Abstract
Cancer of uterine cervix is one of the most common malignancies in women. Metastatic recurrence of cervical cancer in spleen is rare, mostly seen in autopsies. Splenic metastasis from cervical cancer in a living patient without disseminated metastases is rarer. Here, we present the case of a lady aged 46 years with cervical cancer—squamous cell carcinoma—who had undergone radical hysterectomy and postoperative 50 Gy of intensity modulated radiation therapy in 25 fractions and 50 mg of weekly cisplatin for 6 weeks. She was doing well for 17 months. Then, she developed fever and anorexia, and was detected to have splenic lesion and a lesion in the pelvic mesentery in PET/CT (positron emission tomography—computed tomography). Laparoscopy showed enlarged spleen with a mass lesion and a mass in ileal mesentery adherent to the peritoneum over the fundus of bladder and greater omentum. She underwent resection of a segment of ileum with the mesenteric lesion and omentum and bladder peritoneum laparoscopically and splenectomy. Histopathological examination revealed both the mesenteric and splenic lesions to be metastases from poorly differentiated carcinoma, which was from the cervical cancer. Immunohistochemistry was suggestive of squamous cell carcinoma associated with high-risk human papilloma virus. After the postoperative recovery, patient was started on ciplatin with paclitaxel chemotherapy.
Keywords: Cancer of uterine cervix, Splenic metastsis, Squamous cell carcinoma, Isolated metastases, Distant recurrence
Introduction
Uterine cervix is among the common sites of malignancy in women. Patients treated for cervical cancer may develop local recurrence, distant recurrence or both. Splenic metastasis from cervical cancer is very rare. And most of them have been detected during autopsy. We present a case of squamous cell carcinoma of cervix that had splenic metastasis detected on PET/CT (positron emission tomography—computed tomography) and confirmed by surgery and histopathology.
Case Report
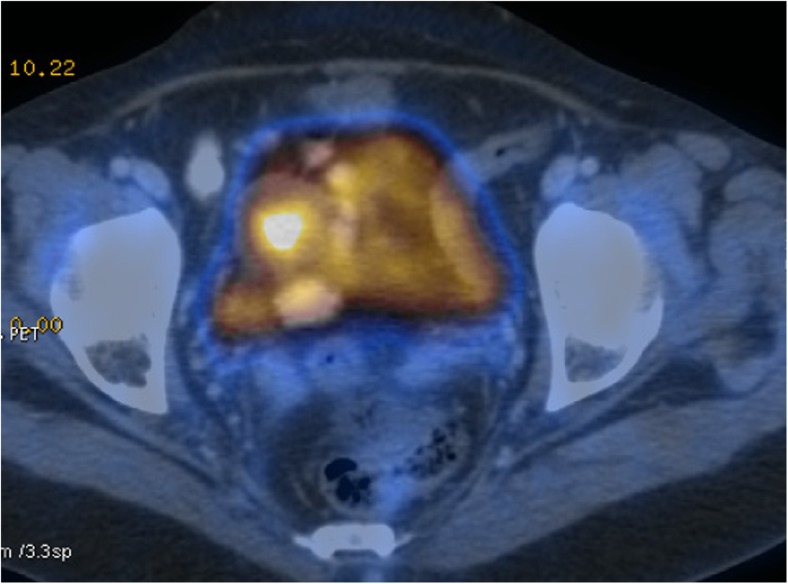
A lady aged 46 years presented with history of fever and anorexia. PET/CT showed 6.6×5.8 cm heterogeneously enhancing necrotic metabolically active splenic mass lesion and a 3.6×3.0 cm enhancing metabolically active soft tissue mass in the lower pelvic mesentery suggestive of metastases. SUV (standardised uptake value) of the splenic lesion was 19.3 and that of mesenteric lesion was 19.9. There was no evidence of any other metastases (Figs. 1 and 2).
Fig. 1.
