Abstract
Drug-eluting stents are an effective therapy for symptomatic arterial obstructions, substantially reducing the incidence of restenosis by suppressing the migration and proliferation of vascular smooth muscle cells into the intima. However, current drug-eluting stents also inhibit the growth of endothelial cells, which are required to cover the vascular stent to reduce an excessive inflammatory response. As a result, the endothelial lining of the lumen is not regenerated. Since the loss of this homeostatic monolayer increases the risk of thrombosis, patients with drug-eluting stents require long-term antithrombotic therapy. Thus, there is a need for improved devices with enhanced effectiveness and physiological compatibility towards endothelial cells. Current developments in nanomaterials may enhance the function of commercially available vascular devices. In particular, modified design schemes might incorporate nanopatterns or nanoparticle-eluting features that reduce restenosis and enhance re-endothelialization. The intent of this review is to discuss emerging nanotechnologies that will improve the performance of vascular stents.
Keywords: nanotechnology, nanopatterning, nanoparticle-eluting stents, drug-eluting stents, bare-metal stents
Introduction
Balloon angioplasty can be a useful procedure for patients with symptomatic arterial obstructive disease. However, during the procedure, the endothelial lining of the treated segment is denuded, the atherosclerotic plaque is usually ruptured, and the underlying vascular smooth muscle is dissected. The result is a highly thrombogenic surface that could lead to rapid clot formation and reocclusion of the vessel. Accordingly, patients are treated with antithrombotic drugs during and for variable periods of time after the procedure. Elastic recoil that occurs immediately after the procedure can reduce procedural success. The placement of a bare metal stent during angioplasty obviates elastic recoil and improves immediate procedural success. However, both balloon angioplasty and bare metal stent implantation are complicated within months by restenosis.
As discussed elsewhere in this issue, restenosis is a response to vascular injury characterized by the recruitment of vascular smooth muscle cells (and/or mesenchymal stem cells) to the injured region. These cells proliferate and generate a substantial extracellular matrix that, over a period of a few months, causes restenosis of the vessel. This is a very different process than atherosclerosis. Restenosis occurs more rapidly, and the pathobiology involves more vascular smooth muscle and mesenchymal cell proliferation and generation of an extracellular matrix, with less lipid deposition. Although restenosis is reduced by the placement of a stent after angioplasty,1,2 in-stent restenosis occurs as vascular cells migrate between the stent struts and proliferate in the intimal space.
Mechanical treatments for in-stent restenosis are often suboptimal. These may include implantation of a replacement stent, some form of catheter-directed atherectomy, or surgical bypass.3 Drug-eluting stents designed to reduce in-stent restenosis have some deficiencies that are discussed below. Accordingly, stents with modified surface properties—including biologically inspired nanoscale alterations—are under development.
Drug-Eluting Stents
The current clinically approved drug-eluting stents release drugs locally that suppress vascular smooth muscle cell proliferation. These stents have the added advantage of suppressing the autocrine and paracrine mechanisms responsible for excessive generation of extracellular matrix proteins.4 However, all currently available drug-eluting stents also suppress local regeneration of the natural endothelium. Consequently, the endothelial monolayer may not completely regenerate across the surface of the stent, leading to the loss of a key homeostatic feature that regulates interactions of the vessel wall with the circulating blood elements.5 For this reason, stent-related thrombosis has emerged as a life-threatening side effect of the drug-eluting stent, primarily among patients who have suspended any adjunctive antiplatelet or anticoagulant therapy.6–12 Stent thrombosis may result in myocardial infarction or death in up to 45% of cases.10 Accordingly, alternative agents for elution from the stent that have a more favorable profile (e.g., that suppress vascular smooth muscle proliferation while enhancing endothelial regeneration) are under investigation. Paradigmatic of such agents are nitric oxide donors, which enhance endothelial regeneration while suppressing vascular smooth muscle proliferation.13
Biocompatible Stent Coatings
Introduction
Stent surface structures may be enhanced by the application of a hemocompatible coating to a base material having some fixed geometric configuration. Distinct performance profiles have been associated with a range of nano- and macroscale stent coatings recognized categorically as drug-delivery-enhancing, inorganic, biocompatible, polymer, or polymer-free.14 Typically, the biocompatibility constraint is applicable to drug-eluting stents as well as stents having variable constitutional and functional properties. The concept of utilizing stent coatings was initially introduced as a means for trapping ions released from the metal structure and keeping them from entering the body. Since the inorganic materials used for these applications have demonstrated minimal drug-importing potential, nonbiodegradable polymeric coatings, such as polyhydroxyalkanoates (PHA) or polyurethane, have been developed to transport and locally release agents from the stent.15,16 Although PHA-coated stents have a tendency to reduce intimal thickness relative to bare metal stents, hemodynamic shear stresses have contributed to degradation of the polymer stent surface structure, in turn leading to stent thrombosis.17
Alternatively, biodegradable polymeric stents, while prone to induce inflammation, are currently used in various phases of developmental and market research. Novel solutions are being tested using stents with polymer-free macro- and nanofeatures that provide a nonthrombogenic surface to suppress in-stent restenosis and promote re-endothelialization.18 The promise of such nanofeatures resides in their ability to mimic the natural nanofeatures of vascular tissue itself.
