Abstract
Objective
The postpartum period represents a crucial transition period in which weight gain or loss can affect lifetime obesity risk. This study examined the prevalence of obesity and the influence of childhood abuse and family conflict on postpartum weight among low-income Mexican-origin women. Depressive symptoms and partner support were evaluated as mediators.
Methods
At a prenatal assessment, low-income Mexican-origin women (N=322; mean age = 27.8; SD = 6.5) reported on childhood abuse and family conflict. Weight was measured seven times between 6 weeks and 2 years postpartum and calculated as body mass index (BMI). Regression and growth models were used to estimate the impact of childhood abuse, childhood family conflict, partner support, and depressive symptoms on weight and weight change.
Results
Higher family conflict predicted higher weight across the first (β = .12, p = .037) and second (β = .16, p = .012) postpartum years. Family conflict (β = .17; p = .018) and low partner support (β = −.16, p = .028) also predicted increasing weight in the first year. Partner support partially mediated the effect of childhood abuse on weight change in the first year (p = .031). Depressive symptomatology mediated the effects of childhood abuse and family conflict on weight status in the second year (abuse: p = .005; conflict: p = .023).
Conclusions
For low-income Mexican-origin women with a history of childhood abuse or high family conflict, depression and low partner support may be important targets for obesity prevention efforts in the postpartum period.
Keywords: Mexican, postpartum, weight, childhood abuse, conflict, depression
Childhood exposure to high conflict or abusive family environments increases the risk of multiple physical and psychological disorders across the lifespan (1). Among adult health concerns with probable early life origins, obesity deserves focused attention. Considered the third leading cause of preventable death in the US (2), overweight and obesity are primary targets of public health efforts. The health risks associated with obesity are numerous, and include cardiovascular disease, stroke, type 2 diabetes, respiratory problems, mental health problems, and premature mortality (3). Worldwide, rates of overweight and obesity have increased dramatically in the past few decades (4). In the US, approximately two-thirds of adults are overweight and more than a third are obese (5). There are considerable health disparities in obesity risk. Obesity rates are elevated among ethnic minority women, with 43.3% of Hispanic women classified as obese in 2012 compared to 36.7% of non-Hispanic White women (5). While overall obesity rates among women in the U.S. show signs of stabilizing, they have continued to increase among Mexican-American women (4). Low-income women and those with less education are also at elevated risk of obesity (6). The high prevalence of obesity among Mexican-origin women (i.e., women born in Mexico or who trace their family ancestry to Mexico) in the U.S., especially those in low-income neighborhoods (7), contributes to a wide range of health disparities (8–9). It is critical to develop a better understanding of predictors of obesity in this population for targeted prevention efforts to be maximally effective.
Prior research indicates that family-related adversities in childhood, including abuse, conflict, violence, and general dysfunctions may significantly increase lifespan obesity risk (10–13). Retrospective recall of physical abuse, witnessing abuse of a family member, family conflict, and household dysfunction during childhood have each been associated with increased BMI in middle-age (13–14). Exposure to physical and sexual abuse during childhood was similarly associated with obesity in adulthood in the US National Longitudinal Study of Adolescent Health (15). Evidence from a recent meta-analysis suggests a stronger impact of childhood abuse on obesity risk for women than men (16). The literature is mixed regarding rates of childhood abuse in Mexican-American families in the U.S., with studies finding comparable (17), higher (18), or lower (19) rates relative to ethnic majority families. However low-SES and high stress environments are associated with greater abuse risk across ethnic groups, and observed higher rates among Hispanic children typically diminish after adjusting for sociodemographic risk factors (19–20). Little is known about the relation of childhood adversity to adult obesity in Mexican-origin women living in the U.S.
For women, the highest risk of major weight gain occurs during the childbearing years, and retention of pregnancy weight in the postpartum period is a significant risk factor for continuing weight gain and obesity (21–22). Although most women lose weight in the first six weeks after the birth, many women retain pregnancy weight or even gain weight in the subsequent months (21–22). Estimates of average pre-post pregnancy weight gain vary depending on samples and methods, but range around 1–6 lbs. (23–24). Walker (25) reported a median weight gain of 0.9 kg (2 lbs.; range −6.8–29.5) over pre-pregnancy weights in a mixed ethnic sample at 12 months postpartum. Postpartum weight gain may partially explain higher obesity risk in low-income Mexican-origin women. Low-income women in the U.S. are more likely to retain weight gained during pregnancy than higher income women (26–27). Mexican-origin women in the US have higher birth rates than ethnic majority women (28) and are more than twice as likely to live in poverty (29); they are also less likely to lose pregnancy weight and more likely to gain weight in the first postpartum year than ethnic majority women (24). Given the implications for lifetime obesity risk, identifying influences on postpartum weight may enhance obesity prevention efforts among Mexican-origin women. Previous research has identified socioeconomic hardship, stress, low social support, and postpartum depressive symptoms as risk factors for postpartum weight retention (21, 25–26). Little is known about the impact of childhood adversity on postpartum weight.
There are several potential mediating pathways in the relation between childhood adversity and maternal weight status. Adults who were abused as children have higher risk of interpersonal problems, substance abuse, aggressive behavior, and affective disorders such as anxiety and depression (31). Particularly relevant to perinatal Mexican-origin women, the current study focuses on depressive symptoms and intimate relationship (partner) support as potential mediators in the relation between maltreatment and postpartum weight.
Childhood maltreatment is a robust risk factor for adult depression, particularly among women (32–33). A recent review extended this relation to the perinatal period, concluding that women with a history of childhood abuse had significantly elevated risk of postpartum depression (35). Mexican-origin and low SES women, particularly recent immigrants, are at substantially elevated risk for the development of postpartum depressive symptoms (36). In general population samples, strong associations have been found between depression and obesity, with a stronger association for women than for men (37–38). Postpartum depressive symptoms specifically have been associated with women’s weight gain and pregnancy weight retention in the early postpartum period (25–26, 39–40). In combination, a history of childhood maltreatment in low-income Mexican-origin women may further increase the already elevated risk of postpartum depressive symptoms, and subsequently impact postpartum weight and obesity risk.