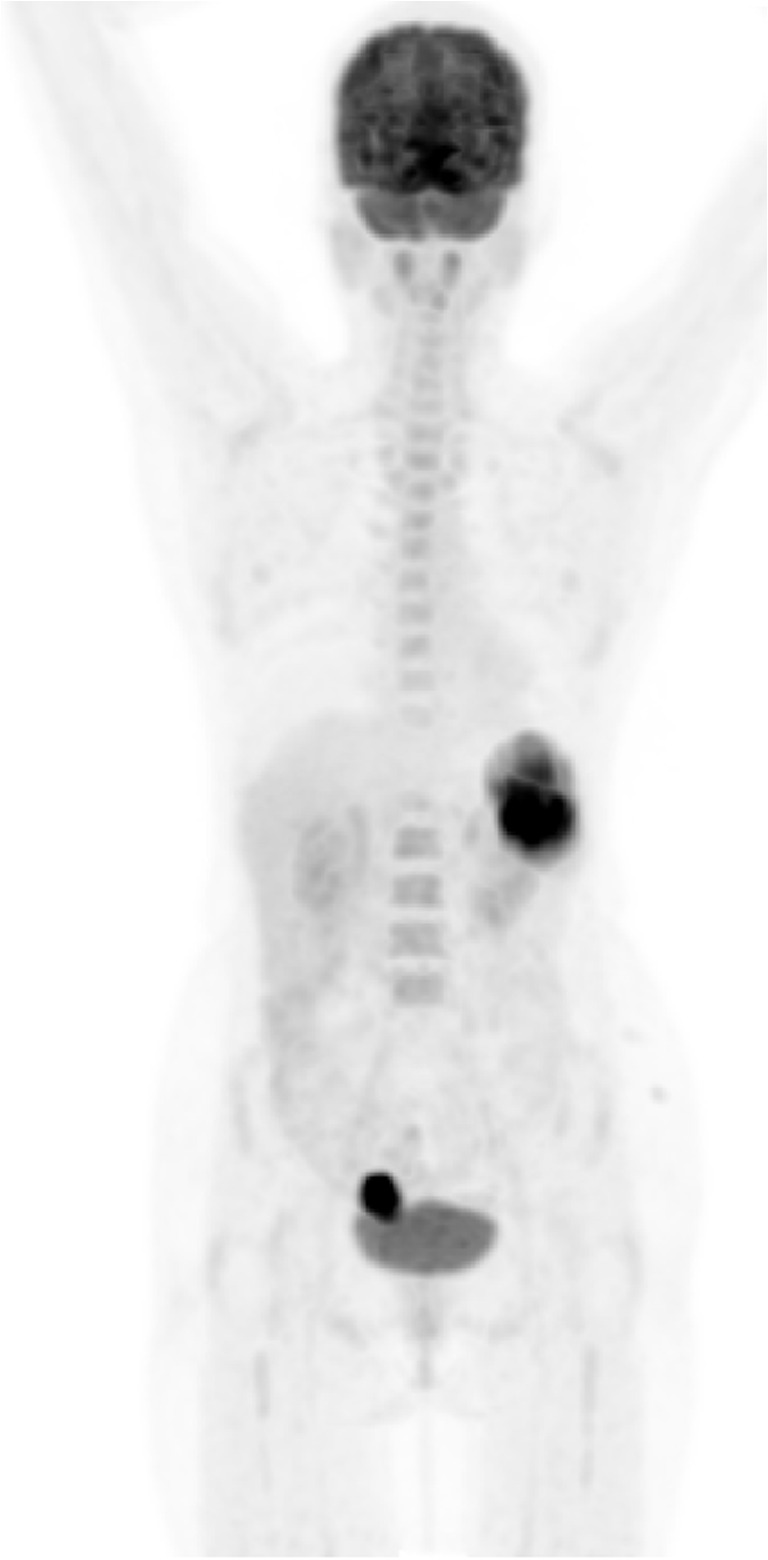
PET image
Fig. 2.
PET/CT image
She had undergone radical hysterectomy for carcinoma of cervix one and a half years back. Histopathology was moderately differentiated squamous cell carcinoma. The tumour was 2×1 cm in size and friable. It involved the entire cervix with superior extent for 1.8 cm and involving the serosa laterally on both sides. The endometrium and endometrial cervical junction were free of tumour. Lymphatic emboli were seen.
She had also received 50 Gy of intensity modulated radiation therapy (IMRT) in 25 fractions and weekly cisplatin 50 mg for 6 weeks.
Patient underwent laparoscopy and intraoperative findings were - enlarged spleen with a mass lesion and a mass in ileal mesentery adherent to the peritoneum over fundus of bladder and greater omentum. A segment of ileum along with the mesenteric mass, attached part of omentum and bladder peritoneum was resected and anastomosed laparoscopically, and splenectomy was done.
