Abstract
Background
Poor diabetes self-care can have a negative impact on psychological well-being and quality of life. Given the scarcity of traditional psychological support and the barriers to uptake of and attendance at face-to-face education programs, Web-based interventions are becoming a popular approach to provide an additional platform for psychological support in long-term conditions. However, there is limited evidence to assess the effect of Web-based psychological support in people with type 2 diabetes.
Objective
This systematic review is the first review to critically appraise and quantify the evidence on the effect of Web-based interventions that aim to improve well-being in people with type 2 diabetes.
Methods
Searches were carried out in the following electronic databases: MEDLINE, EMBASE, CINAHL, PsycINFO, and Cochrane Library. Reference lists were hand-searched. A meta-analysis was conducted for depression and distress outcomes.
Results
A total of 16 randomized controlled studies met the inclusion criteria for the systematic review and 9 were included in the meta-analyses. Theories were applied to the majority of the interventions. The most common behavior change techniques were “General information” and “Tracking/monitoring.” Interventions with a duration of 2-6 months providing professional-led support with asynchronous and synchronous communication appeared to be associated with significant well-being outcomes. The pooled mean (95% confidence interval) difference between the intervention and control arms at follow-up on depression score was -0.31 (-0.73 to 0.11). The pooled mean difference on distress scores at follow-up was -0.11 (-0.38 to 0.16). No significant improvements in depression (P=.15) or distress (P=.43) were found following meta-analyses.
Conclusions
While the meta-analyses demonstrated nonsignificant results for depression and distress scores, this review has shown that there is a potential for Web-based interventions to improve well-being outcomes in type 2 diabetes. Further research is required to confirm the findings of this review.
Keywords: type 2 diabetes, Web-based intervention, Internet, well-being, systematic review, meta-analysis
Introduction
Diabetes has become a global health concern, with 415 million people estimated to be living with diabetes worldwide. This figure is estimated to rise to around 642 million by 2040, with approximately 90% of those cases being type 2 diabetes mellitus [1-3]. Despite a growing number of treatment and therapy options available to people with type 2 diabetes, the number of diabetes-related complications continues to rise [4]. Risk of such complications can be reduced by making appropriate lifestyle changes in addition to diabetes therapies [5]. However, for some, making these changes can become overwhelming, as they must adjust to a new lifestyle and live with diabetes for the rest of their life [6-8]. National and international surveys highlight that poor diabetes self-care and the daily demands of diabetes management can lead to low quality of life and poor well-being [9-12]. The prevalence of poor psychological health is evident, with depression twice as common in people with type 2 diabetes, than those without the condition [13-16], and with distress affecting 10-30% of people with type 2 diabetes [17], leading to poor glycemic control, medication adherence, and overall low health outcomes [18-22].
Well-Being
The Diabetes Management and Impact for Long-term Empowerment and Success report defines well-being as how satisfied an individual is with their quality of life. Other sources state that quality of life is not the end-all definition of well-being but is in fact one of many elements of well-being [23]. The World Health Organization defines well-being as when an individual “…can cope with the normal stresses in life, can work productively and is able to make a contribution to his/her community” [24], whereas the National Institute for Health and Care Excellence guidelines define well-being as when a person is happy and confident with no feelings of anxiety or depression, managing their feelings and emotions and being resilient [25].
It is evident that well-being remains a complex, multifaceted construct that is used interchangeably with various definitions existing across the literature demonstrating subjectively experienced domains and constructs [26,27]. The unclear definition of well-being creates difficulties in measuring this construct, and as a consequence, there are currently numerous questionnaires that measure a wide range of psychological constructs that include aspects of well-being, such as depression, distress, and quality of life [26].
Web-Based Programs
Diabetes self-management education, including structured education and behavior change programs, can prevent or prolong diabetes-related complications [28,29]. However, there is a reported gap in these services’ provision of support focusing on well-being [10,30]. Attendance rates at self-management programs are reported to be low due to logistical or infrastructure issues that may contribute to low uptake [31,32]. Given the scarcity of psychological support provided through local services and the barriers to uptake at traditional education programs, Web-based interventions are becoming an additional or alternative provider of support to people with long-term conditions, including type 2 diabetes [33-36].
Evidence on Web-Based Interventions in Type 2 Diabetes and Well-Being
Web-based interventions are described as self-guided programs that aim to change and improve knowledge and awareness around a health condition. Evidence indicates that such interventions are cost-effective, able to reach a wide range of audiences, especially those with a more restrictive lifestyle [37,38]. Recent reviews of Web-based interventions in type 2 diabetes have suggested positive impacts for outcomes of depression and anxiety [35,39]. Other studies and meta-analyses that looked at Web-based interventions for depression also reported effectiveness in elevating lowered mood [40,41]. Some recent reviews, however, have demonstrated no significant improvement in depression or distress [33,34]. Overall, current literature illustrates that there is limited evidence around the effect of such interventions on well-being in people with type 2 diabetes.
According to Corbin and Strauss, self-management programs, whether face-to-face or online, must consist of three constructs: medical, emotional, and role management. For example, they must include tasks around medical or diet adherence (medical self-management), tasks in changing or maintaining new behavioral/life roles within social relationships (role management), or tasks in coping with the emotional burden of living with a long-term condition (emotional management) [42]. To our knowledge, existing reviews mostly focus on medical management [43]. For instance, a recent review that explored online self-management interventions around lifestyle modification examined outcomes that were behavioral (role) and physiological (medical), excluding psychological and emotional management [44].
The aim of this paper is to report the first systematic review to identify and evaluate the current literature on Web-based programs or interventions for emotional management in type 2 diabetes and their impact on well-being.
Methods
Reporting Standards
This systematic review has been registered on PROSPERO (No. CRD42015020281) and meets the requirements of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [45].
Data Sources and Search Methods
The search strategy was carried out to identify relevant studies using the following five databases: MEDLINE, Embase, CINAHL, PsycINFO, and Cochrane Library.
Databases were searched using a combination of Medical Subject Headings (MeSH) topics and free-text terms. An example of the full electronic search strategy used for the databases is included in Multimedia Appendix 1. Publication year was between 1995 and 2016; this limitation was based on the recognition that the Internet became mainstream in 1995 with the launch of Windows 95; therefore, any use of the Internet prior to 1995 would not have met the study criteria [46].
After conducting the search, duplicates were removed and 2 reviewers (MH and JB) independently checked the titles and abstracts. The full text of the remaining papers was retrieved and again independently assessed for inclusion by the same 2 reviewers. Discrepancies were resolved through a third reviewer (DB). Reference lists of included papers were hand-searched. Experts in this topic area were contacted to ensure recent publications were included in this review.
Study Selection
We included studies that were randomized controlled trials (RCTs), including RCT feasibility or pilot studies, with a follow-up of at least 2 months (8 weeks). Due to inconsistent usage of the term “well-being” across the literature and to ensure that no relevant papers were omitted and that the deficits and assets of the term “well-being” were captured, it was decided to use “well-being” as an umbrella term and include the following outcomes: well-being, distress, depression, anxiety, quality of life, self-efficacy, and social support. We incorporated studies that used validated tools to measure the above outcomes.
