Abstract
Background
Abdominal obesity is a major risk factor for morbidity and mortality. The aim of this study was to investigate the effect of yoga on waist circumference and other anthropometric and self-reported variables in women with abdominal obesity.
Methods
60 women with abdominal obesity (waist circumference = 88 cm; body-mass index [BMI] = 25) were randomly allocated in a 2:1 ratio to either a 12-week yoga intervention (n = 40) or a waiting list (n = 20). The waist circumference was the primary endpoint. Secondary (exploratory) endpoints included the waist/hip ratio, body weight, BMI, body fat percentage, body muscle mass percentage, blood pressure, health-related quality of life, self-esteem, subjective stress, body awareness, and body responsiveness, and the safety of the intervention. The persons assessing the outcomes were blinded to the group to which the patients belonged.
Results
The patients in the yoga group participated in a mean of 30.2±9.2 (maximum, 42) hours of supervised yoga practice. Their abdominal circumference was significantly reduced in comparison to the participants on the waiting list, with an intergroup difference of –3.8 cm (95% confidence interval [-6.1; –1,.5]; p = 0.001). There were further, moderate intergroup differences in the waist/hip ratio, body weight, BMI, body fat percentage, body muscle mass percentage, mental and physical well-being, self-esteem, subjective stress, body awareness, and trust in bodily sensations (all p<0.05). There were no serious adverse events. None of the participants embarked on a low-calorie diet while participating in the study.
Conclusion
The 12-week yoga intervention had moderately strong positive effects on anthropometric and self-reported variables in women with abdominal obesity. Yoga is safe in this population and can be recommended as a technique for combating abdominal obesity in women.
The prevalence of obesity worldwide is rising, especially in developing countries and newly industrializing countries. The point prevalence is higher in women (15%) than in men (11%), which corresponds to a relative risk of 1.4 (1). Especially abdominal obesity—an unfavorable accumulation of fat around the stomach, which is not limited to overweight persons—has been identified as an important risk factor for cardiovascular and metabolic disorders (2, 3). Since, in addition to inadequate eating habits, a sedentary lifestyle is the main cause of obesity (4), regular physical activity is recommended in the medical guidelines as the most important therapeutic option in non-morbid obesity (5). However, the fact that a substantial proportion of obese persons does not adhere to such recommendations (6) provides a legitimate reason for studying alternative forms of physical activity to reduce weight.
Yoga is one such alternative form of physical activity that is used increasingly for the purpose of health promotion (7, 8). In North America and Europe, yoga comprises mainly body postures (asanas), breathing exercises (pranayama), and meditation (dhyana). Yoga is also gaining increasing popularity as a therapeutic measure. Some 80% of persons practicing yoga in the US (more than 16 million people) reported that they had taken up the practice with the explicit goal of improving their health (10, 11). In this setting, the hope to lose weight was one of the most important reasons for taking up yoga (12).
Although initial evidence for the effectiveness of yoga on weight control and improved body composition from surveys (13) and clinical studies (14) is now available, the effects of yoga on abdominal obesity have not been investigated to date. Our study investigated the effect of yoga on waist circumference and further anthropometric measures in women with abdominal obesity.
Method
Study design
The study was conceived as a single center, single blinded randomized controlled trial (RCT). Before patients were recruited, the study was approved by the ethics committee at the University of Duisburg-Essen (approval number 15–6194-BO), and it was registered with ClinicalTrials.gov (registration number NCT02420145). The study was conducted and reported in accordance with the CONSORT 2010 statement (15).
Study participants
Participants were recruited by placing announcements in the local press and by using email lists from local businesses. Women who expressed an interest underwent a telephone interview with a study assistant and were invited for a medical examination after an initial selection had been made. The exam included a physical examinationi as well as medical and medication histories. Suitable participants (box) received detailed information in written and verbal form, and written consent was obtained from these women.
Box. Inclusion and exclusion criteria.
-
Inclusion criteria
Female sex
No regular physical exercise
Age 18-64 years
Waist circumference = 88 cm
Body mass index (BMI) = 25
Willingness to participate at least in the full-day workshop and 18 of the 24 weekly sessions and to practice at home
-
Exclusion criteria
Physical impairments that preclude participation in easy yoga exercises
Regular physical activity or yoga practice within preceding 3 months*
Currently following a weight-loss diet or planning to start such a diet within the following 24 weeks
Dementia
Diagnosed psychosis that is being treated with psychopharmaceutical drugs
Malignant hypertension (diastolic blood pressure >120 mm Hg)
Diabetes mellitus type 1 or type 2 diabetes requiring insulin
Manifest coronary heart disease, myocardial infarction, pulmonary artery embolism, or apoplexy
Current participation in other clinical studies or planning to enter into a study within the following 24 weeks
Pregnancy or breastfeeding period
* Data on regular exercise (at least 2 x 30 minutes per week) and regular yoga practice (at least 60 minutes per week) were collected verbally during telephone screening and medical examination.
Randomization
The participants were allocated to a yoga group or a control group by using a randomized block design with randomly varying block lengths. The randomization list was set out by a biometrician who was not involved in patient recruitment or data collection and who used random allocation software (16). The list was password protected, and only the biometrician had access to it. After written consent had been received and the initial data collection had been completed, participants were centrally randomized by the biometrician.
Interventions
Yoga: The yoga intervention consisted of an initial full-day workshop, followed by two weekly 90-minute classes of traditional hatha yoga over a 12-week period. The yoga classes were based on integral yoga as developed by Swami Sivananda and an adaptation of the basic yoga-vidya sequence (17). eBoxes 1 and 2 show further details of the yoga program.