Microporous and Microstructured Surfaces
The optimal stent is engineered to be highly deliverable; to inhibit vascular smooth muscle proliferation and generation of extracellular matrix proteins; and to enhance endothelial attachment, proliferation, and restoration of a healthy endothelial surface. The stent must be composed of metals or polymers that satisfy biocompatibility constraints and express adequate mechanical flexibility, strength, and dilatability. Stainless steel, titanium, cobalt-chromium alloys, and titanium-nickel alloys have been used as principal structural elements.19–21 Bare-metal stents fabricated from a titanium-nickel alloy (e.g., Nitinol) are preferred due to their excellent biocompatibility and structural versatility.19 Figure 1 shows scanning electron microscopy (SEM) images of micro- and submicro-structured Nitinol surfaces.22 Nevertheless, in-stent restenosis is often attributed to bare-metal stents having micron particle sizes that encourage neointimal tissue formation.23–25 Additionally, the release of metal ions from the stent might increase local inflammation.
Figure 1.
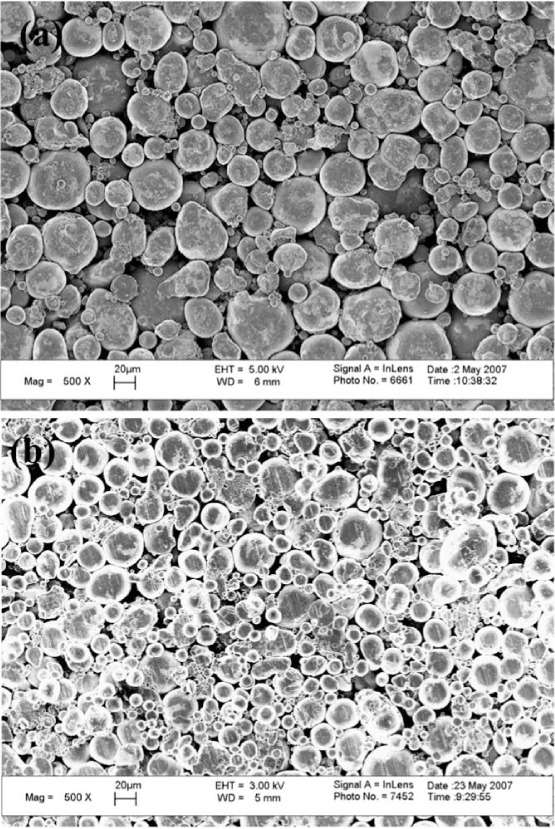
Scanning electron microscopy images of nickel-titanium alloy (NiTi) surfaces. (a) Microstructured NiTi, Mag 500x, bar = 20 μm. (b) Submicro-structured Nitinol, Mag 500x, bar = 20 μm22
Polymer-free microporous, microstructured, and slotted tubular stents are a class of devices with surface features designed to optimize stent applicability. Such stents can be spray coated with selected drugs that are absorbed onto surface micropores26,27 to allow homogeneous drug transfer.28 An alternative polymer-free technology comprises selective microstructuring of the abluminal surface of the stainless steel stent through controlled microabrasion processes.29 This textured surface enables coating with cytostatic drugs that can effectively suppress excessive neointimal tissue formation.30
Slotted Tubular Surfaces
Alternatively, the abluminal stent surface may be fabricated with micro- or nanoscale tubular slots designed to elute controlled quantities of antiproliferative agents. A layered carbon coating enhances hemocompatibility of the drug reservoir.29 Polymer-free stents may also be composed of slotted chromium-cobalt alloy, loaded with antiproliferative drug, and coated with a carbon-based surface intended to reduce thrombogenicity.31
Nanoporous and Nanostructured Surfaces
Recent advances in nanotechnology have enabled researchers to study polymer-free nanoporous, nanostructured, and nanoparticle-eluting stents. These nanofabrications may improve upon the polymer-free macrosystem surface modifications discussed above. One of the earliest attempts at commercializing a stent coated with a nanoporous substance was based on a nanothin-microporous stainless steel platform coated with a 0.3- to 1-μm layer of nanoporous hydroxyapatite and loaded with sirolimus.32,33
A nanoporous aluminum oxide coating has been explored in numerous research studies as an alternative to hydroxyapatite, and both have been demonstrated to improve endothelialization. In such studies, a nanothin layer of aluminum is glazed on a stainless steel base, and the composite structure is anodized to generate porous aluminum oxide. However, preclinical studies have shown variability regarding the effectiveness of stents coated with nanoporous materials.34,35 Although biocompatibility has been documented, nanoparticle debris ejected from the stent surface has been observed. This debris could provoke inflammation and subsequent restenosis. Therefore, in spite of their large surface-area exposure (especially to enhance endothelialization) and high drug-loading capacity, stents coated with nanoporous materials must be refined before becoming viable devices.
