Abstract
Having children or not is one of the most important decisions that a person will make in his or her lifetime. The Reproductive Life Plan (RLP) is a protocol that aims to encourage both women and men to reflect on their reproductive intentions and to find strategies for successful family planning, for example to have the wanted number of children and to avoid unwanted pregnancies as well as ill-health that may threaten reproduction. The RLP was developed in an American context for promotion of reproductive health in a life cycle perspective. Few studies have systematically evaluated the effectiveness of using an RLP protocol in clinical practice. This article describes the application of using the RLP protocol in contraceptive counselling in Sweden.
Keywords: Counselling, preconception care, preconception health, reproduction, reproductive life plan
Introduction
The decision about if and/or when to have children is one of the most important that a person will make in his or her lifetime. Yet, many young adults do not talk with their health care providers or even their partners about their future goals for a family. The Reproductive Life Plan (RLP) is a protocol consisting of a set of questions to guide a conversation about if and when a person might want to become a parent. The RLP protocol was developed in the United States to support reproductive health with a life course perspective (1). The RLP may be used by health care providers and others to encourage both women and men to reflect on their reproductive intentions and then access the appropriate services to achieve those intentions. For some this may be the provision of an appropriate contraceptive method, while for others this may lead to the provision of counselling and care to optimize health before pregnancy to improve birth outcomes. Regardless of the person’s decision, it is essential that health care providers aim to support patient autonomy and intentions so that pregnancies are wanted, planned, and as healthy as possible.
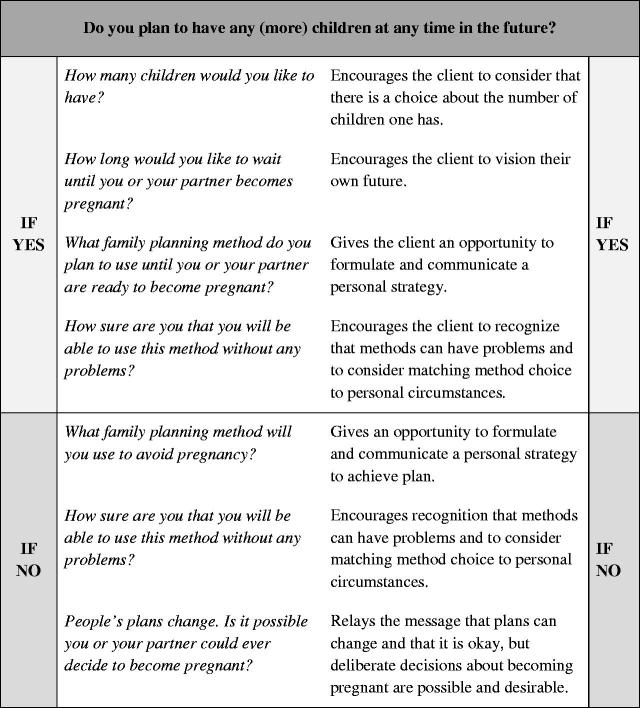
The Centers for Disease Control and Prevention (CDC) has recommended the RLP as a tool to improve preconception health and decrease unintended pregnancies and adverse pregnancy outcomes (2). The CDC offers recommendations for health care providers on how to have conversations about reproductive life planning with patients. Figure 1 describes key questions for this conversation. The CDC also has a RLP worksheet for women to guide their thoughts about their future goals (3). The RLP opens the door for other important conversations around preconception health and wellness. These conversations can happen in a clinic, but they can also happen in community settings or be done by self-assessment. As the concept of reproductive life planning has matured in the US, a number of organizations have developed tools for women and men (4–6) in addition to the national effort Show Your Love Today (7) and The One Key QuestionR Initiative (8).
Figure 1.
Reproductive life planning questions.
A study using reproductive life planning with low-income African-American and Hispanic women and men in publicly funded clinics in the US found this approach to be well acceptable among the target group (9). When tested by physicians at a family health centre in the US targeting women with diabetes, hypertension, and obesity, a RLP intervention was shown to increase women’s knowledge about reproductive health. The authors concluded that the RLP was a brief and cost-effective counselling tool for women with chronic diseases (10). A different study, however, found limited efficacy in using the RLP with urban women utilizing national family planning services in the US (11).
While the CDC and a growing number of partners recommend the use of RLP, more studies that systematically evaluate the effectiveness of using the RLP in clinical practice need to be conducted. This article describes the application of reproductive life planning in clinics in Sweden, highlighting the results and experience in implementing this concept outside the US context.