Childhood family environments characterized by abuse and conflict are also associated with poor social functioning in adulthood. Lasting consequences for interpersonal relationships include low social support, feelings of isolation, lack of trust, attachment anxiety, marital distress, relationship aggression, and marital disruption (31–32, 41–43). Adults who experienced abuse or neglect in childhood report poorer adjustment (44) and less intimacy in their romantic relationships (45), and are less likely to maintain intimate relationships (32). The health benefits of supportive relationships are well-documented in the general population (46). For postpartum women, supportive relationships exert a protective influence on psychological adjustment (47–48), physical activity (49), and weight loss (50). In contrast, lack of social support has been cited as a barrier to postpartum weight loss in low-income women (50). Among pregnant Latina women, partner support helps promote healthier dietary and exercise practices (51).
The current study evaluated predictors and mediators of postpartum weight in low-income Mexican-origin women living in the U.S. The goals were to 1) evaluate the relation of childhood adversity to maternal weight status in the first and second postpartum years, 2) evaluate the impact of adversity on weight change (gain or loss) in the first postpartum year, and 3) evaluate partner support and postpartum depressive symptoms as mediators of the relations of adversity to postpartum weight and weight change. As measures of adversity, we assessed experiences of abuse (adversity directed specifically at the child) as well as a broader measure of adversity captured by a high conflict family-of-origin. We hypothesized that more frequent abuse and higher family conflict during childhood would each predict higher postpartum depressive symptoms, lower partner support, higher weight and less weight loss in the first postpartum year, and higher weight in the 2nd year. We further hypothesized that postpartum depressive symptoms and low partner support would predict higher weight and less weight loss, partially mediating the relations between childhood adversity and postpartum weight.
Methods
Participants
Pregnant Mexican-origin women (N=322; mean age = 27.8, SD = 6.5, range 18–45; 86% born in Mexico) were recruited from prenatal clinics in Maricopa County, Arizona that serve a diverse population, including low-income, uninsured, and/or undocumented immigrants. During prenatal care appointments, potentially eligible pregnant women were approached by a female, bilingual interviewer who explained the study and assessed eligibility. Eligibility criteria included 1) age 18 or older, 2) fluent in Spanish or English, 3) self-identification as Mexican or Mexican American, 4) low-income status (eligibility for Medicaid, or self-reported family income below $25,000), 5) singleton delivery, and 6) no prenatal evidence of an infant health or developmental problem. Of women who were eligible, 56% agreed to a home visit, conducted between 26–38 weeks gestation (mean 35.4 weeks, SD = 2.8). Sample demographics are displayed in Table 1.
Table 1.
Sample demographics and variable descriptives
| Age - Range; M (SD) | 18–45; 27.8 (6.5) |
| Number of children - Range; M (SD) | 1–10; 3 (1.7) |
| Country of birth – N (%) | |
| Mexico | 277 (86%) |
| United States | 45 (14%) |
| Child birthweight (g)- Range; M (SD) | 1190–4935; 3389 (464) |
| Education – N (%) | |
| 0 through 8 years of school | 87 (27%) |
| Some high school completed | 103 (32%) |
| High school graduate | 86 (27%) |
| Some college or vocational school | 26 (8%) |
| College degree (BS/BA) or above | 20 (6%) |
| Family Income - N (%) | |
| ≤$10,000 | 105 (33%) |
| $10,001 – $15,000 | 87 (28%) |
| $15,001 – $25,000 | 77 (25%) |
| ≥$25,001 | 45 (14%) |
| (refused = 8) | |
| Marital status – N (%) | |
| Married/living with partner | 249 (77%) |
| Single, divorced, widowed | 73 (23%) |
| Postpartum BMI - Range; M (SD) | |
| 6 weeks | 17.1–50.0; 29.1 (5.8) |
| 12 weeks | 16.5–51.4; 29.4 (5.8) |
| 18 weeks | 16.0–50.8; 29.6 (6.3) |
| 24 weeks | 17.6–52.1; 29.9 (6.7) |
| 12 months | 15.9–53.3; 29.6 (6.5) |
| 18 months | 15.5–55.9; 29.6 (6.6) |
| 24 months | 15.8–52.8; 29.1 (5.9) |
| Childhood abuse - Range; M (SD); % > 0 | 0–40; 4.8 (7.5); 54% |
| Sexual abuse – Range; M (SD); % > 0 | 0–16; 0.91 (2.4); 20.5% |
| Physical abuse - Range, M (SD); % > 0 | 0–12; 1.6 (2.9); 32.1% |
| Emotional abuse Range, M (SD); % > 0 | 0–12; 2.3 (3.2); 50% |
| Childhood conflict - Range; M (SD) | 0–6; 2.3 (1.8) |
| Depressive symptoms - Range; M (SD) | 0–21; 4.3 (4.8) |
| Partner support - Range; M (SD) | 6–30; 22.6 (7.2) |
Given the intensive home visit schedule in the first 6 postpartum months, a planned missingness design was employed to lower participant burden while retaining statistical power. All women were assigned to complete the prenatal and 6 week visits, but randomly assigned to complete 2 of the 3 remaining home visits, thereby reducing the respondent burden by 1/3. Prenatal data was collected from 322 women, 312 women (97%) completed the 6 week visit, 205 women (95%) completed the 12 week visit, 210 women (93%) completed the 18 week visit, and 210 women (93%) completed the 24 week visit. For the lab-based visits, 6 women were excluded: 4 due to loss of custody, one following safety concerns, and one maternal death. Of remaining women, 266 (83%) completed the 12 month visit, 237 (75%) completed the 18 month visit, and 244 (77%) completed the 24 month visit.
Attrition status was not associated with childhood family conflict, childhood abuse, postpartum partner support, postpartum depressive symptoms, household income, marital status, education, or 6 week maternal weight (all p’s > .05). However, younger women were more likely to miss a data collection time point. An inconsistent pattern emerged in which maternal birth in Mexico predicted attrition at 12 months, but birth in the U.S. predicted attrition at 18 months and 24 months. Mothers with more children had higher attrition at 6 months but less attrition at 12 months and 18 months. Given these results and potential influences on postpartum weight, statistical models adjusted for maternal age, country of birth, and number of children. Additionally, statistical analyses were conducted using MPlus 7.0 (52), which uses full information maximum likelihood to manage missing data.
