Abstract
Despite an improved understanding of its pathophysiology and a wide range of new treatments, cardiovascular disease (CVD) remains a serious public health issue and the number one cause of mortality in the United States. Conditions that promote chronic systemic inflammation, such as obesity, cancer, and autoimmune and infectious diseases, are now known to play an important role in promoting CVD by inducing the expression of endothelial adhesion molecules and chemokines; these in turn promote leukocyte adherence and infiltration, which initiates and spurs the progression of CVD. In response to this new understanding, researchers are evaluating the potential cardiovascular benefits of new-generation therapies based on endogenous molecules with anti-inflammatory properties. Similarly, targeted approaches that leverage the phenotypic differences between non-inflamed and inflamed endothelia have the potential to selectively deliver therapeutics and decrease the morbidity and mortality of CVD patients. In this review, we discuss the role of inflammation in CVD and explore the therapeutic potential of targeting inflamed vasculature through conventional and biomimetic approaches.
Keywords: vascular inflammation, cardiovascular diseases, C-reactive protein, NF-kB, endotheliopathies, endothelium, drug delivery platform, theranostic, statins
The Epidemiology and Pathophysiology of Cardiovascular Disease
Cardiovascular disease (CVD) is the major cause of hospital emergency admissions and continues to be the leading cause of death in the United States. Acute vascular events such as myocardial infarction and stroke are typically associated with vascular inflammation, endothelial erosion, and plaque rupture in the coronary or carotid arteries.1 The economic impact of these diseases—including direct and indirect costs—surpasses $500 billion annually, higher than that of cancer and Alzheimer's combined.2
CVD is a multifactorial condition typically associated with hypercholesterolemia, diabetes, smoking, hypertension, and aging. Each of these conditions is known to promote endothelial activation and vascular inflammation.3 In addition, the increasing prevalence of obesity is a public health concern since it contributes to metabolic syndrome, vascular inflammation, and the progression of atherosclerosis. Almost one-third of American children are overweight or obese,2 promoting the initiation of vascular lesions during childhood.4 In obese patients, the number of macrophages, free fatty acids (FFA), and proinflammatory mediators (e.g., tumor necrosis factor-α [TNFα], interleukin-6 [IL-6], C-reactive protein [CRP], and leptin) proportionally increase with the amount of visceral fat, while anti-inflammatory factors (e.g. adiponectin) have an inverse relationship.5 Free fatty acids induce the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, triggering the production of TNFα. In turn, TNFα activates lipolysis, increases macrophage recruitment, and induces the synthesis of IL-6, which stimulates the production and secretion of CRP.6 The interaction between macrophages and adipocytes augments hepatic CRP production and may increase CRP levels, which is a key risk factor for CVD.7,8
The Role of Inflammation in Cardiovascular Disease
