Abstract
Purpose
The objective of this study was to evaluate the impact of regionalization on sepsis survival, to describe the role of inter-hospital transfer in rural sepsis care, and to measure the cost of inter-hospital transfer in a predominantly rural state.
Materials and Methods
Observational case-control study using statewide administrative claims data from 2005-2014 in a predominantly rural Midwestern state. Mortality and marginal costs were estimated with multivariable generalized estimating equations (GEE) models and with instrumental variables models.
Results
A total of 18,246 patients were included, of which 59% were transferred between hospitals. Transferred patients had higher mortality and longer hospital length-of-stay than non-transferred patients. Using a multivariable GEE model to adjust for potentially confounding factors, inter-hospital transfer was associated with increased mortality (aOR 1.7, 95%CI 1.5 – 1.9). Using an instrumental variables model, transfer was associated with a 9.2% increased risk of death. Transfer was associated with additional costs of $6,897 (95%CI $5,769-8,024). Even when limiting to only those patients who received care in the largest hospitals, transfer was still associated with $5,167 (95%CI $3,696-6,638) in additional cost.
Conclusions
The majority of rural sepsis patients are transferred, and these transferred patients have higher mortality and significantly increased cost of care.
Keywords: sepsis, health services, health care economics and organizations, hospitals, rural, emergency medical services, emergency service, hospital
Background
Sepsis is a life-threatening condition that has doubled in incidence over the past decade, now constituting 17% of U.S. in-hospital deaths at a cost of almost $15 billion annually.1 Severe sepsis and septic shock cases in the emergency department (ED) have increased as well, with an estimated 390,000 U.S. ED visits in 2009.2 Aggressive early ED care has been shown to decrease mortality.3, 4 Although no sepsis-specific therapies that target sepsis pathophysiology have been introduced, mortality has fallen by 25% over the past two decades,5 suggesting that systematic improvements in care processes are responsible for much of the survival increase.4 The ED plays a pivotal role in sepsis survival, and quality improvement in the ED has been shown to decrease mortality.4 Unfortunately, this outcome improvement has not completely extended to low-volume EDs, where sepsis mortality can be up to 38% higher than in high-volume EDs.6
Strategies to improve outcomes in low-volume rural hospitals include improvement in local quality of care and regionalization. Regionalization is the practice of transferring patients to higher volume hospitals, and it has been shown to improve outcomes in trauma, myocardial infarction, and ischemic stroke.7-11 Care in high-volume centers has been associated with increased survival in sepsis as well 6, 12, 13, so regionalization could narrow the sepsis survival gap between high-volume and low-volume centers by improving the delivery of life-saving interventions. However, the role of regionalization in changing sepsis survival for those who present to low-volume EDs is less clear. Many transferred sepsis patients in rural states have low adherence with national sepsis resuscitation guidelines.14 As sepsis survival depends in large part on time-sensitive interventions, the transfer process associated with regionalization could also cause harm to patients, driven by the administrative and time-consuming processes associated with inter-hospital transfer. Because both early resuscitation and later hospital care are important to improving patient outcomes, it is unclear what role inter-hospital transfer plays in improving sepsis survival.
The objective of this study was (1) to measure the association between inter-hospital transfer and survival for patients with severe sepsis or septic shock, (2) to describe the prevalence of inter-hospital transfer and factors contributing to its use for rural severe sepsis and septic shock patients, and (3) to estimate the increased health care costs and resource utilization associated with inter-hospital transfer. We also sought to explore the relative contribution of ED care and inpatient care on clinical outcomes.
Methods
Study Design, Setting, and Selection of Participants
This study is a cohort study of all adults (age ≥ 18 years) with severe sepsis or septic shock treated in Iowa EDs from January 1, 2005 – December 31, 2014. Participants were identified by claims data compiled in the Iowa Hospital Association Inpatient and Outpatient data sets. To identify transferred patients, a probabilistic linkage algorithm was used to link records across inter-hospital transfer, using date of birth, sex, patient zip code, county of residence, and date of visit through a sequential matching algorithm, using social security number to break non-matching linkages. A one-day time window between visits was permitted to account for patients whose transfer process spanned across a midnight (if discharge disposition from first visit was consistent with transfer). A sample of 10% of the records was manually verified to confirm appropriate linkages.
Severe sepsis and septic shock were identified using a previously validated definition based on diagnosis billing codes from the International Classification of Diseases, 9th edition, Clinical Modification (ICD-9-CM).15 Inter-hospital transfer was defined as an ED visit with a discharge code (either ED or hospital inpatient) consistent with transfer to another acute care hospital, for which an inpatient visit could be linked. Sepsis patients were divided into two cohorts: (1) those transferred to another hospital and (2) those admitted locally without transfer. This study was approved by the local Institutional Review Board (IRB #01, protocol 201409761) under waiver of informed consent.
Methods and Measurements
Definitions
Index ED was defined as the first ED to which a patient presented. Sepsis capable hospital was defined to be a hospital that presumably had resources to care for patients with severe sepsis or septic shock, and was estimated as any hospital with an intensive care unit that was not a federally-designated critical access hospital, and that had an annual ED volume above the 25th percentile in the data set. These values were selected to identify hospitals that may be able to provide sepsis care without transfer. A top-decile sepsis-volume hospital was a hospital in the top decile for inpatient severe sepsis or septic shock discharges. Rurality was defined using Rural Urban Commuting Area (RUCA) codes mapped to the zip code of the patient’s residence 16, which is an accepted form of classifying census tracts by population density, urbanization, and daily commuting.17 Comorbidities were defined using the Elixhauser methodology: a set of 30 comorbid conditions defined by ICD-9-CM codes that have been shown to predict mortality, hospitalization, and health care utilization in risk adjustment models.18-20 Source of infection was defined from the ICD-9-CM codes from the discharge diagnoses.15
Mapping and Driving Distances
Driving distances were estimated using the GoogleMaps Application Programming Interface (API)21, using geocoded hospital locations from each hospital street address and the centroid of the zip code of residence, using public roads and highways.