Waiting list: The women who had been allocated to the control group were entered into a waiting list and did not participate in any study interventions during the initial 12 weeks of the study. They were asked not to practice yoga during that period and to not change their habitual physical activities. After the end of the 12th week, subjects were free to participate in a yoga program identical to that of the intervention group. The purpose was to motivate participants. No further data were collected.
Outcome measures
The outcome assessment was conducted by persons who had been blinded to the group allocation and had not been involved in patient recruitment, randomization, or interventions. Participants were explicitly asked not to mention their group allocation to these persons, and both parties were instructed to restrict their communication to collecting anthropometric measurements and questionnaire data.
As our primary outcome measure we defined waist circumference at week 12. Secondary researcher-assessed measures defined a priori included the waist-hip ratio, body weight, body mass index (BMI), bioelectrical impedance analysis, and blood pressure (ebox 1). Secondary patient-reported measures defined a priori included:
Key Messages.
An intensive 12 week yoga program in women with abdominal obesity led to a significant reduction in waist circumference compared with an untreated control group.
Yoga reduced the waist-hip ratio, body weight, BMI, and percentage of body fat and increased the percentage of body muscle.
Furthermore, the intervention increased mental and physical quality of life and self-esteem, and it reduced subjective stress.
Both groups experienced only minor adverse events.
Yoga can be recommended to women for the purpose of reducing abdominal obesity.
Quality of life, collected by administering the short form-36 health survey (SF-36) (18)
Self esteem, collected by using Rosenberg’s self esteem scale (19)
Perceived stress, determined by using the German 10-item version of the perceived stress scale (20), and
Body awareness, collected by using the German 17-item version of the body awareness questionnaire (21)
Body responsiveness, captured by using the German two-factorial 6-item version of the body responsiveness scale (22).
All adverse events that occurred during the study period were documented (ebox 1).
Sample size calculation and statistical evaluation
We calculated the required sample size a priori on the basis of a study from South Korea, which compared yoga versus “no intervention” in postmenopausal obese women (23). On the basis of this study, a group difference of d=1.02 in waist circumference was expected. If this effect is assumed, a t test with a two-sided significance level of a = 0.05 requires a total of 48 participants in order to determine a difference between groups with 90% power if a 2:1 allocation ratio is applied. In order to avoid a potential loss in power owing to a dropout rate of up to 20% of study participants, we planned to include 60 subjects into the study and to assign 40 participants to the yoga group and 20 participants to the control group.
We analyzed the outcome measures on the basis of the intention to treat principle. All randomized participants were included in the analysis, independently of whether a complete dataset was available or whether the study was conducted according to the protocol. Missing values were multiply imputed by using the Markov chain Monte Carlo procedure (24, 25). This yielded a total of 50 complete datasets. Additionally, we conducted sensitivity analyses for the main outcome measure, by including, on the one hand, only participants with complete datasets and, on the other hand, only the per protocol population—that is, participants with complete datasets who had participated in at least 18 yoga units and the initial workshop.
We used Students's t tests for continuous data and the chi-square test for categorical data to analyze possible differences in sociodemographic or anthropometric parameters at baseline.
Waist circumference at week 12 was defined as the primary outcome measure and was evaluated by using univariate analysis of covariance (ANCOVA), with the outcome measure modeled as a function of group allocation (two classes) and the respective baseline value (linear covariate), in order to achieve an overall effect estimate, the 95% confidence interval, and the P-value. All other variables were defined as secondary outcome measures and were analyzed exploratively by using analog ANCOVA models.
As a measure of the clinical relevance of the results, we compared the number of participants in both groups, which by week 12 had achieved a clinically relevant reduction in their waist circumference of at least 5% (26). Furthermore, we calculated the number needed to treat (NNT). In order to assess the safety of the intervention we used the chi-square test to compare the number of participants in both groups who experienced adverse events during the study period. All analyses were done by using SPSS software (Statistical Package for Social Sciences-Software, Statistics for Windows, Version 22.0, Armonk, NY, USA: IBM Group).
Results
Participants
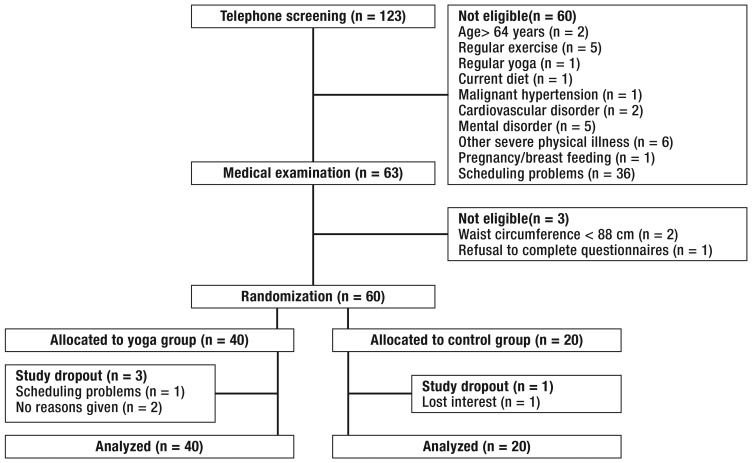
In total we surveyed 123 women in telephone interviews, 60 of whom were excluded because of a lack of interest or because they did not meet the inclusion criteria (Figure). A study physician examined 63 women in order to ascertain their eligiblity for inclusion in the study; 3 of those women were excluded. 60 women met all inclusion criteria and were included in the study after they had given informed consent; these were randomized into the yoga group (n=40) and the control group (n=20). Three participants in the yoga group (7.5%) and one participant in the control group (5%) did not complete the second data collection in week 12 (Figure).
