Abstract
A local anesthetic, lidocaine, is known to affect cutaneous blood flow when injected to the skin. However, it is unknown if dermal lymphatic function can also be affected. Therefore, we characterized lymphatic function in response to administration of lidocaine with and without epinephrine. Non-invasive near-infrared fluorescence imaging (NIRFI) with intradermal injection of indocyanine green (ICG) was used to characterize lymphatic “pumping” function in mice after subcutaneous injection of 2% lidocaine with and without 1:100,000 epinephrine or saline. NIRFI was performed for 10–20mins immediately after and 1, 3, and 5hrs after these interventions. Lymphatic contraction frequencies significantly decreased 10mins after s.c. injection of lidocaine and remained plateaued for another 5mins, before returning to baseline. However, addition of 1:100,000 epinephrine to 2% lidocaine rapidly increased lymphatic contraction frequencies at 5mins post-injection, which returned to baseline levels 15mins later. Injection of saline also increased lymphatic contraction frequency 5 mins after injection, which returned to baseline 10min post-injection. Although lidocaine administration showed a decrease in lymphatic function, the combination of epinephrine with lidocaine resulted in a predominant net effect of increased contractile activity.
Keywords: lymphatic function, near-infrared fluorescence imaging, local anesthetics, lidocaine, epinephrine
Lidocaine, also known as xylocaine and lignocaine, is the most widely used local anesthetic and reported to have an onset <2mins and a duration for up to 2hrs by blocking voltage-gated sodium channels [1, 2]. Lidocaine is also known to be a vasodilator at clinically relevant doses [3]. A significant increase in blood flow was observed at the site of injection in response to administration of 1–2% lidocaine in human skin [3–5]. Vasodilation and thus increased blood flow can lead to an increased rate of systemic absorption of lidocaine into the blood, thus decreasing the duration and depth of pain control. Therefore, epinephrine, more commonly known as adrenaline and a potent vasoconstrictor, is often added to provide vasoconstriction, thereby prolonging the duration of anesthesia and limiting systemic absorption and toxic reactions [6, 7]. Significantly decreased blood flow has been demonstrated following injection with epinephrine combined with lidocaine [8, 9]. Yet to date, it is unknown whether dermal lymphatic function can be affected after administration of local anesthetics in vivo, although lymphatic vessels are abundant in many organs of the body, such as the skin. Therefore, we non-invasively imaged and characterized dermal lymphatic function in mice following subcutaneous injection of lidocaine with and without epinephrine using near-infrared fluorescence imaging (NIRFI).
Female C57BL6 mice (8–10 weeks old; Charles River) were housed and fed sterilized pelleted food and sterilized water. All experiments were approved by University of Texas Health Science Center Institutional Animal Care and Usage Committee. Animals were clipped and residual hair removed with depilatory cream 24hrs before NIRFI. NIRFI was conducted prior to injection of any agents for baseline data. Anesthesia was induced with 2% isoflurane in 100% oxygen, which was administered continuously through a nose mask in spontaneously breathing mice, and maintained at 37°C on a warming pad. Waste isoflurane gas was removed by an exhaust ventilation system and the charcoal canister. No abnormal respiratory conditions were observed in any mice. NIRFI was conducted immediately following intradermal (i.d.) injection of 2μl of indocyanine green (ICG; 0.5mg/ml; Akorn, Inc) to the dorsal aspect of the left foot using 34-gauge needles using a custom-built NIRFI system [10, 11]. A macrolens was used to zoom in on a specific area in fluorescent lymphatic vessels. After 10min of NIRFI, 10μl of 2% lidocaine hydrochloride with or without 1:100,000 epinephrine (Hospira, Inc), or saline, was injected to the area below the afferent popliteal lymphatic vessels in the hind limb (n=8/group; arrow in Supplementary Material 1) and mice were imaged for another 20mins. Beginning at 5mins after injection of agents, the data was analyzed every 5mins for 15mins. Different groups of mice were also imaged for 10mins following i.d. injection of 2μl ICG at 1, 3, and 5hrs after administration of 10μl of lidocaine alone (n=8/group), lidocaine with epinephrine (n=8/group), or saline (n=6/group). Those data were quantified for 4mins at 5mins after injection of ICG. The data were analyzed with ImageJ (National Institutes of Health). The same size of fixed regions of interest (ROIs) in fluorescent afferent popliteal lymphatic vessels were defined on fluorescence images and the averaged fluorescence intensity within each ROI in each fluorescence image was plotted as a function of imaging time. The number of “pulses” of ICG-laden lymph is an indication of lymphatic contractile activity and termed “contractions.” Data were presented as average values ± standard error. Statistical analysis was performed with GraphPad Prism 7 (GraphPad Software, Inc). The data were analyzed by two-way analysis of variance followed by Tukey’s multiple comparison test. The differences were considered significant at p<0.05. The effect of local anesthetics on lymphatic contractile function in vivo was unknown. Therefore, no power calculations were performed.