Calculation of Health Care Costs
Health care costs were estimated both from medical costs and family costs borne additionally by transferred patients. Medical costs were estimated from charges by using hospital-specific cost-to-charge ratios calculated from each hospital’s annual financial statements, corrected for inflation (Consumer Price Index – Medical Costs), using methods similar to ratios published by the Health Care Utilization Project.22, 23 The objective of this correction was to account for imbalances in pricing similar care between different hospitals. Ambulance transfer costs were estimated from the 2010 Medicare ambulance reimbursement rate for an Advanced Life Support ambulance from the index hospital to the admitting hospital.
Family costs were estimated to be the sum of: (1) transportation (driving) to the admission hospital plus (2) either: (a) lodging near the admission hospital for the duration of admission or (b) daily commuting from home to the admission hospital (whichever was less expensive). Mileage costs were estimated from the Internal Revenue Service deduction rate for medical travel.24 Lodging costs were estimated from a survey of hotel hospital rates near the 5 hospitals that accepted most inter-hospital transfers. All hotels on the hospital preferred hotel list were contacted and the hospital-preferred rate for the lowest cost double-occupancy room was elicited. The mean of the 3 lowest-cost hotels (tax included) was taken as the affordable hotel rate for each location. Since the mean rate for each of the 5 hospitals was very close, the mean of all 15 hotels was selected as the daily lodging rate ($70.85 2010$USD, with tax included). Additional costs, such as lost wages, were not included since those costs would likely apply equally to both transferred and non-transferred patients.
Outcomes
The primary outcome of the study was the association between inter-hospital transfer and hospital mortality. The secondary outcomes were to estimate the transfer rate for severe sepsis and septic shock patients, and to estimate the incremental cost of transfer among sepsis patients. Additionally, an analysis of clustering was conducted to determine the relative value of ED hospital vs. inpatient hospital and clinical outcomes.
Availability of Data and Materials
Because this study was conducted with protected health information that could allow identification of study participants under waiver of informed consent, the data set upon which the conclusions were based is not publicly available.
Analysis
Univariate analysis was conducted using t-test, Wilcoxon rank-sum test, and the chi-squared test, as appropriate.
Variables for inclusion in multivariable models were selected based on both statistical and clinical criteria, screening statistically-significant variables (p<0.20) for clinical relevance prior to inclusion (since statistical significance can be misleading with large samples). We included year of presentation in our models to capture changes in sepsis survival over time. Covariates were retained in the model according to Bayesian Information Criterion (BIC), and collinearity and statistical interactions were examined with each model.
No physiologic severity of illness measure was available in the data set, so severity of illness was estimated in two ways: (1) Elixhauser comorbidity variables were used to estimate conditions associated with mortality, and (2) the cost of the index ED visit was selected as an additional estimate of illness severity. Because index ED care was provided prior to inter-hospital transfer and because more severely ill patients receive more care, we hypothesized that cost of care would approximate the intensity of care in aggregate, and that intensity would be associated with illness severity at the time of presentation. This cost includes tests, interventions, and professional fees, so it is a relatively broad-based estimate of intensity of care. We determined a priori that this parameter would only be included for risk adjustment if it improved the fit of the mortality model significantly (based on Bayesian Information Criteria, BIC).
Clustering
To determine whether ED hospital or inpatient hospital was more strongly associated with outcome, a clustering analysis was conducted. Prior to multivariable GEE model development, a preliminary analysis using logistic regression was performed to determine whether index hospital or admission hospital was more closely associated with variability in the outcome. This model included the hospital identifier for both the index ED and the admission hospital, and the variable with the strongest association based on BIC criteria was selected as the clustering variable. Admission hospital was more strongly associated, so all subsequent multilevel models were clustered on admission hospital (χ2=294.0 vs. 151.7).
Multivariable Mortality Models
Two comparative effectiveness techniques were proposed to account for illness severity in measuring the association of inter-hospital transfer on mortality:
Generalized Estimating Equations Model
An explanatory GEE model was constructed with a dependent variable of mortality, a logit link function and an exchangeable correlation matrix. Included variables were selected from the univariate analysis based on both clinical relevance and statistical association (p<0.20), and BIC criteria were used to select the most parsimonious model that explained variability in survival.
Instrumental Variables Model
The second technique that we used to estimate the effect of inter-hospital transfer on mortality was an instrumental variables (IV) approach using a 2-stage least-squares estimator. This technique adjusts for unmeasured confounders, which in our case includes severity of illness. To use this technique, we proposed to define distance to a top-decile sepsis-volume hospital as our instrument. Distance to top-decile sepsis-volume hospital is strongly associated with likelihood of transfer (first-stage model F-statistic=463.0) because of the relatively even geographic spacing of Iowa hospitals, but it should not predict mortality except through the process of inter-hospital transfer. Furthermore, the instrument satisfies the exclusion restriction, because distance to a top-decile sepsis-volume hospital cannot influence care except through inter-hospital transfer, and no plausible reverse causal pathway exists. We assume that sepsis severity is equally distributed across geography at the time of presentation. Importantly, the estimate provided by the IV model is a local average treatment effect, which is a marginal effect for the population who is transferred because of specific hospital factors, rather than the effect for all transferred patients.