Figure 1.
Flow chart of study participation
Table 1 shows participants’ sociodemographic and anthropometric characteristics. The participants’ mean age was 47.8±8.2 years, most were married or in long-term relationships, had (vocational) A level equivalents, and were in work. Some participants had previous experiences with yoga.
No significant differences existed between the groups with regard to sociodemographic data. The mean waist circumference was 104.3±10.3 cm, the mean BMI was 34.2±5.4. At baseline, the participants in the control group had higher values in terms of height, hip circumference, BMI, and percentage of body fat compared with the participants in the yoga group (table 1).
Table 1. Sociodemographic and anthropometric characteristics at baseline (mean ± standard deviation).
|
Total (n = 60) |
Yoga (n = 40) |
Control group (n = 20) |
P | |
| Sociodemographic characteristics | ||||
| Age years | 47.8±8.2 | 48.5±7.9 | 46.4±8.9 | 0.340 |
| Marital status n (%) | 0.328 | |||
|
44 (73.3 %) | 31 (77.5 %) | 13 (65.0 %) | |
|
16 (26.7 %) | 9 (22.5 %) | 7 (35.0 %) | |
| No of children | 1.3±0.9 | 1.4±0.9 | 1.3±0.9 | 0.058 |
| Education n (%) | 0.378 | |||
|
3 (5.0 %) | 2 (5.0 %) | 1 (5.0 %) | |
|
21 (35.0 %) | 11 (27.5 %) | 10 (50.0 %) | |
|
13 (21.7 %) | 10 (25.0 %) | 3 (15.0 %) | |
|
23 (38.3 %) | 17 (42.5 %) | 6 (30.0 %) | |
| Employment status n (%) | 0.176 | |||
|
30 (50 %) | 19 (47.5 %) | 11 (55.0 %) | |
|
23 (33.3 %) | 18 (45.0 %) | 5 (25.0 %) | |
|
7 (11.7 %) | 3 (7.5 %) | 4 (20.0 %) | |
| Nationality n (%) | 1.000 | |||
|
57 (95.0 %) | 38 (95.0 %) | 19 (95.0 %) | |
|
3 (5.0 %) | 2 (5.0 %) | 1 (5.0 %) | |
| Anthropometric characteristics | ||||
| Height (cm) | 166.8±6.6 | 168.1±6.5 | 164.1±6.0 | 0.024 |
| Weight (kg) | 95.3±16.2 | 93.2±14.7 | 99.5±18.5 | 0.155 |
| Body mass index | 34.2±5.4 | 32.9±4.1 | 36.9±6.6 | 0.018 |
| Waist circumference (cm) | 104.3±10.3 | 102.9±8.6 | 107.0±13.0 | 0.211 |
| Hip circumference (cm) | 120.3±11.5 | 118.0±10.5 | 124.8±12.3 | 0.029 |
| Waist-hip ratio | 0.87±0.05 | 0.87±0.04 | 0.86±0.06 | 0.247 |
| Percentage of body fat (%) | 45.0±4.8 | 44.0±4.5 | 46.8±5.0 | 0.033 |
| Percentage of body muscle mass (%) | 24.6±2.2 | 24.9±2.0 | 23.8±2.4 | 0.053 |
| Blood pressure | ||||
| Systolic mm Hg | 134.0±14.1 | 133.3±14.1 | 135.4±14.1 | 0.594 |
| Diastolic mm Hg | 86.7±10.1 | 86.2±11.2 | 87.8±7.6 | 0.556 |
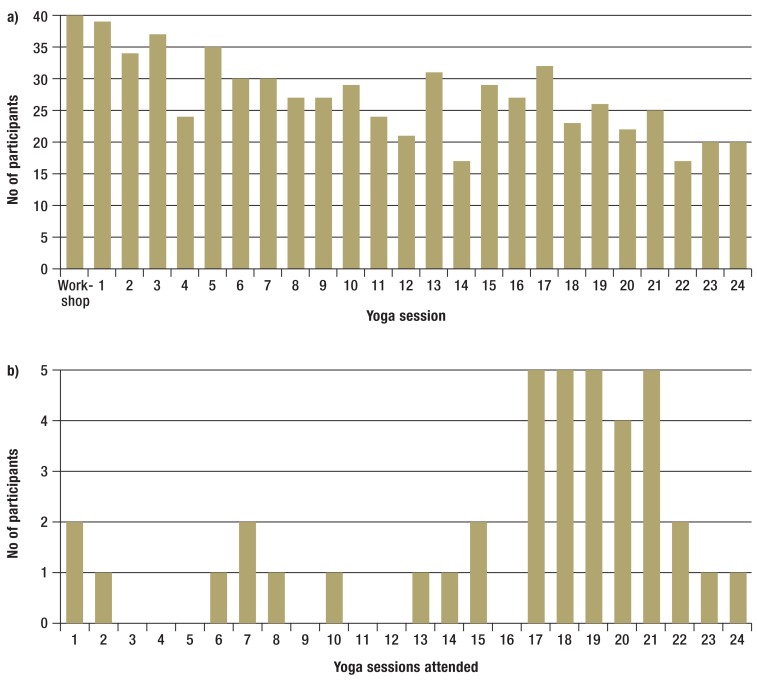
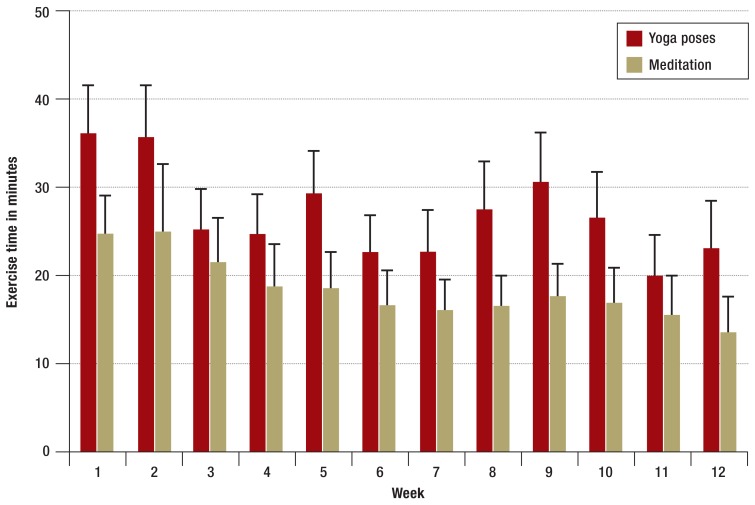
All participants in the yoga group participated in the initial full-day workshop; adherence to the intervention fell during the course of the study (figure 1). In total, the participants in the yoga group underwent a mean of 16.1±6.1 of a maximum of 24 yoga units (67.1%). This corresponds to an overall mean value of 30.2±9.2 of a maximum of 42 hours of supervised yoga practice (workshop plus weekly yoga sessions) (71.9%). Furthermore, they practiced a mean of 38.7±16.1 minutes at home (eFigure 2).
None of the participants started a calorie-reduced diet during the study period.
Researcher-assessed measures
With regard to the primary outcome measure, participants in the yoga group were found to have a significantly lower waist circumference than those in the control group (P=0.001; Table 2).
