Abstract
Objective
We tested the hypothesis that socioeconomic status (SES) would predict children’s physical health problems at the end of kindergarten among children whose parent reported greater parent-child relationship (PCR) negativity and/or who exhibited greater parasympathetic (RSA) reactivity. We also tested whether RSA and PCR negativity mediated the SES-health association.
Methods
Data were collected from 338 kindergarten children (M age = 5.32 years; SD = .32) and their primary caregivers (87% biological mothers) during the fall and subsequent spring of kindergarten. In the fall, parents reported on income and education level (SES) and PCR negativity, and RSA reactivity was assessed via a standardized challenge protocol for young children. In the fall and subsequent spring, parents reported on children’s chronic medical conditions and physical health impairments. Multivariate regression was conducted within a structural equation modeling framework to test hypotheses.
Results
Significant interactions were found between SES and PCR negativity (b = −.074, p = .035) and between SES and RSA reactivity (b = .169, p = .019) as predicts children’s spring health impairment, adjusting for health in the preceding fall. Lower SES was associated with greater health impairment among children whose parents reported more PCR negativity (b = −.110, p = .024) and children who showed greater RSA reactivity (b = −.106, p = .011). SES was unrelated to physical health at low PCR negativity or RSA reactivity. Mediation models were not supported.
Conclusion
Parent-child relationship quality and individual differences in stress reactivity may modulate the influence of SES on physical health in childhood.
As aptly summarized by Shonkoff and colleagues, “adult disease prevention begins with reducing early toxic stress” (1) (p. 2256). Socioeconomic adversity in childhood is a particularly powerful form of early life stress that contributes to poor global physical health and greater health-related impairment throughout the lifespan (2–5). Illustratively, lower socioeconomic status (SES) is associated with greater rates of respiratory illness, obesity, and cardiovascular conditions in childhood and adolescence and greater morbidity and mortality in adulthood (6–8). Despite national public health campaigns to reduce health disparities (e.g., Healthy People 2010), a strong, inverse association between SES and physical health continues (9).
The negative association between SES and physical health is found across the entire range of the socioeconomic continuum in adulthood (10). Robust evidence for these social disparities in health at the population level may mask important variation at the individual level. Inconsistent findings have been observed in regard to the steepness of the gradient across childhood (9), raising questions about individual differences that may determine which children are most likely to show poor health in the context of low SES. Indeed, the identification of moderators is essential for early determination of risk as well as the design of well-targeted interventions tailored to those most likely to benefit. It has also been suggested that the origins of SES-related health issues may be traced to developmental processes that are compromised early in life (11). As such, identifying explanatory mechanisms that mediate the negative effects of SES on physical health at a young age would improve understanding of how adversity becomes biologically embedded to affect health (12). Surprisingly few investigations into the link between SES and physical health outcomes have focused on the first five years of life, and even fewer have examined putative moderators or mediators of this association in childhood. This may be partially explained by a reliance on cross-sectional designs; prospective investigations are better suited to examine how risk factors work together to produce disorder (13). The current study addresses this gap by examining under what conditions (i.e., moderation) and how (i.e., mediation) SES is associated with changes in young children’s physical health.
The quality of the parent-child relationship is one of the most critical influences on health early in life and represents an important, micro-level dimension of the larger social ecology within which children develop. Socioeconomic adversity may be more likely to “get under the skin” and increase physical health problems in children whose relationship with a primary caregiver is compromised by negativity. There is some evidence that maternal sensitivity can buffer the effects of poverty on adult health (14). However, research evaluating the role of parent-child relationship quality in the association between SES and children’s physical health is limited (15), most likely due to an assumed divide between the socioemotional lives of children and their biomedical well-being. Lower quality parenting has been shown prospectively to predict poorer health among offspring during early childhood (16). Few if any investigations have examined the potential for parent-child relationship quality to moderate the link between SES and physical health in early childhood. This gap is notable given that, for young children, their perceptions of stressful circumstances are largely filtered through the parent-child relationship, with children relying on their parent to signal when there is threat or stress in the environment. Conflict or negativity in this relationship is likely to exacerbate a child’s vulnerability to the negative effects of economic adversity. Alternatively, parenting practices have been described as “socially patterned”, and as such, parent-child relationship quality may also mediate the association between SES and physical health (6).
Developmental models of vulnerability to stress have long emphasized the importance of individual physiological reactivity and regulation in the development of psychopathology (17). A burgeoning body of literature suggests that high physiological reactivity to stress may signal heightened susceptibility to environmental influences (11,18). For example, multiple researchers have reported that high physiological reactivity to stress increases vulnerability to maladjustment among children exposed to family stress (19,20). These studies focused on changes in heart rate variability (HRV), or rapid changes in the beat-to-beat timing of systole. Although both sympathetic and parasympathetic branches of the ANS influence HRV, psychophysiological theories of HRV emphasize the role of respiratory sinus arrhythmia (RSA) in emotion regulation (21). RSA, the oscillation in heart rate produced by the respiratory cycle, indexes parasympathetically-mediated HRV. During a challenging task, RSA decreases (parasympathetic withdrawal), and the magnitude of this decrease reflects reactivity to the task. Several investigations have found that physiological reactivity moderates the association between quality of the family environment and physical health (22,23), and that reactivity may play a similarly sensitizing in the prediction of physical health in the context of socioeconomic adversity. Alternatively, adversity-induced alterations in biological systems may play a mechanistic, explanatory role in the SES-health connection such that physiological reactivity mediates the relation between SES and physical health (24). Evan’s and Kim’s finding that greater durations of poverty in childhood predicted blunted blood pressure responses during adolescence provides some evidence in support of such early life biological embedding of SES-related stress (25), but additional work is needed in this area, particularly with longitudinal designs (26).