Multivariable Cost Models
Since cost data is typically right-skewed, we proposed to conduct the analysis in two separate ways: using a log-transformed model and using a linear model. The statistical advantage of the log-transformed model is that it more accurately represents the distribution of costs in the population, but the linear model is much more intuitive to interpret. If the estimates between the two models are similar, we decided a priori that we would report linear regression means.
Generalized Estimating Equations Model
An explanatory GEE model was built with an outcome of total cost, using an identity link and an exchangeable correlation matrix to measure the association between inter-hospital transfer on total medical and non-medical costs. Variables were included from the univariate analysis in the same manner (excluding ED cost as a covariate because of its inclusion in total cost). This model was constructed with a dependent variable of cost, then separately with an output of log-transformed cost.
Subgroup Analyses
Three subgroup analyses were planned a priori. The first subgroup analysis was stratified on ED volume sextile, and was designed to understand the role of ED volume on modifying the transfer mortality relationship. Subsequent analysis stratified on inpatient sepsis volume sextile.
The second analysis was designed to measure the effect of inter-hospital transfer only among patients presenting to hospitals most equipped to provide severe sepsis and septic shock care (sepsis-capable hospitals). This analysis was intended as a robustness check, assuming that care available pre-transfer would be more homogenous in these hospitals, even among those who are ultimately transferred.
The third subgroup analysis was performed to more closely measure the impact of inter-hospital transfer on cost of care, and included only patients who were admitted to top-decile sepsis-volume hospitals. Recognizing that there is large inter-hospital variability in inpatient costs of care, this analysis was intended to limit the assertion that the increase in cost is attributable only to differences in the efficiency of high-volume inpatient care.
All statistical analyses were completed using SAS v.9.2 (SAS Institute, Cary, North Carolina) or Stata v.13.1 (StataCorp LP, College Station, Texas), and this study is reported in accordance with the Strengthening The Reporting of OBservational Studies in Epidemiology (STROBE) statement.25
Results
Characteristics of the Study Subjects
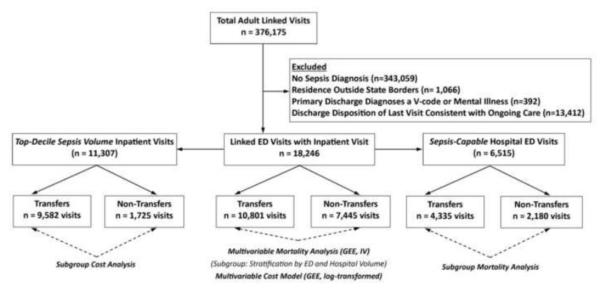
A total of 23,067 cases of severe sepsis or septic shock were identified over a 10-year period, of which 79% (n = 18,246) were successfully linked, with higher proportions of failed linkages in border counties adjacent to major metropolitan areas outside Iowa (likely transfers across the state border) (Figure 1). Most patients resided in rural zip codes, and 63% of patients (n=11,523) initially sought care in critical access hospitals (a federal designation for hospitals that serve vulnerable rural populations). The majority of transfers occurred directly from the ED, with 36% (n=3,846) of patients being admitted to an inpatient service locally and being subsequently transferred. The mortality rate in this cohort was 17% (n=3,082), and the median total costs of care were $14,744 (IQR $7,513 – $31,482 2010$USD).
Figure 1.
Proportion of cases transferred between hospitals indexed to population, Iowa, 2005-2013, by zip code tabulation area (ZCTA). Regions of Iowa that are the most rural have the highest transfer rates. Some regions (southwest Iowa near border with Nebraska) have low levels of observed transfer, likely because most transferred patients have a destination outside Iowa, so no linkage was created across transfer. These unlinked cases were excluded from the analysis.
Main Results
Descriptive Analysis
Of all ED severe sepsis and septic shock patients, 10,801 (59.2%) were transferred between hospitals (Figure 2). Nearly two-thirds were transferred directly from the ED (n=6,955), and 7% (n=710) were transferred more than once during their care. The proportion of severe sepsis patients transferred between hospitals increased by 2.8% (95%CI 2.6 – 3.1%) per year during the study period, and mortality fell by 0.7% (95%CI 0.5 – 0.9%) per year while the number of cases increased by 11.3% per year over the same time (Figure 3).
Figure 2.
Flow chart of study subjects. The italicized analyses listed at the bottom of the figure (with dashed arrows) highlight the statistical comparisons that are conducted with each comparator group. V-Code, an ICD-9 code associated with a procedure alone without an associated diagnosis (e.g., infusion therapy); Top-Decile Sepsis Volume, hospital in the top decile of inpatient sepsis volume; Sepsis-Capable ED, an emergency department that (1) is not a federally-designated critical access hospital, (2) has an intensive care unit, and (3) has an ED volume above the 25th percentile in state data; ED, emergency department.
Figure 3.
Change in inter-hospital transfer rate, total number of sepsis case, and sepsis-associated mortality over time, Iowa, 2005-2013. During the study period, the sepsis transfer rate was increasing and sepsis mortality was decreasing.
Patients in rural areas presented to smaller EDs than those in urban areas, but most patients were hospitalized in high-volume hospitals. Mortality was the highest for patients living in large rural areas (defined by RUCA methodology, Figure 4).
Figure 4.
Clinical outcomes stratified by rurality (based on Rural-Urban Commuting Area Codes). A. Mortality rate and transfer rate of patients, stratified by rurality of patient residence. B. Distribution of patients being cared for in EDs of hospitals in each sextile of ED volume stratified by rurality of residence. C. Distribution of patients being cared for inpatient status of hospitals in each sextile of hospital sepsis volume, stratified by rurality of residence. The largest hospitals are those in Sextile 6, while the smallest hospitals are in Sextile 1.