A related nanotechnology approach uses controlled nanopatterning of stent surfaces as a means for promoting endothelial regeneration. Topographical modifications generated through a standardized patterning process have demonstrated favorable interactions between the surface and cells.14 Therefore, re-endothelialization may be enhanced by incorporating specialized nanopatterns onto polymer-free stent surface structures. Additional research studies have concluded that the submicron patterning of titanium surfaces with crevices having a lateral magnitude of > 100 nm is especially efficient at stimulating endothelial cell adhesion.36 An example of the benefit of nanopatterning bare-metal stents (titanium) with aligned features is shown in Figure 2. Increased coverage of a bare-metal stent through nanotexturing could reduce an aggressive inflammatory response that would ordinarily result from exposure to bare metal.
Figure 2.
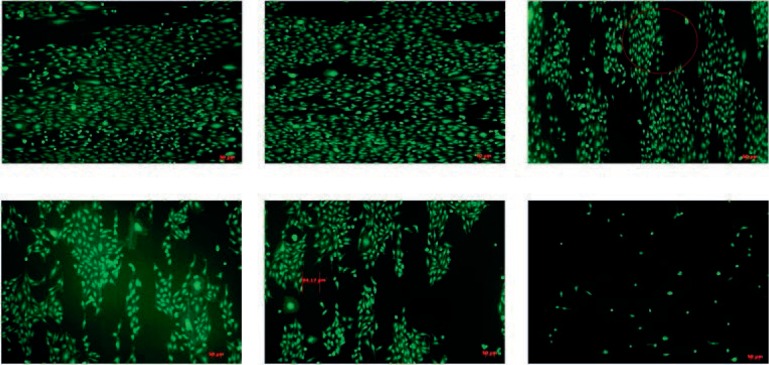
Increased endothelialization of nanostructured titanium vascular stents.
As an alternative to patterning stent surfaces with superficial nanofeatures, nanoparticles may be electrophoretically loaded onto bare-metal stents.37 The concept of a nanoparticle-eluting stent is especially useful for systems requiring dynamic drug delivery vehicles. Nakano et al. investigated the viability of nanoparticle-eluting stents having a biodegradable polymer coating.37 Their in vitro and in vivo results indicated excellent internalization of drug nanoparticles into smooth muscle cells as well as homogenous nanoparticle distribution in the region of implantation. Related research has investigated the loading of endothelial cells with poly(lactic acid)-modified magnetic nanoparticles and administering these modified cells to enhance endothelialization of stainless steel stents.38 However, the biological effect of such particles on endothelial functions will need to be carefully characterized.
Another possible approach is to coat the stent with nanopatterned extracellular matrix proteins. Endothelial cells are responsive to nanofeatures in a collagen matrix.39–41 For example, a collagen matrix composed of an array of longitudinally oriented fibers with diameters in the range of 30 nm can induce endothelial cells to align longitudinally. These aligned endothelial cells resemble the endothelial monolayer in a vessel segment exposed to laminar shear stress in that they have a greater length-to-width ratio compared to endothelial cells cultured in the absence of flow, which have a more “cobblestone paving” appearance. The aligned endothelial cells are biologically different in that they generate more nitric oxide and express less cell-adhesion molecules. These biological attributes would be favorable for a vascular conduit since such an endothelial monolayer would resist inflammation and thrombosis. Of note, endothelial cells aligned on the nanopatterned collagen resist the effects of shear in an orthogonal direction and remain aligned in the direction of the nanofibers. This is scientifically interesting and of potential clinical relevance, as such aligned endothelial cells might then be able to resist the adverse effects of disturbed or turbulent flow in a bypass graft or stent.
Titanium as a Nanopatterned Material
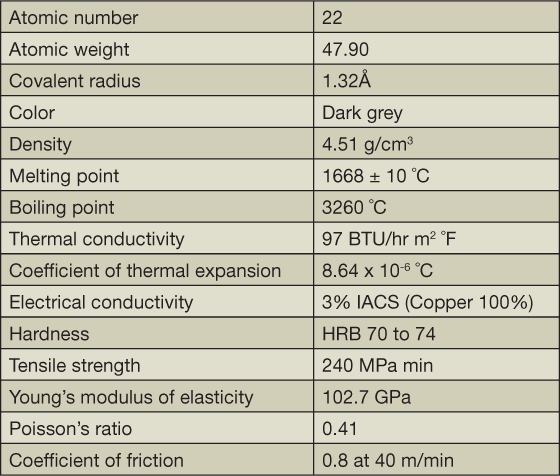
Titanium and titanium alloys are materials that are well-suited to several nano- or macroscale modifications. The physical properties of titanium are listed in Table 1. In addition to expressing great physiological compatibility, titanium light metal structures have adaptable mechanical properties that can be adjusted to suit the anatomical or other constraints associated with a stenting system.42 This is a direct consequence of the alpha and beta crystalline phases through which titanium and its alloys can transition. Strength and hardness are common features associated with unalloyed or alpha titanium alloys. Mechanical testing among classes of beta alloys has indicated a stronger design and increased ductility relative to the two alternate types. Titanium has the added capacity of microstructural morphological distortion through mechanical processing or heat treatment. In particular, the surface roughness and feature sizes of titanium-based stenting materials should be regulated for adequate procedural suitability.