In sum, much remains to be learned about the prospective effects of low SES on children’s physical health in early childhood and under what conditions or by which pathways these effects are most likely to occur. Comprehensively addressing such questions is best achieved by examining risk and explanatory factors that exist at multiple levels and across physiological and socioemotional domains (27). It is important to consider the temporal order of variables when developing hypotheses of moderation and mediation (13). The pattern of relations between socioeconomic factors, family environment, and children’s health are likely to be complex and transactional, making several different orderings of relations among SES, parent-child relationship quality, and children’s stress reactivity plausible. Our primary hypothesis was that parent-child relationship quality and children’s parasympathetic reactivity would each moderate the association between SES and children’s physical health. Given the importance of examining the longer-term effects of SES across children’s transition to kindergarten, we predicted that this finding would be present for children’s physical health in the spring, adjusting for physical health in the preceding fall. Inclusion of children’s baseline physical health at the beginning of the school year allows for potential conclusions to be drawn regarding the prospective effects of SES, rather than its correlates. Specifically, we expected that low SES would predict significantly poorer health in the spring among children whose parent reported high negativity in the parent-child relationship and who exhibited elevated physiological reactivity to stress in the preceding fall. Although evidence in young children is limited, in light of the advancing theories of allostatic load and biological embedding, as well as evidence that parenting can be affected by SES, we also examined whether parasympathetic reactivity and parent-child relationship quality mediated the association between SES in the fall and physical health in the subsequent spring.
Methods
Participants
The current study comprised 338 children (163 females, 175 males) who participated in a longitudinal study of social status, biological responses to adversity, and child mental and physical health. Participants were recruited in three waves from 29 kindergarten classrooms within six public schools in the San Francisco Bay Area (Oakland, Albany, and Piedmont Unified school districts) during the fall seasons of 2003, 2004, and 2005. The schools were selected to represent the sociodemographic and racial/ethnic characteristics of the metropolitan area. Families were recruited through home mailings, presentations at kindergarten parents’ welcome nights, and in-person recruitment during school drop-off and pick-up times. Although every family with a child in a participating classroom was invited to take part in the study, families who were not fluent in either English or Spanish were excluded to ensure adequate comprehension of study questionnaires. Schools were provided with $20 per child enrolled in the study.
Participant characteristics are displayed in Table 1. The mean age of the children at the kindergarten entry was 5.32 years (SD = 0.32, range = 4.75–6.28). The sample was racially and ethnically diverse, and among families that provided demographic information (n = 322), children were identified as 19% African American, 11% Asian, 43% European or White, 4% Latino, 22% multiethnic, and 2% as “other” race/ethnicity. Primary caregivers were 87% biological mothers, 9% biological fathers, 2.5% adoptive mothers, 0.6% biological grandmothers, and 0.9% “other” relations. As the vast majority of primary caregivers were parents, these terms are used interchangeably here.
Table 1.
Participant Characteristics
| Sex | |
| Female | 163 (48%) |
| Male | 175 (52%) |
| Participant Age (M, SD); range = 4.75–6.28 | 5.32 (SD = .32) |
| Ethnicity (n = 322) | |
| White, non-Hispanic | 43% |
| Hispanic/Latino | 4% |
| Black/African-American | 19% |
| Asian | 11% |
| Multiethnic/Multiracial | 22% |
| Other | 2% |
| Family Income (n = 322) | |
| Less than $10,000 | 13 (4%) |
| $10,000 – $14,999 | 8 (3%) |
| $15,000 – $19,999 | 7 (2%) |
| $20,000 – $29,999 | 15 (5%) |
| $30,000 – $39,999 | 22 (7%) |
| $40,000 – $49,999 | 15 (5%) |
| $50,000 – $59,999 | 16 (5%) |
| $60,000 – $79,999 | 40 (13%) |
| $80,000 – $99,999 | 50 (16%) |
| >$100,000 | 125 (40%) |
| Highest education level completed in household (n = 322) | |
| Less than high school | 8 (2%) |
| High school | 18 (6%) |
| Some college or 2-year degree | 55 (17%) |
| 4-year college graduate | 57 (18%) |
| Some graduate or professional school beyond college | 39 (12%) |
| Professional or graduate degree | 145 (45%) |
Procedures
Data for this study were collected in the fall (T1) and spring (T2) during the kindergarten year. Parents’ informed consent and children’s assent were obtained prior to the start of data collection. Parental reports of parental education, family income, parent-child relationship negativity, and children’s physical health were collected through an extensive series of home mailings, and families were compensated with $50 for each completed time point. In addition, children participated in a 20-minute, in-school reactivity protocol during which time their autonomic activity was assessed.
Measures
Socioeconomic status (SES)
Assessing multiple dimensions of SES allows for greater understanding of how social determinants contribute to an outcome under study, thus we assessed both family income and education. Total household annual income, including all sources, was assessed on an 11-point scale that ranged from < $10,000 to > $200,000 (Mean = $60,000–79,999; Median = $80,000–99,999). Highest level of educational attainment for any caregiver in the household was assessed using a 6-point scale that ranged from less than a high school diploma to a professional or graduate degree, with 75% of caregivers having at least a college degree, a level commensurate with the surrounding community. See also Table 1. SES was calculated as the average of standardized highest household education of adults in the home and standardized total annual household income.
Negativity in the Parent-Child Relationship
The quality of the parent-child relationship was assessed using three items from the Child-Rearing Practices Report (28), which were rated on a scale from 1 (extremely true) to 7 (extremely untrue). Items were: “I often feel angry with my child,” “There is a good deal of conflict between my child and me,” and “I feel that my child is a bit of a disappointment to me”. These items have been used together in numerous prior studies to capture parent-child relationship negativity and have shown the expected associations with multiple aspects of child functioning (29–32). The items were reverse-scored and averaged to create a composite of negativity in the parent-child relationship, with higher scores indicating greater negativity in the parent-child relationship. Internal consistency was low (α = 0.59) but reasonable given the small number of items (33).
Respiratory sinus arrhythmia (RSA) reactivity
Children’s autonomic reactivity was assessed by computing changes in RSA (34) during a developmentally challenging reactivity protocol. This kindergarten “stress reactivity” protocol is detailed extensively elsewhere (29,35) and only briefly summarized here. Following a 2-minute baseline period during which the experimenter read a calming story aloud, children were challenged with four age-appropriate tasks designed to elicit moderate stress responses to social, cognitive, sensory, and emotional challenges (22). In order to measure the psychophysiological response to the four challenges without confounding by motor activity, each challenge task in the reactivity protocol was preceded by a non-challenging “control task” that paralleled the motor and engagement demands of the corresponding challenge task (35). The challenge tasks included a structured interview (social challenge), a digit span recitation task (cognitive challenge), taste identification (sensory challenge), and watching an emotion-evoking movie clip (emotional challenge).