Univariate Analysis
Transferred patients were younger, more likely to have commercial insurance, and more likely to require surgery than those who were not transferred. Surgery may be related to transfer because of the need for specialized surgical services not available in many rural hospitals. Transferred patients also had higher mortality (20% vs. 12%, p<0.001) and had longer hospital length-of-stay (median 9 vs. 4 days, p<0.001). Mortality for those transferred from inpatient status was higher than those transferred from the ED (23% vs. 19%, p<0.001). Care for transferred patients was more costly than for patients who weren’t transferred ($13,486 additional cost, 95%CI $13,043-$13,941 2010$USD), with the majority of cost differences attributable to differences in inpatient medical costs (Table 1).
Table 1.
Baseline characteristics and outcomes of sepsis patients, stratified by inter-hospital transfer
| Factor |
Not Transferred (n =
7,445) |
Transferred (n =
10,801) |
p |
|---|---|---|---|
| Age, y (mean, SD) | 76.8 (15.3) | 66.3 (15.7) | < 0.001 |
| 18 – 50 y | 550 (7.4) | 1779 (16.5) | < 0.001 |
| 51 – 69 y | 1336 (17.9) | 4136 (38.3) | |
| 70 – 81 y | 2224 (29.9) | 3042 (28.2) | |
| Over 82 y | 3335 (44.8) | 1844 (17.0) | |
| Non-White, n (%) | 504 (6.7) | 1084 (10.0) | < 0.001 |
| Male, n (%) | 3552 (47.7) | 5646 (52.3) | < 0.001 |
| Rural Residence16, n (%) | 5484 (73.7) | 8450 (78.2) | < 0.001 |
| Primary Source of Health Insurance | < 0.001 | ||
| Medicare, n (%) | 6445 (86.6) | 7278 (67.4) | |
| Medicaid, n (%) | 237 (3.2) | 960 (8.9) | |
| Commercial, n (%) | 587 (7.9) | 1888 (17.5) | |
| Uninsured, n (%) | 106 (1.4) | 530 (4.9) | |
| Source of Infection15 | |||
| Pneumonia, n (%) | 2853 (38.2) | 3030 (28.1) | < 0.001 |
| Urinary Tract Infection, n (%) | 2381 (32.0) | 1807 (16.7) | |
| Cellulitis and Soft Tissue Infection, n (%) | 536 (7.2) | 834 (7.7) | |
| Other | 1675 (22.5) | 5130 (47.5) | |
| Surgery During Hospitalization (Broad Definition), n (%)34 |
935 (12.6) | 4158 (38.5) | < 0.001 |
| Comorbidities‡ (Elixhauser methodology)20 | |||
| Congestive Heart Failure, n (%) | 1746 (23.4) | 2820 (26.1) | < 0.001 |
| Valvular Heart Disease, n (%) | 390 (5.2) | 947 (8.8) | < 0.001 |
| Peripheral Vascular Disease, n (%) | 492 (6.6) | 1346 (12.5) | < 0.001 |
| Hypertension, n (%) | 3686 (49.5) | 6348 (58.8) | < 0.001 |
| Neurologic Disorders, n (%) | 1063 (14.3) | 1254 (11.6) | < 0.001 |
| Chronic Pulmonary Disease, n (%) | 1647 (22.1) | 3477 (32.2) | < 0.001 |
| Diabetes Mellitus with Complications, n (%) | 1362 (18.3) | 2703 (25.0) | < 0.001 |
| Renal Failure, n (%) | 1667 (22.4) | 3049 (28.2) | < 0.001 |
| Liver Disease, n (%) | 227 (3.1) | 808 (7.5) | < 0.001 |
| Metastatic Cancer, n (%) | 205 (2.8) | 425 (3.9) | < 0.001 |
| Distance21 | |||
| First Hospital, miles (SD) | 10.3 (18.3) | 10.2 (18.3) | 0.698 |
| Admitting Hospital, miles (SD) | 10.3 (18.3) | 59.6 (36.8) | < 0.001 |
| Top-Decile Sepsis-Volume Hospital, miles (SD) |
48.2 (34.0) | 41.7 (25.0) | < 0.001 |
| Transfer Distance, miles (SD) | 0 | 39.1 (47.8) | < 0.001 |
| Critical Access Hospital, n (%) | 5256 (71) | 6267 (58) | < 0.001 |
| Outcomes | |||
| Hospital Length-of-Stay, median (IQR) | 4 (3 – 7) | 9 (5 – 16) | < 0.001 |
| Cost of Care | |||
| ED Cost, $USD2010 (median, IQR) | $2,204 (1,331 – 3,504) |
$2,492 (1,409 – 3,955) |
< 0.001 |
| Ambulance Transfer Cost, $USD2010 (median, IQR) |
$0 | $763 (612 – 940) | < 0.001 |
| Inpatient Care Cost, $USD2010 (median, IQR) |
$6,041 (3,470 – 11,400) |
$20,928 (10,891 – 41,691) |
< 0.001 |
| Family Costs, $USD2010 (median, IQR) |
$0 | $205 (90 – 441) | < 0.001 |
| Total Cost of Care, $USD2010 (median, IQR) |
$7,709 (4,970 – 13,113) |
$23,344 (12,993 – 44,462) |
< 0.001 |
| Died | 894 (12.0) | 2188 (20.2) | < 0.001 |
y, years; SD, standard deviation; IQR, interquartile range; $USD2010, US Dollars with inflation indexed to 2010
For brevity, not all Elixhauser comorbidity variables are listed. The remaining variables either had very low prevalence or had no significant differences between cohorts.
Multivariable Mortality Models
GEE Model
Adjusting for potentially confounding covariates (i.e., age, year, ED cost, insurance, surgical intervention, inpatient sepsis volume, critical access hospital status, source of infection, and comorbidities) using a GEE model, inter-hospital transfer was associated with increased mortality (adjusted odds ratio = 1.72, 95%CI 1.53 – 1.94, Supplemental Table 1).