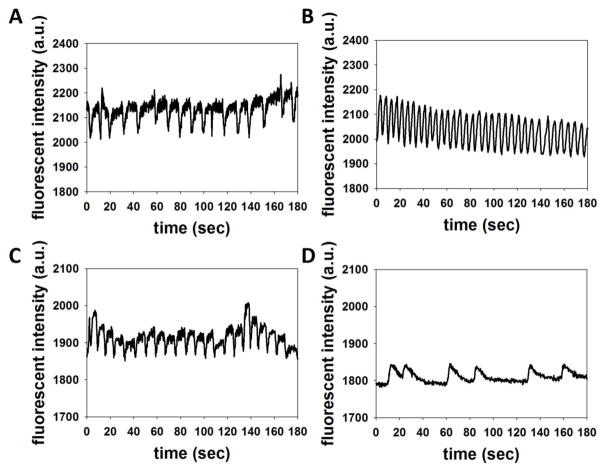
Baseline data prior to injection of local anesthetics (Figures 1A and 1C) show dynamic changes of fluorescent intensities as a function of time in the ROI, demonstrating propulsive lymphatic function. Fluorescent intensity profiles as shown in Figure 1B, show more lymphatic pulses in mice 10mins after injection of lidocaine with epinephrine as compared to its baseline, whereas we observed reduced pulses in mice at 10mins post-injection of lidocaine alone. As shown in Figure 2, at 10minutes post-injection of lidocaine alone, our NIRFI data demonstrated a significant decrease in the lymphatic contraction frequency for 5min (45.3% baseline). Contraction frequencies remained at plateau for 5mins and started to return to baseline 60min post-injection. The addition of epinephrine 1:100,000 to 2% lidocaine resulted in an immediate increase (174% baseline) in the lymphatic contraction frequency between baseline and 5mins post injection, followed by a decrease lasting 15min post-injection, when there was no difference in the contraction frequency as compared to baseline. Wang et al. [12] showed that lymphatics contracted spasmodically as soon as epinephrine was applied to afferent popliteal lymphatic vessels in rats. Smith et al. [13] also demonstrated that, when applied to exposed afferent lymphatic vessels draining to the PLN, epinephrine produced spasm of the lymphatics followed by a markedly increased rate of contraction. Lymph flow and contraction frequency in afferent popliteal lymphatic vessels of sheep increased immediately at the beginning of the intravenous infusion of epinephrine [14]. Hall et al. [15] observed a rapid two-fold increase in lymph flow rate and the frequency of the lymphatic pulses in the thoracic duct when adrenaline was directly injected into the popliteal lymph duct. Since epinephrine is a vasoconstrictor and decreases local blood flow in the skin, blood flow changes may not account for an increase in lymphatic contractility. Instead, epinephrine may cause an increase in lymphatic contractility by acting directly on adrenoceptors on the lymphatic vessels [14, 16, 17], although further studies are needed to examine the mechanism of this change with epinephrine alone and thus to measure lymph flow rate. Thus, our data showed that the combination of epinephrine with lidocaine results in a predominant net effect of increased contractile activity.
Figure 1.
Representative fluorescent intensity profiles as a function of time prior to (A, C) and 10 mins after injection of 2% lidocaine with (B) and without (D) 1:100,000 epinephrine.
Figure 2.
Lymphatic contraction frequencies prior to (baseline) and 5, 10, 15, 60, 180, and 300 mins after injection of 2% lidocaine with (square) or without (circle) epinephrine, or saline alone (triangle). Error bars show the standard error. * p<0.05 vs. baseline. # p<0.05 vs. saline. + p<0.05 vs. lidocaine.
Saline injection also resulted in a moderate increase in the contraction frequency in the first 5mins (23.2% baseline) as compared to baseline. However, contraction frequency returned to baseline 10min post-injection due to redistribution in the surrounding tissue and remained for 5 hours. It was reported that injection of higher volume (50μl to 300μl) of the Locke’s solution into the footpad of rats and mice increased lymph formation and thus resulted in a significantly increased rate of lymphatic contractility [12, 13], suggesting the injection volume-dependent increase of lymphatic contraction frequency. Previous studies also showed that PBS or saline injection to human skin resulted in vasodilation and thus increased blood flow; however, the maximal increases in cutaneous blood flow after injection of control agents was less than injection of local anesthetics and the vasodilation effect resolved quickly [4, 9]. The contraction frequencies at 5 and 10min post-injection with 1:100,000 epinephrine combined with 2% lidocaine were significantly greater than saline and 2% lidocaine alone (p<0.05). The contraction frequencies in mice injected with 2% lidocaine were significantly lower than saline and 2% lidocaine combined with 1:100,000 epinephrine at 5, 10, and 15min post-injection (p<0.05).
