Abstract
Baicalein (5,6,7-trihydroxy-2-phenyl-chromen-4-one) is a flavone, a type of flavonoid, originally isolated from the roots of Scutellaria baicalensis. This study evaluated the protective effects of baicalein against oxidative damage-mediated apoptosis induced by ultraviolet B (UVB) radiation in a human keratinocyte cell line (HaCaT). Baicalein absorbed light within the wavelength range of UVB. In addition, baicalein decreased the level of intracellular reactive oxygen species (ROS) in response to UVB radiation. Baicalein protected cells against UVB radiation-induced DNA breaks, 8-isoprostane generation and protein modification in HaCaT cells. Furthermore, baicalein suppressed the apoptotic cell death by UVB radiation. These findings suggest that baicalein protected HaCaT cells against UVB radiation-induced cell damage and apoptosis by absorbing UVB radiation and scavenging ROS.
Keywords: Baicalein, Ultraviolet B, Oxidative stress, Reactive oxygen species, HaCaT cells
INTRODUCTION
Reactive oxygen species (ROS) are naturally produced in the body as a result of normal metabolism or environmental exposure. At high concentrations, ROS may induce oxidative damage to DNA, lipids, and proteins. Oxidation of these cellular substrates can cause degenerative diseases (Dhumrongvaraporn and Chanvorachote, 2013; Lee et al., 2014). Ultraviolet B (UVB) radiation can generate ROS including singlet oxygen, superoxide anion, and hydroxyl radical. These ROS can oxidize and damage cellular lipids, proteins, and DNA, leading to changes and photo-aging in skin (Palmer and Kitchin, 2010; Sklar et al., 2013). UVB radiation also have deleterious effects on the skin, including carcinogenesis, inflammation, solar erythema, and premature aging (Sime and Reeve, 2004; Narayanan et al., 2010; Lee and Park, 2014).
Recently, natural compounds have attracted attention as antioxidant because many synthetic compounds have toxic side effects. They show antioxidant effects via free radical scavenging capacity and/or enhancing antioxidant system (Sen et al., 2010; Vera Saltos et al., 2015). Baicalein (5,6,7-trihydroxyflavone), a flavone compound, is originally isolated from the roots of Scutellaria baicalensis and the aglycone of baicalin. It is also reported in Oroxylum indicum, known as Indian trumpet flower. This flavonoid inhibits certain types of lipoxygenases and acts as an anti-inflammatory agent (Deschamps et al., 2006; Hsieh et al., 2007). It also has anti-proliferative effect on endothelin-1-induced proliferation of pulmonary artery smooth muscle cells via inhibition of transient receptor potential channel 1 expression (Lin et al., 2011). Our recent work showed that baicalein ameliorates mitochondrial oxidative stress via induction of manganese superoxide dismutase (Lee et al., 2011). Baicalein also protects cellular components against oxidative damage by scavenging ROS, inhibiting apoptosis and attenuates oxidative stress-induced expression of matrix metalloproteinase-1 by regulating the mitogen-activated protein kinase pathway in human keratinocytes (Kim et al., 2012a). In addition, baicalein reduces oxidative stress-induced DNA damage by upregulating the DNA repair system (Kim et al., 2012b). However, UVB-induced oxidative damage has not been researched. Therefore, this study investigated HaCaT cells to evaluate whether baicalein protects cells against UVB-induced oxidative stress.
MATERIALS AND METHODS
Reagents
Baicalein, N-acetyl cysteine (NAC), 1,1-diphenyl-2-picrylhydrazyl (DPPH), 2′,7′-dichlorodihydrofluorescein diacetate (DCF-DA), [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium] bromide (MTT), Hoechst 33342 and 5,5-dimethyl-1-pyrroline-N-oxide (DMPO) were obtained from Sigma-Aldrich (St. Louis, MO, USA). Diphenyl-1-pyrenylphosphine (DPPP) was purchased from Molecular Probes (Eugene, OR, USA). All other chemicals and reagents were of analytical grade.
Cell culture and UVB radiation
HaCaT cells were supplied by the Amore Pacific Company (Yongin, Republic of Korea) and maintained in an incubator at 37°C in a humidified atmosphere containing 5% CO2 plus 95% air. The cells were grown in RPMI 1640 medium containing 10% fetal bovine serum heated for 30 min at 56°C, streptomycin (100 μg/ml), and penicillin (100 units/ml). A CL-1000M UV Crosslinker (UVP, Upland, CA, USA) was used as the UVB source, which delivers a UVB energy spectrum of 280–320 nm, and UVB dose is 30 mJ/cm2.
Ultraviolet/visible absorption analysis
To observe the UVB absorption spectra of baicalein, which was diluted in DMSO (1:500), the compound was scanned by UV at 220–520 nm using Biochrom Libra S22 ultraviolet/visible spectrophotometer (Biochrom Ltd., Cambridge, UK).