On gross examination, the spleen showed a tumour of size 8×6×4.5 cm reaching up to the capsule, with the capsule being focally deficient (Fig. 3). The ileal resection specimen showed a mesenteric soft tissue mass lesion of size 3.3×3×1.5 cm with necrotic areas within (Fig. 4). The ileal wall was not involved.
Fig. 3.

Specimen of spleen
Fig. 4.

Specimen of ileum with mesenteric deposit
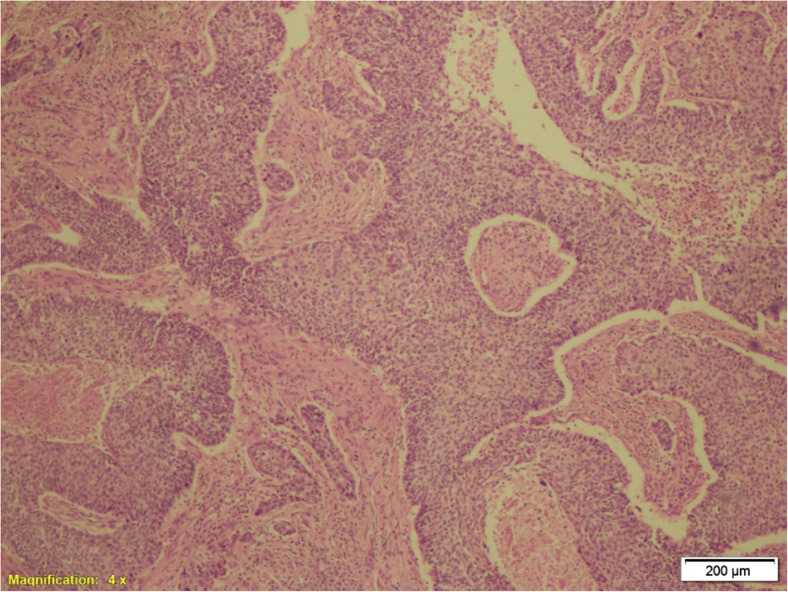
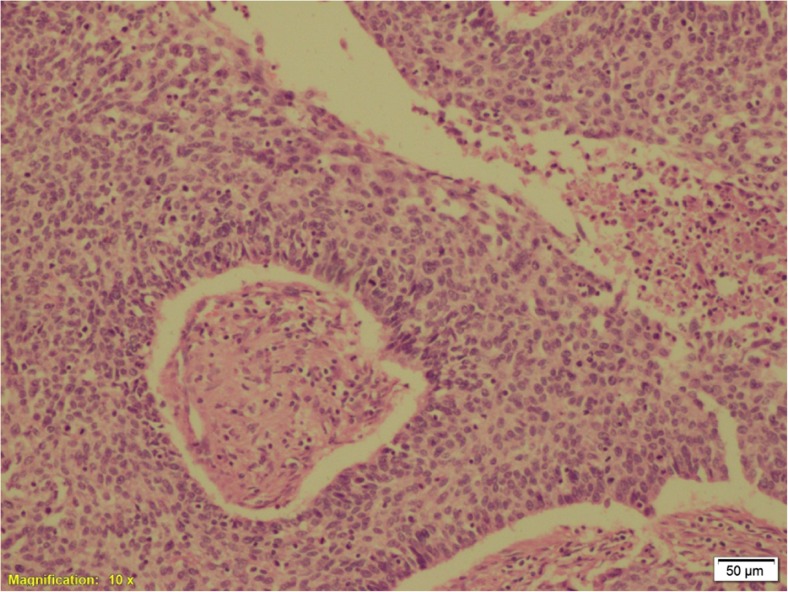
Histology showed metastatic poorly differentiated carcinoma in both specimens (Figs. 5 and 6). Immunohistochemistry showed neoplastic cells diffusely expressing CK 5/6 and p16, which are suggestive of squamous cell carcinoma associated with high-risk human papilloma virus. CK 5/6 has a sensitivity of 0.84 and specificity of 0.79 for squamous cell carcinoma [1]. p16 in squamous cell carcinoma is suggestive of association with high-risk HPV [2].
Fig. 5.
Histopathologic slide of the metastasis in spleen
Fig. 6.