Instrumental Variables Model
Using an instrumental variables model, distance to a top-decile sepsis-volume hospital was a strong instrument (F-statistic 466, p<0.001). Inter-hospital transfer was associated with a 9.2% (95%CI 0.3 – 18.0%) increased risk of death (local average treatment effect), even when adjusting for the same covariates as in the GEE model (Table 2)
Table 2.
Instrumental variables model, predicting mortality. The instrument selected was distance to a top-decile sepsis-volume hospital to predict inter-hospital transfer.
| Factor | β (95%CI) | p |
|---|---|---|
| Inter-hospital Transfer | 0.092 (0.003 – 0.180) | 0.042 |
| Age, per decade increase | 0.021 (0.013 – 0.030) | <0.001 |
| Year | −0.016 (−0.019 – −0.012) | <0.001 |
| Insurance Type | 0.002 | |
| Medicare | 0 (ref) | |
| Medicaid | 0.010 (−0.029 – 0.051) | |
| Commercial | −0.005 (−0.034 – 0.024) | |
| Other Public Insurance | 0.024 (−0.057 – 0.105) | |
| Self-Pay/No Insurance | 0.074 (0.028 – 0.120) | |
| Surgery34 | 0.001 (−0.034 – 0.035) | 0.955 |
| Total ED Cost, per increase in $1000 2010$USD |
0.0013 (0.001 – 0.002) | 0.001 |
| High Inpatient Sepsis Volume† | −0.003 (−0.051 – 0.045) | 0.905 |
| Critical Access Hospital Status |
−0.023 (−0.048 – 0.001) | 0.061 |
| Infection Category15 | <0.001 | |
| Pneumonia | 0 (ref) | |
| Meningitis | −0.083 (−0.194 – 0.027) | |
| Abdominal | −0.041 (−0.079 – −0.003) | |
| Post-Operative | −0.073 (−0.139 – −0.007) | |
| Cellulitis/Soft Tissue | −0.056 (−0.089 – −0.023) | |
| Urinary | −0.063 (−0.084 – −0.041) | |
| Ear, nose, throat | 0.008 (−0.115 – 0.132) | |
| Bloodstream | −0.001 (−0.048 – 0.045) | |
| Osteomyelitis | −0.054 (−0.185 – 0.077) | |
| Diarrhea | −0.004 (−0.069 – 0.061) | |
| Other | 0.111 (0.086 – 0.136) |
First-stage F-statistic = 463.0
95%CI,95% confidence interval; ED, emergency department
Defined as greater than 1 case/month
Subgroup: Volume Effects
Stratifying on sextiles of total ED volume, the association between transfer and mortality is strongest for intermediate-sized hospitals (sextiles 2-5, Supplemental Figure 1), for which inter-hospital transfer was associated with an even larger increase in mortality (adjusted odds ratio = 2.17, 95%CI 1.79 – 2.62). Stratifying similarly on sextiles of inpatient sepsis-only volume, the association between transfer and mortality is similarly strongest for intermediate sized hospitals, and the inpatient sepsis volume association with mortality is even stronger than for ED volume (Supplemental Figure 1).
Subgroup: Sepsis Capable Hospitals
Limiting the data set to sepsis-capable hospitals, the effect of inter-hospital transfer on mortality remained significant (adjusted odds ratio = 1.40, 95%CI 1.18 – 1.66).
Multivariable Cost Models
GEE Model
The log-transformed costs were similar to the costs estimated from the linear model, so the linear estimates are provided for clarity. A multivariable GEE model suggested that inter-hospital transfer was associated with $6,897 (95%CI $5,769 – $8,024) in additional costs. Nearly all of this additional cost was attributable to inpatient care, with only $890 attributable to the ambulance costs and $141 attributable to family costs (Table 3).
Table 3.
Cost-based analysis, using both a linear model and log-transformed costs. The difference estimates from the linear model can be interpreted to be additional cost associated with inter-hospital transfer (difference in means). The estimates from the log-transformed cost model can be interpreted to be the ratio of costs (e.g., costs of care in patients who were transferred / costs of care in patients who were not transferred).
| Model (Cost of Transfer) |
Difference (95%CI) – Linear
Model ($USD2010) |
eβ (95%CI) = Log-
Transformed Cost Model |
|---|---|---|
| Unadjusted | ||
| Total Additional Cost | $13,486 ($13,043 – $13,941) | 2.834 (1.451 – 3.277) |
| Medical Cost | ||
| Emergency Department | $212 ($165 - $259) | 1.088 (1.010 – 1.172) |
| Inpatient Care | $12,776 ($12,330 – $13,234) | 3.236 (2.713 – 3.861) |
| Transport Costs | $763 ($612 – $940) | N/A |
| Family Costs | $205 ($90 – $441) | N/A |
| Model 1 (GEE Model, All Patients)† | ||
| Total Additional Cost | $6,897 ($5,769 – $8,024) | 1.389 (1.331 – 1.449) |
| Medical Cost | ||
| Emergency Department | $8 ($-102 - $117) | 1.031 (0.989 – 1.074) |
| Inpatient Care | $5,345 ($4,282 – $6,408) | 1.441 (1.370 – 1.516) |
| Transport Costs | $890 ($787-$993) | N/A |
| Family Costs | $141 ($126 - $155) | N/A |
| Model 2 (GEE Model, Admitted to | ||
| Top-Decile Sepsis Hospitals) † | ||
| Total Additional Cost | $5,268 ($3,737 – $6,799) | 1.361 (1.292 – 1.432) |
| Medical Cost | ||
| Emergency Department | −$10 ($-135 – $115) | 1.021 (0.975 – 1.069) |
| Inpatient Care | $5,167 ($3,696 – $6,638) | 1.396 (1.314 – 1.482) |
| Transport Costs | $744 ($727 – $761) | N/A |
| Family Costs | $168 ($148 - $189) | N/A |
Each multivariable model adjusts for age, insurance type, surgery, critical access hospital status, source of infection, comorbidities, and sepsis inpatient volume, clustered on inpatient hospital.