Cell viability
Cells were seeded in a 24 well plate at a density of 5×104 cells/well. Sixteen hours after seeding, cells were treated with baicalein at a concentration of 5, 10, 20, 30 μM. In addition, 1 mM NAC or 20 μM baicalein was treated the cells, followed 1 h later by 30 mJ/cm2 of UVB radiation. After incubating for 24 h at 37°C, 10 μl of MTT stock solution (2 mg/ml) was added to each well to yield a total reaction volume of 500 μl and incubating cells for 4 h. Next, the plate was centrifuged at 1500 rpm for 5 min and the supernatants were aspirated. The formazan crystals in each well were dissolved in 500 μl dimethyl sulfoxide (DMSO), and the absorbance at 540 nm was measured by a scanning multi-well spectrophotometer.
DPPH radical scavenging activity
Baicalein (10, 20, 30 μM) and 1 mM NAC was added to a solution of 0.1 mM DPPH in methanol. The resulting reaction mixture was shaken vigorously. After 3 h, the amount of residual, unreacted DPPH was measured at 520 nm by using a spectrophotometer.
Detection of hydroxyl radical
Hydroxyl radical generated by the Fenton reaction (FeSO4+ H2O2) was reacted with DMPO. The resultant DMPO/•OH adduct was detected using an ESR spectrometer (Li et al., 2004). The ESR spectrum was recorded 2.5 min after a phosphate buffer solution (pH 7.4) was reacted with 20 μl each of 0.3 M DMPO, 10 mM FeSO4, 10 mM H2O2, and 20 μM baicalein. The ESR spectrometer parameters were set as follows: central magnetic field=336.8 mT; power=1.00 mW; frequency= 9.4380 GHz; modulation width=0.2 mT; amplitude=600; sweep width=10 mT; sweep time=0.5 min; gain=200, time constant=0.03 sec; temperature=25°C.
Detection of superoxide anion
Superoxide anion generated by the xanthine/xanthine oxidase system was reacted with DMPO, and the resultant DMPO/•OOH adduct was detected using an ESR spectrometer. ESR signaling was read 2.5 min after 20 μl of xanthine oxidase (0.25 U/ml) was mixed with 20 μl each of xanthine (10 mM), DMPO (3 M) and baicalein (20 μM). The ESR spectrometer parameters were set as follows: central magnetic field=336.8 mT; power=1.00 mW; frequency=9.4380 GHz; modulation width=0.2 mT; amplitude=600; sweep width=10 mT; sweep time=0.5 min; gain=500, time constant=0.03 sec; temperature=25°C.
Measurement of intracellular ROS
The DCF-DA method was used to measure the levels of intracellular ROS (Rosenkranz et al., 1992). Cells were seeded in a 96 well plate at 1×104 cells per well and at 16 h after plating, cells were treated with baicalein at the concentration of 5, 10, 20 and 30 μM for 1 h. 1 mM H2O2 or UVB radiation (30 mJ/cm2) was then treated to the medium, and cells were incubated for an additional 24 h at 37°C. After the addition of 25 μM DCF-DA for 10 min, the fluorescence of 2′,7′-dichlorofluorescein was detected using a LS-5B spectrofluorometer (Perkin-Elmer, Waltham, MA, USA). The scavenging effect of ROS generation (in percent) was calculated as [(fluorescence value of H2O2 or UVB-treated cells alone)−(fluorescence value of H2O2 or UVB-treated cells with baicalein treatment) / (fluorescence value of H2O2 or UVB-treated cells alone)]×100. For imaging analysis of the generation of intracellular ROS, cells were seeded on a four-well chamber slide at a density of 2×105 cells/ml. At 16 h after plating, cells were treated with baicalein at the concentration of 20 μM for 1 h. UVB (30 mJ/cm2) was exposed to the plate and cells were incubated for an additional 24 h at 37°C. And then, 100 μM of DCF-DA was added to each well, and the cells were incubated for an additional 30 min at 37°C. After washing with PBS, the stained cells were mounted on the chamber slide with mounting medium (DAKO, Carpinteria, CA, USA). The images were obtained on a confocal microscope using the Laser Scanning Microscope 5 PASCAL software (Carl Zeiss, Oberkochen, Germany).
Single-cell gel electrophoresis (Comet assay)
The degree of oxidative DNA damage was determined in a Comet assay (Rajagopalan et al., 2003). The cell suspension was mixed with 75 μl of 0.5% low-melting agarose (LMA) at 39°C and the mixture was spread on a fully frosted microscopic slide pre-coated with 200 μl of 1% normal melting agarose (NMA). After solidification of the agarose, the slide was covered with another 75 μl of 0.5% LMA and then immersed in a lysis solution (2.5 M NaCl, 100 mM Na-EDTA, 10 mM Tris, 1% Trion X-100, 10% DMSO and pH 10) for 1 h at 4°C. The slides were subsequently placed in a gel electrophoresis apparatus containing 300 mM NaOH and 10 mM Na-EDTA (pH 13) for 40 min to allow for DNA unwinding and the expression of alkali-labile damage. An electrical field was then applied (300 mA, 25 V) for 20 min at 4°C to draw the negatively charged DNA towards the anode. The slides were washed three times for 5 min at 4°C in a neutralizing buffer (0.4 M Tris, pH 7.5), stained with 80 μl of ethidium bromide (10 μg/ml) and observed under a fluorescence microscope and an image analyzer Komet 5.5 (Andor Technology, Belfast, UK). The percentage of the total fluorescence in the comet tails and the tail lengths of 50 cells per slide were recorded.