For the purpose of this review, Web-based interventions are defined as an intervention that may comprise modules or can be a health-related website that aims to change an outcome. Studies were included if they evaluated one Web-based/online intervention, with a combination of other modes, such as telephone calls or SMS (short message service) texts, that provided information, education, peer support, and/or overall therapeutic components to people with type 2 diabetes over the age of 18 years. Studies with any participants with type 2 diabetes (including studies with both type 1 diabetes and type 2 diabetes) were included in the review. Studies were excluded if they were computer-based and not Internet-based, such as studies using a computer for glucose monitoring. Also, studies were excluded if they were not RCTs and if they did not measure well-being or its constructs as a primary or secondary outcome.
Data Extraction and Quality Assessment
An appropriate quality assessment tool was used to assess the validity of the methodology following the Centre for Reviews and Dissemination guidelines [47]. The quality appraisal checklist, the Jadad scale, is used to help assess the quality of the design and conduct of RCTs. The Jadad scale is a 7-item scale and consists of questions indicating whether the quality of the trial is good or poor. Despite the negative criticism of this scale around allocation concealment, this scale has a strong emphasis on the report of trials and was considered appropriate for the review of RCTs [48]. The quality assessment was carried out independently by 2 researchers (MH and JB). A third assessor was consulted in the case of a disagreement (DB).
A standardized data extraction form was used for this review. Qualitative information, including a summary of the interventions and results, was extracted separately. Two reviewers (MH and JB) independently extracted the data and discussed any discrepancies. Where data were missing for the meta-analysis, authors of the eligible studies were contacted.
Data Synthesis
Due to the heterogeneity of the study designs, interventions, and outcomes, qualitative data were summarized and collated using a descriptive data synthesis. Due to the inconsistency of outcome measures across the studies, a meta-analysis was carried out for two outcomes (ie, depression and distress), as these outcomes were reported in the majority of the studies. Both depression and distress were treated as separate constructs. Measures that were used for depression and distress were validated and were as follows. For depression, we included studies that used questionnaires such as the Center for Epidemiologic Studies Depression Scale (CES-D), the Patient Health Questionnaire (PHQ-9), or the Hospital Anxiety and Depression Scale (HADS). For distress, we included studies that used questionnaires such as the Problem Areas in Diabetes Questionnaire (PAID), the Diabetes Distress scale (DDS), or the Health Distress Scale (HDS).
Pooled mean depression and distress scores were estimated separately using random-effects meta-analysis to account for the large heterogeneity that was observed. Standardized means were used to account for the different scales used to measure depression and distress. Publication bias was assessed using the Egger test, and heterogeneity was assessed using the I2statistic. There were insufficient data to allow subgroup analyses or meta-regression analyses to be performed.
Sensitivity analyses were performed by pooling means depression and distress scores: (1) excluding pilot/feasibility studies, and (2) excluding trials with type 1 diabetes and type 2 diabetes.
All analyses were performed in Stata version 14 (StataCorp), using the METAN command for continuous data.
Results
Study Selection
The search identified 1172 potentially eligible articles (Figure 1). Of these, 63 full texts were assessed for eligibility. Figure 1 illustrates the main reasons for exclusion of articles. Three papers by different first authors reported the same study with identical study population [49-51]; therefore, only one paper was included in the review [50]. A total of 16 studies met the predefined criteria and were included in the review [50,52-66] (Figure 1).
Figure 1.
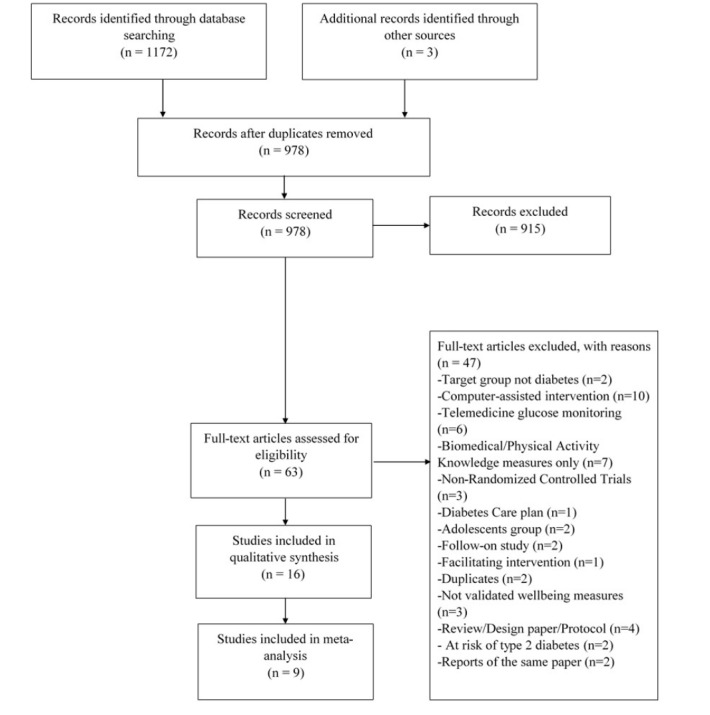
Study selection process.
Study Characteristics
A total of 15 studies used a parallel RCT design, with one study using a crossover design [52]. We identified 14 studies that recruited patients diagnosed with type 2 diabetes [50,52,54-65], while four out of those studies recruited participants with both type 2 diabetes and type 1 diabetes [60,61,63,64]. Two studies did not specify the type of diabetes [53,66]. Studies were reported between 2002 and 2015 and were predominantly based in the United States (n=12), with one study carried out in each of the following countries: Canada [65], Norway [63], Germany [60], and the Netherlands [61]. The total number of participants across the studies was 3612 with a range of 17-761 (mean 220.32, SD 172.15). All 16 studies recruited more women (2208/3612, 61.13%) than men (1404/3612, 38.87%). The mean age across the studies was 53.4 years (range 23.9-67.2 years). Seven out of 16 studies (47%) reported having a predominantly white population (Table 1). A total of six studies (40%) did not report the ethnicity of their study population [57,58,62-64]. The interventions and control groups are described in Multimedia Appendix 2.
Table 1.
Characteristics of the studies included in the review.
| Study (year) and location | Name of intervention | Well-being outcome | Type of diabetes | Duration of intervention, months | Total N | Usage over time |
| Bond (2010) USA [53] | — | Depression Self-efficacy Quality of life Social support |
Not specified | 6 | 62 | Not reported |
| Tang (2013) USA [54] | EMPOWER-D | Depression Distress |
Type 2 | 12 | 415 | Not reported |
| Heisler (2014) USA [55] | iDecide | Distress Self-efficacy |
Type 2 | 3 | 188 | Not reported |
| Glasgow (2012) USA [56] | CASM | Quality of life Self-efficacy |
Type 2 | 12 | 463 | Declined |
| McMahon (2012) USA [57] | — | Distress | Type 2 | 12 | 151 |
|
| McKay (2001) USA [50] | D-Net | Depression | Type 2 | 2 | 78 | Declined |
| McKay (2002) USA [58] | D-Net | Depression Quality of life |
Type 2 | 3 | 160 | Declined |
| Lorig (2010) USA [59] | IDSMP | Depression Distress Self-efficacy |
Type 2 | 6-18 | 761 | Not reported |
| Nobis (2015) Germany [60] | GET.ON Mood | Depression Distress |
Both types 1 and 2 (76% T2Da) | 2 | 260 | — |
| Van Bastelaar (2011) Netherlands [61] | — | Depression Distress |
Both types 1 and 2 (82% T2D) | 2 | 255 | Not reported |
| Fisher (2013) USA [62] | REDEEM (CASM) | Distress | Type 2 | 12 | 392 | Not reported |
| Wangberg (2008) Norway [63] | — | Self-efficacy | Both types 1 and 2 (28% T2D) | 1 | 64 | — |
| Hunt (2014) USA [52] | — | Self-efficacy | Type 2 | 3 | 17 | Not reported |
| Smith (2000) USA [64] | Women to Women | Quality of life Social Support |
Both types 1 and 2 (80% T2D) | 5 | 30 | Declined |
| Pacaud (2012) Canada [65] | — | Quality of life Self-efficacy |
Type 2 | 12 | 68 | Not reported |
| Fonda (2009) USA [66] | MyCare Team | Distress | Not specified | 12 | 104 | Not reported |
aT2D: type 2 diabetes
Methodological Quality Assessment
The methodological quality of the studies was generally high (Table 2). Nevertheless, some aspects, such as intention-to-treat, single-blinding, and sample size calculation, were not clearly reported in some studies.
