nutr Metab. 2007;32(32E):S69–S108. [PubMed] [Google Scholar]
- 3.van der Bij AK, Laurant MGH, Wensing M. Effectiveness of physical activity interventions for older adults: a review. Am J Prev Med. 2002;22(2):120–133. doi: 10.1016/s0749-3797(01)00413-5. [DOI] [PubMed] [Google Scholar]
- 4.Sattelmair JR, Pertman JH, Forman DE. Effects of physical activity on cardiovascular and noncardiovascular outcomes in older adults. Clin Geriatr Med. 2009;25(4):677–702. viii–ix. doi: 10.1016/j.cger.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 5.Taunton JE, Martin AD, Rhodes EC, Wolski LA, Donelly M, Elliot J. Exercise for the older women: choosing the right prescription. Br J Sports Med. 1997;31(1):5–10. doi: 10.1136/bjsm.31.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CBC News. Canadian health-care spending to top $180B. CBC News; [Accessed November 19, 2009]. http://www.cbc.ca/health/story/2009/11/19/health-care-spending-canada.html. [Google Scholar]
- 7.Ariste R, Rondeau A, Arnold J, et al. Provincial and Territorial Government Health Expenditure by Age Group, Sex and Major Category: Recent and Future Growth Rates. Ottawa, Ontario, Canada: Canadian Institute for Health Information; May, 2005. [Google Scholar]
- 8.Skelton DA, Beyer N. Exercise and injury prevention in older people. Scand J Med Sci Sports. 2003;13(1):77–85. doi: 10.1034/j.1600-0838.2003.00300.x. [DOI] [PubMed] [Google Scholar]
- 9.Yeom HA, Keller C, Fleury J. Interventions for promoting mobility in community-dwelling older adults. J Am Acad Nurse Pract. 2009;21(2):95–100. doi: 10.1111/j.1745-7599.2008.00390.x. [DOI] [PubMed] [Google Scholar]
- 10.Bean JF, Vora A, Frontera WR. Benefits of exercise for community-dwelling older adults. Arch Phys Med Rehabil. 2004;85(7 suppl 3):S31–S42. doi: 10.1016/j.apmr.2004.03.010. quiz S43–S44. [DOI] [PubMed] [Google Scholar]
- 11.Daniels R, van Rossum E, de Witte L, Kempen GI, van den Heuvel W. Interventions to prevent disability in frail community-dwelling elderly: a systematic review. BMC Health Serv Res. 2008;8:278. doi: 10.1186/1472-6963-8-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brill PA, Cornman CB, Davis DR, et al. The value of strength training for older adults. Home Care Provid. 1999;4(2):62–66. doi: 10.1016/s1084-628x(99)90105-3. [DOI] [PubMed] [Google Scholar]
- 13.Chin A, Paw MJ, van Poppel MN, Twisk JW, van Mechelen W. Once a week not enough, twice a week not feasible? A randomised controlled exercise trial in long-term care facilities [ISRCTN87177281] Patient Educ Couns. 2006;63(1/2):205–214. doi: 10.1016/j.pec.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Wolf SL, Barnhart HX, Kutner NG, et al. Selected as the best paper in the 1990’s: reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. J Am Geriatr Soc. 2003;51(12):1794–1803. doi: 10.1046/j.1532-5415.2003.51566.x. [DOI] [PubMed] [Google Scholar]
- 15.Sawka AM, Ismaila N, Cranney A, et al. A scoping review of strategies for the prevention of hip fracture in elderly nursing home residents. PLoS ONE. 2010;5(3):e9515. doi: 10.1371/journal.pone.0009515. [Electronic Resource] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazzeo RS, Tanaka H. Exercise prescription for the elderly: current recommendations. Sports Med. 2001;31(11):809–818. doi: 10.2165/00007256-200131110-00003. [DOI] [PubMed] [Google Scholar]
- 17.Elsawy B, Higgins KE. Physical activity guidelines for older adults. Am Fam Physician. 2010;81(1):55–59. [PubMed] [Google Scholar]
- 18.Public Health Agency of Canada. Canada’s Physical Activity Guide to Healthy Active Living for Older Adults. Ottawa, Ontario, Canada: Public Health Agency of Canada; 2003. [Google Scholar]
- 19.Rose DJ, Hernandez D. The role of exercise in fall prevention for older adults. Clin Geriatr Med. 2010;26(4):607–631. doi: 10.1016/j.cger.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 20.Cameron ID, Murray GR, Gillespie LD, et al. Interventions for preventing falls in older people in nursing care facilities and hospitals. Cochrane Database Syst Rev. 2010;(1):CD005465. doi: 10.1002/14651858.CD005465.pub2. [DOI] [PubMed] [Google Scholar]