Sexual and reproductive health in Sweden
With almost 10 million inhabitants, Sweden is one of the world’s most family-friendly countries. The country offers extensive parental benefits. Parents receive 480 days of parental leave for one child, and for the first 390 days the compensation is 80% of the parent’s original income (12). Parents also receive child allowance from the state until the child is 18 years old. This child allowance (12,600 SEK/year ≈ US$1,555/year) is equal for all parents, regardless of income. Temporary parental benefits can be obtained if a parent needs to stay at home and take care of a sick child up to the age of 12 years. In spite of these benefits, the total fertility rate in Sweden is 1.9, which is lower than needed to maintain a steady population level. The mean age of first-time mothers has increased from 24 years to 29 years over the past four decades (13).
Delayed childbearing is even more pronounced among women with postgraduate education. Skoog Svanberg et al. (14) demonstrated that more than half of female postgraduate students did not want to have children during their studies, and as many as 66% wished to have their last child after the age of 35. In 2014, almost 3 out of 10 women attending antenatal care in Sweden were 35 years or older (13). The postponement of parenthood has been attributed to the following: (1) introduction of contraceptive technology, (2) increased educational levels and women’s labour force participation, (3) norm and value changes, (4) gender equity, (5) changing partnerships and increasing number of people living alone, and (6) housing and economic uncertainties (15).
It is well known that advanced maternal age is a risk factor for pregnancy complications such as chromosomal abnormality, preterm birth, being small for gestational age, stillbirth, neonatal death, gestational diabetes, and pre-eclampsia (16–23). These risks, however, do not appear to be common knowledge.
The median age for first intercourse among girls in Sweden is 16 years (24). This means that the majority of women are in need of effective contraceptives many years before most intend to begin childbearing. Repeated surveys among female university students show that this group of young women has sexual behaviours that may threaten their fertility. The mean number of sexual partners has increased for this population from 4 to 12 over the past 25 years. In 2014, one out of four women receiving contraceptive counselling had a sexually transmitted infection (25). As sexually transmitted infections can lead to infertility and other health problems, health care professionals in Sweden are recommended to discuss sexuality and sexual risk-taking with their patients as part of contraceptive counselling (26).
Contraceptive counselling in Sweden is free of charge, with midwives providing approximately 80%–90% of all of this service. Midwives can prescribe hormonal contraceptives as well as insert and remove intrauterine devices and implants for healthy women at antenatal/family planning clinics. They also provide care through youth clinics within the primary health care system. The Medical Product Agency in Sweden has issued recommendations for contraceptive counselling (26). The aim of these recommendations is to prevent unwanted pregnancies and preserve women’s fertility until a pregnancy is desired.
Integrating RLP into contraceptive counselling in Sweden
One opportunity for offering RLP is during contraceptive counselling. In this situation, providers have a golden opportunity to ask women about their intentions to have children or not and about their possibility of conceiving. We used the RLP in a randomized clinical trial (RCT) with female university students (27). We chose this group of young women since highly educated women and men tend to postpone having children until ages when their reproductive capacity has started to decrease. They are not sufficiently aware of the age-related decline in fecundity, and this can impact their plans for a future family (14,28,29).
The study took place in a university city in Sweden in the spring of 2012. Swedish-speaking female university students requesting contraceptive counselling at the student health centre were invited to participate. The women received both verbal and written information from the midwives before giving their written consent, and then all women completed a baseline questionnaire. The response rate was 88% (n = 299).
All participants received standardized contraceptive counselling including a medical history, measuring blood pressure and weight, and provision of contraceptives (26). Women allotted to the intervention group also received the RLP-based intervention. This intervention consisted of a semi-structured discussion aimed to encourage the woman to reflect on her RLP. An interview guide based on the RLP as described by Moos et al. and the CDC (1,2) and a fact sheet served as guidance for the midwife. The women also received a specially designed booklet with information about, for example, the fertile window, the use of folic acid, and the importance of a healthy lifestyle when planning a pregnancy. Telephone interviews were conducted with all participants two months after their clinic visit. At follow-up, women in the intervention group had better knowledge about reproduction compared to the control group, and they wished to have their last child earlier in life than at baseline. Nine out of 10 also considered it rather or very positive that the midwife initiated the RLP discussion, and an equal proportion had the opinion that midwives routinely should discuss RLP with their patients.