Table 2.
Methodological quality assessment per intervention.
| Study (year) | Criteria | |||||||
|
|
Eligibility criteria | Method of randomization | Single-blinded | Description of intervention | Description of withdrawals | Timing of assessment | Sample size calculation | Intention-to-treat analysis |
| Bond (2010) [53] | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | x |
| Tang (2013) [54] | ✓ | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ |
| Heisler (2014) [55] | x | ✓ | x | ✓ | ✓ | ✓ | ✓ | x |
| Glasgow (2012) [56] | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | ✓ |
| McMahon (2012) [57] | ✓ | ✓ | x | ✓ | ✓ | ✓ | x | ✓ |
| McKay (2001) [50] | ✓ | ✓ | x | ✓ | ✓ | ✓ | x | x |
| McKay (2002) [58] | ✓ | x | x | ✓ | ✓ | ✓ | x | x |
| Lorig (2010) [59] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | x |
| Nobis (2015) [60] | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | x |
| Van Bastelaar (2011) [61] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Fisher (2013) [62] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | x | x |
| Wangberg (2008) [63] | ✓ | x | x | ✓ | x | x | ✓ | x |
| Hunt (2014) [52] | ✓ | ✓ | x | ✓ | ✓ | ✓ | x | x |
| Smith (2000) [64] | ✓ | ✓ | x | ✓ | ✓ | ✓ | x | x |
| Pacaud (2012) [65] | x | x | x | x | x | ✓ | x | ✓ |
| Fonda (2009) [66] | x | x | x | ✓ | x | ✓ | x | x |
Descriptive Data Synthesis
The most common duration of the interventions was 12 months [54,56,57,62,65,66]. Compliance rates ranged between 42-100%, while attrition rates were reported by the majority of the studies (n=13); these ranged from 6-22%. A few studies (n=4) reported a decline of intervention adherence over time [50,56,58,64]; reporting that the usage declined over 8 weeks [50], 5 months [64], and 12 months [56] (Table 1).
Modes of Communication and Type of Intervention Providers
The communication between intervention provider and/or peers was synchronous (eg, telephone calls) and/or asynchronous (eg, bulletin boards). Intervention providers were those involved in running the online intervention and often had direct or indirect contact with the users. They varied across the studies as follows: psychologists (n=4), nurses (n=6), dieticians (n=3), diabetes educators (n=2), coaches (n=2), social worker (n=1), physician (n=1), pharmacist (n=1), and endocrinologist (n=1). Two studies included nonprofessional providers [59,62], such as lay people and graduates, whereas three studies failed to report any characteristics of their intervention providers [55,63,65].
10 studies provided both asynchronous and synchronous communication [53,56-60,62,64-66], whereas six studies provided communication both with providers and other users [50,53,56,59,64,65]. Out of the seven studies that provided peer support, four were moderated [56,58,59,64], one was not moderated [53], and two studies did not report on moderation [50,65]. The intervention modules varied between 6-8 sessions. Half the studies specified the duration of their modules (which were online sessions); these varied from 45-120 minutes [54-56,59-62,65].
Theories and Behavior Change Techniques
Six studies failed to report whether their intervention was theory based [42,53,57,64-66]. The remaining ten studies were based on at least one theory: the Chronic Care Model [54], Motivational Interviewing [55,62], Social Cognitive Theory [56,63], Social Ecological Model [50,56], Self-Efficacy Theory [58], Social Support Theory [51], Systematic Behavioral Activation [60], Cognitive Behavioral Theory [61], or Self-Determination Theory [52].
All studies explicitly reported at least one behavior change technique, which we attempted to map onto Michie’s taxonomy [67] as follows: information provision (n=14); tracking/self-monitoring (n=12); providing motivation (n=12); providing feedback (n=9); goal setting (n=9); problem solving (n=9); action planning (n=7); social support (n=7); emotional control training (n=6); and prompt review of behavioral goals (n=1) (Table 3).
Table 3.
Behavior change techniques used in interventions.
| Study (year) | Behavior change techniques | |||||||||
|
|
General information | Goal setting | Action planning | Problem solving/ barrier | Prompt review of behavioral goals | Prompt self-monitoring/ tracking | Social support | Emotional control training | Motivational approach | Provide feedback on performance |
| Bond (2010) [53] | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | x |
| Tang (2013) [54] | ✓ | ✓ | ✓ | x | x | x | x | ✓ | ✓ | x |
| Heisler (2014) [55] | ✓ | ✓ | ✓ | ✓ | x | ✓ | x | x | ✓ | x |
| Glasgow (2012) [56] | ✓ | ✓ | ✓ | ✓ | x | ✓ | ✓ | x | ✓ | ✓ |
| McMahon (2012) [57] | ✓ | x | x | x | ✓ | ✓ | x | x | ✓ | ✓ |
| McKay (2001) [50] | x | ✓ | ✓ | ✓ | x | ✓ | ✓ | x | ✓ | ✓ |
| McKay (2002) [58] | ✓ | ✓ | x | ✓ | x | ✓ | ✓ | ✓ | ✓ | ✓ |
| Lorig (2010) [59] | ✓ | x | ✓ | ✓ | x | ✓ | ✓ | ✓ | ✓ | x |
| Nobis (2015) [60] | ✓ | ✓ | x | ✓ | x | x | x | ✓ | ✓ | ✓ |
| Van Bastelaar (2011) [61] | ✓ | x | x | x | x | x | x | x | x | ✓ |
| Fisher (2013) [62] | x | ✓ | ✓ | ✓ | x | ✓ | x | x | ✓ | ✓ |
| Wangberg (2008) [63] | ✓ | x | x | x | x | x | x | x | x | ✓ |
| Hunt (2014) [52] | x | x | x | x | x | ✓ | x | x | x | x |
| Smith (2000) [64] | ✓ | x | x | x | x | x | ✓ | x | x | x |
| Pacaud (2012) [65] | ✓ | x | x | x | x | ✓ | ✓ | x | x | x |
| Fonda (2009) [66] | ✓ | x | x | x | x | ✓ | x | x | x | x |
Outcomes and Measures
There was a variety of questionnaires used across studies to measure the same outcome. For depression, the following measures were used: CES-D [50,53,58,60,61], PHQ-9 [54,59], and HADS [60]. For distress, studies used PAID [54,57,60,61,66], DDS [55,62], and HDS [59]. Quality of life was assessed by using PAID [53], DDS [56], the Short Form-12 (SF-12) [58], the Quality of Life Index (QoL Index) [64], and the Diabetes Quality of Life Questionnaire [65]. Social support was assessed using the Diabetes Support Scale [53] and the Personal Resource Question [64], whereas self-efficacy was assessed by using the Diabetes Empowerment Scale [53], the Diabetes Self-Efficacy Scale [56,59], the Perceived Competence Scale [63], the Diabetes Management Self-Efficacy Scale [52], and the Rosenberg Self-Esteem Scale [65].