Subgroup: Top-Decile Sepsis Volume Hospitals
Among those who received inpatient care at top-decile sepsis hospitals, inter-hospital transfer continued to be associated with increased costs (additional cost $5,268, 95%CI $3,737 – $6,799).
Discussion
Regionalization, or transferring patients to high-volume centers for specialized care, has been well described as a strategy to improve survival for many high risk conditions, including trauma, stroke, and ST-elevation myocardial infarction (STEMI) care.7-11 In contrast to trauma and STEMI care, however, sepsis has no specific procedural intervention that requires transfer. Early resuscitation is critical to survival, and inter-hospital transfer during the critical period of resuscitation may delay appropriate time-sensitive therapy for a benefit that is not as time-critical.14
While many studies have examined the effects of hospital volume on patient outcomes, ours is the first to evaluate whether regionalization can achieve outcomes similar to presenting to a high-volume hospital. Three previous studies have reported lower mortality in hospitals that treat more sepsis patients, but each of these studies excluded transferred patients.6, 12, 13 Whereas these studies compare sepsis outcomes between patients who initially present to high-volume hospitals compared to those who present to low-volume hospitals26, our analysis compares outcomes between those who are transferred to those who aren’t transferred, regardless of the characteristics of the index hospital.
Although these results seem to be an indictment of the decision to transfer, they explain previous research in this area. These findings may simply be a result of delays in early sepsis care. We have shown previously that transferred sepsis patients have lower adherence with Surviving Sepsis Campaign Guidelines and that inter-hospital transfer itself is associated with significant delays in sepsis care.14, 27 Our findings may simply be a reflection that delays in sepsis care translate to worse clinical outcomes, and that transferred patients have systematic delays in their resuscitation. This justification also may explain why inpatient transfers were at even higher risk of mortality: if sepsis resuscitation were delayed further, patients may have decompensated prior to transfer and experienced worse outcomes. The systemic factors that allow hospitals to care for patients on the margin (e.g., those patients who benefit from aggressive early care but who would be transferred from smaller hospitals) may be magnifying the detrimental effect of transfer in intermediate-sized hospitals. These findings, in aggregate, may suggest that realizing the benefits of higher volume hospital care may only be apparent if transfer is conducted after high quality sepsis care is delivered in rural hospitals.
How should these findings influence the development of systems of care for rural sepsis patients? Currently, national adherence with Surviving Sepsis Campaign guidelines is low, and rural sepsis patients often do not receive guideline-adherent sepsis care.14, 28-32 We showed previously that transferred patients had hospital admission delayed nearly 6 hours, and that appropriate empiric antibiotics were administered prior to transfer in only one-third of cases.14 If inter-hospital transfer is to be the most effective strategy for improving population-based outcomes, perhaps transfer must occur more rapidly (median time in ED prior to transfer was 3.6 h). Alternatively, bolstering rural resuscitation algorithms, either through standard care pathways, electronic order sets, or telemedicine may improve the quality of rural resuscitation. In the latter case, timeliness of transfer may be significantly less important than early care, although this has not yet been proven. Based on prior studies and international guidelines, Table 4 suggests some elements of rural sepsis care that may be most important prior to transfer.
Table 4.
Suggested elements of rural sepsis protocols in patients who are being transferred between hospitals
|
Our study is also the first to report the system-wide costs of inter-hospital transfer. Although estimates have been derived from medical costs alone using single institution data among ICU patients33, those estimates have been limited by significant selection bias. Although transfer was associated with $6,897 in additional costs in all Iowa hospitals, limiting to the cohort ultimately treated in one of Iowa’s highest volume hospitals dropped the incremental cost to $5,268 (24% reduction). Presumably, the $5,268 is the cost associated with transfer itself (i.e., transportation, family costs, repeated ED evaluation, repeated tests and imaging), while the additional 24% in all hospitals may be partially attributable to efficiencies in care at high volume hospitals that treat a large number of these patients. Interestingly, the $5,268 mirrors closely the increased cost previously shown in an analysis of patients transferred into a single tertiary academic hospital.33
This study has a few important limitations. First, as an observational study of medical claims data, our sample is limited by data that is available for billing. Severe sepsis and septic shock are inconsistently coded in administrative data, so we used an accepted alternative definition that has been validated from billing codes.15 Physiologic severity of illness indices and other clinical data are also not available from administrative data, so we have used comorbidity indices, subgroup analyses, and instrumental variables to provide several estimates to adjust for severity of illness in sepsis patients. We also have no data on the method of transport, although air transfer for sepsis was rare in a previous study of transferred sepsis patients.14 The 79% linkage rate could introduce bias in our findings if inter-hospital transfer affects linked differently than those that are not. We think this is unlikely because many of these failed linkages we believe are associated with transfer across the state border, but it is impossible to test this hypothesis in our data. Finally, there could be additional family-associated costs (e.g., lost wages) that may be higher in transferred patients but that are not included in our model. We have elected to choose a more conservative estimate because we can be more certain about these costs, but additional costs may not be fully represented in our model.
Our results are internally consistent using multiple analytic approaches and they are consistent with prior published data suggesting that pre-transfer sepsis bundle adherence is lacking14, lending face validity to our findings. The consistency of the result is reassuring and likely reflects that transferred sepsis patients bear actual additional risk from inter-hospital transfer itself.