Table 1.
Physical properties of titanium.22
Techniques for Substrate Modification of Titanium Stents
Physical deposition approaches and photolithography have been implemented to construct empirically useful nanoconfigurations. Among the most commonly employed micro- and nanofabrication techniques, photolithography enables the generation of grooves, pores, ridges, needles, or other protruding aspects along the surface.43,44 The process is facilitated by a photochemical reaction in which a substrate, having a thin polymeric photoresist, is exposed to light through an opaque patterned mask. A substrate expressing the desired structural motif emerges upon exposure of the body to a developer solution (Figure 3). Tissue regeneration can be enhanced and controlled by microgrooved titanium-coated surfaces.45
Figure 3.
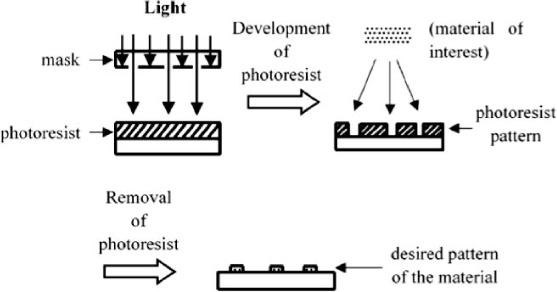
Schematic of micro/nanopatterning by photolithography.44
Micropatterned poly(dimethylsiloxane) (PDMS) is an especially suitable material for generating surface structures on stents so as to study their effects on the growth of smooth muscle and endothelial cell co-cultures.46,47 Microcontact printing is an alternate micro/nano fabrication procedure that uses an initial photolithography process in which silicon wafers are treated to produce a patterned PDMS stamp.44 The PDMS stamp is then coated by functionalized or chemically conjugated alkanethiol monolayers that assist in the patterning of cells and associated proteins before being transferred onto the stent or other substrate surface.44Figure 4 is a depiction of the microcontact printing procedure.
Figure 4.
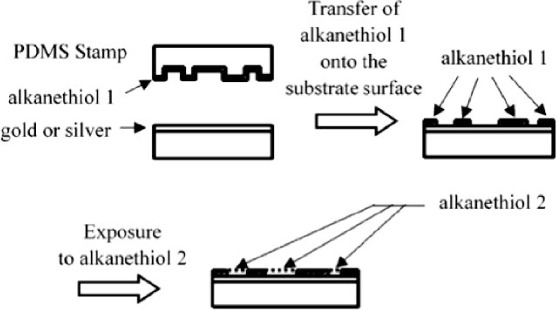
Schematic of micro/nanopatterning by microcontact printing.44
Among the physical vapor deposition (PVD) methods, electron beam evaporation is one of the most efficient systems. The PVD of titanium-nitride-oxide alloys onto stainless steel stents results in substrates that may be less prone to platelet adhesion and fibrinogen adsorption.48
Absorbable Stents
Metallic stents permanently alter the biophysical properties of the vessel wall.49,50 There is a localized increase in vascular stiffness and a loss of vasomotor regulation of luminal dimension. Furthermore, the metal stent is a foreign body that induces inflammation and cellular proliferation, and in the rare cases in which a stent becomes infected, antibiotic therapy is typically insufficient without removal of the stent.
In recent years, scientists have been investigating the feasibility of a drug-eluting absorbable stent that would promote long-term positive remodeling within the vasculature and restoration of its biophysical and physiological properties.49,51,52 Several mechanical properties and degradation times can be associated with a range of absorbable stents made of polymers or metals. One approach is to integrate biocompatible polymers such as poly(lactide-co-glycolide), poly-DL-lactide (PDLLA), or poly-L-lactide into absorbable stents.53–55 Their excellent shape-memory and self-expanding capabilities could facilitate stent placement. Balloon-expandable fiber-based stents also have been developed as absorbable stents.56–59 Imaging studies of a PDLLA-based absorbable balloon-expandable stent have indicated efficient integration into the arterial wall.60–63
Corrodible metals such as iron and magnesium have also been explored as potential constituents of absorbable stents. Preclinical studies have confirmed negligible toxicity and excellent biocompatibility.63,64 However, clinical trials of a magnesium-based absorbable stent have suggested a rehospitalization rate of 45% among patients receiving the stents.65–67 Even so, absorbable stent research is steadily developing in an effort to correct structural deficiencies and enhance absorption rates. This has especially important implications for children suffering from congenital cardiovascular diseases since absorbable stents would facilitate continued arterial growth in pediatric patients.68
Conclusions
Physicochemical properties of stents, surface coatings, and micro- and nanopatterning may be manipulated to enhance drug delivery, reduce restenosis, and improve re-endothelialization. A variety of strategies are under development. In particular, micro- and nanopatterning of the surface of bare-metal or drug-eluting stents may improve the results of cardiovascular interventions. Titanium may be particularly suited to nanofabrication processes, including photolithography and electron beam deposition. An ideal stent would prevent elastic recoil, resist thrombosis, suppress vascular smooth muscle proliferation and generation of extracellular matrix, and enhance re-endothelialization with minimal use of systemic antiplatelet and antithrombotic drugs. Nanofeatures may improve drug delivery and/or have favorable biological effects to maintain lumen patency.