After the child was familiar with the equipment, four spot electrodes were placed in the standard tetrapolar configuration on the child’s neck and chest, and ECG electrodes were placed on the right clavicle and lower left rib. A 4 mA AC current at 100 kHz was passed through the two current electrodes. RSA was monitored continuously during the protocol. Data were acquired using the Biopac MP150 (Biopac Systems, Santa Barbara, CA) interfaced to a PC-based computer. Analog data were continuously monitored on the computer for signal and noise, and digitized data were stored for offline analysis. RSA was derived in accordance with recommendations of the Society for Psychophysiological Research committee on heart rate variability (36). The sampling frequency was 1 kHz. Prior to analyses, each waveform was verified, IBIs were visually checked, and artifacts were identified using an algorithm (37) created for the MindWare software program (http://www.mindwaretech.com). RSA was estimated as the natural logarithm of the variance of heart period within the high-frequency bandpass associated with respiration at this age (i.e., 0.15–0.80 Hz) (38). Outlier data were checked and verified minute by minute if they were > 3 SD from the group mean. Missing ANS data were due to acquisition or scoring problems such as equipment malfunction, research assistant error, extraneous movement, and electrode displacement; 96% of the 338 children had scorable ANS reactivity data (n = 326). Mean RSA magnitude was calculated for each 1-min interval and averaged within task. RSA levels during each of the control tasks were used as baseline reference to create four task RSA reactivity scores (task – baseline). These four difference scores were then averaged to create one index of RSA reactivity. Negative scores, indicating a decrease in RSA and vagal withdrawal in response to the challenge, represented greater parasympathetic reactivity. Conversely, positive scores, reflecting an increase in RSA and vagal augmentation in response to the challenge, constituted low parasympathetic reactivity. Average control-task RSA was significantly correlated with RSA change (r = .19, p < .01), but control-task RSA was not correlated with any of the physical health indices, negativity in the parent-child relationship, or SES (p values ranged from .42 to .74).
Child Physical Health Outcomes
Children’s physical health was assessed using parent-report on two subscales from the MacArthur Health and Behavior Questionnaire (HBQ) (39). The 5-item Global Physical Health (PHI) subscale measures children’s general physical health, including physical health-related distress and impairment. The Chronic Medical Conditions (CMC) subscale is a checklist of 22 chronic medical conditions (e.g., asthma, diabetes, hearing problems, etc.). The latter subscale is scored by summing the number of conditions endorsed. Higher scores on PHI or CMC indicate greater health-related impairment or more chronic health conditions, respectively. These HBQ subscales have demonstrated good test-retest reliability and rank-order stability, good cross-informant agreement, and independence from demographic factors (39,40). Further, scores on these subscales have been shown to positively relate to objective health measures, such as body mass index (41).
Statistical Analysis
All analyses were conducted using Mplus with full information maximum likelihood estimation and bias-corrected bootstrapped standard errors; these estimation techniques enable the use of all available data points, are robust to multivariate non-normality and, as noted by MacKinnon and colleagues, maximize statistical power (42). Path models with observed variables were estimated within a structural equation modeling (SEM) framework, which has many advantages over other statistical methods, including the ability to examine multiple mediator and outcome variables simultaneously, to estimate both individual coefficients and overall model fit, and to model error terms rather than pooling error across variables (43–45). In addition, this method allowed for the examination of specific indirect effects even if there was an absence of significant total or direct effects in the mediation model (44).
Two path models were tested, and adequacy of model fit was determined by examining the following fit indices were examined: RMSEA, SRMR, and CFI. Specifically, we first tested a multiple moderation model (Model 1) in which the association between SES at T1 and physical health outcomes at T2 was hypothesized to be moderated by both T1 parent-child relationship negativity and T1 RSA reactivity, adjusting for T1 physical health outcomes. If the estimates associated with either interaction term were significant, we examined the nature of the interactions by computing and testing the statistical significance of the simple slopes for the association between T1 SES and T2 physical health impairment at 1 SD above and below the mean of the moderating variables, following guidelines outlined by Aiken and West (46). Next, we tested a multiple mediation model (Model 2) in which T1 parent-child relationship negativity and T1 RSA reactivity were hypothesized to mediate the association between T1 SES and T2 physical health outcomes, adjusting for T1 physical health outcomes. Finally, based on research indicating differences in the association between SES and health depending on race/ethnicity, we also tested two multiple group models (Model 1 and Model 2 by racial/ethnic minority status) to ascertain whether relations among our variables of interest were specific to or different across White children and children from other racial/ethnic groups.
Results
Zero-order correlations for all study variables are included in Table 2. As shown, chronic medical conditions in the fall and spring were not significantly related to parent-child relationship negativity, RSA, or SES; however, T1 and T2 physical health-related impairment were positively associated with parent-child relationship negativity and negatively associated with SES at T1.
Table 2.
Zero-order correlations among study variables
| 1 | 2 | 3 | 4 | 5 | 6 | ||
|---|---|---|---|---|---|---|---|
| 1. | S ES | ||||||
|
| |||||||
| 2. | PCR | −.03 | |||||
| (n) | (297) | ||||||
|
| |||||||
| 3. | RSA | −.06 | .002 | ||||
| (n) | (310) | (286) | |||||
|
| |||||||
| 4. | CMC-F | −.07 | .04 | .017 | |||
| (n) | (294) | (289) | (284) | ||||
|
| |||||||
| 5. | PHI-F | −.14* | .24** | .06 | .39** | ||
| (n) | (293) | (287) | (282) | (290) | |||
|
| |||||||
| 6. | CMC-S | −.01 | .04 | .04 | .77** | .31** | |
| (n) | (246) | (241) | (237) | (236) | (237) | ||
|
| |||||||
| 7. | PHI-S | −.18** | .30** | −.08 | .28** | .50** | .33** |
| (n) | (279) | (297) | (269) | (268) | (264) | (245) | |
Note: PCR = Parent-child relationship negativity; RSA = Respiratory sinus arrhythmia reactivity; CMC = Chronic medical conditions (Fall or Spring); PHI = Physical health-related impairment (Fall or Spring)
Multiple moderation model
Model fit was adequate, according to recommendations for cut-off points (47,48): RMSEA= .074 [90% CI 0,.149]; CFI=.989; Chi-Square=5.694, p = .058; SRMR = .019. As shown in (Table 3 and Figure 1), the positive association between SES and T2 chronic medical conditions did not reach statistical significance (p = .078), and there was no evidence of moderation by either parent-child relationship negativity or RSA. In contrast, lower SES (p = .041), greater parent-child relationship negativity (p = .001), and greater RSA reactivity (p = .012) predicted greater health-related impairment at T2; however, these main effects must be examined within the context of two statistically significant interactions: both parent-child relationship negativity (p = .035) and RSA reactivity (p =.019) moderated the effect of T1 SES on T2 physical health-related impairment. To test whether these associations varied by race/ethnicity, an unconstrained multiple group (White and Non-White) model was estimated, followed by a constrained multiple group model in which associations among variables were constrained the be equal. A chi-square difference test indicated there was no improvement in model fit (p = .549); thus, there was no evidence that associations among the variables varied by race/ethnicity.