The sensitivity analyses showed comparable results in the participants with complete datasets (difference between groups –3.7 cm; 95% confidence interval [–6.2; –1.2]; P=0.004) and in the per-protocol analysis (between group difference –4.8 cm; [–7.5;–2.0]; P=0.001).
13 participants in the yoga group (32.5%) achieved a clinically relevant reduction in waist circumference of at least 5%, compared with 2 participants in the control group (10.0%). This corresponds to an NNT of 4.3 [2.4; 33.3].
Further differences between the groups were observed for the waist-hip ratio (P=0.034), body weight (P=0.003), BMI (P=0.008), percentage of body fat (P=0.007), and percentage of body muscle mass (P=0.010; Table 1). No differences between groups were observed for systolic (P=0.446) and diastolic (P=0.709) blood pressure.
Patient-reported measures
Regarding health related quality of life, differences between the groups were observed in week 12 in favor of the yoga group, on the physical (P=0.018) and mental component score (P=0.009) and all subscales of health related quality of life (P<0.05), with the exception of the subscale for emotional role functioning (table 3). Further differences between the groups were found with regarding to self esteem (P<0.002), perceived stress (P=0.016), body awareness (P=0.001), and the subscale “trust in bodily sensations” (subscale of the body responsiveness scale) (P<0.001); Table 3).
Table 3. Effects (mean ± standard deviation) in the yoga and control groups on self-assessment measures.
| Yoga group (n = 40) | Control group (n = 20) | Difference between groups [95% CI] week 12 | P | |||
| Week 1 | Week 12 | Week 1 | Week 12 | |||
| Health related quality of life (SF-36) | ||||||
|
80.4±17.6 | 87.8±13.2 | 74.3±20.1 | 74.3±17.5 | 11.1 [3.9; 18.2] | 0.003 |
|
76.3±29.9 | 85.2±27.2 | 58.8±40.0 | 60.9±38.4 | 17.2 [1.1; 33.3] | 0.037 |
|
75.5±24.4 | 78.5±22.6 | 57.1±23.1 | 56.2±24.5 | 12.2 [0.8; 23.4] | 0.036 |
|
71.1±15.2 | 76.5±15.7 | 61.0±18.3 | 60.0±19.1 | 10.6 [2.5; 18.6] | 0.011 |
|
55.8±18.0 | 68.3±13.6 | 48.3±17.9 | 51.1±17.1 | 13.9 [6.5; 21.3] | < 0.001 |
|
85.0±21.4 | 86.7±17.5 | 71.3±24.4 | 68.6±28.6 | 11.7 [0.7; 22.7] | 0.038 |
|
84.2±29.2 | 87.1±25.9 | 66.7±39.0 | 66.8±41.9 | 10.5 [−4.5; 25.4] | 0.167 |
|
70.0±14.4 | 80.0±13.1 | 63.2±18.3 | 63.2±18.3 | 12.6 [5.4; 19.7] | 0.001 |
|
48.9±7.8 | 51.5±7.4 | 44.0±10.2 | 44.2±9.4 | 4.5 [0.8; 8.2] | 0.018 |
|
49.4±9.5 | 53.4±7.2 | 44.7±12.2 | 44.8±13.9 | 5.6 [1.4; 9.8] | 0.009 |
| Self-esteem (SES) | 38.8±4.3 | 39.9±4.3 | 37.3±5.7 | 35.6±6.3 | 3.1 [1.2; 5.0] | 0.002 |
| Perceived stress (PSS) | 28.0±4.5 | 24.9±3.9 | 29.8±5.0 | 28.8±6.5 | −3.1 [−5.6; −0.6] | 0.016 |
| Body awareness (BAQ) | 76.9±14.4 | 83.0±13.1 | 76.8±9.9 | 73.6±15.0 | 9.3 [4.0; 14.6) | 0.001 |
| Body responsiveness (BRS) | ||||||
|
17.5±4.0 | 21.0±3.4 | 16.7±3.8 | 16.2±4.3 | 4.4 [2.6; 6.2] | < 0.001 |
|
6.1±3.1 | 5.1±3.0 | 5.7±3.0 | 5.0±2.6 | 0.3 [−0.9; 1.5] | 0.662 |
CI, confidence interval
Safety: no serious adverse events occurred. 13 women (32.5%) in the yoga group experienced 16 mild adverse effects; 5 women in the control group (25.0%) experienced a total of 6 mild adverse effects (P=0.550; eBox 1).