The positive results among female university students inspired us to explore how this intervention would work in everyday practice and in a larger context (30). We partnered with the senior consultant in the regional antenatal care and the co-ordinating midwife in one Swedish county. After an informational meeting about reproductive life planning, 53 of 68 midwives in 16 clinics agreed to participate. The midwives received a RLP guide and booklets. Three months later, the midwives received a questionnaire about their opinions and experiences (if any) of using RLP with their clients. We also invited them to participate in a focus group interview to explore their opinions and experiences further. We conducted five focus groups with a total of 22 midwives.
The questionnaire revealed that 68% of the midwives had used RLP. The most common reason for not having used RLP was not having received enough information. Nine out of 10 who had used RLP considered the very idea of RLP as rather/very good and had rather/very positive experiences of using it. Some midwives used the booklet during counselling as a starting-point for discussion, others just handed it out. The booklet was generally considered an asset for the midwife and as an accessible information source for the woman, particularly when time was restricted.
The findings from the focus group interviews resulted in four categories.
1. A predominantly positive experience
The RLP was experienced as a rewarding and easy way to broaden the counselling. The midwives experienced predominantly positive reactions from women but acknowledged that the counselling required tactfulness and professionalism.
2. The RLP—a health-promoting tool
The midwives considered the RLP to give additional value to the contraceptive counselling, by motivating health-promoting actions. They stressed that women need knowledge about fertility and that family planning counselling is a suitable opportunity for RLP discussions. However, it was also stated that the RLP cannot always be prioritized in clinical practice, and there was disagreement on whether it was suitable for all groups of clients.
3. Individual and societal factors influence the RLP counselling
The midwives believed many factors could influence the RLP counselling. First, they recognized that their own prejudices and their clientele influence which patients receive this service. Second, women’s varying individual knowledge, norms, and premises strongly influence the conditions for the discussion. Finally, influences by societal norms and the media were acknowledged to be an important factor. For example, women are expected to postpone parenthood, but still have children, and the media strongly influence the public awareness, for instance through very unbalanced reporting about older celebrity mothers.
4. Long-term implementation comprises opportunities, risks, and needs
The midwives expressed different opinions regarding whether making RLP mandatory and requiring documentation would facilitate or impede its use in practice. It was suggested that more in-depth preparation for all midwives through role-plays and group discussions would improve uptake and enhance provider receptivity. The midwives also suggested that there was potential for expanding RLP counselling to other arenas and health care professions.
Lessons learned
Efforts to integrate the RLP concept into contraceptive services offered valuable lessons that will be useful in replicating this work more widely in Sweden and informing care in other countries. First, firmly anchoring the concept of RLP among the managers is of utmost importance for implementing the RLP in routine clinical practice. Our studies were both supported and encouraged by the senior consultant and co-ordinating midwife.
Further, health care providers require education and training before they start using the RLP tools. As highlighted by the midwives, respectful, unbiased patient engagement requires tactfulness and professionalism. Women and men of reproductive age have different backgrounds and reasons for their individual reproductive life plans. The aim of counselling is to aid the client to formulate their plan and find strategies to reach them, not to pressure the clients to change their plan into what the midwife finds appropriate. This is critical for health professionals to understand and apply to their practice. For successful implementation, health care providers need education both to refresh their general knowledge about lifestyles and fertility and to improve and practise communication skills. Education and training should be based on scientific literature and best practice strategies.
Midwives liked the quality of the RLP materials and found them easy to use (30). Clients responded positively to the RLP materials and conversation as well (27). Our studies were restricted by a short follow-up period and a non-population-based group of participants. The women included in the RCT represented female university students, and the midwives were from one county only.
In Sweden three research projects on RLP are currently underway: (1) an RCT among a general population of women (n = 1,993) visiting 60 clinics for contraceptive counselling, (2) an RCT among men (n = 201) visiting two clinics for testing for sexually transmitted infection, and (3) a prospective study examining the long-term implementation of RLP in one county in Sweden. Further studies need to explore the long-term impact of RLP in a general population, which could be foundational for also examining the economic impact of this work. As e-health is a growing field of health care, it would also be interesting to compare different modes of delivery of the RLP, for example a mobile application or a web page. Finally, the RLP deserves to be explored for other target groups and by other health care providers, in different settings and countries.
Recommendations for implementation of RLP
The Swedish experience informs several key factors for implementing reproductive life planning conversations into routine contraceptive counselling and general preventive health care. Seven key factors that may facilitate or hinder improvement of health care in general, as for example moving RLP into practice, include: (1) the innovation or guideline itself, (2) health professionals, (3) clients/patients, (4) professional interactions, (5) incentives and resources, (6) capacity for organizational change, and (7) social, political, and legal factors (31).