Table 3.
Unstandardized estimates in the multiple moderation model predicting T2 physical health outcomes.
| T2 Chronic Medical Conditions | T2 Physical Health Impairment | |||||
|---|---|---|---|---|---|---|
| Coefficient | SE | P value | Coefficient | SE | P value | |
| T1 CMC | .736 | .047 | < .001 | – | – | – |
| T1 PHI | – | – | – | .443 | .081 | < .001 |
| T1 RSA | −.071 | .164 | .663 | −.152 | .060 | .012 |
| T1 PCR | .001 | .046 | .986 | .093 | .028 | .001 |
| SES | .093 | .053 | .078 | −.054 | .026 | .041 |
| SES*RSA | .070 | .217 | .747 | .169 | .072 | .019 |
| SES*PCR | −.070 | .057 | .218 | −.074 | .035 | .035 |
Note: CMC=Chronic medical conditions; PHI=Physical health impairment; RSA=RSA reactivity; PCR=Parent-child relationship negativity; SES=Socioeconomic status.
Figure 1.
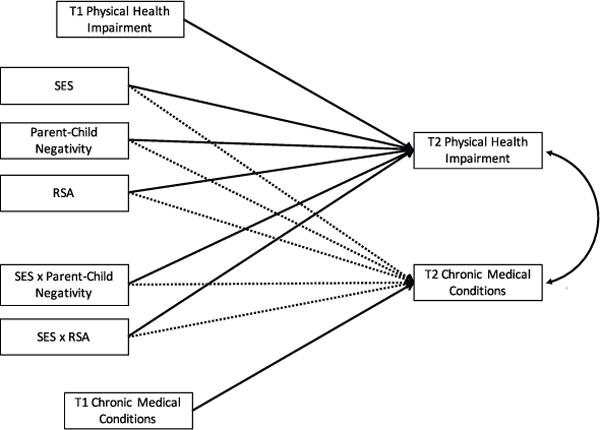
Hypothesized associations between SES, parent-child relationship negativity, RSA reactivity, and physical health outcomes.
Note: Bolded lines are significant at p < .05.
As shown in Figure 2, our continuous measure of SES was negatively related to T2 health-related impairment for children with higher levels of negativity in the parent-child relationship (unstandardized estimate = −.110, SE = .049, p = .024); however, there was no association between SES and health at lower levels of negativity (unstandardized estimate = .016, SE = .033, p = .63). As shown in Figure 3, SES was negatively related to T2 health-related impairment for children exhibiting higher RSA reactivity (unstandardized estimate = −.106, SE = .042, p = .011); however, there was no association between SES and health at lower levels of RSA reactivity (unstandardized estimate = −.006, SE = .034, p = .86).
Figure 2.
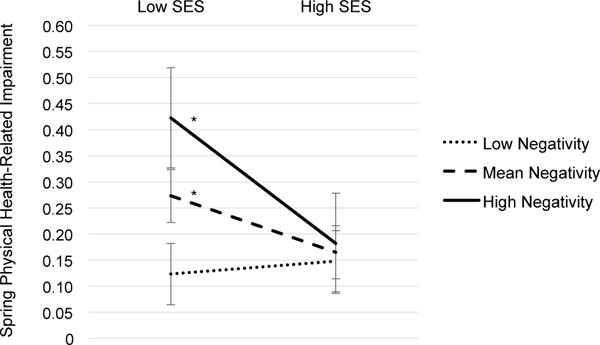
The prospective association between SES and spring physical-health impairment in children at low (−1 SD), mean, and high (+1 SD) levels of parent-child relationship negativity.
Note: *p < .05. Error bars reflect 95% CI.
Figure 3.
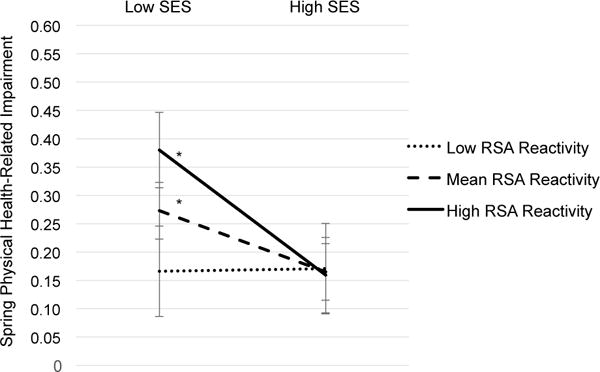
The prospective association between SES and spring physical-health impairment in children at low (+1 SD), mean, and high (−1 SD) levels of RSA reactivity.
Multiple mediation model
A multiple mediation model was tested in which the effect of SES on the two physical health outcomes was mediated by negativity in the parent-child relationship and RSA reactivity. Model fit was excellent: RMSEA= .029 [90%CI 0,.10]; CFI=.997; Chi-Square=3.829, p = .28; SRMR = .020. However, consistent with the zero-order correlations (Table 2), there was no association between SES and either parent-child relationship negativity (p = .88) or RSA reactivity (p = .35), and there was no indirect effect of SES on either measure of physical health at T2 (specific indirect effect p’s between .44 – .99, and total indirect effect p’s between .10 – .11), indicating no mediation. A multiple group model was estimated to test whether mediation was evident in either White or Non-White participants. The model would not converge, suggesting poor fit, and was not examined further.