Discussion
In the present randomized trial of women with abdominal obesity, participation in an intensive 12-week yoga intervention led to a positive—if not very pronounced—change in anthropometric measures, quality of life, and mental health, while incurring only a small number of adverse events.
Thus far, only few randomized studies have explicitly focused on the effect of yoga on anthropometric measures in overweight or obese persons. On the basis of the few available studies, recent meta-analyses showed that yoga was effective with regard to anthropometric variables in overweight or obese persons as well as in patients with type 2 diabetes or other cardiovascular risk constellations (14, 27).
However, as far as we are aware, no study to date has investigated the effect of yoga on waist circumference in otherwise healthy women with abdominal obesity. Since abdominal obesity is a much stronger predictor for the risk of cardiovascular disorders than body weight or the BMI (2, 3), our study closes an important gap in assessing the effectiveness of yoga regarding cardiovascular risk.
The existing publications give rise to the assumption that the effects of yoga on anthropometric measures can be increased by a greater frequency, a longer duration, and the use of complex yoga interventions with multiple components and in combination with dietary/nutritional recommendations (especially of a vegetarian diet with or without calorie reduction) and homework (28). Accordingly, these factors were considered in developing the intervention in the present study.
While yoga lessons for beginners are associated with little intense physical activity and therefore do not meet the recommendations for adequate cardiovascular exercise (29), more intensive styles of yoga can lead to higher energy consumption (29, 30) and thus contribute to weight loss and weight control (13). However, we think that it is unlikely that the identified anthropometric effects of the intervention are due exclusively to the increase in physical activity: the reduction in the proportion in body fat that was achieved in the yoga group corresponds to a reduction of 1.3 kg of pure fat, or 12 000 kcal. The mean energy expenditure in yoga (including yoga postures, breathing exercises, and meditation) is 2.2–3.2 kcal/minute (29, 31); higher values can be assumed for overweight participants (32). Accordingly, a conservative estimate would mean that the effect we found would require a yoga exercise commitment of between 63 and 92 hours, whereas the mean practice time in our study amounted to just under 38 hours. However, an interpretation that is based on physical activity only and does not consider other possible mechanisms of action is not far reaching enough: the practice of yoga can reduce back pain and joint pain (33, 34) and increase the extent of other physical activity (not associated with yoga) (35).
In addition to physical activity, the yoga intervention in the present study also comprised yoga-based nutritional advice and psychologically oriented elements, such as relaxation techniques, meditation, breathing exercises, and instructions for positive thinking. Yoga has been shown to alleviate chronic depression, stress, and other psychological disorders (36– 38). This could mean a reduction in overeating to compensate for negative feelings (emotional eating) and the resultant overweight (39). Accordingly, the mechanisms of action of the yoga intervention presented in this article might include a reduction in the physical factors (inadequate physical activity and diet) as well as the emotionally sustaining factors (emotional eating) underlying obesity. The comparatively good effectiveness of the intervention investigated in the present study may be due to this combination of different components.
Limitations
Our study has several limitations. The control group did not provide a control for attention-related unspecific effects or regression to the mean: while the participants in the intervention group may have experienced positive effects owing to expectation-related effects, participants in the control group may have experienced negative effects as a result of being disappointed about their group allocation. Furthermore, it was not possible to exclude completely independent participation in a yoga class outside the study setting by fundamentally motivated participants who had been allocated to a waiting-control group, which may bias the results. It was not possible to blind participants with regard to their allocated intervention. The study used an intensive program of yoga, and its results can therefore not be generalized to other, less intensive, yoga programs. Adherence to the intervention decreased over the course of the study. In spite of randomization, differences between the groups—by definition random—in terms of anthropometric variables occurred at the start of the study, although their effect was minimized by our use of analyses of covariance (40).
Implications for clinical practice
Future studies should investigate the effectiveness of yoga compared with other types of sports and nutritional programs and should study the long-term effects of the intervention. Studies should also investigate the generalizability to other populations, especially men. The dose-response relation should be investigated, especially with regard to adherence, which was very low towards the end of the study.
Conclusions
An intensive yoga intervention lasting 12 weeks including women with abdominal obesity reduced participants’ waist circumference, waist-hip ratio, body weight, BMI, and percentage of body fat and increased the percentage of muscle mass. Yoga improved participants’ mental and physical wellbeing and self esteem, and reduced their perceived stress. As the intervention constitutes a safe and effective intervention in this population, yoga can be recommended to women in order to reduced their abdominal obesity.