- 21.Faber MJ, Bosscher RJ, Chin A, Paw MJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: a multicenter randomized controlled trial. Arch Phys Med Rehabil. 2006;87(7):885–896. doi: 10.1016/j.apmr.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 22.Rakobowchuk M, Tanguay S, Burgomaster KA, Howarth KR, Gibala MJ, MacDonald MJ. Sprint interval and traditional endurance training induce similar improvements in peripheral arterial stiffness and flow-mediated dilation in healthy humans. Am J Physiol Regul Integr Comp Physiol. 2008;295(1):R236–R242. doi: 10.1152/ajpregu.00069.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacRae PG, Asplund LA, Schnelle JF, Ouslander JG, Abrahamse A, Morris C. A walking program for nursing home residents: effects on walk endurance, physical activity, mobility, and quality of life. J Am Geriatr Soc. 1996;44(2):175–180. doi: 10.1111/j.1532-5415.1996.tb02435.x. [DOI] [PubMed] [Google Scholar]
- 24.Sauvage LR., Jr A clinical trial of strengthening and aerobic exercise to improve gait and balance in elderly male nursing home residents. Am J Phys Med Rehabil. 1992;71(6):333. doi: 10.1097/00002060-199212000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Pilon M, Thomas KJ, Hendrix K. Improvements in walking speed experienced by elders participating in a cardiovascular exercise program. J Geriatr Phys Ther. 2006;29(3):87–91. doi: 10.1519/00139143-200612000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Mazzeo RS, Cavanagh P, Evans WJ, et al. ACSM position stand: exercise and physical activity for older adults. Med Sci Sports Exerc. 1998;30(6):992–1008. [PubMed] [Google Scholar]
- 27.Hui EK, Rubenstein LZ. Promoting physical activity and exercise in older adults. J Am Med Dir Assoc. 2006;7(5):310–314. doi: 10.1016/j.jamda.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 28.Hellebrant FA. Exercise for the long term care aged—benefits, deterrents, and hazards. Long Term Care Health Serv Adm. 1979;3(1):33–47. [PubMed] [Google Scholar]
- 29.Pratt MA. Physical exercise: a special need in long-time care. J Gerontol Nurs. 1978;4(5):38–42. doi: 10.3928/0098-9134-19780901-10. [DOI] [PubMed] [Google Scholar]
- 30.Lazowski D, Ecclestone NA, Myers AM, et al. A randomized outcome evaluation of group exercise programs in long-term care institutions. J Gerontol A Biol Sci Med Sci. 1999;54(12):621–628. doi: 10.1093/gerona/54.12.m621. [DOI] [PubMed] [Google Scholar]
- 31.Bo M, Fontana M, Mantelli M, Molaschi M. Positive effects of aerobic physical activity in institutionalized older subjects complaining of dyspnea. Arch Gerontol Geriatr. 2006;43(1):139–145. doi: 10.1016/j.archger.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 32.Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10(1):1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mackay-Lyons MJ, Makrides L. Exercise capacity early after stroke. Arch Phys Med Rehabil. 2002;83(12):1697–1702. doi: 10.1053/apmr.2002.36395. [DOI] [PubMed] [Google Scholar]
- 34.Teng EL, Chui HC. The Modified Mini-Mental State (3MS) Examination. J Clin Psychiatry. 1987;48(8):314–318. [PubMed] [Google Scholar]
- 35.Crapo RO, Casaburi R, Coates AL, et al. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 36.Blanchard R, Myers AM, Pearce NJ. Reliability, construct validity, and clinical feasibility of the Activities-Specific Fall Concern scale for residential living seniors. Arch Physical Med Rehabil. 2007;88(6):732–739. doi: 10.1016/j.apmr.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 37.Borg G. Borg’s Perceived Exertion and Pain Scales. 3. Champaign, IL: Human Kinetics; 1998. [Google Scholar]
- 38.Stamford BA. Physiological effects of training upon institutionalized geriatric men. J Gerontol. 1972;27(4):451. doi: 10.1093/geronj/27.4.451. [DOI] [PubMed] [Google Scholar]
- 39.Cornish AK, Broadbent S, Cheema BS. Interval training for patients with coronary artery disease: a systematic review. Eur J Appl Physiol. 2011;111(4):579–589. doi: 10.1007/s00421-010-1682-5. [DOI] [PubMed] [Google Scholar]
- 40.Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people: the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehabil. 2004;83(7):493–499. doi: 10.1097/01.phm.0000130025.54168.91. [DOI] [PubMed] [Google Scholar]
- 41.Tappen RM, Roach KE, Applegate EB, Stowell P. Effect of a combined walking and conversation intervention on functional mobility of nursing home residents with Alzheimer disease. Alzheimer Dis Assoc Disord. 2000;14(4):196–201. doi: 10.1097/00002093-200010000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63(8):834–840. doi: 10.1016/j.jclinepi.2010.02.005. [DOI] [PubMed] [Google Scholar]