Histopathologic slide of the metastasis in spleen
Post-operative recovery of the patient was good. Since the patient had distant metastatic recurrence, she was started on chemotherapy 4 weeks after the surgery. Patient was started on a combination of cisplatin and paclitaxel and was undergoing chemotherapy during the submission of this article.
Discussion
Cancer of uterine cervix is the most common cancer in females in India [3]. Seventy to eighty percent are squamous cell carcinoma and 10–15 % are adenocarcinoma. The most common path of spread of cervical cancer is direct lateral extension in the parametria. Lymphatic and hematogenous spread also occur. A 10–20 % recurrence rate has been reported following primary surgery or radiotherapy in women with stage IB-IIA cervical tumours with no evidence of lymph node involvement, while up to 70 % of patients with nodal metastases and/or more locally advanced tumours will relapse [4–7]. Pelvic recurrence is more common than distant recurrence. In a study by Fagundes et al., the most frequently observed distant metastatic sites are lung (21 %), para-aortic nodes (11 %), abdominal cavity (8 %) and supraclavicular nodes (7 %). The 10-year incidence of distant metastases was 3 % in stage IA, 16 % in stage IB, 31 % in stage IIA, 26 % in stage IIB, 39 % in stage III and 75 % in stage IVA. The median survival of patients with distant metastasis was 12 weeks, which was less than for those with lymph node metastasis [8]. Patients with metastatic or recurrent tumour have pain, anorexia, cachexia and/or generalised weakness.
In the case which we are reporting, the patient had undergone radical hysterectomy followed by radiation therapy and chemotherapy. Histopathologically, the tumour was stage IB1. She was asymptomatic for a period of 17 months. Then, she developed fever and anorexia. PET/CT showed recurrence in the spleen and in the mesentery within pelvis. Histology of spleen and mesenteric lesion after surgery showed metastatic poorly differentiated carcinoma; immunohistochemistry confirmed the primary to be from squamous cell carcinoma of uterine cervix associated with high-risk HPV.
Metastases to the spleen from solid tumours are very rare. They were mainly detected in autopsy specimen. Splenic artery, splenic vein and lymphatics are the possible routes of metastasis to spleen [9]. There are many proposed reasons given for the decreased incidence of metastasis to the spleen—acute angle at the origin of splenic artery and its tortuosity, lack of afferent lymphatics to the splenic parenchyma, splenic capsule which may act as an effective barrier, rhythmic contractions of the spleen, immunity and possibly antineoplastic properties of the splenic tissue [10]. However, the frequency of detection of splenic metastases in living patients has increased due to the improvement in imaging. They can occur as a part of disseminated metastases more commonly or as a solitary splenic metastasis rarely.
Solitary splenic metastasis can cause a diagnostic dilemma with primary tumours of spleen. They can present with abdominal pain, fullness of abdomen, abdominal mass or uncommonly with splenic rupture as an emergency. Splenectomy is an appropriate treatment in these cases which can confirm the histopathology and avoid complications like splenic rupture, splenic vein thrombosis and painful splenomegaly, and to prevent the splenic metastasis being a source for further metastatic disease [11].
The most common primary sources of splenic metastasis are breast, lung, colorectal, and ovarian carcinomas and melanoma in cases of multivisceral cancer and colorectal and ovarian carcinomas in cases of solitary splenic lesion [12]. In 2001, Agha-Mohammadi et al. reported a series of 54 patients, with isolated splenic metastasis, and found the most common malignancy to be gynaecologic [13] (Table 1). According to a study by Piura et al. published in 2010, less than 100 cases of solitary splenic metastases have been reported with half of them being metastases from female genital tract malignancies: 30—ovarian carcinoma, 11—endometrial carcinoma, 8—cervical carcinoma and 1—tubal carcinoma [14].
Table 1.
Percentage of isolated splenic metastases caused by different primary cancers [13]
| Site of primary | Percentage of isolated splenic metastases caused |
|---|---|
| Gynaecologic | 61 % |
| Colorectal | 15 % |
| Lung | 9 % |
| Stomach | 4 % |
Cervical cancer giving rise to metastasis in spleen is rarely seen. It is still rarer in living patients. Splenic metastases from cervical carcinoma are divided equally between metastases as part of a disseminated disease and solitary metastases [14]. Solitary splenic metastasis from squamous cell carcinoma of uterine cervix was first reported by Brufman et al. in 1977 [15]. As per our knowledge, 11 cases of squamous cell carcinoma metastatic to spleen without evidence of disseminated disease have been reported [9, 15–24]. Our case is possibly the 12th reported case.