Table 2. Effects (mean ± standard deviation) in the yoga and control groups on externally assessed measures.
| Yoga group (n = 40) | Control group (n = 20) | Difference between groups [95% CI] week 12 | p | |||
| Week 1 | Week 12 | Week | Week 12 | |||
| Waist circumference (cm) | 102.9±8.6 | 99.2±9.8 | 107.0±13.0 | 107.1±13.2 | –3.8 [–6.1; –1.5] | 0.001 |
| Waist-hip ratio | 0.87±0.04 | 0.85±0.05 | 0.86±0.06 | 0.86±0.07 | –0.02 [–0.04; –0.00] | 0.034 |
| Body weight (kg) | 93.2±14.7 | 91.7±14.2 | 99.5±18.5 | 100.2±18.1 | –2.4 [–4.0; –0.9] | 0.003 |
| Body mass index | 32.9±4.1 | 32.4±4.2 | 36.9±6.6 | 37.2±6.4 | –0.8 [–1.4; –0.2] | 0.008 |
| Percentage of body fat (%) | 44.0±4.5 | 42.6±4.2 | 46.8±5.0 | 46.7±5.0 | –1.7 [–2.9; –0.5] | 0.007 |
| Percentage of body muscle mass (%) | 24.9±2.0 | 25.5±1.9 | 23.8±2.4 | 23.8±2.4 | 0.8 [0.2; 1.3] | 0.010 |
| Systolic blood pressure mm Hg | 133.3±14.1 | 129.5±14.6 | 135.4±14.1 | 133.1±12.6 | –2.6 [–9.4; 4.2] | 0.446 |
| Diastolic blood pressure mm Hg | 86.2±11.2 | 82.1±11.5 | 87.8±7.6 | 82.5±9.7 | 0.8 [–3.5; 5.1] | 0.709 |
CI, confidence interval
eBox 1. Additional methods and results.
-
Methods
Yoga intervention
The yoga intervention was specially conceived for this study by a certified teacher of hatha yoga with longstanding experience, in cooperation with a large national professional association of yoga teachers (BYV). The intervention was specifically adapted to the needs, capabilities, and limitations of women with abdominal obesity, with a particular focus on a reduction in waist circumference. The yoga sessions were delivered by a certified teacher of hatha yoga. The initial, full day, workshop (6 hours) and each yoga session comprised a series of selected yoga poses (asanas), breathing exercises (pranayama), deep relaxation (savasana), and dietary/nutritional recommendations on the basis of traditional yoga teachings, as well as instructions and practical exercises from the areas of meditation, positive thinking, and relaxation. Each yoga lesson consisted of 50–60 minutes of yoga poses and 30–40 minutes of other exercises, short lectures, and Q&A sessions. eBox 2 shows the key elements of the yoga program. All the exercises were introduced slowly and cautiously, and their intensity was increased throughout the course of the program. If required, props were used and/or the exercises were modified for individual participants.
The nutritional/dietary recommendations were based on traditional yoga teachings. The aim was to achieve a change in the composition of the diet (for example, a mostly plant based diet, more fresh and fewer industrially processed foods) and a more conscious approach to eating (for example, mindful eating), not primarily a reduction in calories. Participants were asked not to start a calorie-restricted diet during the study period.
Participants were encouraged to practice at home, in addition to participating in the intervention sessions, but they were not given a minimal practice time. Before the exercises were repeated at home they were introduced in detail in the yoga sessions. Participants recorded their daily practice period (in minutes) in a diary.
Researcher-assessed measures
Waist circumference was measured by two study assistants, using a tape measure at the horizontal level exactly midway between the costal arch and iliac crest. The measurements were repeated twice and the mean of both measurements was used; where measurements differed by more than 1 cm, both measurements were repeated (e1). The waist-hip ratio was calculated as the ratio of waist and hip circumference, the latter was measured at the horizontal level at the place of the largest circumference either in the hip or buttock region (above the gluteal sulcus), depending on which was larger. Further measurements were taken following the approach for waist circumference (e1). Weight measurements were taken by using the Omron BF511 bioelectrical impedance analysis device. The BMI was calculated as body weight in kg divided by the square of the body height in meters. In the context of the bioelectrical impedance analysis to determine the body composition, percentages of body fat and body muscle mass were determined by using the Omron BF511 bioelectrical impedance analysis device (e2). Systolic and diastolic blood pressure were measured as the mean of two measurements by using an internationally recognized digital blood pressure monitor (Mobil-O-Graph PWA, IEM, Stolberg [e3]).
Safety
All participants who experienced adverse events were asked to consult the study doctor, in order to assess the severity of their adverse events and to initiate the necessary measures, where needed. In week 12, open questions were used in order to document possible adverse events that had not been mentioned previously. Study participants were invited to report all adverse events occurring during the study period, independently of their potential association with the intervention. According to the GCP regulation (e4), an adverse event was defined as “any untoward occurrence in a trial subject administered an investigational medicinal product and which does not necessarily have a causal relationship with this treatment.” A serious adverse event was defined as“ […] any untoward event or reaction that results in death, is life-threatening, requires hospitalisation or prolongation of existing hospitalisation, results in persistent or significant disability or incapacity, or a congenital anomaly or birth defect.” All other adverse effects were defined as minor.