Lipid peroxidation assay
Lipid peroxidation was assayed by colorimetric detection of 8-isoprostane, a stable end-product of lipid peroxidation, in the conditioned medium of HaCaT cells (Beauchamp et al., 2002). A commercial enzyme immune assay (Cayman Chemical, Ann Arbor, MI, USA) was used according to the manufacturer’s instructions to detect 8-isoprostane level. In addition, lipid peroxidation was also estimated by use of diphenyl-1-pyrenylphosphine (DPPP), a fluorescent probe (Okimoto et al., 2000). Cells were treated with 20 μM baicalein for 1 h, followed by exposure to UVB (30 mJ/cm2). Five hours later, 5 mM DPPP was added and incubated for 30 min in the dark. The DPPP fluorescence images were analyzed by a Zeiss Axiovert 200 inverted microscope at an excitation wavelength of 351 nm and an emission wavelength of 380 nm.
Protein carbonyl formation
Cells were treated with 20 μM baicalein for 1 h, followed by the radiation of UVB (30 mJ/cm2) and further incubation for 36 h. The amount of protein carbonyl formation was determined by using an OxiselectTM protein carbonyl enzyme-linked immunosorbent assay (ELISA) kit (Cell Biolabs, San Diego, CA, USA) according to the manufacturer’s instructions.
Nuclear staining with Hoechst 33342
Cells were treated with baicalein at a concentration of 20 μM or 1 mM NAC and exposed to UVB radiation (30 mJ/cm2) into plate 1 h later. After additional 24 h incubation at 37°C, the DNA specific fluorescent dye Hoechst 33342 (1.5 μl of a 10 mg/ml stock) was added to each well and the cells were incubated for 10 min at 37°C. The stained cells were visualized under a fluorescence microscope equipped with a Cool SNAP-Pro color digital camera. The degree of nuclear condensation was evaluated and the apoptotic cells were quantified. The apoptotic index was calculated as follows: (number of apoptotic cells in baicalein-treated group/total number of cells in baicalein-treated group)/(number of apoptotic cells in control group/total number of cells in control group).
Statistical analysis
All measurements were performed in triplicate and all values are expressed as the mean ± standard error. The results were subjected to an analysis of variance (ANOVA) using Tukey’s test to analyze differences between means. In each case, a p-value<0.05 was considered statistically significant.
RESULTS
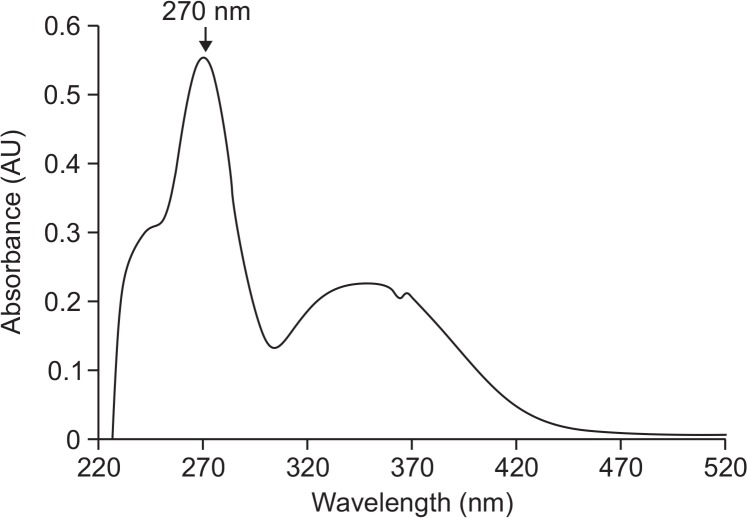
UVB absorption by baicalein
Absorption of UVB by baicalein was determined using an ultraviolet (UV)/visible spectrophotometer. Baicalein showed peak absorption at 270 nm, which is close to the range of UVB (280–320 nm) (Fig. 1). Therefore, light absorption by baicalein might be closely associated with its cytoprotective effect against UVB radiation.
Fig. 1.
Effect of baicalein on UVB absorption. UV/visible spectroscopy was conducted in the spectral range from 220 to 520 nm. The peak absorption is at 270 nm.