In the exploratory study the RLP received rather positive comments on relevance, the quality of materials, and ease of use (30). This suggests that the RLP itself will help the implementation. Also the professionals (midwives) involved were often positive towards the RLP, though some reported their own prejudices on whom the RLP is relevant for and doubt on responsibilities as potential barriers.
Interprofessional and organizational issues that could help or hinder the RLP’s implementation were not assessed in the Swedish study; however, the relevance of resources and societal factors were clearly addressed by some of the midwives. They highlighted that the RLP fits in well with contraceptive counselling visits. They also expressed doubts about the integration with current electronical records. The midwives believed that the RLP tool had the potential to counteract social norms towards postponing parenthood.
The study among midwives (30) implies that the RLP tool and guidelines need little improvement, though perhaps the instructions should include assessing clients’ basic knowledge about fertility. Future implementation efforts should, however, address practical issues of time for using the RLP, integrated documentation of the RLP and other activities during consultations, and integrating this conversation into standard clinical care provision. Further, professionals’ beliefs need to be addressed to some extent to ensure an open mind towards providing RLP counselling to all visitors of reproductive ages, not just certain groups. This implies that change methods might have to be added to the midwives’ introduction into the RLP use in order to convince the midwives of the RLP’s relevance to larger groups; a degree of structural redesign at organizational level and agenda setting at health policy level is probably required to embed the RLP into regular care provision (32). Finally, it should be noted that further analyses of experiences with introducing the RLP are needed to take these first insights beyond the contexts of Swedish health care and use by midwives only. Further explorations of the RLP’s implementation should involve other professions, as well as organizational representatives, e.g. health care administrators and change management experts.
Disclosure statement
The authors report no conflicts of interest.
References
- 1.Moos MK, Dunlop AL, Jack BW, Nelson L, Coonrod DV, Long R, et al. . Healthier women, healthier reproductive outcomes: recommendations for the routine care of all women of reproductive age. Am J Obstet Gynecol. 2008;199:S280–S9. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Recommendations to improve preconception health and health care—United States: a report of the CDC/ATSDR Preconception Care Work Group and the Select Panel on Preconception Care. MMWR Recomm Rep. 2006;55:1–23. [PubMed] [Google Scholar]
- 3.CDC.gov [Internet]. Atlanta: Centers for Disease Control and Prevention. Available from: http://www.cdc.gov/preconception/reproductiveplan.html [updated 2014 Aug 27; cited 2016 Jun 16].
- 4.DEThrives.com [Internet]. Delaware: the Delaware Division of Public Health, the Delaware Healthy Mother and Infant Consortium and partner organizations. Available from: http://dethrives.com/mlmpw/overview [cited 2016 Jun 16].
- 5.Whb.ncpublichealth.com [Internet]. Raleigh: North Carolina Division of Public Health, Women’s and Children’s Health Section, Women’s Health Branch. Available from: http://whb.ncpublichealth.com/Manuals/AreYouReadySexAndYourFutureRevised-9-10-10.pdf [updated 2016 Jun 6; cited 2016 Jun 16].
- 6.Famplan.org [Internet]. Boston: Title X Family Planning Training Center. Available from: http://www.famplan.org/Resources/Docs/adult_rhp_busy_woman.pdf [cited 2016 Jun 16].
- 7.CDC.gov [Internet]. Atlanta: Centers for Disease Control and Prevention. Available from: http://www.cdc.gov/preconception/showyourlove/index.html [updated 2013 Feb 1; cited 2016 Jun 16].
- 8.Onekeyquestion.org [Internet]. Portland: the Oregon Foundation for Reproductive Health. Available from: http://www.onekeyquestion.org/[cited 2016 Jun 16].
- 9.Dunlop AL, Logue KM, Miranda MC, Narayan DA.. Integrating reproductive planning with primary health care: an exploration among low-income, minority women and men. Sex Reprod Healthc. 2010;1:37–43. [DOI] [PubMed] [Google Scholar]
- 10.Mittal P, Dandekar A, Hessler D.. Use of a modified reproductive life plan to improve awareness of preconception health in women with chronic disease. Perm J. 2014;18:28–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bommaraju A, Malat J, Mooney JL.. Reproductive life plan counseling and effective contraceptive use among urban women utilizing Title X services. Womens Health Issues. 2015:25;209–15. [DOI] [PubMed] [Google Scholar]
- 12.Forsakringskassan.se [Internet]. Stockholm: Försäkringskassan. Available from: https://www.forsakringskassan.se/privatpers/foralder/nar_barnet_ar_fott/foraldrapenning [cited 2016 Jun 16].