Procedure
The study was approved by the Internal Review Boards at Arizona State University and Maricopa Integrated Health Services. Data were collected between March 2010 and December 2014. Participation included 5 home visits (prenatal, and 6, 12, 18, and 24 weeks postpartum) and 3 lab visits (12, 18, and 24 months postpartum). Informed consent was obtained at the prenatal home visit. Visits were scheduled between 8 AM and 5 PM. For lab visits, women received free transportation or $50 travel compensation. Interviews were conducted in Spanish (82%) or English (18%). Survey questions were read aloud and women were given written and graphic descriptions of item response options. Home and lab visits lasted approximately 2 hours, and women were compensated $75 and small gifts at the prenatal interview, $50 and small gifts at postpartum home visits, and $100 at the lab visits.
Measures
Childhood abuse and family conflict (assessed at prenatal visit)
Childhood experiences of physical (3 items; e.g., “People in your family hit you so hard that it left you with bruises or marks”), sexual (4 items; e.g., “Someone tried to make you do sexual things or watch sexual things”), and emotional (3 items; e.g., “People in your family called you things like ‘stupid’, ‘lazy’, or ‘ugly’”) abuse were reported with the Childhood Trauma Questionnaire (CTQ [53]; α = .92), a retrospective measure of experiences before the age of 18. Items were rated from 0 (never true) to 4 (very often true) and summed; higher scores indicate more frequent experiences of abuse. Childhood family conflict was measured retrospectively with six items from the Conflict subscale of the Moos Family Environment Scale (54; α = .71; e.g., “Family members sometimes hit each other”, “Family members sometimes got so angry they threw things”); items were rated 0 (false) or 1 (true), and summed. Higher values reflect higher exposure to family conflict.
Partner support (assessed at six weeks postpartum)
Women completed the six-item postpartum version of the partner support subscale of the Prenatal Expectations Scale for Mexican Americans (PES-MA; 55). Developed for low-acculturated Mexican-origin women, the PES-MA measures women’s experiences of support from their partner after the birth of a baby (α = .93; e.g., “Your spouse/partner helps take care of the baby”). Items were rated from 1 (Not at all) to 5 (Completely) and summed. Higher scores represent higher support.
Depressive symptoms (assessed at six weeks postpartum)
The 10-item Edinburgh Postnatal Depression Scale (56; α = .87) has been validated in English (56) and Spanish (57). Because of an error in response options on handheld cards, two items were treated as missing for 82 participants; multiple imputation (MPlus 7) was used to impute missing item-level values for these participants (58). Higher scores reflect higher depressive symptomatology.
Postpartum weight
Maternal height and weight were assessed by trained staff at each postpartum visit. Body mass index (BMI; kg/m2) was used for all analyses.
Covariates
At the prenatal visit, women reported their country of birth (Mexico: 86%; United States:14%), number of children (range 1–10, mean = 3, SD = 1.7), and age (range 18–45, mean = 27.8, SD = 6.5). Because it may influence postpartum weight (61), breastfeeding status (bottle-feeding: 51%; partial or exclusive breastfeeding: 49%) was recorded at 12 weeks postpartum.
Data Analyses
Preliminary analyses
Variable descriptives and correlations are displayed in Tables 1 and 2. Six women reported childhood abuse more than 3 SD above the mean. When analyses were repeated excluding those women, model fit indices remained good and all statistically significant paths retained significance; therefore, all cases were retained for analyses. Preliminary regression analyses predicted maternal BMI at each time point from childhood abuse or family conflict (in separate models), adjusting for age, number of children, country of birth, and breastfeeding status. Preliminary growth models found a statistically significant mean (β = .201, SE = .032, p <.001), and variance (β = .191, SE = .03, p < .001) in the slope of maternal BMI in the first year; however, neither the mean (p = .56) nor the variance (p = .27) in slopes were significant in the second year.
Table 2.
Zero-order correlations among model variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Childhood abuse | 1.0 | |||||||||
| 2. Childhood conflict | .56** | 1.0 | ||||||||
| 3. Depressive symptoms (6wk) | .33** | .22** | 1.0 | |||||||
| 4. Partner support | −.26** | −.21** | −.18** | 1.0 | ||||||
| 5. 6 week BMI | .12† | .15* | .15* | .00 | 1.0 | |||||
| 6. 12 week BMI | .13† | .10 | .15* | −.03 | .99** | 1.0 | ||||
| 7. 18 week BMI | .11 | .18** | .10 | −.06 | .98** | .99** | 1.0 | |||
| 8. 6 month BMI | .07 | .20** | .18* | .02 | .98** | .99** | .99** | 1.0 | ||
| 9. 12 month BMI | .08 | .17* | .23** | .02 | .96** | .94** | .96** | .97** | 1.0 | |
| 10. 18 month BMI | .15* | .20** | .22** | −.004 | .92** | .92** | .93** | .95** | .98** | 1.0 |
| 11. 24 month BMI | .12† | .19** | .16* | −.06 | .89** | .89** | .91** | .92** | .94** | .95** |
p < .10;
p < .05;
p < .01
Primary analyses
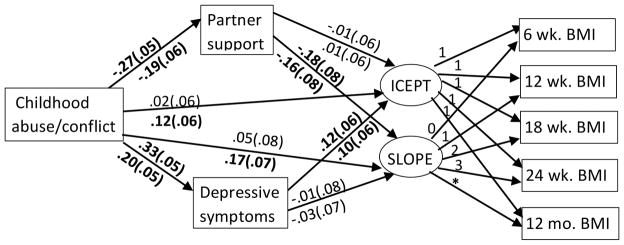
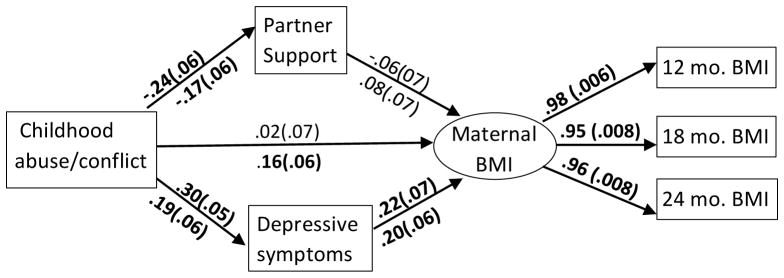
Primary analyses were conducted separately for weight across the first and second postpartum years. We expected significant variability in weight gain or loss in the first year following childbirth, but expected more stable weights in the 2nd year, as was supported by preliminary analyses (above). Evaluating weight in the 2nd year separately also provided a view of the longer-term effect of childhood adversity on maternal weight, distinct from the transitional post-pregnancy period. For the first year, latent growth curve models estimated the weight intercept and slope, predicted by childhood abuse or conflict, partner support, and depressive symptoms, adjusting for maternal age, number of children, country of birth, and breastfeeding (see Figure 1). Analyses in the second year excluded women who had become pregnant again (n = 33). A latent variable, created with maternal BMI at 12, 18, and 24 months as indicators, was predicted from childhood abuse or conflict, partner support, and depressive symptoms, adjusting for maternal age, number of children, breastfeeding, and country of birth (see Figure 2).