Discussion
Socioeconomic status is a robust epidemiologic predictor of health, yet there is substantial heterogeneity in adult physical health outcomes among those exposed to early adversity (1). Much remains to be learned about the conditions under which lower SES environments predict greater physical health problems in childhood and beyond (26). Studies of mediation and moderation examine possible “third variables” (47) posited to shape the relation of economic disadvantage to children’s health. The current study examined the prospective relation between family SES and child physical health as well as factors postulated to influence or underlie the SES-physical health association during the transition to kindergarten. Lower SES predicted greater spring physical-health impairment, over and above fall physical health-impairment, but not chronic medical conditions. In addition, this association was strongest among children who experienced high parent-child relationship negativity or heightened physiological reactivity to stress. There was no evidence of mediation by parent-child relationship quality or stress reactivity. Findings suggest that the effects of socioeconomic adversity – one of the most potent and persistent contributors to physical health problems – can be buffered by more proximal social environments (e.g., the parent-child relationship) and individual differences (e.g., parasympathetic reactivity).
There is extensive evidence that the quality of the parent-child relationship plays a critical role in the mental health of young children. As hypothesized in the current study, we observed detrimental associations between low SES and children’s physical health, but only among children reared in environments characterized by high levels of parent-child relationship negativity. It has been suggested that low SES is associated with greater stress and more chaotic home environments (49). The present findings suggest that the physical health correlates of this adverse context can be diminished by a family environment with lower levels of parental harshness and parent-child conflict or exacerbated by heightened negativity in the parent-child relationship. In the former circumstance, the stressors of socioeconomic disadvantage may be tolerable and amenable to coping strategies, while in the latter condition, such stressors may become more toxic and pathogenic (1). Although a reading of the current study should not conflate positive parenting with low levels of parental negativity, the likelihood of positive parent-child interactions is presumably greater when negativity is lower and may operate as a buffer against the consequences of SES adversity. Cumulative risk research also offers a perspective on the combined detrimental effects of low SES and harsh parenting, as such studies have consistently observed negative consequences of co-occurring environmental adversities on children’s well-being (50).
Prior studies of poverty exposure and physical health in childhood have focused on the role of pro-inflammatory processes (51), elevated HPA axis activity (52), and blood pressure responses to stress (25). To our knowledge, the role of parasympathetic reactivity in the connection between socioeconomic disadvantage and physical health outcomes has not yet been examined. Challenge-induced reductions in parasympathetic activation may represent a particularly relevant indicator of physiological reactivity to psychosocial stress. As described in Porges’ Polyvagal Theory, the vagal system exerts a critical role in regulating adaptive social and emotional responding to environmental challenges (21). Dysregulated vagal responses have implications for psychopathology related to poor emotion regulation (53) and may extend to an influence on the development of physical health problems. The present findings indicated that in the context of socioeconomic disadvantage, physical health impairments at the end of kindergarten were highest among children with greater RSA withdrawal and lowest among less parasympathetically-reactive children. Although there have been well-supported findings that greater RSA reactivity may act as a protective factor (54), the current findings are consistent with previous research showing that physiologically reactive children exposed to adverse early family environments are more susceptible to mental health problems relative to their less reactive peers (55,56). The current study extends such literature, suggesting that heightened RSA reactivity may be viewed as a vulnerability factor that places children at increased risk for experiencing harmful effects of socioeconomic adversity on physical health.
There was no association between any of the variables of interest and chronic medical conditions across the school year. The absence of these relations was surprising given the extensive literature documenting associations between SES and asthma and cardiovascular conditions (57). As might be expected within a community sample of 5-year old children, approximately half of the children did not have chronic health conditions and relatively few had more than one condition. The current study employed statistical methods robust to non-normal data; however, SES relations with health might be better detected in a population with a greater number of conditions. Further, SES has most often been implicated in associations with the severity of a chronic condition in childhood, such as asthma, and it is reasonable to surmise that the link between SES and number of different medical conditions might not arise until later in life when comorbidity is a more common occurrence. In addition, previous research suggests the effects of SES on health may differ among racial groups. Indeed, prior study within this sample observed differences in the associations between SES and children’s daily cortisol between minority and non-minority children (58). However, in the current investigation, associations between parenting, RSA reactivity, and physical health outcomes were not moderated by racial/ethnic minority status. Future studies with larger diverse samples spanning childhood are needed to comprehensively examine the complex relations among SES, race/ethnicity, and children’s health.
Neither the parent-child relationship nor RSA reactivity were associated with SES, precluding those variables from serving as mediators of the association between SES and health within these analyses. Low socioeconomic status is associated with a multitude of environmental challenges and uncertainties, with effects on domains of parenting and the family environment that were not assessed here, including family stress, parental investment, parent psychopathology, and interparental conflict (49,59,60). The absence of a relation between SES and the measure of parent-child negativity employed in the current study suggests that the affective quality of the parent’s perception of their relationship with the child operates independently from SES-related stress to influence the connection between family SES and child physical health. Given this, interventions focused on improving or protecting physical health in children exposed to socioeconomic adversity should incorporate supports for the parent-child relationship. Although it has been proposed that the biological embedding of early life stress can occur through effects on the autonomic nervous system (12), given the ongoing development of RSA regulatory functioning during early childhood, an association between SES and RSA reactivity may not be easily detectable by age 5. Additional research of other indices of biological reactivity (e.g., sympathetic nervous system), and future longitudinal studies will be important for determining whether these theories apply to early life SES effects on health.
A number of limitations must be considered when interpreting the findings. First, although the sample size was significantly larger than the majority of samples reported in psychological studies examining mediation (see 42), there may have not been adequate power to detect small indirect effects in the multiple mediation model. Second, SES can be measured in multiple ways, including objective and subjective assessments. We used a “traditional” measure of SES that encompassed family income and highest level of educational attainment in the household. Other research suggests the importance of “contextual” (e.g., neighborhood-based) approaches to capturing socioeconomic disadvantage since community resources can vary widely even among families with similar SES (61). Third, we cannot rule out the possibility that lower SES parents might over-estimate their children’s health impairments, and findings would be strengthened by an objective measure of physical health (i.e., physical exams, medical record review). Fourth, the current study used a brief parent-report measure of parent-child negativity that has previously demonstrated relations with children’s mental and physical health (31,32). However, the internal consistency of this scale was low in the current sample, which may be attributed to its limited number of items (33). The present study also focused on negative qualities of the parent-child relationships, and supportive parenting is likely also an important protective factor in the association between low SES and health. Observational measures of parent-child relationship quality that capture positive and negative attributes might provide a stronger test of the role of parenting in mitigating the effects of economic adversity on child physical health.