Effects of anesthetics on lymphatic function have been reported previously. In general, conventional anesthetics at clinically relevant concentrations reduced lymphatic contractility and inhibited lymph flow [18]. More recently, van Helden et al. [19] demonstrated that the topical application of the local anesthetic lignocaine (10%) in rats slowed lymph flow, mainly due to blockage of nerve-mediated action potentials. It was also reported that lidocaine at a concentration of 0.3μM reduced the spontaneous contractile activity in human mesenteric lymphatic vessel segments [20]. Lidocaine blocks a broad spectrum of voltage-gated sodium channels (VGSCs), whereas tetrodotoxin (TTX) blocks specific VGSC subtypes, which are also known to inhibit lymphatic contractility [20].
During an ongoing inflammatory response after tissue injury, lymphatic pump function removes excess interstitial fluid and accumulated inflammatory cells and mediators from the inflamed tissues. Insufficient lymphatic function can cause a further inflammatory reaction and thus impair immune responses and wound healing. Although there is no report that lymphedema can result from inhibition of lymphatic function by anesthesia, it was reported that edema can occur after anesthesia [21]. Furthermore, it is unknown whether other local anesthetics or sodium channel blockers affect lymphatic contractile function. In this study, we used clinically relevant doses of 2% lidocaine with and without 1:100,000 epinephrine [1]; however, future studies will need to address effects of different doses of lidocaine and epinephrine, as well as other local anesthetics, on lymphatic function in vivo, since some local anesthetics are known to have a biphasic effect on skin microcirculation [3, 22, 23].
In summary, our study demonstrated for the first time, the effects of lidocaine with and without epinephrine on dermal lymphatic vessel function in mice using non-invasive NIRFI. We have shown that lymphatic contraction frequencies were significantly reduced 10 mins after injection of 2% lidocaine, whereas addition of 1:100,000 epinephrine to 2% lidocaine rapidly increased lymphatic contraction frequencies at 5mins post-injection. However, functional lymphatic changes started to return to baseline 60 and 15mins after injection of lidocaine alone and with epinephrine, respectively.
Supplementary Material
Figure 1. Whole body white light (A) and fluorescent (B) images 10 mins after injection of ICG showing lymphatic drainage of ICG from the paw to the PLN. Arrowhead, ICG injection site. Double arrow, PLN. Arrow, injection site of local anesthetics or saline. (C) Magnified fluorescent image of the white rectangle in (B) showing afferent popliteal lymphatic vessels draining to the PLN (arrow) in mice. The same size ROI (circle) was selected on the same area on the fluorescent images for lymphatic pumping activity. Scale bar, 1 mm.
Acknowledgments
The authors would like to thank veterinarian Dr. Christopher Janssen for the comments on the anesthesia method used in these experiments. This work was supported in part by the National Institutes of Health R21 CA159193 (SK).
Footnotes
Authors’ contributions
S.K.: Study design, Study conduct, data analysis, and writing paper. E.M.S.: writing and revising paper.
References
- 1.Achar S, Kundu S. Principles of office anesthesia: part I. Infiltrative anesthesia. American family physician. 2002;66:91–4. [PubMed] [Google Scholar]
- 2.Cummins TR. Setting up for the block: the mechanism underlying lidocaine’s use-dependent inhibition of sodium channels. J Physiol. 2007;582:11. doi: 10.1113/jphysiol.2007.136671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aps C, Reynolds F. The effect of concentration on vasoactivity of bupivacaine and lignocaine. British journal of anaesthesia. 1976;48:1171–4. doi: 10.1093/bja/48.12.1171. [DOI] [PubMed] [Google Scholar]
- 4.Guinard JP, Carpenter RL, Morell RC. Effect of local anesthetic concentration on capillary blood flow in human skin. Regional anesthesia. 1992;17:317–21. [PubMed] [Google Scholar]
- 5.Cederholm I, Evers H, Lofstrom JB. Effect of intradermal injection of saline or a local anaesthetic agent on skin blood flow--a methodological study in man. Acta anaesthesiologica Scandinavica. 1991;35:208–15. doi: 10.1111/j.1399-6576.1991.tb03275.x. [DOI] [PubMed] [Google Scholar]
- 6.Swerdlow M, Jones R. The duration of action of bupivacaine, prilocaine and lignocaine. British journal of anaesthesia. 1970;42:335–9. doi: 10.1093/bja/42.4.335. [DOI] [PubMed] [Google Scholar]