Figure 1.
Childhood abuse, family conflict, and maternal weight in the first postpartum year.
“Childhood abuse/conflict” (in separate models); standardized estimates (SE) for abuse shown above lines; standardized estimates (SE) for family conflict shown below lines. “wk” – week”; “mo.” = month. Statistically significant estimates are shown in bold font. Covariates (maternal age, number of children, country of birth, and breastfeeding), error terms, covariance between intercept and slope, and the covariance between the two mediators are not displayed in order to simplify presentation.
Figure 2.
Childhood abuse, family conflict, and maternal BMI in the second postpartum year.
“Childhood abuse/ conflict (in separate models); standardized estimates (SE) for abuse model shown above lines; standardized estimates (SE) for family conflict model shown below lines. “mo.” = months. Statistically significant estimates (p < .05) are shown in bold font. Covariates (maternal age, number of children, country of birth, and breastfeeding), error terms, and the covariance between the two mediators are not displayed in order to simplify presentation.
Primary analyses were conducted using MPlus 7.0 and maximum likelihood estimation. Model fit was examined using Chi-square (χ2), cumulative fit index (CFI), root mean square error of approximation (RMSEA), and standard root mean square residual (SRMR), interpreted based on criteria outlined by Hu and Bentler (60). Mediation of the effect of abuse or family conflict on maternal postpartum weight by partner support or depressive symptoms was tested by examining the statistical significance of the indirect paths using the multivariate delta method (61–62).
Results
Preliminary analyses
Rates of obesity
Across the sample, BMI means ranged from 29.1–29.9 in the 2 years following childbirth. These means are comparable to BMI means for Mexican American women in other samples (e.g., 7). Analyses examined whether women met criteria for overweight (BMI ≥ 25.0), obese (BMI ≥ 30), or morbid obesity (BMI ≥ 40) categories at any of the time points. Eighty-one percent of mothers were overweight, 47.5% were obese, and 8.7% met criteria for morbid obesity at one or more measurement points. When only maternal weight in the 2nd postpartum year was considered, 76.5% were overweight, 44.9% were obese, and 8.5% met criteria for morbid obesity. The rates of obesity at 2 years postpartum in our sample parallel rates for non-pregnant Mexican American women (age adjusted ≥ 20 = 44.9%) reported in 2014 by Ogden et al. (5).
Predictors of postpartum weight
Childhood variables were positively correlated with maternal BMI at most time points (see Table 2). Although primary analyses focus on total exposure to abuse, results of exploratory analyses of abuse subtypes suggest that emotional abuse has the strongest correlations to maternal BMI at 1 year (r = .187, p = .007), 18 months (r = .142, p = .055), and 2 years (r .164, p = .019); physical and sexual abuse were not significantly correlated with maternal BMI at any time point (all p’s > .18). Regression analyses adjusting for age, country of birth, breastfeeding, and number of children revealed that abuse (total scale) predicted BMI at 18 months (β = .16, p = .046) and 24 months (β = .13, p = .051). After the same adjustments, family conflict predicted BMI at 6 weeks (β = .45, p = .04), 24 weeks (β = .89, p = .009), 12 months (β = .60, p = .035), 18 months (β = .64, p = .029), and 24 months (β = .59, p = .019) postpartum.
Postpartum depressive symptoms were positively correlated with BMI at all time points except 18 weeks. After adjusting for covariates, depressive symptoms remained a significant predictor of BMI at 12 weeks (β = .18, p = .033), 12 months (β = .36, p = .002), 18 months (β = .29, p = .019), and 24 months (β = .29, p = .004). Partner support was not significantly correlated with BMI at any time point.
Weight change across the first postpartum year
Childhood abuse
A model predicting the BMI intercept and slope from abuse, depressive symptoms, and partner support showed good fit, χ2 (32) = 56.6, p = .005, CFI = .991, RMSEA = .049 {90%CI = .027, .069}, SRMR = .013 (see Figure 1). Higher abuse was associated with less partner support (p < .001) and higher depressive symptoms (p < .001). Depressive symptoms were positively associated with the intercept (p = .050), but not the slope (p = .85). Neither the total effect of abuse on the intercept (p = .27) nor the indirect effect through depressive symptoms (p = .062) was statistically significant. Partner support predicted the slope (p = .016) but not the intercept (p = .99). The total effect of abuse on the slope was not statistically significant (p = .18) but the indirect path through partner support was statistically significant (β = .049, SE=.022, p = .031).
Family conflict
Maternal BMI intercept and slope were predicted from family conflict, depressive symptoms, partner support, and covariates. Model fit was good, χ2 (32) = 56.5, p = .005, CFI = .991, RMSEA = .049 {90%CI = .027, .069}, SRMR = .013. Higher conflict was associated with less partner support (p = .001), higher depressive symptoms (p < .001), higher weight intercept (p = .037) and an increasing slope (p = .021). Partner support was a statistically significant predictor of the slope (p = .028), but not the intercept (p = .79). Depressive symptoms did not predict the intercept (p = .072) or the slope (p = .72).
The total effect of conflict on the intercept (p = .014) and the slope (p = .006) were both statistically significant. For display purposes, the direct effects of conflict on weight intercept and slope are displayed in Figure 3, dichotomized to reflect conflict above and below the sample mean. The indirect effects from conflict to the intercept (p = .10) and the slope (p = .72) through depressive symptoms were not statistically significant. The indirect effect from conflict to the intercept through partner support was not significant (p = .79); the indirect effect to the slope through partner support neared statistical significance (β = .031, SE=.017, p = .065).