Finally, it is important to consider the temporal order of variables when conducting statistical tests of moderation and mediation (13). However, given the dynamic nature of parent-child relationship quality, physiological reactivity and socioeconomic risk early in life, the temporality of each measure relative to another is not easily established. Randomized controlled trials of interventions designed to improve parent-child relationship quality (62) and children’s physiological regulation (63) in the context of family-related stress represent the “gold standard” for establishing causality. Thus, the most powerful test of the associations observed here would involve improvements in physical health as a result of intervention-induced changes in parenting and children’s regulatory capacity in children exposed to socioeconomic adversity. Bolstered by the results of the current study, such examinations are apt for future research.
The present investigation contributes to extant research on the relation between economic adversity and physical health in childhood. The association between SES and physical health varies with age, and is particularly strong for some outcomes during early childhood (8). The transition to kindergarten represents a critical developmental period in the life of a child. It is a time of increased expectations, greater independence and responsibility, and new demands for social competence (64). Physical health is an important component of school readiness and children’s potential for learning (65). In short, the first school year lays a foundation for a child’s academic and social development during the subsequent years, and children who experience physical health problems face greater academic challenges and lower SES later in life (66). Identifying the environmental, familial, and individual qualities that influence children’s physical health during this time can have a substantial impact on their course of development.
In addition to focusing on a sensitive developmental period, the use of physical health measures collected at the beginning and end of the school year offered a unique opportunity to examine the prospective effects of SES on physical health outcomes. By adjusting for baseline health, we were able to ascertain whether SES contributed uniquely to health outcomes at the end of a school year, above and beyond physical health conditions at the time of SES assessment. Findings suggest that intervention need not occur before associations between SES and physical health arise to be effective. Further, in examining two putative moderators, we gave concurrent consideration to both family-level (e.g., parenting) and individual-level (e.g., physiological) factors, thereby advancing research on the conditions under which economic disadvantage influences children’s health. Finally, by employing structural equation modeling, we were able to test these relations simultaneously, avoiding the problems of increased error probability associated with conducting multiple statistical tests and improving our ability to understand the complex, multi-layered predictors of health.
In sum, a robust and growing literature supports the pervasive, detrimental effects of low SES on health across the lifespan. SES-related health disparities have increased over the course of the past several decades (4), elevating the salience and importance of such research. The complexity of this association calls for attention to factors that explain or shape the relation between economic adversity and health outcomes, particularly during the rapid developmental period of early childhood. The current study examined the role of negativity in the parent-child relationship and individual differences in RSA reactivity in the association between SES and physical health outcomes among children during the kindergarten year. Socioeconomic adversity was associated with greater physical health impairment among children exposed to higher levels of parental negativity and among those with elevated RSA reactivity, but was unrelated to health impairment at low levels of negativity or reactivity. Support for a mediating role of either variable was not found. The moderating influence of such individual- and family-level variables may inform public policy and early childhood interventions in order to tailor programmatic efforts to those most vulnerable to the costs of socioeconomic adversity on health and development.
Acknowledgments
Source of Funding: This study was supported by grants awarded to W. Thomas Boyce from the National Institute of Mental Health (R01 MH62320), the MacArthur Foundation Research Network on Psychopathology and Development, and the Canadian Institute for Advanced Research.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
Contributor Information
Melissa J. Hagan, San Francisco State University & University of California, San Francisco.
Danielle S. Roubinov, University of California San Francisco.
Nancy E. Adler, University of California San Francisco.
W. Thomas Boyce, University of California San Francisco.
Nicole R. Bush, University of California San Francisco.
References
- 1.Shonkoff JP, Boyce WT, McEwen BS. Neuroscience, Molecular Biology, and the Childhood Roots of Health Disparities. Jama. 2009;301(21):2252. doi: 10.1001/jama.2009.754. [DOI] [PubMed] [Google Scholar]
- 2.Braveman P, Egerter S, Williams DR. The Social Determinants of Health: Coming of Age. Annu Rev Public Health. 2011;32(1):381–98. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 3.Chen E, Paterson LQ. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychol. 2006;25(6):704–14. doi: 10.1037/0278-6133.25.6.704. [DOI] [PubMed] [Google Scholar]
- 4.Nandi A, Glymour MM, Subramanian SV. Association among socioeconomic status, health behaviors, and all-cause mortality in the United States. Epidemiology. 2014;25(2):170–7. doi: 10.1097/EDE.0000000000000038. [DOI] [PubMed] [Google Scholar]
- 5.Ziol-Guest KM, Duncan GJ, Kalil A, Boyce WT. Early childhood poverty, immune-mediated disease processes, and adult productivity. Proc Natl Acad Sci U S A. 2012 Oct 16;109(Suppl (Supplement_2)):17289–93. doi: 10.1073/pnas.1203167109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belsky J, Bell B, Bradley RH, Stallard N, Stewart-Brown SL. Socioeconomic risk, parenting during the preschool years and child health age 6 years. Eur J Public Health. 2007;17(5):508–13. doi: 10.1093/eurpub/ckl261. [DOI] [PubMed] [Google Scholar]