Key Points
The growth of nanotechnology has engendered novel stent designs.
Stent surface structures may be enhanced by the application of micro- or nanopatterned coatings or surface modifications that improve drug delivery and/or have direct biological effects.
A variety of novel strategies to enhance stent effectiveness include polymer-free, micro- or nanoporous, micro- or nanostructured, and/or nanoparticle-eluting stents.
Titanium and titanium alloys may be more receptive to several nano- or macroscale modifications.
Footnotes
Conflict of Interest Disclosure: This research was funded by Northeastern University and the George J. and Angelina P. Kostas Charitable Foundation. It also was supported in part by grants to Dr. Cooke from the National Institutes of Health (U01 HL100397) and the Cancer Prevention and Research Institute (RP150611).
References
- 1. Fischman D, Leon M, Baim D, . et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994. August 25; 331( 8): 496– 501. [DOI] [PubMed] [Google Scholar]
- 2. Serruys PW, de Jaegere P, Kiemeneij F, . et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994. August 25; 331( 8): 489– 95. [DOI] [PubMed] [Google Scholar]
- 3. Nageh T, Meier B. Treatment of in-stent restenosis. Int J Cardiol. 2005. October 10; 104( 3): 245– 50. [DOI] [PubMed] [Google Scholar]
- 4. Serruys P, Gershlick A. Handbook of drug-eluting stents. London, England: Taylor & Francis Ltd; 2005. 356 p. [Google Scholar]
- 5. Cooke JP. Flow, NO, and atherogenesis. Proc Natl Acad Sci U S A. 2003. February 4; 100( 3): 768– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McFadden EP, Stabile E, Regar E, Cheneau E, . et al. Late thrombosis in drug-eluting coronary stents after discontinuation of anti-platelet therapy. Lancet. 2004. October 23–29; 364( 9444): 1519– 21. [DOI] [PubMed] [Google Scholar]
- 7. Virmani R, Guagliumi G, Farb A, . et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004. February 17; 109( 6): 701– 5. [DOI] [PubMed] [Google Scholar]
- 8. Joner M, Finn A, Farb A, . et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol. 2006. July 4; 48( 1): 193– 202. [DOI] [PubMed] [Google Scholar]
- 9. Ong AT, McFadden EP, Regar E, de Jaegere PP, van Domburg RT, Serruys PW.. Late angiographic stent thrombosis (LAST) events with drug-eluting stents. J Am Coll Cardiol. 2005. June 21; 45( 12): 2088– 92. [DOI] [PubMed] [Google Scholar]
- 10. Iakovou I, Schmidt T, Bonizzoni E, . et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005. May 4; 293( 17): 2126– 30. [DOI] [PubMed] [Google Scholar]
- 11. Kuchulakanti P, Chu W, Torguson R, . et al. Correlates and long-term outcomes of angiographically proven stent thrombosis with sirolimus- and paclitaxel-eluting stents. Circulation. 2006. February 28; 113( 8): 1108– 13. [DOI] [PubMed] [Google Scholar]
- 12. Spertus J, Kettelkamp R, Vance C, . et al. Prevalence, predictors, and outcomes of premature discontinuation of thienopyridine therapy after drug-eluting stent placement: results from the PREMIER registry. Circulation. 2006. June 20; 113( 24): 2803– 9. [DOI] [PubMed] [Google Scholar]
- 13. Cooke JP, Ghebremariam YT. Dietary nitrate, nitric oxide, and restenosis. J Clin Invest. 2011. April; 121( 4): 1258– 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ma X, Wu T, Robich MP.. Drug-eluting stent coatings. J Interv Cardiol. 2012; 4( 1): 73– 83. [Google Scholar]
- 15. Protopopov AV, Kochkina TA, Konstantinov EP, . et al. Investigation of application of PHA coating to enhance biocompatibility of vascular stents. Dokl Biol Sci. 2005. Mar-Apr; 401: 85– 7. [DOI] [PubMed] [Google Scholar]