Conclusions
In conclusion, the majority of severe sepsis and septic shock patients are transferred between hospitals in a rural state. Sepsis patients who are transferred continue to have higher mortality than those who present initially to high-volume hospitals, even when accounting for comorbidities using a GEE model and unmeasured confounders using an instrumental variables approach. Hospital factors contribute to survival for sepsis patients, and the decisions made in the ED (both decisions about care and the decision to transfer) clearly impact survival. Future studies should focus on defining appropriate timing for transfer, risk-stratifying patients to identify those who benefit most from transfer, and defining resource requirements for optimal care of sepsis patients during the early part of their episode of care.
Supplementary Material
Acknowledgements
The authors would like to acknowledge Zachary Miller, Oluwole Akintayo, MD, Shannon Findlay, MD, Olga Kravchuk, MD, and Andrew Stoltze, MD for their assistance with data collection. The authors would also like to acknowledge Craig Jarvie and Sara Hayes for their help in providing and interpreting the discharge data sets. The authors would like to acknowledge research funding from the Emergency Medicine Foundation Research Fellowship, the University of Iowa Department of Emergency Medicine, and the University of Iowa Institute for Clinical and Translational Sciences, which is supported by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant U54TR001356. Dr. Mohr is additionally supported by funding from the Rural Telemedicine Research Center, funded by the Federal Office of Rural Health Policy (Health Resources and Services Administration grant 1U1CRH29074).
Funding: This work was supported by the Emergency Medicine Foundation; by the University of Iowa Department of Emergency Medicine; and by the Institute for Clinical and Translational Science at the University of Iowa, which is supported by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant U54TR001356. Dr. Mohr is additionally supported by funding from the Rural Telemedicine Research Center, funded by the Federal Office of Rural Health Policy (Health Resources and Services Administration grant 1U1CRH29074).
List of Abbreviations
- 2010$USD
U.S. Dollars, indexed to 2010 values
- 95%CI
95% confidence interval
- API
Application programming interface
- aOR
Adjusted odds ratios
- BIC
Bayesian information criteria
- ED
Emergency department
- GEE
Generalized estimating equations
- ICD-9-CM
International Classification of Diseases, 9th edition, Clinical Modification
- RUCA
Rural Urban Commuting Areas
- STEMI
ST-elevation myocardial infarction
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests: The authors have no competing interests to report.
Contributor Information
Nicholas M. Mohr, Department of Emergency Medicine, Division of Critical Care, Department of Anesthesia, University of Iowa Carver College of Medicine, 200 Hawkins Drive, 1008 RCP, Iowa City, IA 52242, nicholas-mohr@uiowa.edu.
Karisa K. Harland, Department of Emergency Medicine, University of Iowa Carver College of Medicine, 200 Hawkins Drive, 1008 RCP, Iowa City, IA 52242, kari-harland@uiowa.edu.
Dan M. Shane, Department of Health Management and Policy, University of Iowa College of Public Health, 145 N. Riverside Drive, N244 CPHB, Iowa City, IA 52242, dan-shane@uiowa.edu.
Azeemuddin Ahmed, Department of Emergency Medicine, University of Iowa Carver College of Medicine, 200 Hawkins Drive, 1008 RCP, Iowa City, IA 52242, azeemuddin-ahmed@uiowa.edu.
Brian M. Fuller, Division of Critical Care, Department of Anesthesia, Division of Emergency Medicine, One Brookings Drive, CB 8072, St. Louis, MO 63130, fullerb@wustl.edu.
James C. Torner, Department of Epidemiology, University of Iowa College of Public Health, 145 N. Riverside Drive, S441A CPHB, Iowa City, IA 52242, james-torner@uiowa.edu.
References
- 1.Hall MJ, Williams SN, DeFrances CJ, et al. Inpatient care for septicemia or sepsis: A challenge for patients and hospitals. National Center for Health Statistics; Hyattsville, MD: 2011. [PubMed] [Google Scholar]
- 2.Filbin MR, Arias SA, Camargo CA, Jr., et al. Sepsis visits and antibiotic utilization in U.S. emergency departments. Crit Care Med. 2014;42:528–535. doi: 10.1097/CCM.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 3.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 4.Rivers EP. Point: adherence to early goal-directed therapy: does it really matter? Yes. After a decade, the scientific proof speaks for itself. Chest. 2010;138:476–480. doi: 10.1378/chest.10-1405. discussion 484-475. [DOI] [PubMed] [Google Scholar]
- 5.Stevenson EK, Rubenstein AR, Radin GT, et al. Two Decades of Mortality Trends Among Patients With Severe Sepsis: A Comparative Meta-Analysis. Crit Care Med. 2014;42:625–631. doi: 10.1097/CCM.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kocher KE, Haggins AN, Sabbatini AK, et al. Emergency Department Hospitalization Volume and Mortality in the United States. Ann Emerg Med. 2014;64:446–457. doi: 10.1016/j.annemergmed.2014.06.008. [DOI] [PubMed] [Google Scholar]
- 7.Heffner AC, Pearson DA, Nussbaum ML, et al. Regionalization of post-cardiac arrest care: implementation of a cardiac resuscitation center. Am Heart J. 2012;164:493–501. doi: 10.1016/j.ahj.2012.06.014. e492. [DOI] [PubMed] [Google Scholar]
- 8.Dalby M, Bouzamondo A, Lechat P, et al. Transfer for primary angioplasty versus immediate thrombolysis in acute myocardial infarction: a meta-analysis. Circulation. 2003;108:1809–1814. doi: 10.1161/01.CIR.0000091088.63921.8C. [DOI] [PubMed] [Google Scholar]