- 7.Chen E, Martin AD, Matthews KA. Understanding Health Disparities: The Role of Race and Socioeconomic Status in Children’s Health. Am J Public Health. 2006;96(4):702–8. doi: 10.2105/AJPH.2004.048124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen E, Matthews KA, Boyce WT. Socioeconomic differences in children’s health: How and why do these relationships change with age? Psychol Bull. 2002;128(2):295–329. doi: 10.1037/0033-2909.128.2.295. [DOI] [PubMed] [Google Scholar]
- 9.Adler NE, Stewart J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186(1):5–23. doi: 10.1111/j.1749-6632.2009.05337.x. [DOI] [PubMed] [Google Scholar]
- 10.Adler N, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, et al. Socioeconomic status and health. Am Psychol. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- 11.Bush NR, Boyce WT. The Contribution of Early Experience to Biological Development and Sensitivity to Context. In: Lewis M, Rudolph KD, editors. Handbook of Developmental Psychopathology. New York: Springer; 2014. pp. 287–309. [Google Scholar]
- 12.Hertzman C, Boyce T. How Experience Gets Under the Skin to Create Gradients in Developmental Health. Annu Rev Public Health. 2010;31(1):329–47. doi: 10.1146/annurev.publhealth.012809.103538. [DOI] [PubMed] [Google Scholar]
- 13.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158(6):848–56. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 14.Miller GE, Lachman ME, Chen E, Gruenewald TL, Karlamangla AS, Seeman TE. Pathways to resilience: maternal nurturance as a buffer against the effects of childhood poverty on metabolic syndrome at midlife. Psychol Sci. 2011 Dec;22(12):1591–9. doi: 10.1177/0956797611419170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spencer N, Thanh TM, Louise S. Low Income/Socio-Economic Status in Early Childhood and Physical Health in Later Childhood/Adolescence: A Systematic Review. Matern Child Health J. 2013;17(3):424–31. doi: 10.1007/s10995-012-1010-2. [DOI] [PubMed] [Google Scholar]
- 16.Mäntymaa M, Puura K, Luoma I, Salmelin R, Davis H, Tsiantis J, et al. Infant-mother interaction as a predictor of child’s chronic health problems. Child Care Health Dev. 2003 May;29(3):181–91. doi: 10.1046/j.1365-2214.2003.00330.x. [DOI] [PubMed] [Google Scholar]
- 17.Derryberry D, Reed Ma, Pilkenton-Taylor C. Temperament and coping: advantages of an individual differences perspective. Dev Psychopathol. 2003;15:1049–66. [PubMed] [Google Scholar]
- 18.Ellis BJ, Boyce WT, Belsky J, Bakermans-Kranenburg MJ, van Ijzendoorn MH. Differential susceptibility to the environment: an evolutionary–neurodevelopmental theory. Dev Psychopathol. 2011;23(1):7–28. doi: 10.1017/S0954579410000611. [DOI] [PubMed] [Google Scholar]
- 19.Obradović J, Bush NR, Boyce WT. The interactive effect of marital conflict and stress reactivity on externalizing and internalizing symptoms: the role of laboratory stressors. Dev Psychopathol. 2011;23(1):101–14. doi: 10.1017/S0954579410000672. [DOI] [PubMed] [Google Scholar]
- 20.Treadwell MJ, Alkon A, Quirolo KC, Boyce WT. Mental Health, and Functional Impairment for Children. 2010;31(6):491–7. doi: 10.1097/DBP.0b013e3181e2830f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Porges SW. The polyvagal theory: Phylogenetic substrates of a social nervous system. Int J Psychophysiol. 2001;42(2):123–46. doi: 10.1016/s0167-8760(01)00162-3. [DOI] [PubMed] [Google Scholar]
- 22.Boyce WT, Chesney M, Alkon A, Tschann JM, Adams S, Chesterman B, et al. Psychobiologic reactivity to stress and childhood respiratory illnesses: results of two prospective studies. Psychosom Med. 1995;57(5):411–22. doi: 10.1097/00006842-199509000-00001. [DOI] [PubMed] [Google Scholar]
- 23.El-Sheikh M, Harger J, Whitson SM. Exposure to interparental conflict and children’s adjustment and physical health: the moderating role of vagal tone. Child Dev. 2001;72(6):1617–36. doi: 10.1111/1467-8624.00369. [DOI] [PubMed] [Google Scholar]
- 24.Gottman JM, Katz LF, Hooven C. Parental meta-emotion philosophy and the emotional life of families: Theoretical models and preliminary data. J Fam Psychol. 1996;10(3):243–68. [Google Scholar]
- 25.Evans GW, Kim P. Childhood poverty and health: Cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18:953–7. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- 26.Adler N, Bush NR, Pantell MS. Rigor, vigor, and the study of health disparities. Proc Natl Acad Sci. 2012;109(Supplement_2):17154–9. doi: 10.1073/pnas.1121399109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schreier HM, Chen E. Socioeconomic Status and the Health of Youth: A Multi-level, Multi-domain Approach to Conceptualizing Pathways. Psychol Bull. 2013;139(3):606–54. doi: 10.1037/a0029416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts GC, Block JH, Block J. Continuity and change in parents’ child-rearing practices. Child Dev. 1984;55(2):586–97. [Google Scholar]
- 29.Obradović J, Bush NR, Stamperdahl J, Adler NE, Boyce WT. Biological sensitivity to context: The interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Dev. 2010;81(1):270–89. doi: 10.1111/j.1467-8624.2009.01394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Essex MJ, Klein MH, Slattery MJ, Goldsmith HH, Kalin NH. Early risk factors and developmental pathways to chronic high inhibition and social anxiety disorder in adolescence. Am J Psychiatry. 2010 Jan;167(1):40–6. doi: 10.1176/appi.ajp.2009.07010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellis BJ, Essex MJ. Family environments, adrenarche, and sexual maturation: a longitudinal test of a life history model. Child Dev. 2007 Jan;78(6):1799–817. doi: 10.1111/j.1467-8624.2007.01092.x. [DOI] [PubMed] [Google Scholar]
- 32.Essex MJ, Klein MH, Cho E, Kalin NH. Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biol Psychiatry. 2002 Oct 15;52(8):776–84. doi: 10.1016/s0006-3223(02)01553-6. [DOI] [PubMed] [Google Scholar]
- 33.Sijtsma K. On the Use, the Misuse, and the Very Limited Usefulness of Cronbach’s Alpha. Psychometrika. 2009 Mar;74(1):107–20. doi: 10.1007/s11336-008-9101-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Berntson GG, Cacioppo JT, Quigley KS. Autonomic determinism: the modes of autonomic control, the doctrine of autonomic space, and the laws of autonomic constraint. Psychol Rev. 1991;98(4):459–87. doi: 10.1037/0033-295x.98.4.459. [DOI] [PubMed] [Google Scholar]