- 16. Kondyurin AV, Romanova V, Begishev V, Kondyurina I, Guenzel R, Maitz M.. Crosslinked polyurethane coating on vascular stents for enhanced X-ray contrast. J Bioact Compat Pol. 2005; 20( 1): 77– 93. [Google Scholar]
- 17. Choudhary S, Haberstroh K, Webster T.. Enhanced functions of vascular cells on nanostructured Ti for improved stent applications. Tissue Eng. 2007. July; 13( 7): 1421– 30. [DOI] [PubMed] [Google Scholar]
- 18. Iakovou I, Schmidt T, Bonizzoni E, . et al. Incidence, predictors and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005. May 4; 293( 17): 2126– 30. [DOI] [PubMed] [Google Scholar]
- 19. Lim IA. Biocompatibility of stent materials. MIT Undergraduate Research Journal. 2004; 11( 1): 33– 7. [Google Scholar]
- 20. Hara H, Nakamura M, Palmaz JC, Schwartz RS.. Role of stent design and coatings on restenosis and thrombosis. Adv Drug Deliv Rev. 2006. June 3; 58( 3): 377– 86. [DOI] [PubMed] [Google Scholar]
- 21. Kereiakes DJ, Cox DA, Hermiller JB, . et al; Guidant Multi-Link Vision Stent Registry Investigators Usefulness of a cobalt chromium coronary stent alloy. Am J Cardiol. 2003. August 15; 92( 4): 463– 6. [DOI] [PubMed] [Google Scholar]
- 22. Lu J. Nano-fabrication and characterization of novel titanium surfaces for vascular stent application [Thesis]. [Providence, RI]: Brown University; 2010. 295 p. [Google Scholar]
- 23. Di Mario C, Marsico F, Adamian M, Karvouni E, Albiero R, Colombo A.. New recipes for in-stent restenosis: cut, grate, roast, or sandwich the neointima? Heart. 2000. November; 84( 5): 471– 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. vom Dahl J, Dietz U, Haager PK, . et al. Rotational atherectomy does not reduce recurrent in-stent restenosis: results of the angioplasty versus rotational atherectomy for treatment of diffuse in-stent restenosis trial (ARTIST). Circulation. 2002. February 5; 105( 5): 583– 8. [DOI] [PubMed] [Google Scholar]
- 25. Michaels AD, Chatterjee K. Cardiology patient pages. Angioplasty versus bypass surgery for coronary artery disease. Circulation. 2002. December 3; 106( 23): e187– 90. [DOI] [PubMed] [Google Scholar]
- 26. Wessely R, Hausleiter J, Michaelis C, . et al. Inhibition of neointima formation by a novel drug-eluting stent system that allows for dose-adjustable, multiple, and on-site stent coating. Arterioscler Thromb Vasc Biol. 2005. April; 25( 4): 748– 53. [DOI] [PubMed] [Google Scholar]
- 27. Hausleiter J, Kastrati A, Wessely R, . et al. Prevention of restenosis by a novel drug-eluting stent system with a dose-adjustable, polymer-free, on-site stent coating. Eur Heart J. 2005. August; 26( 15): 1475– 81. [DOI] [PubMed] [Google Scholar]
- 28. Moore P, Barlis P, Spiro J, . et al. A randomized optical coherence tomography study of coronary stent strut coverage and luminal protrusion with rapamycin-eluting stents. JACC Cardiovasc Interv. 2009. May; 2( 5): 437– 44. [DOI] [PubMed] [Google Scholar]
- 29. Abizaid A, Costa JR Jr.. New drug-eluting stents: an overview on biodegradable and polymer-free next-generation stent systems. Circ Cardiovasc Interv. 2010. August; 3( 4): 384– 93. [DOI] [PubMed] [Google Scholar]
- 30. Tada N, Virmani R, Grant G, . et al. Polymer-free biolimus A9-coated stent demonstrates more sustained intimal inhibition, improved healing, and reduced inflammation compared with a polymer-coated sirolimus-eluting cypher stent in a porcine model. Circ Cardiovasc Interv. 2010. April; 3( 2): 174– 83. [DOI] [PubMed] [Google Scholar]
- 31. Cre8™ Technical Information. Retrieved from http://www.alvi-medica.com/cre8-technical-information/.