- 13.The National Board of Health and Welfare Official Statistics of Sweden. Pregnancies, deliveries and newborn infants: the Swedish Medical Birth Register 1973–2014. 2015. [Google Scholar]
- 14.Skoog Svanberg A, Lampic C, Karlström P-O, Tydén T.. Attitudes toward parenthood and awareness of fertility among postgraduate students in Sweden. Gend Med. 2006;3:187–95. [DOI] [PubMed] [Google Scholar]
- 15.Mills M, Rindfuss RR, McDonald P, te Velde E; ESHRE Reproduction and Society Task Force . Why do people postpone parenthood? Reasons and social policy incentives. Hum Reprod Update. 2011;17:848–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jacobsson B, Ladfors L, Milsom I.. Advanced maternal age and adverse perinatal outcome. Obetet Gynecol. 2004;104:727–33. [DOI] [PubMed] [Google Scholar]
- 17.Cleary-Goldman J, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, et al.; FASTER Consortium . Impact of maternal age on obstetric outcome. Obstet Gynecol. 2005;105:983–90. [DOI] [PubMed] [Google Scholar]
- 18.Luke B, Brown MB.. Elevated risks of pregnancy complications and adverse outcomes with increasing maternal age. Hum Reprod. 2007;22:1264–72. [DOI] [PubMed] [Google Scholar]
- 19.Jolly M, Sebire N, Harris J, Robinson S, Regan L.. The risks associated with pregnancy in women aged 35 years or older. Hum Reprod. 2000;15:2433–7. [DOI] [PubMed] [Google Scholar]
- 20.Hook EB, Cross PH, Schreinemachers DM.. Chromosomal abnormality rates at amniocentesis and in live-born infants. JAMA. 1983;249:2034–8. [PubMed] [Google Scholar]
- 21.Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M.. Maternal age and fetal loss: population based register linkage study. BMJ. 2000;320:1708–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fretts RC, Schmittdiel J, McLean FH, Usher RH, Goldman MB.. Increased maternal age and the risk of fetal death. N Engl J Med. 1995;333:953–7. [DOI] [PubMed] [Google Scholar]
- 23.Flenady V, Koopmans L, Middleton P, Froen JF, Smith GC, Gibbons K, et al. . Major risk factors for stillbirth in high-income countries: a systematic review and meta-analysis. Lancet. 2011;377:1331–40. [DOI] [PubMed] [Google Scholar]
- 24.Häggström-Nordin E, Borneskog C, Eriksson M, Tydén T.. Sexual behaviour and contraceptive use among Swedish high school students in two cities: comparisons between genders, study programmes, and over time. Eur J Contracept Reprod Health Care. 2011;16:36–46. [DOI] [PubMed] [Google Scholar]
- 25.Stenhammar C, Ehrsson YT, Åkerud H, Larsson M, Tydén T.. Sexual and contraceptive behavior among female university students in Sweden - repeated surveys over a 25-year period. Acta Obstet Gynecol Scand. 2015;34:253–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Medical Products Agency Antikonception—behandlingsrekommendation. Information från Läkemedelsverket. 2014;25:14–28 [in Swedish]. [Google Scholar]
- 27.Stern J, Larsson M, Kristiansson P, Tydén T.. Introducing reproductive life plan-based information in contraceptive counseling: an RCT. Hum Reprod. 2013;28:2450–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lampic C, Skoog Svanberg A, Karlström P, Tydén T.. Fertility awareness, intentions concerning childbearing, and attitudes towards parenthood among female and male academics. Hum Reprod. 2006;21:558–64. [DOI] [PubMed] [Google Scholar]
- 29.Eriksson C, Larsson M, Tydén T.. Reflections on having children in the future—interviews with highly educated women and men without children. Ups J Med Sci. 2012;117:328–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stern J, Bodin M, Grandahl M, Segeblad B, Axén L, Larsson M, et al. . Midwives' adoption of the reproductive life plan in contraceptive counselling: a mixed methods study. Hum Reprod. 2015;30:1146–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flottorp SA, Oxman AD, Krause J, Musila NR, Wensing M, Godycki-Cwirko M, et al. . A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci. 2013;3:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kok G, Gottlieb NH, Peters GY, Mullen PD, Parcel GS, Ruiter RA, et al. . A taxonomy of behaviour change methods: an Intervention Mapping approach. Health Psychol Rev. 2016;15:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]