Improvements in Outcomes
Outcomes were measured as primary and/or secondary across the studies (Table 4). Five studies reported significant improvements in distress [55,60-62,66]. Three studies reported nonsignificant/significant improvements in depression [53,60,61]. Self-efficacy improved in four studies [53,56,59,65]. Quality of life showed some or little improvement in the majority of the studies [53,56,58,64]. Social support was significantly improved in one study [53] and “positively influenced” in another study [64].
Table 4.
Primary targets and outcomes (primary or secondary) for each intervention.
| Study (year) | Primary target | Outcome | ||||
|
|
|
Depression | Distress | Quality of life | Self-efficacy | Social support |
| Bond (2010) [53] | Psychosocial well-being | Primary |
|
Primary | Primary | Primary |
| Tang (2013) [54] | Disease management | Secondary | Secondary |
|
|
|
| Heisler (2014) [55] | Unspecified |
|
Secondary |
|
Secondary |
|
| Glasgow (2012) [56] | Psychosocial outcomes |
|
|
Primary | Primary |
|
| McMahon (2012) [57] | Diabetes-related outcomes |
|
Secondary |
|
|
|
| McKay (2001) [50] | Physical activity levels | Primary |
|
|
|
|
| McKay (2002) [58] | Unspecified | Primary |
|
Primary |
|
|
| Lorig (2010) [59] | HbA1c, exercise, self-efficacy, patient activation | Secondary | Secondary |
|
Secondary |
|
| Nobis (2015) [60] | Depression | Primary | Secondary |
|
|
|
| Van Bastelaar (2011) [61] | Depression | Primary | Secondary |
|
|
|
| Fisher (2013) [62] | Diabetes distress, self-management |
|
Primary |
|
|
|
| Wangberg (2008) [63] | Diabetes self-care behaviors |
|
|
|
Secondary |
|
| Hunt (2014) [52] | Self-efficacy, self-management, diabetes outcomes |
|
|
|
Primary |
|
| Smith (2000) [64] | Attitudes |
|
|
Primary |
|
Primary |
| Pacaud (2012) [65] | Unspecified |
|
|
Secondary | Secondary |
|
| Fonda (2009) [66] | Diabetes distress |
|
Primary |
|
|
|
A subset of the studies that had significant improvement in distress or depression shared some common characteristics [53,59-61]; that is, the interventions combined synchronous and asynchronous communication, with the intervention running between 2 and 6 months. Providers were mostly psychologists, and studies including peer support were moderated. General information was the most common behavior change technique.
Meta-Analysis
Pairwise meta-analysis was carried out on a total of nine studies, with five studies included for depression scores only [50,53,58-60], six for distress scores only [54,55,57,59,60,62], and two studies analyzed for both outcomes [59,60]. The remaining seven studies from the qualitative data synthesis were excluded from the meta-analysis as there were not enough data to analyze each outcome.
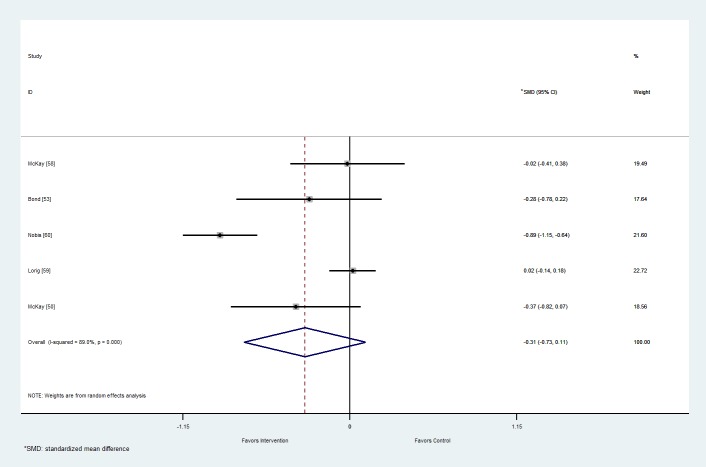
Depression
From the five studies with outcome data for depression, the pooled mean (95% confidence interval) difference between the intervention and control arms on depression score was -0.31 (-0.73 to 0.11; Figure 2). The effect was not significant (P=.15). There was considerable heterogeneity (I2= 89%, P<.001). The funnel plot (Multimedia Appendix 3) and Egger’s test (P=.60) show no obvious publication bias.
Figure 2.
Forest plot of mean difference in depression score between the intervention and control arms at follow-up for studies including Web-based interventions and participants with type 2 diabetes mellitus. SMD: standardized mean difference.
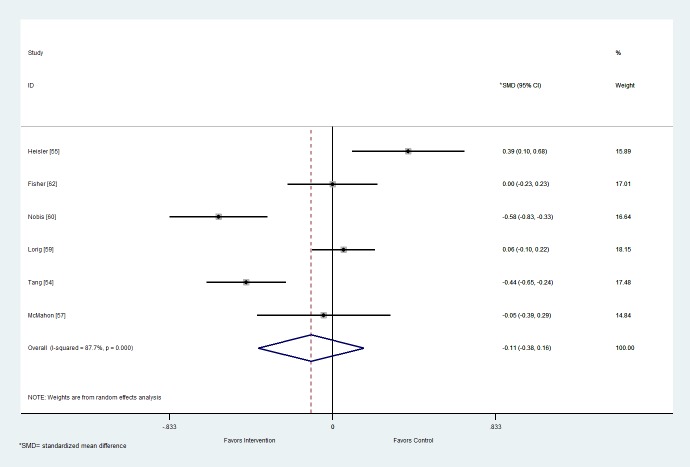
Distress
From the six studies that reported outcome data for distress, the pooled mean (95% confidence interval) difference between the intervention and control arms on distress scores was -0.11 (-0.38 to 0.16; Figure 3). This effect was not significant (P=.43). There was considerable heterogeneity (I2=87.7%, P<.001). Egger’s test (P=.98) showed some indication of publication bias, but the funnel plot (Multimedia Appendix 4) suggests that some of the studies with a small negative standardized mean difference have not been reported. This suggests that the pooled mean may have been biased towards studies showing no effect or that control is preferable to intervention.
Figure 3.
Forest plot of mean difference in distress score between the intervention and control arms at follow-up for studies including Web-based interventions and participants with type 2 diabetes mellitus. SMD: standardized mean difference.
Sensitivity Analyses
When studies with type 1 diabetes and type 2 diabetes participants were excluded for the outcomes depression and distress, the effect size was attenuated and was close to zero (Table 5). Excluding feasibility/pilot studies did not affect the main results (Table 5).
Table 5.