- 32. Rajtar A, Kaluza GL, Yang Q, . et al. Hydroxyapatite-coated cardiovascular stents. EuroIntervention. 2006. May; 2( 1): 113– 5. [PubMed] [Google Scholar]
- 33. Garg S, Bourantas C, Serruys PW.. New concepts in the design of drug-eluting coronary stents. Nat Rev Cardiol. 2013. May; 10( 5): 248– 60. [DOI] [PubMed] [Google Scholar]
- 34. Wieneke H, Dirsch O, Sawitowski T, . et al. Synergistic effects of a novel nanoporous stent coating and tacrolimus on intima proliferation in rabbits. Catheter Cardiovasc Interv. 2003. November; 60( 3): 399– 407. [DOI] [PubMed] [Google Scholar]
- 35. Kollum M, Farb A, Schreiber R. et al. Particle debris from a nanoporous stent coating obscures potential antiproliferative effects of tacrolimus-eluting stents in a porcine model of restenosis. Catheter Cardiovasc Interv. 2005. January; 64( 1): 85– 90. [DOI] [PubMed] [Google Scholar]
- 36. Khang D, Lu J, Yao C, Haberstroh KM, Webster TJ.. The role of nanometer and sub-micron surface features on vascular and bone cell adhesion on titanium. Biomaterials. 2008. March; 29( 8): 970– 83. [DOI] [PubMed] [Google Scholar]
- 37. Nakano K, Egashira K, Masuda S, . et al. Formulation of nanoparticle-eluting stents by a cationic electrodeposition coating technology: efficient nano-drug delivery via bioabsorbable polymeric nanoparticle-eluting stents in porcine coronary arteries. JACC Cardiovasc Interv. 2009. April; 2( 4): 277– 83. [DOI] [PubMed] [Google Scholar]
- 38. Polyak B, Fishbein I, Chorny M, . et al. High field gradient targeting of magnetic nanoparticle-loaded endothelial cells to the surfaces of steel stents. Proc Natl Acad Sci U S A. 2008. January 15; 105( 2): 698– 703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lai ES, Huang NF, Cooke JP, Fuller GG.. Aligned nanofibrillar collagen regulates endothelial organization and migration. Regen Med. 2012. September; 7( 5): 649– 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Huang NF, Okogbaa J, Lee JC, . et al. The modulation of endothelial cell morphology, function, and survival using anisotropic nano-fibrillar collagen scaffolds. Biomaterials. 2013. May; 34( 16): 4038– 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Huang NF, Lai ES, Ribeiro AJ, . et al. Spatial patterning of endothelium modulates cell morphology, adhesiveness and transcriptional signature. Biomaterials. 2013. April; 34( 12): 2928– 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Black J, Hastings G. Handbook of biomaterial properties. London, England: Chapman & Hall; 1998. 589 p. [Google Scholar]
- 43. Park H, Cannizzaro C, Vunjak-Novakovic G, Langer R, Vacanti C, Farokhzad O.. Nanofabrication and microfabrication of functional materials for tissue engineering. Tissue Eng. 2007. August; 13( 8): 1867– 77. [DOI] [PubMed] [Google Scholar]
- 44. Park TH, Shuler ML. Integration of cell culture and microfabrication technology. Biotechnol Prog. 2003. Mar-Apr; 19( 2): 243– 53. [DOI] [PubMed] [Google Scholar]
- 45. Chehroudi B, McDonnell D, Brunette DM.. The effects of micro-machined surfaces on formation of bonelike tissue on subcutaneous implants as assessed by radiography and computer image processing. J Biomed Mater Res. 1997. March 5; 34( 3): 279– 90. [DOI] [PubMed] [Google Scholar]
- 46. Sarkar S, Dadhania M, Rourke P, Desai T, Wong J.. Vascular tissue engineering: microtextured scaffold templates to control organization of vascular smooth muscle cells and extracellular matrix. Acta Biomater. 2005. January; 1( 1): 93– 100. [DOI] [PubMed] [Google Scholar]
- 47. Shin M, Matsuda K, Ishii O, . et al. Endothelialized networks with a vascular geometry in microfabricated poly(dimethyl siloxane). Biomed Microdevices. 2004. December; 6( 4): 269– 78. [DOI] [PubMed] [Google Scholar]
- 48. Windecker S, Mayer I, De Pasquale G, . et al; Working Group on Novel Surface Coating of Biomedical Devices (SCOL) Stent coating with titanium-nitride-oxide for reduction of neointimal hyperplasia. Circulation. 2001. August 21; 104( 8): 928– 33. [DOI] [PubMed] [Google Scholar]
- 49. Sternberg K, Grabow N, Petersen S, . et al. Advances in coronary stent technology--active drug-loaded stent surfaces for prevention of restenosis and improvement of biocompatibility. Curr Pharm Biotechnol. 2013; 14( 1): 76– 90. [PubMed] [Google Scholar]
- 50. Colombo A, Karvouni E. Biodegradable stents: “fulfilling the mission and stepping away”. Circulation. 2000. July 25; 102( 4): 371– 3. [DOI] [PubMed] [Google Scholar]