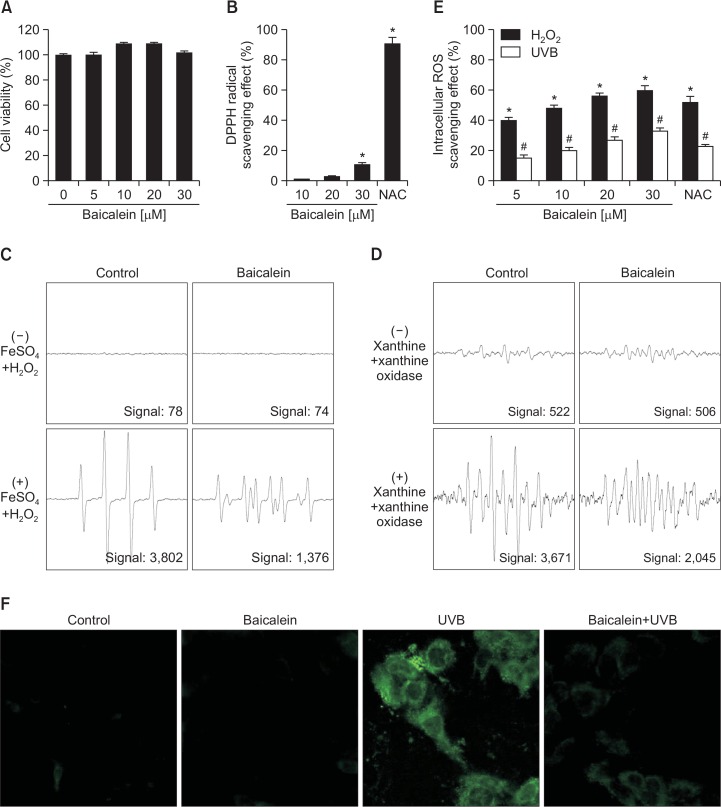
Baicalein reduces ROS generation
The MTT assay revealed that baicalein itself did not have cytotoxic effects on HaCaT cells at any concentrations used up to 30 μM (Fig. 2A). Baicalein scavenged the DPPH radical in a concentration-dependent manner; 1% of radicals were scavenged at 10 μM, 3% at 20 μM, and 11% at 30 μM. By comparison, the well-known ROS scavenger N-acetyl cysteine (NAC) scavenged 91% of radicals at a concentration of 1 mM (Fig. 2B). Moreover, we used electron spin resonance spectrometry to measure the ability of baicalein to scavenge hydroxyl radical and superoxide anion. In the FeSO4+H2O2 system (Fe2++H2O2→Fe3++•OH+OH−), DMPO/•OH adduct yielded signals of 3,802 in the absence of baicalein and 1,376 in the presence of 20 μM baicalein (Fig. 2C). Similarly, in the xanthine/xanthine oxidase system, DMPO/•OOH yielded signals of 3,671 in the absence of baicalein and 2,045 in the presence of 20 μM baicalein (Fig. 2D), indicating that baicalein can scavenge superoxide anion. Next, the intracellular ROS-scavenging activity of baicalein after H2O2 treatment or UVB radiation was determined using the DCF-DA assay (Fig. 2E). Fluorescence spectrometry data revealed that the intracellular ROS-scavenging activity of baicalein in H2O2-treated cells was 40% at 5 μM, 48% at 10 μM, 56% at 20 μM, and 60% at 30 μM, compared with 52% for 1 mM NAC, and in UVB-exposed cells was 12% at 5 μM, 14% at 10 μM, 19% at 20 μM, and 21% at 30 μM, compared with 18% for 1 mM NAC (Fig. 2E). Furthermore, confocal microscopy revealed that 20 μM baicalein ameliorated the increase in intensity (green color) caused by UVB radiation (Fig. 2F), indicating that baicalein treatment reduces ROS generation and that this compound possesses ROS-scavenging properties. Based on the results of these experiments, we chose to use the optimal dose of 20 μM baicalein for subsequent investigations.
Fig. 2.
Baicalein reduces ROS generation. (A) HaCaT cell viability was investigated using the MTT assay to determine the cytotoxic effects of baicalein. (B) The radical-scavenging effect of baicalein were investigated using the DPPH assay. (C) The ability to scavenge hydroxyl radical at 20 μM baicalein was estimated using the Fenton reaction (FeSO4+H2O2 system). (D) The ability to scavenge superoxide anion at 20 μM baicalein was evaluated using the xanthine/xanthine oxidase system. (E) Cells were treated with 5, 10, 20, or 30 μM baicalein or 1 mM NAC. One hour later, cells were irradiated with UVB or treated with 1 mM H2O2. After an additional 30 min, cells were stained with DCFDA and intracellular ROS were detected using a spectrophotometer. *,#Significantly different from control cells of H2O2 or UVB radiation, respectively (p<0.05). (F) Representative confocal images illustrate that UVB radiation increased the fluorescence intensity of DCF (produced by ROS) compared with the control, and baicalein treatment of UVB-exposed cells reduced the fluorescence intensity (green color).