Supporting table of pooled values.
| Analysis | Depression | Distress |
| Main analyses | -0.31 (-0.73 to 0.11) | -0.11 (-0.38 to -0.16) |
| Without feasibility/pilot studies | -0.30 (-0.80 to 0.21) | -0.11 (-0.38 to -0.16) |
| Without T1Da and T2Db studies | -0.05 (-0.24 to 0.14) | -0.02 (-0.28 to 0.24) |
aT1D: type 1 diabetes
bT2D: type 2 diabetes
Discussion
Principal Findings
To our knowledge, this is the first systematic review exploring solely the emotional management construct, specifically the following selected well-being elements: depression, distress, self-efficacy, quality of life, and social support. Individually, a number of studies obtained significant improvements in well-being measures. This improvement was not supported by the meta-analysis for the outcomes of depression and distress, confirming previous findings that Web-based interventions have little effect on distress [34] and emotional outcomes overall [33].
Theories and Behavior Change Techniques
Unlike previous reviews on self-management Web-based interventions in type 2 diabetes [33], our review identified a number of theories across the majority of the papers. Evidence indicates that theory-based Web-based interventions are more effective [36] than non‒theory-based interventions [67,68]; however, there were no conclusive results regarding which theory was associated with the most improved outcomes. Theory-based interventions can help identify behavior change strategies that are also an important element during the development of a condition-specific intervention. In this case, we concluded that Web-based interventions included activities informed by behavior change techniques, with information provision and tracking as the most common techniques. It was evident that there was a wide range of common behavior change techniques used by the majority of the studies, resulting in an inability to identify which behavior change techniques are primarily used, and which are the most effective for this type of intervention. A similar result found in previous reviews on self-management type 2 diabetes interventions [33,36,69].
Type of Intervention Providers
The current evidence around mental health support and online interventions remains divided, with some studies supporting that a professional-led intervention can be beneficial [40], while others suggesting that a non‒professional-led intervention can perform equally well [41,70]. In this review, the majority of studies that provided professional support showed more promising results than those providing nonprofessional support. This conclusion may be influenced by variation in the roles that these providers had in each study, but also the fact that the ratio of professional- and non‒professional-led support was uneven across each intervention, with the majority of the studies including professional-led support.
The Need for Shared Definitions
Issues defining “well-being” and its constructs were iterated in our review. For example, one study [54] that stated it was exploring the well-being outcome, in fact did not assess well-being, nor did it use a well-being measure. Instead, the study measured the constructs “depression” and “distress” with depression- and distress-specific scales. Despite depression being considered as a more established construct and being separate to the construct distress, current literature has argued that both depression and distress are still being used interchangeably [17,71]. Depression and distress are both real established constructs, and even though they may overlap with one another, it is important that they be assessed independently.
The Use of Appropriate Specific Outcome Measures
Another issue is the use of incorrect measures for specific outcomes. With distress becoming an established construct [17], it can be measured with validated and reliable distress questionnaires. Specifically, the DDS and PAID measures are both appropriate tools to assess and quantify the construct of distress. However, despite having existing validated measures for this specific construct, it appeared that some questionnaires were used for other outcomes. For example, in two studies, PAID and DDS scales (both distress measures) were used to measure quality of life. Incorrect use of outcome-specific measures can create barriers to distinguishing aspects of well-being.
Strengths and Limitations
This review has used a robust search strategy, which identified a satisfactory number of studies and is reported in accordance with PRISMA guidelines [72] to determine the usefulness of such interventions for this patient group and to highlight key recommendations for future research in this area. The search was conducted on multiple electronic databases, reference lists were hand-searched, and experts in the area were contacted. The review was based on a strict inclusion and exclusion criteria, and 2 independent authors reviewed quality check and potential articles, and extracted data. Studies with participants with both type 1 diabetes and type 2 diabetes were considered in order to include people with type 2 diabetes and to be consistent with previous reviews. To ensure that the effect of changes was examined, sensitivity analyses were carried out excluding studies with participants with type 1 diabetes and type 2 diabetes. Sensitivity analyses were also carried out to exclude pilot/feasibility studies. Both sensitivity analyses further suggested that Web-based interventions demonstrate little improvement in depression and distress.
As with all systematic reviews, there are some limitations to consider. At a study level, the number of studies included in the meta-analysis was low, and there was considerable heterogeneity across studies with regard to intervention design and measurement of outcomes. This could relate to the fact that the primary aim within interventions varied, with some studies focusing on medical management tasks and other studies focusing on emotional management tasks. At a review level, especially when determining what studies should be included, the terms “well-being” and “Web-based interventions” were based on an in-depth review of the literature and in-depth discussions between 2 independent reviewers throughout the process. The lack of comparable data across all outcomes also led to a less reliable descriptive data synthesis being performed rather than a more robust meta-analysis; therefore, any conclusions must be considered with caution. To minimize bias, this review attempted to explain the results in a logical way for each of the included studies.
Implications
Multicomponent interventions may be useful and may seem effective in studies (eg, Web-based, phone-based), but this creates a challenge for researchers to identify whether the intervention as a whole or only certain aspects contribute to the effect of the intervention. Several implications for the conduct of research in this area can be considered.
Future RCTs looking at similar outcomes should consider using a similar approach to study and/or intervention design in order to make the comparison between interventions much easier, avoiding bias, and in essence producing more reliable conclusions; for example, robust reporting data in line with the Consolidated Standards of Reporting Trials (CONSORT) guidelines and measuring outcomes with similar questionnaires.
Further research may be needed to examine the effect of Web-based interventions in well-being for people with type 2 diabetes, including long-term studies with larger sample sizes.
Future studies may provide a full and detailed description of the intervention including its components to help determine why some studies have some effect and other studies have little or no effect on their outcome.
The majority of RCTs measure psychological outcomes as secondary outcomes, focusing less on the emotional management tasks and more on the medical management. Future studies may aim to approach self-management interventions in a more holistic approach including all three constructs (medical, role, emotional) equally.
Further research may require more consistent definitions of “well-being” and its constructs and may require consistent validated specific measures for each outcome.
Michie’s Taxonomy of Behavior Change Techniques could be considered as a guide for a robust classification system.
Conclusion
The findings of this review collated information and highlighted key issues with the evaluation of Web-based interventions for promoting well-being in people with type 2 diabetes (see Multimedia Appendix 5 for a summary of key findings). It has proposed some recommendations for future research to develop effective interventions. Such interventions could allow stakeholders and health care providers to provide effective, integrated, ongoing Web-based support to promote valuable emotional and general management of type 2 diabetes. Web-based interventions could supplement traditional face-to-face support to improve reach and sustainability and in turn create a more holistic approach to diabetes self-management, bridging the gap between diabetes support and diabetes self-care.
Acknowledgments
The authors acknowledge support from the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care – East Midlands (NIHR CLAHRC – EM), the Leicester Clinical Trials Unit, and the NIHR Leicester-Loughborough Diet, Lifestyle and Physical Activity Biomedical Research Unit, which is a partnership between University Hospitals of Leicester NHS Trust, Loughborough University, and the University of Leicester. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
The authors would also like to acknowledge Keith Nockels, learning and teaching services librarian of the University of Leicester; Selina Lock, research information advisor of the University of Leicester; and Dr Alison Dunkley, research associate in nursing of the University of Leicester, for their input to the search strategy.
The research was funded by the Diabetes Research Centre, University of Leicester.
Abbreviations
- CES-D
Center for Epidemiologic Studies Depression Scale
- CONSORT
Consolidated Standards of Reporting Trials
- DDS
Diabetes Distress Scale
- HADS
Hospital Anxiety and Depression Scale
- HDS
Health Distress Scale
- MeSH
Medical Subject Headings
- PAID
Problem Areas in Diabetes Questionnaire
- PHQ-9
Patient Health Questionnaire
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QoL Index
Quality of Life Index
- RCT
randomized controlled trial
- SF-12
Short Form-12
- SMS
short message service
- WHO
World Health Organization
Search strategy.