-
Results
Safety
Adverse events in the yoga group included transient back or neck pain (n=7), mild strains (n=2), abdominal pain (n=2), a fall (n=1), a broken toe (n=1), transient edema (n=1), toothache (n=1), transient dyspnea (n=1). Two adverse events—the broken toe and one case of abdominal pain—occurred in a temporal, and possible causal, association with the yoga intervention. The adverse events in the control group comprised back and neck pain (n=2), tendonitis (n=1), a torn ligament (n=1), bronchitis (n=1), and toothache (n=1).
Figure 2.
Adherence to the intervention: a) Number of participants in the initial workshop and the individual yoga sessions; b) Number of participants who attended a certain number of yoga sessions
eBox 2. Key elements of the yoga program (modified Yoga-Vidya basic sequence).
-
Theoretical introduction
On yoga, relaxation, yoga-based nutrition, Meditation/positive thinking
-
Body poses (asana)
Mountain pose (tadasana)
Modified sun salutation (surya namaskara)
Core exercises (navasana)
Half shoulder stand (ardha sarvangasana)
Bridge pose (setu bandhasana)
Fish (matsyasana)
(Half) seated forward bend (pascimottanasana)
Cobra (bhujangasana)
(Half) locust (salabhasana)
Cat (marjaryasana)
Downward dog (adho mukha svanasana)
Child pose (garbhasana)
Spinal twist pose (ardha matsyendrasana)
Tree (vrksasana)
Warrior II (virabhadrasana II)
Triangle (trikonasana)
Standing forward bend (pada hastasana)
-
Breathing exercises (pranayama)
Diaphragmatic breathing
Complete yoga breathing
Alternate nostril breathing (nadi sodhana)
Rapid inhalation and exhalation (kapalabhati)
-
Deep relaxation (savasana)
Progressive muscle relaxation
Autosuggestion
Visualization
Yoga nidra
-
Meditation (dhyana)
Breathing meditation
Simple mantra meditation
Gazing steadily at a fixed point (trataka)
-
Positive thinking
Affirmations
Figure 3.
Adherence to intervention: Exercise time at home in minutes per study week, by yoga pose and meditation
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Acknowledgment
We thank the professional association of Yoga Vidya Teachers (BYV), especially Vera Bohle and Vicara Shakti Müller, for their help in developing the yoga intervention, and Sonja Omlor for her support with patient recruitment and data collection.
Interessenskonflikt
Yoga Vidya reg. assoc. has reimbursed Ms Thoms for travel expenses. The remaining authors declare that no conflict of interest exists.
References
- 1.World Health Organization. WHO Press. Geneva: 2014. Global status report on noncommunicable diseases 2014. [DOI] [PubMed] [Google Scholar]
- 2.Westphal SA. Obesity, abdominal obesity, and insulin resistance. Clin Cornerstone. 2008;9:23–29. doi: 10.1016/s1098-3597(08)60025-3. [DOI] [PubMed] [Google Scholar]
- 3.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 4.Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet. 2010;376:1775–1784. doi: 10.1016/S0140-6736(10)61514-0. [DOI] [PubMed] [Google Scholar]
- 5.Suppl 2: American College of Cardiology/American Heart Association. Task Force on Practice Guidelines, Obesity Expert Panel: Guidelines (2013) for the management of overweight and obesity in adults. Obesity (Silver Spring) 2014;22:S5–S39. doi: 10.1002/oby.20821. [DOI] [PubMed] [Google Scholar]
- 6.Castellani W, Ianni L, Ricca V, Mannucci E, Rotella CM. Adherence to structured physical exercise in overweight and obese subjects: a review of psychological models. Eat Weight Disord. 2003;8:1–11. doi: 10.1007/BF03324983. [DOI] [PubMed] [Google Scholar]
- 7.Feuerstein G. The yoga tradition. Prescott: Hohm Press. 1998 [Google Scholar]
- 8.Iyengar BKS. Light on Yoga. New York: Schocken Books. 1966 [Google Scholar]
- 9.De Michelis E. Continuum International Publishing Group. London UK: 2005. A History of Modern Yoga: Patanjali and Western Esotericism. [Google Scholar]
- 10.Birdee GS, Legedza AT, Saper RB, Bertisch SM, Eisenberg DM, Phillips RS. Characteristics of yoga users: results of a national survey. J Gen Intern Med. 2008;23:1653–1658. doi: 10.1007/s11606-008-0735-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cramer H, Ward L, Steel A, Lauche R, Dobos G, Zhang Y. Prevalence, Patterns, and Predictors of Yoga Use: Results of a US. Nationally Representative Survey. Am J Prev Med. 2016;50:230–235. doi: 10.1016/j.amepre.2015.07.037. [DOI] [PubMed] [Google Scholar]
- 12.Park CL, Riley KE, Bedesin E, Stewart VM. Why practice yoga? Practitioners’ motivations for adopting and maintaining yoga practice. J Health Psychol. 2014 doi: 10.1177/1359105314541314. [DOI] [PubMed] [Google Scholar]
- 13.Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-aged men and women. Altern Ther Health Med. 2005;11:28–33. [PubMed] [Google Scholar]
- 14.Lauche R, Langhorst J, Lee MS, Dobos G, Cramer H. A systematic review and meta-analysis on the effects of yoga on weight-related outcomes. Prev Med. 2016;87:213–232. doi: 10.1016/j.ypmed.2016.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726–732. doi: 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 16.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4 doi: 10.1186/1471-2288-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vishnu-devananda S. Harmony. New York: 1995. The Complete Illustrated Book of Yoga. [Google Scholar]