Figure 3.
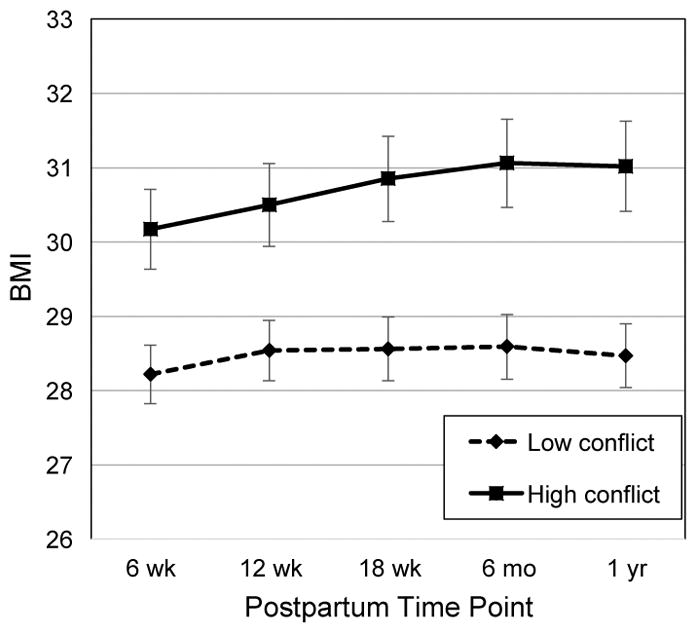
Estimated means of postpartum BMI in the first postpartum year by childhood family conflict.
BMI = body mass index (kg/m2); “Low conflict” = childhood family conflict < sample mean; “High conflict” = childhood family conflict > sample mean. “wk” = weeks; “mo” = months; “yr” = year. Error bars are standard errors.
Weight in the second postpartum year
Childhood abuse
Analyses evaluated maternal BMI in the 2nd year after giving birth (see Figure 2). For childhood abuse, model fit was good, χ2 (15) = 19.9, p = .18, CFI = .995, RMSEA = .034 {90% CI = .00, .069}, SRMR = .014. Higher postpartum depressive symptoms predicted higher maternal BMI (p = .001), but partner support did not (p = .47). Although the total effect from abuse to BMI was not statistically significant (p = .20), the indirect effect from abuse to BMI through depressive symptoms was statistically significant (β = .066, SE=.023, p = .005).
Family conflict
For family conflict, model fit was good, χ2 (15) = 19.7, p = .18, CFI = .995, RMSEA = .033 {90% CI = .00, .069}, SRMR = .014. Higher conflict predicted higher BMI (p = .012). Higher postpartum depressive symptoms also predicted higher BMI (p = .001). Both the total effect from conflict to BMI (β = .184, SE=.06, p = .003) and the indirect effect from conflict to BMI through depressive symptoms (β = .038, SE=.017, p = .021) were statistically significant.
We also conducted ancillary analyses examining an alternative model in which abuse and conflict were considered in the same model. The model fit remained good for both the 1st and 2nd postpartum years. In the 1st year, the indirect effect of abuse on BMI slope in the first year via partner support was no longer statistically significance (p = .056). In the 2nd year, the indirect effect of abuse on BMI in the 2nd year via depressive symptoms remained statistically significant (p = .011) and the direct effect of conflict on BMI also remained statistically significant (p = .008) but the indirect effect of conflict through depressive symptoms was no longer statistically significant (p = .63) in these alternative models.
Discussion
Pregnancy and the birth of a child are high risk times for weight gain that persists long after the birth. Hispanic women are at elevated risk of obesity and related health problems, and identifying predictors of postpartum weight in this population is critical for targeted obesity programs. The current study evaluated the relation of childhood family adversity to maternal postpartum weight in a sample of low-income Mexican-origin women. Our results suggest that self-reported childhood abuse or high family conflict is associated with increasing weight and greater obesity risk in the postpartum period. Abuse and family conflict also predicted elevated postpartum depressive symptoms and lower partner support, each of which played a role in explaining the process by which childhood adversity influences obesity risk in this population.
Self-reported abuse before the age of 18 predicted maternal BMI at 18 and 24 months after the birth, but was not directly associated with weight or weight change in the first postpartum year. Exploratory analyses suggest that emotional abuse may be a stronger predictor than physical or sexual abuse of BMI in the 2nd year, however these results should be interpreted with caution due to their exploratory nature and the low incidence of reported sexual abuse in this sample. Higher exposure to family conflict predicted maternal BMI at all time periods except for 12 and 18 weeks postpartum, and predicted an increasing BMI slope across the first postpartum year and higher BMI in the first and second postpartum years. Although abuse and conflict were significantly correlated (r = .56), exposure to conflict was a more consistent predictor of postpartum weight and weight gain. For women reporting family conflict 1 SD higher than the mean, this amounted to approximately 4 pounds of weight gain in the first postpartum year. Items assessing family conflict reflect less extreme adversity than the abuse measure, and scores were more normally distributed. Although abuse is frequently the focus of research, these results suggest that childhood family adversity within a more normative range of experience may also exert a significant influence on adult obesity risk.
There are several pathways through which adverse childhood experiences could influence women’s weight and postpartum weight trajectory. The current study evaluated postpartum depressive symptoms and partner support as mediators. Strong evidence documents that women abused in childhood are more vulnerable to depression in adulthood (32–33), and postpartum depression has been linked to postpartum weight retention (25–26). We found that childhood abuse and family conflict were each associated with higher postpartum depressive symptoms, and depressive symptoms predicted women’s weight in the first two postpartum years, partially mediating the associations of childhood abuse with maternal weight in the second postpartum year. Depressive symptoms were not, however, associated with the slope of weight gain or loss in the first year. In short, depressive symptomatology appears to directly affect women’s weight level without affecting the trajectory of postpartum weight change.