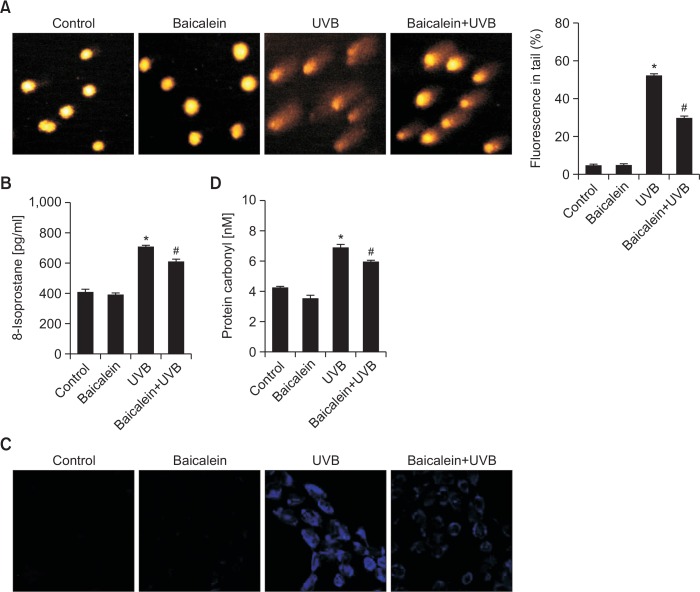
Baicalein protects DNA, lipids, and proteins against UVB-induced oxidative damage
We next investigated whether baicalein can inhibit damage to macromolecules in UVB-exposed cells. First, we monitored UVB-induced DNA damage using the Comet assay. The length of comet tails in microscopy images and the percentage of cellular fluorescence in tails are shown in Fig. 3A. After treatment of cells with UVB radiation, the comet tail length was distinctly elongated, as well as the ratio of damaged DNA outside of nuclei. Treatment of UVB-exposed cells with baicalein clearly reduces the percentage of damaged DNA in comet tails from 52% to 30%. Second, we examined the level of 8-isoprostane, a hallmark of lipid peroxidation, which is released by cells into the culture medium upon oxidative damage. Cells exposed to UVB secreted a higher level of 8-isoprostane than untreated cells; however, pretreatment of UVB-exposed cells with baicalein significantly reduced the 8-isoprostane level (Fig. 3B). In addition, lipid peroxidation was investigated by examining the fluorescent product DPPP oxide produced from DPPP. The intensity of DPPP oxide was higher in UVB-exposed cells than in control cells (blue color). Pretreatment of UVB-exposed cells with baicalein reduced the fluorescence intensity (Fig. 3C). Finally, we measured protein carbonylation, which is a reaction that occurs during the process of protein oxidation to form carbonyl group (Pirinccioglu et al., 2010). UVB irradiation obviously increased the level of carbonyl moieties, whereas pretreatment of UVB-exposed cells with baicalein notably suppressed the formation of protein carbonyl (Fig. 3D). Taken together, these results indicate that baicalein effectively protects DNA, lipids, and proteins against oxidative damage induced by UVB radiation.
Fig. 3.
Baicalein protects cells against UVB-induced DNA damage, lipid peroxidation, and protein carbonylation. (A) The Comet assay was performed to assess DNA damage. Representative images and percentage of cellular fluorescence within comet tails are shown. *Significantly different from control cells (p<0.05) and #significantly different from cells only exposed to UVB radiation (p<0.05). (B) Cells were treated with 20 μM baicalein. After 1 h, cells were exposed to UVB radiation. After incubation for a further 24 h, lipid peroxidation was determined using an 8-isoprostane enzyme immunoassay kit. *Significantly different from control cells (p<0.05) and #significantly different from cells only exposed to UVB radiation (p<0.05). (C) Lipid peroxidation was detected using a confocal microscope after DPPP staining. (D) Protein oxidation was assayed by measuring the amount of carbonyl formation. *Significantly different from control cells (p<0.05) and #significantly different from cells only exposed to UVB radiation (p<0.05).