- 18.Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 19.Rosenberg M. Society and the adolescent self-image Princeton. Princeton University Press. 1965 [Google Scholar]
- 20.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 21.Shields SA. The body awareness questionnaire. Journal of personality Assessment. 1989;53:802–815. [Google Scholar]
- 22.Daubenmier J. The relationship of yoga, body awareness, and body responsiveness to self-objectification and disordered eating. Psychology of Women Quaterly. 2005;29:207–219. [Google Scholar]
- 23.Lee JA, Kim JW, Kim DY. Effects of yoga exercise on serum adiponectin and metabolic syndrome factors in obese postmenopausal women. Menopause. 2012;19:296–301. doi: 10.1097/gme.0b013e31822d59a2. [DOI] [PubMed] [Google Scholar]
- 24.Rubin DB. John Wiley & Sons. New York: 1987. Multiple Imputation for Nonresponse in Surveys. [Google Scholar]
- 25.Schafer JL. Chapman and Hall. New York: 1997. Analysis of Incomplete Multivariate Data. [Google Scholar]
- 26.Verweij LM, Terwee CB, Proper KI, Hulshof CT, van Mechelen W. Measurement error of waist circumference: gaps in knowledge. Public Health Nutr. 2013;16:281–288. doi: 10.1017/S1368980012002741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cramer H, Lauche R, Haller H, Steckhan N, Michalsen A, Dobos G. Effects of yoga on cardiovascular disease risk factors: a systematic review and meta-analysis. Int J Cardiol. 2014;173:170–183. doi: 10.1016/j.ijcard.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 28.Rioux JG, Ritenbaugh C. Narrative review of yoga intervention clinical trials including weight-related outcomes. Altern Ther Health Med. 2013;19:32–46. [PubMed] [Google Scholar]
- 29.Hagins M, Moore W, Rundle A. Does practicing hatha yoga satisfy recommendations for intensity of physical activity which improves and maintains health and cardiovascular fitness? BMC Complement Altern Med. 2007;7 doi: 10.1186/1472-6882-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mody BS. Acute effects of Surya Namaskar on the cardiovascular & metabolic system. J Bodyw Mov Ther. 2011;15:343–347. doi: 10.1016/j.jbmt.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Clay CC, Lloyd LK, Walker JL, Sharp KR, Pankey RB. The metabolic cost of hatha yoga. J Strength Cond Res. 2005;19:604–610. doi: 10.1519/15144.1. [DOI] [PubMed] [Google Scholar]
- 32.Mcardle WD, Katch FI, Katch VL. Lippincott Williams and Wilkins. Philadelphia: 2000. Essentials of exercise physiology. [Google Scholar]
- 33.Cramer H, Lauche R, Haller H, Dobos G. A systematic review and meta-analysis of yoga for low back pain. Clin J Pain. 2013;29:450–460. doi: 10.1097/AJP.0b013e31825e1492. [DOI] [PubMed] [Google Scholar]
- 34.Cramer H, Lauche R, Langhorst J, Dobos G. Rheumatology. Vol. 52. (Oxford): 2013. Yoga for rheumatic diseases: a systematic review; pp. 2025–2030. [DOI] [PubMed] [Google Scholar]
- 35.Bryan S, Pinto Zipp G, Parasher R. The effects of yoga on psychosocial variables and exercise adherence: a randomized, controlled pilot study. Altern Ther Health Med. 2012;18:50–59. [PubMed] [Google Scholar]
- 36.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013;30:1068–1083. doi: 10.1002/da.22166. [DOI] [PubMed] [Google Scholar]
- 37.Chong CS, Tsunaka M, Tsang HW, Chan EP, Cheung WM. Effects of yoga on stress management in healthy adults: A systematic review. Altern Ther Health Med. 2011;17:32–38. [PubMed] [Google Scholar]
- 38.Klatte R, Pabst S, Beelmann A, Rosendahl JS. The efficacy of body-oriented yoga in mental disorders. Dtsch Arztebl Int. 2016;113:195–202. doi: 10.3238/arztebl.2016.0195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: a new view of „comfort food“. Proc Natl Acad Sci USA. 2003;100:11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vickers AJ, Altman DG. Analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–1124. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E1.World Health Organization Waist circumference and waist-hip ratio report of a WHO expert consultation. World Health Organization (WHO) Geneva: 2011. [Google Scholar]
- E2.Bosy-Westphal A, Later W, Hitze B, Sato T, Kossel E, Gluer CC, et al. Accuracy of bioelectrical impedance consumer devices for measurement of body composition in comparison to whole body magnetic resonance imaging and dual X-ray absorptiometry. Obes Facts. 2008;1:319–324. doi: 10.1159/000176061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E3.Westhoff TH, Straub-Hohenbleicher H, Schmidt S, Tolle M, Zidek W, van der Giet M. Convenience of ambulatory blood pressure monitoring: comparison of different devices. Blood Press Monit. 2005;10:239–242. doi: 10.1097/01.mbp.0000172711.82287.7f. [DOI] [PubMed] [Google Scholar]
- E4.Bundesministerium der Justiz und für Verbraucherschutz. Verordnung über die Anwendung der Guten Klinischen Praxis bei der Durchführung von klinischen Prüfungen mit Arzneimitteln zur Anwendung am Menschen (GCP-Verordnung - GCP-V) https://www.gesetze-im-internet.de/gcp-v/BJNR208100004.html. doi: 10.1007/s00103-004-0979-0. (last accessed on 2 May 2016). [DOI] [PubMed] [Google Scholar]