Women’s reported support from their partner six weeks after childbirth was also evaluated as a mediator. Considerable research documents lasting interpersonal difficulties that can result from adverse family-of-origin relationships. Adults abused as children may lack skills to develop and maintain healthy relationships, or may experience a continuation of abuse in their intimate relationships (31–32, 41–43). Following the birth of a baby, supportive relationships can improve adherence to healthy diet and exercise (51); the lack of support may exert the opposite effect, challenging efforts to obtain or maintain a healthy weight. Relatively high levels of partner support were reported by women in the current study, consistent with cultural values of familism in low-acculturated Mexican-origin families. However, more frequent childhood abuse and higher family conflict were each associated with lower partner support, and lower partner support was associated with increasing postpartum weight, partially mediating the effect of childhood abuse on postpartum weight gain. Partner support, however, was not significantly associated with the level of maternal weight at any time point. In contrast to depressive symptomatology, partner support may not directly predict maternal weight, but may instead influence the process of weight gain/loss after the birth of a baby.
The current analyses only evaluated potential mediators in the postpartum period, but experiences prior to pregnancy likely influence the relations of childhood abuse and family conflict to maternal weight, potentially forming a chain of mediators across development. In the short-term, children in abusive family environments are at risk of developmental delays, externalizing problems, and internalizing problems (31). Affective distress in childhood may precede and predict depression in adulthood, and may also influence weight gain in childhood and pre-pregnancy (63–64). Similarly, developmental delays are associated with problematic social relationships (65) as well as overweight and obesity (66).
There are limitations to the conclusions that can be drawn from these analyses. First, because pre-pregnancy and pregnancy weight measures were not available, we could not evaluate gestational weight gain or retention of weight gained during pregnancy. If related to abuse or conflict, gestational weight gain may mediate their impact on postpartum weight. Because most women in the study (78%) were not first-time mothers, a “true” baseline weight would be difficult to assess; instead, statistical analyses adjusted for maternal age and number of children. Second, all participants were low-income and of Mexican origin. The results may not generalize to higher SES women or those from other ethnic groups. Third, childhood abuse and family conflict were assessed by retrospective report, raising potential concerns about recall biases. The CTQ is a well-validated measure (67), and measurement error from retrospective reports has minimal impact on estimates in models of the long-term consequences of childhood adversity (68). A recent meta-analysis found statistically significant relations of childhood maltreatment to adult obesity whether abuse was assessed retrospectively or prospectively (16). Similarly, da Silva & da Costa Maia (69) found that retrospective reports of childhood adversity were stable longitudinally among obese adults, and were not associated with symptoms of psychopathology. Nonetheless, the study would be strengthened by objective or prospective measures of childhood experiences. Finally, although the study is longitudinal, causal conclusions assume adequate measurement of all possible confounding variables. There may be unmeasured confounds (e.g., genetic or environmental) in the relation between reported childhood experiences and postpartum weight status.
Despite these limitations, the current investigation provides insight into pathways through which abuse and family conflict during childhood can increase risk for overweight, obesity, and unhealthy patterns of weight change during the postpartum period. Among low-income Mexican-origin women, self-reported childhood abuse and family conflict were associated with increasing weight and greater risk of obesity in the first two postpartum years. Childhood abuse and conflict also predicted elevated postpartum depressive symptoms and lower postpartum partner support, both of which influenced obesity risk and postpartum weight gain and loss. Depressive symptoms and partner support may present modifiable targets for health promoting efforts among this high-risk population.
Acknowledgments
Source of Funding: The study was funded by the National Institute of Mental Health (R01 MH083173-01). The funding source had no role in study design, collection, analysis, interpretation, or writing of the report; or in the decision to submit the article for publication.
Abbreviations
- BMI
Body mass index
- SES
Socioeconomic status
- SD
Standard deviation
- CFI
Comparative Fit Index
- RMSEA
Root Mean Square Error of Approximation
- SRMR
Standardized Root Mean Square Residual
- CI
Confidence Interval
Footnotes
Conflicts of Interest
The authors have no conflicts of interest, financial or otherwise.
References
- 1.Shonkoff JP, Boyce W, McEwen BS. Neuroscience, molecular biology, and the childhood roots of health disparities: Building a new framework for health promotion and disease prevention. JAMA. 2009;301(21):2252–2259. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 2.Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. Plos Med. 2009;6(4):365. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Managing overweight and obesity in adults: Systematic evidence review from the Obesity Expert Panel. National Institutes of Health Web site. 2013 https://www.nhlbi.nih.gov/sites/www.nhlbi.nih.gov/files/obesity-evidence-review.pdf.