- 9.Kim DH, Cha JK, Bae HJ, et al. Organized Comprehensive Stroke Center is Associated with Reduced Mortality: Analysis of Consecutive Patients in a Single Hospital. J Stroke. 2013;15:57–63. doi: 10.5853/jos.2013.15.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.LaMonte MP, Bahouth MN, Magder LS, et al. A regional system of stroke care provides thrombolytic outcomes comparable with the NINDS stroke trial. Ann Emerg Med. 2009;54:319–327. doi: 10.1016/j.annemergmed.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 11.Garwe T, Cowan LD, Neas B, et al. Survival benefit of transfer to tertiary trauma centers for major trauma patients initially presenting to nontertiary trauma centers. Acad Emerg Med. 2010;17:1223–1232. doi: 10.1111/j.1553-2712.2010.00918.x. [DOI] [PubMed] [Google Scholar]
- 12.Powell ES, Khare RK, Courtney DM, et al. Volume of emergency department admissions for sepsis is related to inpatient mortality: results of a nationwide cross-sectional analysis. Crit Care Med. 2010;38:2161–2168. doi: 10.1097/CCM.0b013e3181f3e09c. [DOI] [PubMed] [Google Scholar]
- 13.Gaieski DF, Edwards JM, Kallan MJ, et al. The relationship between hospital volume and mortality in severe sepsis. Am J Respir Crit Care Med. 2014;190:665–674. doi: 10.1164/rccm.201402-0289OC. [DOI] [PubMed] [Google Scholar]
- 14.Faine BA, Noack JM, Wong T, et al. Interhospital Transfer Delays Appropriate Treatment for Patients With Severe Sepsis and Septic Shock: A Retrospective Cohort Study. Crit Care Med. 2015;43:2589–2596. doi: 10.1097/CCM.0000000000001301. [DOI] [PubMed] [Google Scholar]
- 15.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Trezzi M, Torzillo D, Ceriani E, et al. Lung ultrasonography for the assessment of rapid extravascular water variation: evidence from hemodialysis patients. Intern Emerg Med. 2013;8:409–415. doi: 10.1007/s11739-011-0625-4. [DOI] [PubMed] [Google Scholar]
- 17.Cromartie J. Rural-Urban Commuting Area (RUCA) Codes. 2010 Available at: http://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx (accessed: 18 Oct 2015)
- 18.Southern DA, Quan H, Ghali WA. Comparison of the Elixhauser and Charlson/Deyo methods of comorbidity measurement in administrative data. Med Care. 2004;42:355–360. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- 19.Mehta HB, Dimou F, Adhikari D, et al. Comparison of Comorbidity Scores in Predicting Surgical Outcomes. Med Care. 2016;54:180–187. doi: 10.1097/MLR.0000000000000465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elixhauser A, McCarthy EM. Clinical Classifications Software (CCS) for ICD-9-CM. Available at: http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp (accessed: June 2015)
- 21.Google Maps APIs. Available at: https://developers.google.com/maps/?hl=en (accessed: February 2015)
- 22.Consumer Price Index - Medical Care. Available at: http://data.bls.gov/timeseries/CUUR0000SAM? (accessed: March 2015)
- 23.Cost-to-Charge Ratio Files. Available at: www.hcup-us.ahrq.gov/db/state/costtocharge.jsp (accessed: Dec 2015)
- 24.IRS Announces 2010 Standard Mileage Rates. Available at: https://www.irs.gov/uac/IRS-Announces-2010-Standard-Mileage-Rates (accessed: March 2015)
- 25.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen Y-L, Wallace DJ, Yordanov Y, et al. The volume-outcome relationship in critical care: A systematic review and meta-analysis. Chest. 2015;148:79–92. doi: 10.1378/chest.14-2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dellinger RP, Levy M, Rhodes A, et al. Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock, 2012. Intensive Care Medicine. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glickman SW, Krubert C, Koppenhaver J, et al. Increased rate of central venous catheterization procedures in community EDs. Am J Emerg Med. 2010;28:208–212. doi: 10.1016/j.ajem.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 29.Djogovic D, Green R, Keyes R, et al. Canadian Association of Emergency Physicians sepsis treatment checklist: optimizing sepsis care in Canadian emergency departments. CJEM. 2012;14:36–39. doi: 10.2310/8000.2011.110610. [DOI] [PubMed] [Google Scholar]
- 30.Salhi RA, Edwards JM, Gaieski DF, et al. Access to Care for Patients With Time-Sensitive Conditions in Pennsylvania. Ann Emerg Med. 2013 doi: 10.1016/j.annemergmed.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 31.Burenheide K. Developing Disease State Management Guidelines for Rural Health Care. Midwest Critical Care Collaborative; Topeka, Kansas: 2008. [Google Scholar]
- 32.Kaukonen K, Bailey M, Suzuki S, et al. MOrtality related to severe sepsis and septic shock among critically ill patients in australia and new zealand, 2000-2012. JAMA. 2014;311:1308–1316. doi: 10.1001/jama.2014.2637. [DOI] [PubMed] [Google Scholar]
- 33.Bernard AM, Hayward RA, Rosevear J, et al. Comparing the hospitalizations of transfer and non-transfer patients in an academic medical center. Acad Med. 1996;71:262–266. doi: 10.1097/00001888-199603000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Surgery Flag Software. Agency for Healthcare Research and Quality; Rockville, Maryland: Available from: http://www.hcup-us.ahrq.gov/toolssoftware/surgflags/surgeryflags.jsp (accessed 6 Dec 2015) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Because this study was conducted with protected health information that could allow identification of study participants under waiver of informed consent, the data set upon which the conclusions were based is not publicly available.