- 35.Bush NR, Alkon A, Obradović J, Stamperdahl J, Thomas Boyce W. Differentiating challenge reactivity from psychomotor activity in studies of children’s psychophysiology: Considerations for theory and measurement. J Exp Child Psychol. 2011;110(1):62–79. doi: 10.1016/j.jecp.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berntson GG, Bigger JT, Eckberg DL, Grossman P, Kaufmann PG, Malik M, et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997 Nov;34(6):623–48. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- 37.Berntson GG, Quigley KS, Jang JF, Boysen ST. An approach to artifact identification: application to heart period data. Psychophysiology. 1990 Sep;27(5):586–98. doi: 10.1111/j.1469-8986.1990.tb01982.x. [DOI] [PubMed] [Google Scholar]
- 38.Bar-Haim Y, Marshall PJ, Fox NA. Developmental changes in heart period and high-frequency heart period variability from 4 months to 4 years of age. Dev Psychobiol. 2000 Jul;37(1):44–56. doi: 10.1002/1098-2302(200007)37:1<44::aid-dev6>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 39.Essex MJ, Boyce WT, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood. II: developing the Macarthur health and Behavior Questionnaire. J Am Acad Child Adolesc Psychiatry. 2002 May;41(5):588–603. doi: 10.1097/00004583-200205000-00017. [DOI] [PubMed] [Google Scholar]
- 40.Burk LR, Armstrong JM, Park JH, Zahn-Waxler C, Klein MH, Essex MJ. Stability of early identified aggressive victim status in elementary school and associations with later mental health problems and functional impairments. J Abnorm Child Psychol. 2011;39(2):225–38. doi: 10.1007/s10802-010-9454-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Williams NA, Fournier J, Coday M, Richey PA, Tylavsky FA, Hare ME. Body esteem, peer difficulties and perceptions of physical health in overweight and obese urban children aged 5 to 7 years. Child Care Health Dev. 2013 Nov;39(6):825–34. doi: 10.1111/j.1365-2214.2012.01401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007 Mar;18(3):233–9. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Byrne BM. Structural Equation Modeling with Mplus: Basic Concepts, Applications, and Programming. New York: Routledge; 2013. [Google Scholar]
- 44.MacKinnon DP. Introduction to Statistical Mediation Analysis. New York: Lawrence Erlbaum; 2008. [Google Scholar]
- 45.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6th. New York: Pearson; 2012. [Google Scholar]
- 46.Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Sage Publications; 1991. [Google Scholar]
- 47.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J. 1999;6(1):1–55. [Google Scholar]
- 48.Steiger JH. Understanding the limitations of global fit assessment in structural equation modeling. Pers Individ Dif. 2007;42(5):893–8. [Google Scholar]
- 49.Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, Salpekar N. The role of chaos in poverty and children’s socioemotional adjustment. Psychol Sci. 2005 Jul;16(7):560–5. doi: 10.1111/j.0956-7976.2005.01575.x. [DOI] [PubMed] [Google Scholar]
- 50.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–96. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 51.Miller GE, Chen E. The Biological Residue of Childhood Poverty. Child Dev Perspect. 2013;7(2):67–73. doi: 10.1111/cdep.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lupien SJ, King S, Meaney MJ, McEwen BS. Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biol Psychiatry. 2000 Nov 15;48(10):976–80. doi: 10.1016/s0006-3223(00)00965-3. [DOI] [PubMed] [Google Scholar]
- 53.Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal Theory and developmental psychopathology: Emotion dysregulation and conduct problems from preschool to adolescence. Biol Psychol. 2007;74(2):174–84. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.El-Sheikh M, Whitson Sa. Longitudinal relations between marital conflict and child adjustment: Vagal regulation as a protective factor. J Fam Psychol. 2006;20(1):30–9. doi: 10.1037/0893-3200.20.1.30. [DOI] [PubMed] [Google Scholar]
- 55.Boyce WT, Essex MJ, Alkon A, Goldsmith HH, Kraemer HC, Kupfer DJ. Early father involvement moderates biobehavioral susceptibility to mental health problems in middle childhood. J Am Acad Child Adolesc Psychiatry. 2006 Dec;45(12):1510–20. doi: 10.1097/01.chi.0000237706.50884.8b. [DOI] [PubMed] [Google Scholar]
- 56.Gentzler AL, Santucci AK, Kovacs M, Fox NA. Respiratory sinus arrhythmia reactivity predicts emotion regulation and depressive symptoms in at-risk and control children. Biol Psychol. 2009;82(2):156–63. doi: 10.1016/j.biopsycho.2009.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen E, Hanson MD, Paterson LQ, Griffin MJ, Walker Ha, Miller GE. Socioeconomic status and inflammatory processes in childhood asthma: The role of psychological stress. J Allergy Clin Immunol. 2006;117(5):1014–20. doi: 10.1016/j.jaci.2006.01.036. [DOI] [PubMed] [Google Scholar]
- 58.Bush NR, Obradović J, Adler N, Boyce WT. Kindergarten stressors and cumulative adrenocortical activation: the “first straws” of allostatic load? Dev Psychopathol. 2011;23(4):1089–106. doi: 10.1017/S0954579411000514. [DOI] [PubMed] [Google Scholar]
- 59.Evans GW. The Environment of Childhood Poverty. Am Psychol. 2004;59(2):77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- 60.Conger RD, Conger KJ, Martin MJ. Socioeconomic status, family processes, and individual development. J Marriage Fam. 2011;72(3):685–704. doi: 10.1111/j.1741-3737.2010.00725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Matthews Ka, Gallo LC. Psychological perspective on pathways linking socioeconomic status and physical health. Annu Rev Psychol. 2011;62:501–30. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hagan MJ, Tein J, Sandler IN, Wolchik Sa, Ayers TS, Luecken LJ. Strengthening effective parenting practices over the long term: Effects of a preventive intervention for parentally bereaved Families. J Clin Child Adolesc Psychol. 2012;41(2):177–88. doi: 10.1080/15374416.2012.651996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Luecken LJ, Hagan MJ, Sandler IN, Tein JY, Ayers TS, Wolchik Sa. Cortisol levels six-years after participation in the Family Bereavement Program Psychoneuroendocrinology. 5. Vol. 35. Elsevier Ltd; 2010. pp. 785–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rimm-Kaufman SE, Pianta RC. An Ecological Perspective on the Transition to Kindergarten. J Appl Dev Psychol. 2000 Sep;21(5):491–511. [Google Scholar]
- 65.Guhn M, Janus M, Hertzman C. The Early Development Instrument: Translating School Readiness Assessment Into Community Actions and Policy Planning. Early Educ Dev. 2007;18(3):369–74. [Google Scholar]
- 66.Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. J Health Econ. 2005;24(2):365–89. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]