- 7.Liu S, Carpenter RL, Chiu AA, McGill TJ, Mantell SA. Epinephrine prolongs duration of subcutaneous infiltration of local anesthesia in a dose-related manner. Correlation with magnitude of vasoconstriction. Regional anesthesia. 1995;20:378–84. [PubMed] [Google Scholar]
- 8.Larrabee WF, Jr, Lanier BJ, Miekle D. Effect of epinephrine on local cutaneous blood flow. Head & neck surgery. 1987;9:287–9. doi: 10.1002/hed.2890090507. [DOI] [PubMed] [Google Scholar]
- 9.Ghali S, Knox KR, Verbesey J, Scarpidis U, Izadi K, Ganchi PA. Effects of lidocaine and epinephrine on cutaneous blood flow. Journal of plastic, reconstructive & aesthetic surgery: JPRAS. 2008;61:1226–31. doi: 10.1016/j.bjps.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Kwon S, Agollah GD, Wu G, Chan W, Sevick-Muraca EM. Direct visualization of changes of lymphatic function and drainage pathways in lymph node metastasis of B16F10 melanoma using near-infrared fluorescence imaging. Biomed Opt Express. 2013;4:967–77. doi: 10.1364/BOE.4.000967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwon S, Sevick-Muraca EM. Mouse phenotyping with near-infrared fluorescence lymphatic imaging. Biomed Opt Express. 2011;2:1403–11. doi: 10.1364/BOE.2.001403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang GY, Zhong SZ. Experimental study of lymphatic contractility and its clinical importance. Ann Plast Surg. 1985;15:278–84. doi: 10.1097/00000637-198510000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Smith RO. Lymphatic contractility; a possible intrinsic mechanism of lymphatic vessels for the transport of lymph. J Exp Med. 1949;90:497–509. doi: 10.1084/jem.90.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McHale NG, Roddie IC. The effect of intravenous adrenaline and noradrenaline infusion of peripheral lymph flow in the sheep. J Physiol. 1983;341:517–26. doi: 10.1113/jphysiol.1983.sp014821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall JG, Morris B, Woolley G. Intrinsic rhythmic propulsion of lymph in the unanaesthetized sheep. J Physiol. 1965;180:336–49. doi: 10.1113/jphysiol.1965.sp007706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Takahashi N, Kawai Y, Ohhashi T. Effects of vasoconstrictive and vasodilative agents on lymphatic smooth muscles in isolated canine thoracic ducts. J Pharmacol Exp Ther. 1990;254:165–70. [PubMed] [Google Scholar]
- 17.McHale NG, Roddie IC. The effects of catecholamines on pumping activity in isolated bovine mesenteric lymphatics. J Physiol. 1983;338:527–36. doi: 10.1113/jphysiol.1983.sp014687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McHale NG, Thornbury KD. The effect of anesthetics on lymphatic contractility. Microvascular research. 1989;37:70–6. doi: 10.1016/0026-2862(89)90073-3. [DOI] [PubMed] [Google Scholar]
- 19.van Helden DF, Thomas PA, Dosen PJ, Imtiaz MS, Laver DR, Isbister GK. Pharmacological approaches that slow lymphatic flow as a snakebite first aid. PLoS neglected tropical diseases. 2014;8:e2722. doi: 10.1371/journal.pntd.0002722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Telinius N, Majgaard J, Kim S, Katballe N, Pahle E, Nielsen J, et al. Voltage-gated sodium channels contribute to action potentials and spontaneous contractility in isolated human lymphatic vessels. J Physiol. 2015;593:3109–22. doi: 10.1113/JP270166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hattori J, Yamakage M, Seki S, Okazaki K, Namiki A. Inhibitory effects of the anesthetics propofol and sevoflurane on spontaneous lymphatic vessel activity in rats. Anesthesiology. 2004;101:687–94. doi: 10.1097/00000542-200409000-00017. [DOI] [PubMed] [Google Scholar]
- 22.Newton DJ, Burke D, Khan F, McLeod GA, Belch JJ, McKenzie M, et al. Skin blood flow changes in response to intradermal injection of bupivacaine and levobupivacaine, assessed by laser Doppler imaging. Regional anesthesia and pain medicine. 2000;25:626–31. doi: 10.1053/rapm.2000.9853. [DOI] [PubMed] [Google Scholar]
- 23.Newton DJ, McLeod GA, Khan F, Belch JJ. Vasoactive characteristics of bupivacaine and levobupivacaine with and without adjuvant epinephrine in peripheral human skin. British journal of anaesthesia. 2005;94:662–7. doi: 10.1093/bja/aei095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure 1. Whole body white light (A) and fluorescent (B) images 10 mins after injection of ICG showing lymphatic drainage of ICG from the paw to the PLN. Arrowhead, ICG injection site. Double arrow, PLN. Arrow, injection site of local anesthetics or saline. (C) Magnified fluorescent image of the white rectangle in (B) showing afferent popliteal lymphatic vessels draining to the PLN (arrow) in mice. The same size ROI (circle) was selected on the same area on the fluorescent images for lymphatic pumping activity. Scale bar, 1 mm.