- 51. Grabow N, Bünger CM, Schultze C, . et al. A biodegradable slotted tube stent based on poly(L-lactide) and poly(4-hydroxy-butyrate) for rapid balloon-expansion. Ann Biomed Eng. 2007. December; 35( 12): 2031– 8. [DOI] [PubMed] [Google Scholar]
- 52. Zartner P, Buettner M, Singer H, Sigler M.. First biodegradable metal stent in a child with congenital heart disease: evaluation of macro and histopathology. Catheter Cardiovasc Interv. 2007. February 15; 69( 3): 443– 6. [DOI] [PubMed] [Google Scholar]
- 53. Uurto I, Juuti H, Parkkinen J.. Biodegradable self-expanding poly-L/D-lactic acid vascular stent: a pilot study in canine and porcine iliac arteries. J Endovasc Ther. 2004. December; 11( 6): 712– 8. [DOI] [PubMed] [Google Scholar]
- 54. Venkatraman SS, Tan LP, Joso JF, Boey YC, Wang X.. Biodegradable stents with elastic memory. Biomaterials. 2006. March; 27( 8): 1573– 8. [DOI] [PubMed] [Google Scholar]
- 55. Wong YS, Xiong Y, Venkatraman SS, Boey FY.. Shape memory in un-cross-linked biodegradable polymers. J Biomater Sci Polym Ed. 2008; 19( 2): 175– 91. [DOI] [PubMed] [Google Scholar]
- 56. Bünger CM, Grabow N, Kröger C, . et al. Iliac anastomotic stenting with a sirolimus-eluting biodegradable poly-L-lactide stent: a preliminary study after 6 weeks. J Endovasc Ther. 2006. October; 13( 5): 630– 9. [DOI] [PubMed] [Google Scholar]
- 57. Venkatraman S, Poh TL, Vinalia T, Mak KH, Boey F.. Collapse pressures of biodegradable stents. Biomaterials. 2003. May; 24( 12): 2105– 11. [DOI] [PubMed] [Google Scholar]
- 58. Zilberman M, Nelson KD, Eberhart RC.. Mechanical properties and in vitro degradation of bioresorbable fibers and expandable fiber-based stents. J Biomed Mater Res B Appl Biomater. 2005. August; 74( 2): 792– 9. [DOI] [PubMed] [Google Scholar]
- 59. Welch TR, Eberhart RC, Chuong CJ.. The influence of thermal treatment on the mechanical characteristics of a PLLA coiled stent. J Biomed Mater Res B Appl Biomater. 2009. July; 90( 1): 302– 11. [DOI] [PubMed] [Google Scholar]
- 60. Ormiston JA1, Webster MW, Armstrong G.. First-in-human implantation of a fully bioabsorbable drug-eluting stent: the BVS poly-L-lactic acid everolimus-eluting coronary stent. Catheter Cardiovasc Interv. 2007. January; 69( 1): 128– 31. [DOI] [PubMed] [Google Scholar]
- 61. Serruys PW, Ormiston JA, Onuma Y, . et al. A bioabsorbable everolimus-eluting coronary stent system (ABSORB): 2-year outcomes and results from multiple imaging methods. Lancet. 2009. March 14; 373( 9667): 897– 910. [DOI] [PubMed] [Google Scholar]
- 62. Bruining N, de Winter S, Roelandt JR, . et al. Monitoring in vivo absorption of a drug-eluting bioabsorbable stent with intravascular ultrasound-derived parameters a feasibility study. JACC Cardiovasc Interv. 2010. April; 3( 4): 449– 56. [DOI] [PubMed] [Google Scholar]
- 63. Peuster M, Wohlsein P, Brügmann M, . et al. A novel approach to temporary stenting: degradable cardiovascular stents produced from corrodible metal-results 6–18 months after implantation into New Zealand white rabbits. Heart. 2001. November; 86( 5): 563– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Peuster M, Hesse C, Schloo T, Fink C, Beerbaum P, von Schnakenburg C.. Long-term biocompatibility of a corrodible peripheral iron stent in the porcine descending aorta. Biomaterials. 2006. October; 27( 28): 4955– 62. [DOI] [PubMed] [Google Scholar]
- 65. Di Mario C, Griffiths H, Goktekin O, . et al. Drug-eluting bioabsorbable magnesium stent. J Interv Cardiol. 2004. December; 17( 6): 391– 5. [DOI] [PubMed] [Google Scholar]
- 66. Erbel R, Di Mario C, Bartunek J, PROGRESS-AMS (Clinical Performance and Angiographic Results of Coronary Stenting with Absorbable Metal Stents) Investigators. . Temporary scaffolding of coronary arteries with bioabsorbable magnesium stents: a prospective, non-randomised multicentre trial. Lancet. 2007. June 2; 369( 9576): 1869– 75. [DOI] [PubMed] [Google Scholar]
- 67. Waksman R, Erbel R, Di Mario C, . et al; PROGRESS-AMS (Clinical Performance Angiographic Results of Coronary Stenting with Absorbable Metal Stents) Investigators. Early- and long-term in-travascular ultrasound and angiographic findings after bioabsorbable magnesium stent implantation in human coronary arteries. JACC Cardiovasc Interv. 2009. April; 2( 4): 312– 20. [DOI] [PubMed] [Google Scholar]
- 68. Santos A, Aw MS, Bariana M, Kumeria T, Wang Y, Losic D.. Drug-releasing implants: current progress, challenges, and perspectives. J Mater Chem. 2014; 2: 6157– 82. [DOI] [PubMed] [Google Scholar]