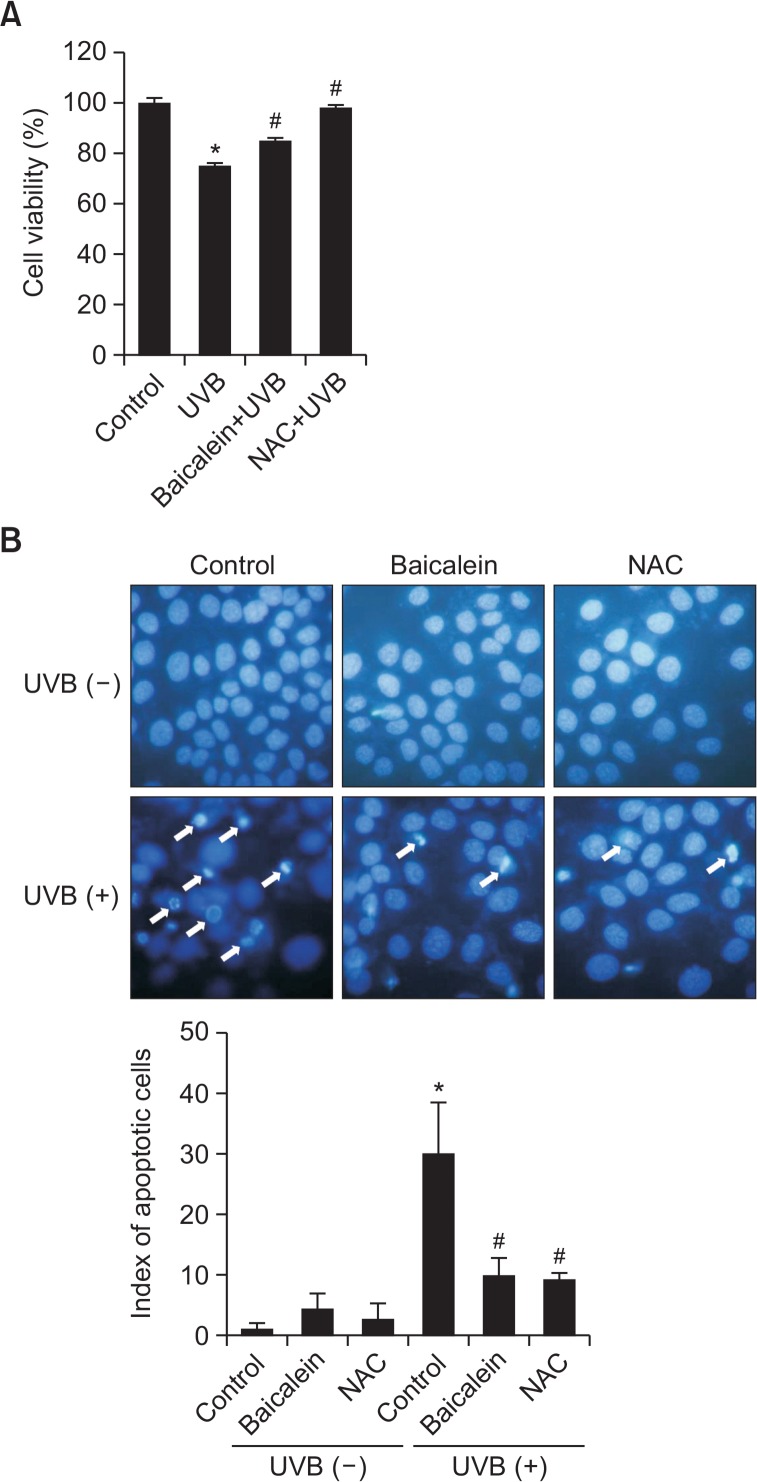
Baicalein suppresses apoptosis induced by UVB radiation
To elucidate the cytoprotective effect of baicalein against UVB-induced apoptosis, we examined the viability of HaCaT cells exposed to UVB, pretreated or not with 20 μM baicalein. The viability of UVB-exposed cells was reduced to 75% relative to control cells; however, pretreatment with baicalein increased viability to 85% compared to 95% of NAC (Fig. 4A). Nuclei were stained with Hoechst 33342, and then cells were assessed by microscopy. Normal nuclei were observed in control and baicalein-treated cells, whereas significant nuclear condensation was observed in UVB-exposed cells (apoptotic index=30). However, when these cells were pretreated with baicalein or NAC, nuclear fragmentation was reduced (baicalein, apoptotic index=9.8; NAC, apoptotic index=9.2) (Fig. 4B). These results indicate that baicalein protects cells against UVB-induced apoptosis.
Fig. 4.
Baicalein protects cells against apoptosis induced by UVB. (A) Cells were treated with 20 μM baicalein and exposed to UVB radiation 1 h later. After incubation for a further 24 h, cell viability was determined by the MTT assay and is expressed as a percentage of the control. 1 mM NAC was used as a positive control. *Significantly different from control cells (p<0.05) and #significantly different from cells only exposed to UVB radiation (p<0.05). (B) Cells were stained with Hoechst 33342 dye and observed by fluorescence microscopy. Apoptotic bodies were quantitated. 1 mM NAC was used as a positive control. *Significantly different from control cells (p<0.05) and #significantly different from cells only exposed to UVB radiation (p<0.05).
DISCUSSION
In the present study, we focused on the protective effects of baicalein against UVB radiation-induced oxidative stress. Our results indicated that baicalein absorbed UV photons, which was likely due to its polyphenolic constituents. Spectral data of natural phenols show a typical UV absorbance characteristic of benzene aromaticity at 270 nm. Baicalein is also natural phenol; therefore, its UV light absorbance (peak 270 nm) may be via benzene aromaticity (Jean-Denis et al., 2006).
UVB radiation induces ROS generation such as singlet oxygen, superoxide anion, hydroxyl radical and peroxy radical. In the present study, baicalein scavenged ROS such as superoxide anion and hydroxyl radical in cell free system, and intracellular ROS induced by treatment with H2O2 or UVB radiation. The distinct pathways by which flavonoid molecules (ArOH) transfer their charge provide several mechanisms of their antioxidant action. The representative one leads to the direct O-H bond breaking and proceeds by rapid donation of the proton and electron to a radical form (ArOH+HO•→ArO•+HOH), while the second one assumes indirect H atom abstraction (ArOH+HO•→ArOH++OH•→ArO•+HOH) (Marković et al., 2011). Baicalein has O-H bonds, and can scavenge radical by O-H bonds.