Since it is considered distant metastasis, it is rational to give chemotherapy for all cases of splenic metastasis. Cisplatin was considered the most active drug in cancer of uterine cervix for a long time [25]. However, combination chemotherapy is more commonly used now with evidence of better response. Cisplatin/paclitaxel combination is one of the first line chemotherapy combinations considered in the treatment of recurrent or metastatic cervical cancer [26, 27].
Conclusion
This was a rare case of early cancer of cervix which received treatment in the form of surgery, radiation and chemotherapy, and presented 17 months later with vague symptoms and was found to have metastasis in the spleen and mesentery of ileum.
Metastasis from cervical cancer does not occur frequently to spleen. But it should be suspected if splenic lesion is detected during follow-up. Splenectomy is an appropriate option which prevents further complications and has possible good results.
References
- 1.Kaufmann O, Fietze E, Mengs J, Dietel M. Value of p63 and cytokeratin 5/6 as immunohistochemical markers for the differential diagnosis of poorly differentiated and undifferentiated carcinomas. Am J Clin Pathol. 2001;116(6):823–830. doi: 10.1309/21TW-2NDG-JRK4-PFJX. [DOI] [PubMed] [Google Scholar]
- 2.O’Neill CJ, McCluggage VVG. p16 expression in the female genital tract and its value in diagnosis. Adv Anat Pathol. 2006;13(1):8–15. doi: 10.1097/01.pap.0000201828.92719.f3. [DOI] [PubMed] [Google Scholar]
- 3.Nandakumar A, Ramnath T, Chaturvedi M. The magnitude of cancer cervix in India. Indian J Med Res. 2009;130:219–221. [PubMed] [Google Scholar]
- 4.Delgado G, Bundy B, Zaino R, et al. Prospective surgical-pathological study of disease-free interval in patients with stage IB squamous cell carcinoma of the cervix: a gynecologic oncology group study. Gynecol Oncol. 1990;38:352–357. doi: 10.1016/0090-8258(90)90072-S. [DOI] [PubMed] [Google Scholar]
- 5.Zaino RJ, Ward S, Delgado E, et al. Histopathologic predictors of the behavior of surgically treated stage IB squamous cell carcinoma of the cervix. A Gynecol Oncol Group Study Cancer. 1992;69:1750–1758. doi: 10.1002/1097-0142(19920401)69:7<1750::aid-cncr2820690717>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 6.Burghardt E, Baltzer J, Tulusan AH, et al. Results of surgical treatment of 1028 cervical cancers studied with volumetry. Cancer. 1992;70:648–655. doi: 10.1002/1097-0142(19920801)70:3<648::AID-CNCR2820700318>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 7.Stehman FB, Bundy BN, DiSaia PJ, et al. Carcinoma of the cervix treated with radiation therapy I. A multi-variate analysis of prognostic variables in the gynecologic oncology group. Cancer. 1991;67:2776–2785. doi: 10.1002/1097-0142(19910601)67:11<2776::AID-CNCR2820671111>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 8.Fagundes H, Perez CA, Grigsby PW, et al. Distant metastases after irradiation alone in carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys. 1992;24:197–204. doi: 10.1016/0360-3016(92)90671-4. [DOI] [PubMed] [Google Scholar]
- 9.Pang LC. Solitary recurrent metastasis of squamous cell carcinoma of the uterine cervix in the spleen: case report. South Med J. 2004;97(3):301–304. doi: 10.1097/01.SMJ.0000078684.66137.89. [DOI] [PubMed] [Google Scholar]
- 10.Koh YS, Kim JC, Cho CK. Splenectomy for solitary splenic metastasis of ovarian cancer. BMC Cancer. 2004;4:96. doi: 10.1186/1471-2407-4-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Piura B, Rabinovich A, Apel-Sarid L, Shacol-Levy R. Splenic metastasis from endometrial carcinoma: report of a case and review of literature. Arch Gynecol Obstet. 2009;280(6):1001–1006. doi: 10.1007/s00404-009-1039-7. [DOI] [PubMed] [Google Scholar]