- 4.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in adults: United States 1988–1994 and 2005–2008. Hyattsville, MD: National Center for Health Statistics; 2010. NCHS data brief no 50. [Google Scholar]
- 7.Gallo LC, Fortmann AL, de low Monteros KE, Mills PJ, Barrett-Connor E, Roesch SC, Matthews KA. Individual and neighborhood socioeconomic status and inflammation in Mexican-American women: What is the role of obesity? Psychosom Med. 2012;74(5):535. doi: 10.1097/PSY.0b013e31824f5f6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laitinen J, Power C, Järvelin MR. Family social class, maternal body mass index, childhood body mass index, and age at menarche as predictors of adult obesity. Am J Clin Nut. 2001;74(3):287–294. doi: 10.1093/ajcn/74.3.287. [DOI] [PubMed] [Google Scholar]
- 9.Oken E. Maternal and child obesity: the causal link. Obstet Gyn Clin N Am. 2009;36(2):361–377. doi: 10.1016/j.ogc.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 10.Chartier MJ, Walker JR, Naimark B. Health risk behaviors and mental health problems as mediators of the relationship between childhood abuse and adult health. Am J Public Health. 2009;99(5):847–854. doi: 10.2105/AJPH.2007.122408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Noll JG, Zeller MH, Trickett PK, Putnam FW. Obesity risk for female victims of childhood sexual abuse: A prospective study. Pediatrics. 2007;120:61–67. doi: 10.1542/peds.2006-3058. [DOI] [PubMed] [Google Scholar]
- 12.Springer KW. Childhood physical abuse and midlife physical health: Testing a multi-pathway life course model. Soc Sci Med. 2009;69(1):138–146. doi: 10.1016/j.socscimed.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas C, Hyppönen E, Power C. Obesity and type 2 diabetes risk in midadult life: the role of childhood adversity. Pediatrics. 2008;121(5):e1240–e1249. doi: 10.1542/peds.2007-2403. [DOI] [PubMed] [Google Scholar]
- 14.Dube SR, Cook ML, Edwards VJ. Health-related outcomes of adverse childhood experiences in Texas, 2002. Prev Chronic Dis. 2010;7(3):1–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Richardson AS, Dietz WH, Gordon-Larsen P. The association between childhood sexual and physical abuse with incident adult severe obesity across 13 years of the National Longitudinal Study of Adolescent Health. Pediatr Obesity. 2013;9:351–361. doi: 10.1111/j.2047-6310.2013.00196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Danese A, Tan M. Childhood maltreatment and obesity: systematic review and meta-analysis. Mol Psychiatr. 2014;19:544–554. doi: 10.1038/mp.2013.54. [DOI] [PubMed] [Google Scholar]
- 17.Sumner SA, Mercy JA, Dahlberg LL, Hillis SD, Klevens J, Houry D. Violence in the United States. Status, Challenges, and Opportunities. JAMA. 2015;314(5):478–488. doi: 10.1001/jama.2015.8371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wildeman C, Emanuel N, Leventhal JM, Putnam-Hornstein E, Waldfogel J, Lee H. The prevalence of confirmed maltreatment among US children, 2004–2011. JAMA Pediatr. 2014;168(8):706–713. doi: 10.1001/jamapediatrics.2014.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Putnam-Hornstein E, Needell B, King B, Johnson-Motoyama M. Racial and ethnic disparities: A population-based examination of risk factors for involvement with child protective services. Child Abuse Negl. 2013;37(1):33–46. doi: 10.1016/j.chiabu.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Hussey JM, Chang JJ, Kotch JB. Childhood maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118(3):933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- 21.Gore SA, Brown DM, Smith West D. The role of postpartum weight retention in obesity among women: A Review of the Evidence. Ann Behav Med. 2003;26:149–159. doi: 10.1207/S15324796ABM2602_07. [DOI] [PubMed] [Google Scholar]
- 22.Linné Y, Dye L, Barkeling B, Rössner S. Long-term weight development in women: A 15-year follow-up of the effects of pregnancy. Obes Res. 2004;12(7):1166–1178. doi: 10.1038/oby.2004.146. [DOI] [PubMed] [Google Scholar]
- 23.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidemiol Rev. 2000;22:261–274. doi: 10.1093/oxfordjournals.epirev.a018038. [DOI] [PubMed] [Google Scholar]
- 24.Walker LO, Freeland-Graves JH, Milani T, Hanss-Nuss H, George G, Sterling BS, Kim M, Timmerman GM, Wilkinson S, Arheart KL, Stuifbergen A. Weight and behavioral and psychosocial factors among ethnically diverse, low-income women after childbirth: I. Methods and Context. Women Health. 2004;4(2):1–17. doi: 10.1300/J013v40n02_01. [DOI] [PubMed] [Google Scholar]
- 25.Walker LO. Weight and weight-related distress after childbirth: relationships to stress, social support, and depressive symptoms. J Holist Nurs. 1997;15(4):389–405. doi: 10.1177/089801019701500406. [DOI] [PubMed] [Google Scholar]
- 26.Pedersen P, Baker JL, Henriksen TB, Lissner L, Heitmann BL, Sorensen TI, Nohr EA. Influence of psychosocial factors on postpartum weight retention. Obesity. 2011;19(3):639–646. doi: 10.1038/oby.2010.175. [DOI] [PubMed] [Google Scholar]
- 27.Sterling BS, Fowles ER, Garcia AA, Jenkins SK, Wilkinson S, Kim M, Kim S, Latimer L, Walker LO. Altered perceptions of personal control about retained weight and depressive symptoms in low-income postpartum women. J Comm Health Nurs. 2009;26(3):143–157. doi: 10.1080/07370010903034524. [DOI] [PubMed] [Google Scholar]
- 28.Births: Final data for 2013. Centers for Disease Control Web site; http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf. [PubMed] [Google Scholar]
- 29.Macartney S, Bishaw A, Fontenot K. US Census Bureau, 2007–2011 American Community Survey. Poverty rates for selected detailed race and Hispanic groups by state and place: 2007–2011; pp. 1–20. [Google Scholar]
- 30.Ranchod YK, Headen IE, Petito LC, Deardorff JK, Rehkopf DH, Abrams BF. Maternal childhood adversity, prepregnancy obesity, and gestational weight gain. Am J Prev Med. 2015;50(4):463–469. doi: 10.1016/j.amepre.2015.08.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malinosky-Rummell R, Hansen DJ. Long-term consequences of childhood physical abuse. Psychol Bull. 1993;114:68–79. doi: 10.1037/0033-2909.114.1.68. [DOI] [PubMed] [Google Scholar]
- 32.Colman RA, Widom CS. Childhood abuse and neglect and adult intimate relationships: A prospective study. Child Abuse Negl. 2004;28(11):1133–1151. doi: 10.1016/j.chiabu.2004.02.005. [DOI] [PubMed] [Google Scholar]
- 33.MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Duku EK, Walsh CA, Wong MYY, Beardslee WR. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiat. 2014;158(11):1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- 34.Frias-Armenta M. Long-term effects of child punishment on Mexican women: a structural model. Child Abuse Negl. 2002;26:371–386. doi: 10.1016/s0145-2134(02)00314-9. [DOI] [PubMed] [Google Scholar]