Description of intervention and control groups per study.
Funnel plot for depression.
Funnel plot for distress.
Summary of key findings.
Footnotes
Authors' Contributions: MH developed the study protocol, carried out the scientific literature search, extracted and analyzed data, interpreted the results, and drafted the report. JB extracted the data, interpreted the results, and reviewed the report. DB analyzed the data, interpreted the results, and reviewed the report. NR, HE, KK, and MJD contributed to the study protocol and reviewed the report.
Conflicts of Interest: MJD has acted as consultant, advisory board member, and speaker for Novo Nordisk, Sanofi-Aventis, Lilly, Merck Sharp & Dohme, Boehringer Ingelheim, AstraZeneca, and Janssen and as a speaker for Mitsubishi Tanabe Pharma Corporation and Takeda Pharmaceuticals International Inc.
KK has acted as a consultant and speaker for AstraZeneca, Novartis, Novo Nordisk, Sanofi-Aventis, Lilly, Merck Sharp & Dohme, Janssen, and Boehringer Ingelheim. He has received grants in support of investigator and investigator instigated trials from AstraZeneca, Novartis, Novo Nordisk, Sanofi-Aventis, Lilly, Boehringer Ingelheim, Merck Sharp & Dohme, and Roche. KK has served on advisory boards for AstraZeneca, Novartis, Novo Nordisk, Sanofi-Aventis, Lilly, Merck Sharp & Dohme, Janssen, and Boehringer Ingelheim.
References
- 1.World Health Organization. 2016. [2016-09-30]. Diabetes Key Facts http://www.who.int/mediacentre/factsheets/fs312/en/
- 2.Diabetes.co.uk. [2016-09-30]. Diabetes Prevalence http://www.diabetes.co.uk/diabetes-prevalence.html .
- 3.World Health Organization. 2016. [2016-09-30]. Diabetes Media Centre http://www.who.int/mediacentre/factsheets/fs312/en/
- 4.Endocrine Web. 2014. [2016-09-30]. Type 2 Diabetes Complications http://www.endocrineweb.com/conditions/type-2-diabetes/type-2-diabetes-complications .
- 5.Russell LB, Suh D, Safford MA. Time requirements for diabetes self-management: too much for many? J Fam Pract. 2005 Jan;54(1):52–56.jfp_0105_5401j [PubMed] [Google Scholar]
- 6.Bohlen K, Scoville E, Shippee N, May C, Montori V. Overwhelmed patients: a videographic analysis of how patients with type 2 diabetes and clinicians articulate and address treatment burden during clinical encounters. Diabetes Care. 2012;35(1):a–9. doi: 10.2337/dc11-1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brown JB, Nichols GA, Perry A. The burden of treatment failure in type 2 diabetes. Diabetes Care. 2004 Jul;27(7):1535–1540. doi: 10.2337/diacare.27.7.1535.27/7/1535 [DOI] [PubMed] [Google Scholar]
- 8.Franciosi M, Pellegrini F, DeBerardis G, Belfiglio M, Cavaliere D, DiNardo B, Greenfield S, Kaplan S, Sacco M, Tognoni G, Valentini M, Nicolucci A, QuED Study Group The impact of blood glucose self-monitoring on metabolic control and quality of life in type 2 diabetic patients: an urgent need for better educational strategies. Diabetes Care. 2001 Nov;24(11):1870–7. doi: 10.2337/diacare.24.11.1870. [DOI] [PubMed] [Google Scholar]
- 9.Schram M, Baan C, Pouwer F. Depression and quality of life in patients with diabetes: a systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev. 2009 May;5(2):112–119. doi: 10.2174/157339909788166828. http://europepmc.org/abstract/MED/19442096 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diabetes UK . Minding the Gap: The Provision of Psychological Support and Care for People With Diabetes in the UK. London: Diabetes UK; 2008. [2016-09-30]. https://www.diabetes.org.uk/Documents/Reports/Minding_the_Gap_psychological_report.pdf . [Google Scholar]
- 11.Karlsen B, Idsoe T, Dirdal I, Rokne HB, Bru E. Effects of a group-based counselling programme on diabetes-related stress, coping, psychological well-being and metabolic control in adults with type 1 or type 2 diabetes. Patient Educ Couns. 2004 Jun;53(3):299–308. doi: 10.1016/j.pec.2003.10.008.S0738399104000680 [DOI] [PubMed] [Google Scholar]
- 12.Naess S, Midthjell K, Moum T, Sørensen T, Tambs K. Diabetes mellitus and psychological well-being. Results of the Nord-Trøndelag health survey. Scand J Soc Med. 1995 Sep;23(3):179–188. doi: 10.1177/140349489502300308. [DOI] [PubMed] [Google Scholar]
- 13.Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-related emotional distress in Dutch and U.S. diabetic patients: cross-cultural validity of the problem areas in diabetes scale. Diabetes Care. 2000 Sep;23(9):1305–1309. doi: 10.2337/diacare.23.9.1305. http://care.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=10977023 . [DOI] [PubMed] [Google Scholar]
- 14.Grigsby A, Anderson R, Freedland K, Clouse R, Lustman P. Prevalence of anxiety in adults with diabetes: a systematic review. J Psychosom Res. 2002 Dec;53(6):1053–1060. doi: 10.1016/s0022-3999(02)00417-8.S0022399902004178 [DOI] [PubMed] [Google Scholar]
- 15.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001 Jun;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Health and Care Excellence. Depression in Adults With a Chronic Physical Health Problem: Recognition and Management. Clinical guideline CG91. London, UK. NICE. 2009. [2016-09-30]. https://www.nice.org.uk/Guidance/CG91 .
- 17.Snoek F, Bremmer M, Hermanns N. Constructs of depression and distress in diabetes: time for an appraisal. Lancet Diabetes Endocrinol. 2015;3(6):450–460. doi: 10.1016/S2213-8587(15)00135-7. [DOI] [PubMed] [Google Scholar]
- 18.Adriaanse MC, Pouwer F, Dekker JM, Nijpels G, Stehouwer CD, Heine RJ, Snoek FJ. Diabetes-related symptom distress in association with glucose metabolism and comorbidity: the Hoorn Study. Diabetes Care. 2008 Dec;31(12):2268–2270. doi: 10.2337/dc08-1074. http://europepmc.org/abstract/MED/18728236 .dc08-1074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fisher L, Skaff MM, Mullan JT, Arean P, Glasgow R, Masharani U. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with Type 2 diabetes. Diabet Med. 2008 Sep;25(9):1096–1101. doi: 10.1111/j.1464-5491.2008.02533.x. http://europepmc.org/abstract/MED/19183314 .DME2533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garay-Sevilla ME, Malacara JM, Gutiérrez-Roa A, González E. Denial of disease in Type 2 diabetes mellitus: its influence on metabolic control and associated factors. Diabet Med. 1999 Mar;16(3):238–244. doi: 10.1046/j.1464-5491.1999.00033.x. [DOI] [PubMed] [Google Scholar]
- 21.Lustman P, Anderson R, Freedland K, de Groot M, Carney R, Clouse R. Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care. 2000 Jul;23(7):934–942. doi: 10.2337/diacare.23.7.934. http://care.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=10895843 . [DOI] [PubMed] [Google Scholar]
- 22.Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-related emotional distress in Dutch and U.S. diabetic patients: cross-cultural validity of the problem areas in diabetes scale. Diabetes Care. 2000 Sep;23(9):1305–1309. doi: 10.2337/diacare.23.9.1305. http://care.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=10977023 . [DOI] [PubMed] [Google Scholar]
- 23.Speight J, Browne JL, Holmes-Truscott E, Hendrieckx C, Pouwer F, on behalf of the Diabetes MILES-Australia reference group Diabetes MILES Study: Diabetes MILES-Australia 2011 Survey Report. Melbourne, VIC: Diabetes Australia; 2011. https://static.diabetesaustralia.com.au/s/fileassets/diabetes-australia/4e052ae5-2d13-421e-b6f8-5e323b5c48a6.pdf .