The UVB-induced ROS induce chemical modifications in DNA by the formation of purine/pyrimidine dimers and strand breaks leading to mutagenesis and loss of normal cellular metabolic functions. And they can damage lipids, producing lipid peroxides that are converted to products such as 8-isoprostane, malondialdehyde and conjugated dienes (Schneider et al., 2006; Petrova et al., 2011). Furthermore, UVB-induced oxidative stress damages proteins by site-specific modifications of amino acids, aggregation of cross-linked reaction products, increased susceptibility to proteolysis, fragmentation of peptide chains, and oxidation of specific amino acids (Rastogi and Madamwar, 2015). Therefore, UVB-induced oxidative stress triggers cell damage. However, baicalein protects cellular components such as DNA, lipids, and proteins against UVBinduced oxidative damage. The oxidative stress by UVB radiation mediates apoptosis via the release of mitochondrial cytochrome c into the cytosol and activation of apoptosis-related caspases (Pallela et al., 2010). However, baicalein protects cells against UVB-induced apoptotic cell death.
In conclusion, baicalein protects against UVB-induced oxidative stress via scavenging ROS, inhibiting apoptosis, and absorbing UV photons. In a future study, we will elucidate the mechanisms by which baicalein prevents ROS generation and inhibits apoptosis.
Acknowledgments
This work was supported by National Research Foundation of Korea (NRF) grant funded by Korea government (No. NRF-2015M2A2A7061657).
REFERENCES
- Beauchamp MC, Letendre E, Renier G. Macrophage lipoprotein lipase expression is increased in patients with heterozygous familial hypercholesterolemia. J Lipid Res. 2002;43:215–222. [PubMed] [Google Scholar]
- Deschamps JD, Kenyon VA, Holman TR. Baicalein is a potent in vitro inhibitor against both reticulocyte 15-human and platelet 12-human lipoxygenases. Bioorg Med Chem. 2006;14:4295–4301. doi: 10.1016/j.bmc.2006.01.057. [DOI] [PubMed] [Google Scholar]
- Dhumrongvaraporn A, Chanvorachote P. Kinetics of ultraviolet B irradiation-mediated reactive oxygen species generation in human keratinocytes. J Cosmet Sci. 2013;64:207–217. [PubMed] [Google Scholar]
- Hsieh CJ, Hall K, Ha T, Li C, Krishnaswamy G, Chi DS. Baicalein inhibits IL-1β- and TNF-α-induced inflammatory cytokine production from human mast cells via regulation of the NF-κB pathway. Clin. Mol. Allergy. 2007;5:5. doi: 10.1186/1476-7961-5-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean-Denis JB, Pezet R, Tabacchi R. Rapid analysis of stilbenes and derivatives from downy mildew-infected grapevine leaves by liquid chromatography-atmospheric pressure photoionisation mass spectrometry. J. Chromatogr. A. 2006;1112:263–268. doi: 10.1016/j.chroma.2006.01.060. [DOI] [PubMed] [Google Scholar]
- Kim KC, Kang SS, Lee J, Park D, Hyun JW. Baicalein attenuates oxidative stress-induced expression of matrix metalloproteinase-1 by regulating the ERK/JNK/AP-1 pathway in human keratinocytes. Biomol. Ther. (Seoul) 2012a;20:57–61. doi: 10.4062/biomolther.2012.20.1.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KC, Lee IK, Kang KA, Kim HS, Kang SS, Hyun JW. Baicalein (5,6,7-trihydroxyflavone) reduces oxidative stress-induced DNA damage by upregulating the DNA repair system. Cell Biol Toxicol. 2012b;28:421–433. doi: 10.1007/s10565-012-9233-y. [DOI] [PubMed] [Google Scholar]
- Lee IK, Kang KA, Zhang R, Kim BJ, Kang SS, Hyun JW. Mitochondria protection of baicalein against oxidative damage via induction of manganese superoxide dismutase. Environ Toxicol Pharmacol. 2011;31:233–241. doi: 10.1016/j.etap.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Lee KO, Kim SN, Kim YC. Anti-wrinkle effects of water extracts of teas in hairless mouse. Toxicol Res. 2014;30:283–289. doi: 10.5487/TR.2014.30.4.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee SJ, Park JW. Enhancement of UVB radiation-mediated apoptosis by knockdown of cytosolic NADP+-dependent isocitrate dehydrogenase in HaCaT cells. BMB Rep. 2014;47:209–214. doi: 10.5483/BMBRep.2014.47.4.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin YL, Lin RJ, Shen KP, Dai ZK, Chen IJ, Wu JR, Wu BN. Baicalein, isolated from Scutellaria baicalensis, protects against endothelin-1-induced pulmonary artery smooth muscle cell proliferation via inhibition of TRPC1 channel expression. J Ethnopharmacol. 2011;138:373–381. doi: 10.1016/j.jep.2011.09.014. [DOI] [PubMed] [Google Scholar]