- 12.Compéra E, Bardier-Dupas A, Camparo P, Capron F, Charlott F. Clinicopathologic presentation, differential diagnosis, and pathogenesis. Arch Pathol Lab Med. 2007;131:965–969. doi: 10.5858/2007-131-965-SMCPDD. [DOI] [PubMed] [Google Scholar]
- 13.Agha-Mohammadi S, Calne RY. Solitary splenic metastasis. Am J Clin Oncol. 2001;24:306–310. doi: 10.1097/00000421-200106000-00020. [DOI] [PubMed] [Google Scholar]
- 14.Piura E, Piura B. Splenic metastases from female genital tract malignancies. Harefuah. 2010;149(5):315–320. [PubMed] [Google Scholar]
- 15.Brufman G, Biran S, Goldschmidt Z, et al. Solitary metastatic involvement of the spleen in squamous cell carcinoma of the cervix. Harefuah. 1977;92(8):349–350. [PubMed] [Google Scholar]
- 16.Carvalho L, et al. Squamous cell carcinoma of the cervix metastatic to spleen- case report. Gynecol Oncol. 1997;67(1):107–110. doi: 10.1006/gyno.1997.4814. [DOI] [PubMed] [Google Scholar]
- 17.Goktolga U, Dede M, Deveci G, Yenen MC, et al. Solitary splenic metastasis of squamous cell carcinoma of the uterine cervix: a case report and review of literature. Eur J Gynaecol Oncol. 2004;25(6):742–744. [PubMed] [Google Scholar]
- 18.Aitelhaj M, Khoyaali SL, Boukir A, et al. Breast and splenic metastases of squamous cell carcinoma from the uterine cervix: a case report. J Med Case Rep. 2014;8:359. doi: 10.1186/1752-1947-8-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taga S, Sawada M, Nagai A, et al. Splenic metastasis of squamous cell carcinoma of the uterine cervix: a case report and review of literature. Case Rep Obstet Gynecol. 2014;2014:798948. doi: 10.1155/2014/798948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sharma P, Chatterjee P, Mazumdar B. Recurrent carcinoma cervix presenting as metastatic splenomegaly: 18F-FDG PET?CT findings in a rare scenario. Indian J Nucl Med. 2014;29(3):200–201. doi: 10.4103/0972-3919.136608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhardwaj S, Mahajan D, Vir Gupta Y. Metastatic squamous cell carcinoma of the cervix presenting as a splenic cyst. J K Science. 2008;10(3):146–148. [Google Scholar]
- 22.Gupta T, Nair N, Fuke P, et al. Splenic metastases from cervical carcinoma: a case report. Int J Gynecol Cancer. 2006;16(2):911–914. doi: 10.1111/j.1525-1438.2006.00220.x. [DOI] [PubMed] [Google Scholar]
- 23.Kim JH, et al. Solitary splenic metastases from uterine cervical cancer: case reports and review of the literature. The Korean Journal of Pathology. 2008;42:317–322. [Google Scholar]
- 24.Di Donato V, Palaia I, Perniola G, Polidori N, Burratti M, Besharat A, Panici PB. Splenic metastasis from cervical cancer: case report and review of literature. J Obstet Gynaecol Res. 2010;36(4):887–890. doi: 10.1111/j.1447-0756.2010.01210.x. [DOI] [PubMed] [Google Scholar]
- 25.Thigpen JT, Shingleton H, Homesley H, et al. Cis-platinum in treatment of advanced or recurrent squamous cell carcinoma of the cervix: a phase II trial of the gynecologic oncology group. Cancer. 1981;48:899–903. doi: 10.1002/1097-0142(19810815)48:4<899::AID-CNCR2820480406>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 26.Monk BJ, Sill MW, McMeekin DS, et al. Phase III trial of four cisplatin- containing doublet combinations in stage IVB, recurrent, or persistent squamous cell carcinoma: a gynecologic oncology group study. J Clin Oncol. 2009;27:4649–4655. doi: 10.1200/JCO.2009.21.8909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Moore DH, Blessing JA, McQuellon RP, et al. Phase III study of cisplatin awith or without paclitaxel in stage IVB, recurrent, or persistent squamous cell carcinoma of the cervix: a gynecologic oncology group study. J Clin Oncol. 2004;22:3113–3119. doi: 10.1200/JCO.2004.04.170. [DOI] [PubMed] [Google Scholar]