- 24.World Health Organization. 2015. [2016-09-30]. Mental Health: A State of Well-Being http://www.who.int/features/factfiles/mental_health/en/
- 25.National Institute for Health and Care Excellence (NICE) 2013. [2016-09-30]. Social and Emotional Wellbeing for Children and Young People https://www.nice.org.uk/advice/lgb12/chapter/introduction . [PubMed]
- 26.Winefield H, Gill T, Taylor A, Pilkington R. Psychological well-being and psychological distress: is it necessary to measure both? Psychology of Well-Being: Theory, Research and Practice. 2012;2(1):3. doi: 10.1186/2211-1522-2-3. [DOI] [Google Scholar]
- 27.Pollard E, Lee P. Child well-being: A systematic review of the literature. Social Indicators Research. 2003;61(1):A–78. doi: 10.1023/A:1021284215801. [DOI] [Google Scholar]
- 28.Funnell M, Brown T, Childs B, Haas L, Hosey G, Jensen B, Maryniuk M, Peyrot M, Piette J, Reader D, Siminerio L, Weinger K, Weiss M. National Standards for Diabetes Self-Management Education. Diabetes Care. 2010;33(Suppl 1):S89–S96. doi: 10.2337/dc10-S089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Department of Health. UK Government; 2001. [2016-09-30]. National Service Framework for Diabetes: Standards https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/198836/National_Service_Framework_for_Diabetes.pdf . [Google Scholar]
- 30.Nicolucci A, Kovacs BK, Holt RIG, Comaschi M, Hermanns N, Ishii H, Kokoszka A, Pouwer F, Skovlund SE, Stuckey H, Tarkun I, Vallis M, Wens J, Peyrot M. Diabetes Attitudes, Wishes and Needs second study (DAWN2™): cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabet Med. 2013 Jul;30(7):767–777. doi: 10.1111/dme.12245. [DOI] [PubMed] [Google Scholar]
- 31.Diabetes UK Diabetes.org.uk. 2009. [2016-09-30]. Improving Supported Self-Management for People with Diabetes https://www.diabetes.org.uk/Documents/Reports/Supported_self-management.pdf .
- 32.Wantland D, Portillo C, Holzemer W, Slaughter R, McGhee E. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004 Nov 10;6(4):e40. doi: 10.2196/jmir.6.4.e40. http://www.jmir.org/2004/4/e40/ v6e40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pal K, Eastwood S, Michie Susan, Farmer Andrew, Barnard Maria L, Peacock Richard, Wood Bindie, Edwards Phil, Murray Elizabeth. Computer-based interventions to improve self-management in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2014 Jun;37(6):1759–1766. doi: 10.2337/dc13-1386.37/6/1759 [DOI] [PubMed] [Google Scholar]
- 34.Beatty L, Lambert S. A systematic review of internet-based self-help therapeutic interventions to improve distress and disease-control among adults with chronic health conditions. Clin Psychol Rev. 2013 Jun;33(4):609–622. doi: 10.1016/j.cpr.2013.03.004.S0272-7358(13)00044-5 [DOI] [PubMed] [Google Scholar]
- 35.Griffiths F, Lindenmeyer A, Powell J, Lowe P, Thorogood M. Why are health care interventions delivered over the internet? A systematic review of the published literature. J Med Internet Res. 2006;8(2):e10. doi: 10.2196/jmir.8.2.e10. http://www.jmir.org/2006/2/e10/ v8i2e10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Van Vugt M, De Wit M, Cleijne WJ, Snoek FJ. Use of behavioral change techniques in web-based self-management programs for type 2 diabetes patients: systematic review. J Med Internet Res. 2013;15(12):e279. doi: 10.2196/jmir.2800. http://www.jmir.org/2013/12/e279/ v15i12e279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Murray E. Web-based interventions for behavior change and self-management: potential, pitfalls, and progress. Med 2 0. 2012;1(2):e3. doi: 10.2196/med20.1741. http://www.medicine20.com/2012/2/e3/ v1i2e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paul C, Carey M, Sanson-Fisher R, Houlcroft L, Turon H. The impact of web-based approaches on psychosocial health in chronic physical and mental health conditions. Health Educ Res. 2013 Jun;28(3):450–471. doi: 10.1093/her/cyt053. http://her.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=23660463 .cyt053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barak A, Klein B, Proudfoot JG. Defining internet-supported therapeutic interventions. Ann Behav Med. 2009 Aug;38(1):4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- 40.Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med. 2007 Mar;37(3):319–328. doi: 10.1017/S0033291706008944.S0033291706008944 [DOI] [PubMed] [Google Scholar]
- 41.Richards D, Richardson T. Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev. 2012 Jun;32(4):329–342. doi: 10.1016/j.cpr.2012.02.004.S0272-7358(12)00027-X [DOI] [PubMed] [Google Scholar]
- 42.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003 Aug;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 43.Lepard M, Joseph A, Agne A, Cherrington A. Diabetes self-management interventions for adults with type 2 diabetes living in rural areas: a systematic literature review. Curr Diab Rep. 2015 Jun;15(6):608. doi: 10.1007/s11892-015-0608-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cotter A, Durant N, Agne A, Cherrington A. Internet interventions to support lifestyle modification for diabetes management: a systematic review of the evidence. J Diabetes Complications. 2014;28(2):243–251. doi: 10.1016/j.jdiacomp.2013.07.003. http://europepmc.org/abstract/MED/24332469 .S1056-8727(13)00165-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liberati A, Altman D, Tetzlaff J, Mulrow C, Gotzsche P, Ioannidis J, Clarke M, Devereaux P, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009 Jul 21;339(jul21 1):b2700–b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leiner B, Cerf V, Clark D, Kahn R, Kleinrock L, Lynch D, Postel J, Roberts L, Wolff S. The past and future history of the Internet. Commun. ACM. 1997;40(2):102–108. doi: 10.1145/253671.253741. [DOI] [Google Scholar]
- 47.Centre for Reviews and Dissemination. [2016-09-30]. Systematic Reviews: CRD's Guidance for Undertaking Reviews in Health care. York, UK: York Publishing Services Ltd; 2008 https://www.york.ac.uk/media/crd/Systematic_Reviews.pdf .
- 48.Cochrane reviews. 2016. [2016-09-30]. Quality Scales and Cochrane Reviews http://handbook.cochrane.org/chapter_8/8_3_3_quality_scales_and_cochrane_reviews.htm .