- Li L, Abe Y, Kanagawa K, Usui N, Imai K, Mashino T, Mochizuki M, Miyata N. Distinguishing the 5,5-dimethyl-1-pyrroline N-oxide (DMPO)-OH radical quenching effect from the hydroxyl radical scavenging effect in the ESR spin-trapping method. Anal. Chim. Acta. 2004;512:121–124. doi: 10.1016/j.aca.2004.02.020. [DOI] [Google Scholar]
- Marković JMD, Marković ZS, Brdarić TP, Pavelkić VM, Jadranin MB. Iron complexes of dietary flavonoids: Combined spectroscopic and mechanistic study of their free radical scavenging activity. Food Chem. 2011;129:1567–1577. doi: 10.1016/j.foodchem.2011.06.008. [DOI] [Google Scholar]
- Narayanan DL, Saladi RN, Fox JL. Ultraviolet radiation and skin cancer. Int J Dermatol. 2010;49:978–986. doi: 10.1111/j.1365-4632.2010.04474.x. [DOI] [PubMed] [Google Scholar]
- Okimoto Y, Watanabe A, Niki E, Yamashita T, Noguchi N. A novel fluorescent probe diphenyl-1-pyrenylphosphine to follow lipid peroxidation in cell membranes. FEBS Lett. 2000;474:137–140. doi: 10.1016/S0014-5793(00)01587-8. [DOI] [PubMed] [Google Scholar]
- Pallela R, Na-Young Y, Kim SK. Anti-photoaging and photoprotective compounds derived from marine organisms. Mar. Drugs. 2010;8:1189–1202. doi: 10.3390/md8041189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer DM, Kitchin JS. Oxidative damage, skin aging, antioxidants and a novel antioxidant rating system. J Drugs Dermatol. 2010;9:11–15. [PubMed] [Google Scholar]
- Petrova A, Davids LM, Rautenbach F, Marnewick JL. Photoprotection by honeybush extracts, hesperidin and mangiferin against UVB-induced skin damage in SKH-1 mice. J Photochem Photobiol B, Biol. 2011;103:126–139. doi: 10.1016/j.jphotobiol.2011.02.020. [DOI] [PubMed] [Google Scholar]
- Pirinccioglu AG, Gökalp D, Pirinccioglu M, Kizil G, Kizil M. Malondialdehyde (MDA) and protein carbonyl (PCO) levels as biomarkers of oxidative stress in subjects with familial hypercholesterolemia. Clin Biochem. 2010;43:1220–1224. doi: 10.1016/j.clinbiochem.2010.07.022. [DOI] [PubMed] [Google Scholar]
- Rajagopalan R, Ranjan S, Nair CK. Effect of vinblastine sulfate on gamma-radiation-induced DNA single-strand breaks in murine tissues. Mutat Res. 2003;536:15–25. doi: 10.1016/S1383-5718(03)00015-9. [DOI] [PubMed] [Google Scholar]
- Rastogi PR, Madamwar D. UV-Induced Oxidative Stress in Cyanobacteria: How life is able to survive? Biochem Anal Biochem. 2015;4:173. doi: 10.4172/2161-1009.1000173. [DOI] [Google Scholar]
- Rosenkranz AR, Schmaldienst S, Stuhlmeier KM, Chen W, Knapp W, Zlabinger GJ. A microplate assay for the detection of oxidative products using 2′,7′-dichlorofluorescin-diacetate. J. Immunol. Methods. 1992;156:39–45. doi: 10.1016/0022-1759(92)90008-H. [DOI] [PubMed] [Google Scholar]
- Schneider LA, Bloch W, Kopp K, Hainzl A, Rettberg P, Wlaschek M, Horneck G, Scharffetter-Kochanek K. 8-Isoprostane is a dose-related biomarker for photo-oxidative ultraviolet (UV) B damage in vivo: a pilot study with personal UV dosimetry. Br J Dermatol. 2006;154:1147–1154. doi: 10.1111/j.1365-2133.2006.07192.x. [DOI] [PubMed] [Google Scholar]
- Sen S, Chakraborty R, Sridhar C, Reddy YSR, De B. Free radicals, antioxidants, diseases and phytomedicines: current status and future prospect. Int J Pharm Sci Rev Res. 2010;3:91–100. [Google Scholar]
- Sime S, Reeve VE. Protection from inflammation, immunosuppression and carcinogenesis induced by UV radiation in mice by topical Pycnogenol®. Photochem Photobiol. 2004;79:193–198. doi: 10.1562/0031-8655(2004)079<0193:PFIIAC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54–64. doi: 10.1039/C2PP25152C. [DOI] [PubMed] [Google Scholar]
- Vera Saltos MB, Naranjo Puente BF, Milella L, De Tommasi N, Dal Piaz F, Braca A. Antioxidant and free radical scavenging activity of phenolics from Bidens humilis. Planta Med. 2015;81:1056–1064. doi: 10.1055/s-0035-1545928. [DOI] [PubMed] [Google Scholar]