- 35.Alvarez-Segura M, Garcia-Esteve L, Torres A, Plaza A, Imaz ML, Hermida-Barros L, San L, Burtchen N. Are women with a history of abuse more vulnerable to perinatal depressive symptoms? A systematic review. Arch Women Ment Hlth. 2014;17:343–357. doi: 10.1007/s00737-014-0440-9. [DOI] [PubMed] [Google Scholar]
- 36.Liu CH, Tronick E. Rates and predictors of postpartum depression by race and ethnicity: Results from the 2004 to 2007 New York City PRAMS survey (Pregnancy Risk Assessment Monitoring System) Matern Child Healt J. 2013;17(9):1599–1610. doi: 10.1007/s10995-012-1171-z. [DOI] [PubMed] [Google Scholar]
- 37.deWit L, Luppino F, va Straten A, Penninx B, Zitman F, Cuijpers P. Depression and obesity: A meta-analysis of community-based studies. Psychiatry Res. 2010;178:230–235. doi: 10.1016/j.psychres.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 38.Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke OI, Lucas M, Manson JE, Ascherio A, Hu FB. Bidirectional associations between depression and obesity in middle-aged and older women. Int J Obes. 2012;36(4):595–602. doi: 10.1038/ijo.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goldstein ND, Rogers S, Ehrenthal DB. The impact of psychosocial stressors on postpartum weight retention. Arch Womens Ment Health. doi: 10.1007/s00737-016-0613-9. published online 24 February 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Whitaker K, Young-Hyman D, Vernon M, Wilcox S. Maternal stress predicts postpartum weight retention. Matern Child Health J. 2014;18:2209–2217. doi: 10.1007/s10995-014-1470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cyr C, Euser EM, Bakermans-Kranenburg MJ, Van Ijzendoorn MH. Attachment security and disorganization in maltreating and high-risk families: A series of meta-analyses. Dev Psychopathol. 2010;22(01):87–108. doi: 10.1017/S0954579409990289. [DOI] [PubMed] [Google Scholar]
- 42.Muller RT, Gragtmans K, Baker R. Childhood physical abuse, attachment, and adult social support: Test of a mediational model. Can J Beh Sci. 2008;40(2):80. [Google Scholar]
- 43.Varia R, Abidin RR, Dass P. Perceptions of abuse: Effects on adult psychological and social adjustment. Child Abuse Negl. 1996;20(6):511–526. doi: 10.1016/0145-2134(96)00033-6. [DOI] [PubMed] [Google Scholar]
- 44.Riggs SA, Cusimano AM, Benson KM. Childhood emotional abuse and attachment processes in the dyadic adjustment of dating couples. J Couns Psychol. 2011;58(1):126–138. doi: 10.1037/a0021319. [DOI] [PubMed] [Google Scholar]
- 45.DiLillo D, Lewis T, Loreto-Colgan AD. Child maltreatment history and subsequent romantic relationships: Exploring a psychological route to dyadic difficulties. J Aggress Maltreat Trauma. 2007;15(1):19–36. [Google Scholar]
- 46.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1998;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 47.Beck CT. Predictors of postpartum depression: an update. Nurs Res. 2001;50(5):275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 48.Diaz MA, Le H, Cooper BA, Muñoz RF. Interpersonal factors and perinatal depressive symptomatology in a low-income Latina sample. Cult Divers Ethn Min. 2007;13:328–336. doi: 10.1037/1099-9809.13.4.328. [DOI] [PubMed] [Google Scholar]
- 49.Evenson KR, Aytur SA, Borodulin K. Physical activity beliefs, barriers, and enablers among postpartum women. J Womens Health. 2009;18(12):1925–1934. doi: 10.1089/jwh.2008.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lambert L, Raidl M, Safaii S, Conner C, Geary EJ, Ault S. Perceived benefits and barriers related to postpartum weight loss of overweight/obese postpartum WIC participants. Top Clin Nutr. 2005;20(1):16–27. [Google Scholar]
- 51.Shah MK, Kieffer EC, Choi H, Schumann C, Heisler M. Mediators and moderators of the effectiveness of a community health worker intervention that improved dietary outcomes in pregnant Latino women. Health Educ Behav. 2015;42(5):593–603. doi: 10.1177/1090198114568307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 53.Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Psy. 1997;36(3):340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 54.Moos RH, Moos BS. Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press; 1994. [Google Scholar]
- 55.Gress-Smith JL, Roubinov DS, Tanaka R, Crnic K, Gonzales N. Prenatal expectations in Mexican American women: Development of a culturally sensitive measure. Arch Women Ment Hlth. 2013;16(4):303–314. doi: 10.1007/s00737-013-0350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Brit J Psychiat. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 57.Garcia-Esteve L, Ascaso C, Ojuel J, Navarro P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in Spanish mothers. J Affect Disord. 2003;75(1):71–76. doi: 10.1016/s0165-0327(02)00020-4. [DOI] [PubMed] [Google Scholar]
- 58.Reiter JP, Raghunathan TE. The multiple adaptations of multiple imputation. J Am Stat Assoc. 2007;102(480):1462–1471. [Google Scholar]
- 59.Østbye T, Peterson BL, Krause KM, Swamy GK, Lovelady CA. Predictors of postpartum weight change among overweight and obese women: Results from the Active Mothers Postpartum Study. J Womens Health. 2012;21(2):215–222. doi: 10.1089/jwh.2011.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. [Google Scholar]
- 61.MacKinnon DP. Introduction to statistical mediation analysis. NY: Erlbaum; 2008. [Google Scholar]
- 62.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982;13(1):290–312. [Google Scholar]
- 63.Suglia SF, Duarte CS, Chambers CC, Boyton-Jarrett R. Social and behavioral risk factors for obesity in early childhood. J Dev Behav Pediatr. 2013;34(8):549–556. doi: 10.1097/DBP.0b013e3182a509c0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xie B, Ishibashi K, Lin C, Peterson DV, Susman EJ. Overweight trajectories and psychosocial adjustment among adolescents. Prev Med. 2013;57:847–853. doi: 10.1016/j.ypmed.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Guralnick MJ. Early intervention approaches to enhance the peer-related social competence of young children with developmental delays. Infant Young Child. 2010;23:73–83. doi: 10.1097/IYC.0b013e3181d22e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Emerson E. Overweight and obesity in 3-and 5-year-old children with and without developmental delay. Public Health. 2009;123(2):130–133. doi: 10.1016/j.puhe.2008.10.020. [DOI] [PubMed] [Google Scholar]
- 67.Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- 68.Fergusson DM, Horwood LJ, Boden JM. Structural equation modeling of repeated retrospective reports of childhood maltreatment. Int J Meth Psych Res. 2011;20:93–104. doi: 10.1002/mpr.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.da Silva SSP, da Costa Maia Â. The stability of self-reported adverse experiences in childhood: A longitudinal study on obesity. J Interpers Violence. 2013;28(10):1989–2004. doi: 10.1177/0886260512471077. [DOI] [PubMed] [Google Scholar]