- 49.Glasgow RE, Boles SM, McKay HG, Feil EG, Barrera M. The D-Net diabetes self-management program: long-term implementation, outcomes, and generalization results. Prev Med. 2003 Apr;36(4):410–419. doi: 10.1016/s0091-7435(02)00056-7.S0091743502000567 [DOI] [PubMed] [Google Scholar]
- 50.McKay H, King D, Eakin E, Seeley J, Glasgow R. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care. 2001 Aug;24(8):1328–1334. doi: 10.2337/diacare.24.8.1328. [DOI] [PubMed] [Google Scholar]
- 51.Barrera J, Glasgow RE, McKay HG, Boles SM, Feil EG. Do Internet-based support interventions change perceptions of social support?: An experimental trial of approaches for supporting diabetes self-management. Am J Community Psychol. 2002 Oct;30(5):637–654. doi: 10.1023/A:1016369114780.10.1023/A:1016369114780 [DOI] [PubMed] [Google Scholar]
- 52.Hunt C, Sanderson B, Ellison K. Support for diabetes using technology: a pilot study to improve self-management. Medsurg Nurs. 2014;23(4):a–7. [PubMed] [Google Scholar]
- 53.Bond G, Burr R, Wolf F, Feldt K. The effects of a web-based intervention on psychosocial well-being among adults aged 60 and older with diabetes: a randomized trial. Diabetes Educ. 2010;36(3):446–456. doi: 10.1177/0145721710366758.0145721710366758 [DOI] [PubMed] [Google Scholar]
- 54.Tang P, Overhage J, Chan A, Brown N, Aghighi B, Entwistle B, Hui S, Hyde S, Klieman L, Mitchell C, Perkins A, Qureshi L, Waltimyer T, Winters L, Young C. Online disease management of diabetes: engaging and motivating patients online with enhanced resources-diabetes (EMPOWER-D), a randomized controlled trial. J Am Med Inform Assoc. 2013 May 1;20(3):526–534. doi: 10.1136/amiajnl-2012-001263. http://jamia.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=23171659 .amiajnl-2012-001263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heisler M, Choi H, Palmisano G, Mase R, Richardson C, Fagerlin A, Montori VM, Spencer M, An LC. Comparison of community health worker-led diabetes medication decision-making support for low-income Latino and African American adults with diabetes using e-health tools versus print materials: a randomized, controlled trial. Ann Intern Med. 2014 Nov 18;161(10 Suppl):S13–22. doi: 10.7326/M13-3012. http://europepmc.org/abstract/MED/25402398 .1935739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Glasgow RE, Kurz D, King D, Dickman JM, Faber AJ, Halterman E, Woolley T, Toobert DJ, Strycker LA, Estabrooks PA, Osuna D, Ritzwoller D. Twelve-month outcomes of an Internet-based diabetes self-management support program. Patient Educ Couns. 2012 Apr;87(1):81–92. doi: 10.1016/j.pec.2011.07.024. http://europepmc.org/abstract/MED/21924576 .S0738-3991(11)00391-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McMahon GT, Fonda SJ, Gomes HE, Alexis G, Conlin PR. A randomized comparison of online- and telephone-based care management with internet training alone in adult patients with poorly controlled type 2 diabetes. Diabetes Technol Ther. 2012 Nov;14(11):1060–1067. doi: 10.1089/dia.2012.0137. http://europepmc.org/abstract/MED/22953754 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McKay HG, Glasgow RE, Feil EG, Boles SM, Barrera Jr M. Internet-based diabetes self-management and support: Initial outcomes from the Diabetes Network project. Rehabilitation Psychology. 2002;47(1):31–48. doi: 10.1037/0090-5550.47.1.31. [DOI] [Google Scholar]
- 59.Lorig K, Ritter P, Laurent D, Plant K, Green M, Jernigan V, Case S. Online diabetes self-management program: a randomized study. Diabetes Care. 2010 Jun;33(6):1275–1281. doi: 10.2337/dc09-2153. http://europepmc.org/abstract/MED/20299481 .dc09-2153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nobis S, Lehr D, Ebert D, Baumeister H, Snoek F, Riper H, Berking M. Efficacy of a web-based intervention with mobile phone support in treating depressive symptoms in adults with type 1 and type 2 diabetes: a randomized controlled trial. Diabetes Care. 2015 May;38(5):776–783. doi: 10.2337/dc14-1728.dc14-1728 [DOI] [PubMed] [Google Scholar]
- 61.Van Bastelaar KM, Pouwer F, Cuijpers P, Riper H, Snoek FJ. Web-based depression treatment for type 1 and type 2 diabetic patients: a randomized, controlled trial. Diabetes Care. 2011 Feb;34(2):320–325. doi: 10.2337/dc10-1248. http://europepmc.org/abstract/MED/21216855 .dc10-1248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fisher L, Hessler D, Glasgow R, Arean P, Masharani U, Naranjo D, Strycker L. REDEEM: a pragmatic trial to reduce diabetes distress. Diabetes Care. 2013 Sep;36(9):2551–2558. doi: 10.2337/dc12-2493. http://europepmc.org/abstract/MED/23735726 .dc12-2493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wangberg SC. An Internet-based diabetes self-care intervention tailored to self-efficacy. Health Educ Res. 2008 Feb;23(1):170–9. doi: 10.1093/her/cym014. http://her.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17412717 .cym014 [DOI] [PubMed] [Google Scholar]
- 64.Smith L, Weinert C. Telecommunication support for rural women with diabetes. Diabetes Educ. 2000;26(4):645–55. doi: 10.1177/014572170002600412. [DOI] [PubMed] [Google Scholar]
- 65.Pacaud D, Kelley H, Downey A, Chiasson M. Successful delivery of diabetes self-care education and follow-up through eHealth media. Can J Diabetes. 2012;36(5):257–262. [Google Scholar]
- 66.Fonda SJ, McMahon GT, Gomes HE, Hickson S, Conlin PR. Changes in diabetes distress related to participation in an internet-based diabetes care management program and glycemic control. J Diabetes Sci Technol. 2009 Jan;3(1):117–24. doi: 10.1177/193229680900300113. http://europepmc.org/abstract/MED/20046656 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol. 2008;57(4):660–680. doi: 10.1111/j.1464-0597.2008.00341.x. [DOI] [Google Scholar]
- 68.Webb T, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. J Med Internet Res. 2010;12(1):e4. doi: 10.2196/jmir.1376. http://www.jmir.org/2010/1/e4/ v12i1e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ramadas A, Quek K, Chan CKY, Oldenburg B. Web-based interventions for the management of type 2 diabetes mellitus: a systematic review of recent evidence. Int J Med Inform. 2011 Jun;80(6):389–405. doi: 10.1016/j.ijmedinf.2011.02.002.S1386-5056(11)00047-5 [DOI] [PubMed] [Google Scholar]
- 70.Johansson R, Andersson G. Internet-based psychological treatments for depression. Expert Rev Neurother. 2012 Jul;12(7):861–9; quiz 870. doi: 10.1586/ern.12.63. [DOI] [PubMed] [Google Scholar]
- 71.Fisher L, Gonzalez J, Polonsky W. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabet Med. 2014 Jul;31(7):764–772. doi: 10.1111/dme.12428. http://europepmc.org/abstract/MED/24606397 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cochrane Community. 2016. [2016-09-30]. Reporting Guidelines https://community-archive.cochrane.org/about-us/evidence-based-health-care/webliography/books/reporting .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategy.
Description of intervention and control groups per study.
Funnel plot for depression.
Funnel plot for distress.
Summary of key findings.