Inflammation is the cornerstone of CVD.9 Chronic inflammation in remote sites may promote coronary atherosclerosis.10,11 The relationship between systemic inflammation and coronary events is likely due to the aggravation of local inflammation in coronary plaque. Systemic inflammation may cause endothelial activation, a state characterized by increased expression of endothelial adhesion molecules and chemokines (e.g., vascular cell adhesion molecules [VCAM] and monocyte chemotactic protein [MCP-1]) and reduced expression of antiatherogenic molecules (e.g., nitric oxide and prostacyclin). This state of endothelial activation facilitates leukocyte adherence and infiltration into the vessel wall.1,12 Systemic inflammation also alters the coagulation pathway and increases platelet activation, creating a procoagulant state prone to the formation of thrombi.13,14 Endothelial activation due to systemic inflammation may also be a feature of end-stage cardiovascular diseases such as congestive heart failure, in which there are increased circulating levels of inflammatory cytokines (TNFα, IL-6, CRP).11
Previous work has suggested that the risk of CVD is influenced by the balance between low-density lipoprotein (LDL-C) cholesterol particles, which are believed to be more atherogenic, and high-density lipoprotein (HDL-C) cholesterol particles, which are believed to be protective.15 (Note that this conventional paradigm may need to be revisited based upon disappointing clinical trials in which agents increasing HDL-C did not protect against major cardiovascular events.16) Inflammatory cytokines generally reduce the concentration of HDL-C and increase triglyceride concentrations, which is an unfavorable lipid profile associated with cardiovascular events.17,18 Furthermore, LDL-C is believed to be more atherogenic when oxidized (oxLDL), as when it is trapped in the subendothelial space. In an inflamed vessel wall, there is increased generation of reactive oxygen species (ROS) by infiltrating immune cells and activated vascular cells.19 The accumulating oxLDL is imbibed by resident macrophages, inducing the immune cells to generate more inflammatory cytokines and chemokines.20 A positive feedback loop is established, increasing the expression of endothelial adhesion molecules to facilitate monocyte adhesion and diapedesis.1 The endothelium is particularly vulnerable to this process at sites of low shear stress, such as bends or bifurcations, or downstream of a stenotic lesion.1 In summary, the initiation and propagation of atherosclerosis is heavily influenced by endothelial activation and vascular inflammation, both of which lead to the initiation of atherogenesis, the progression of plaque formation, plaque rupture, and thrombosis.1,20
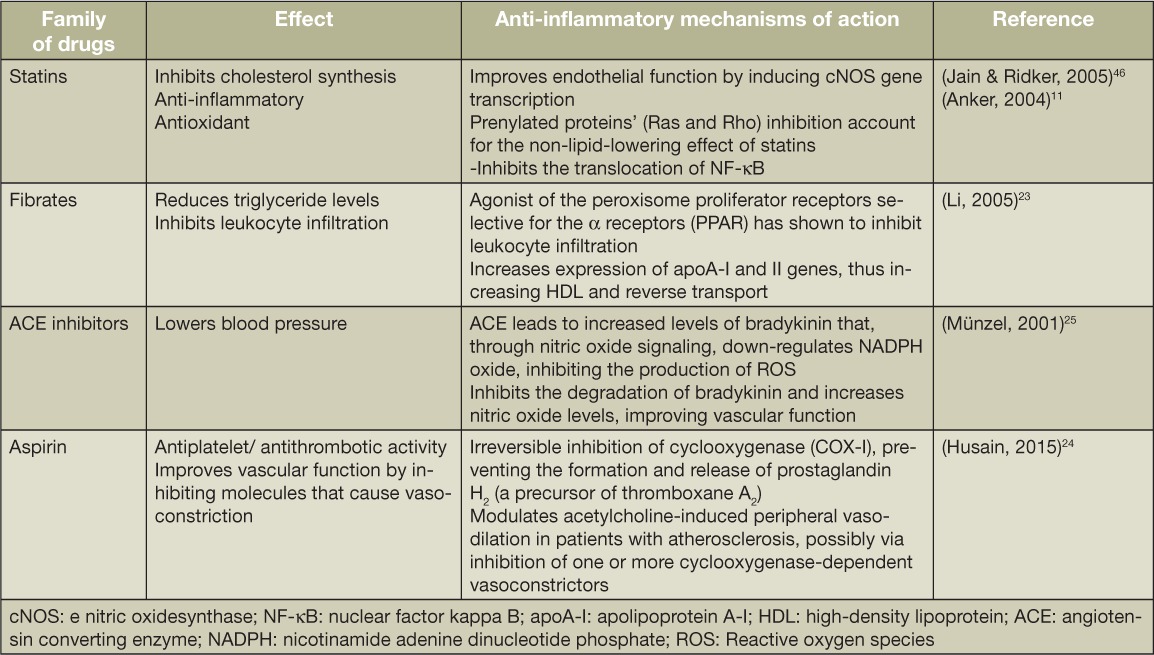
The benefit of antilipid therapy is clearly proportional to the extent of LDL-C reduction, but there are data indicating that the benefits may also be due to anti-inflammatory effects.7 Statins are the most effective therapeutic option for reducing LDL-C and remain the gold standard for treating CVD. Numerous clinical trials—including 4S, WOSCOP, CARE, LIPID, AFCAPS/TexCAPS, ASCOT-LLA, and HPS—have proven the benefits of statins and their effects on LDL-C. Statins also have substantial anti-inflammatory effects that may contribute to the inhibition of NF-κB activity, reducing the downstream activation of genes that regulate endothelial adhesiveness, permeability, and prothrombotic response. Statins also reduce blood levels of CRP,11 another risk factor for CVD.21
Other classes of drugs used to treat CVD—such as fibrates, angiotensin-converting enzyme inhibitors (ACEI), angiotensin receptor blockers (ARBs), and aspirin—may have beneficial effects through anti-inflammatory pathways. Fibrates facilitate reverse cholesterol transport22 but may also repress TNFα expression23 and inhibit NF-κB activation. The antiplatelet effects of aspirin largely mediate its cardiovascular benefits, but they also inhibit the production of proinflammatory and vasoconstrictor products of the cyclooxygenase I (COX-1) pathway.24 The beneficial effects of ACEIs are due to inhibition of angiotensin II formation and preservation of bradykinin, which enhance vasodilation and reduce afterload. However, anti-inflammatory effects may also contribute.25 For example, angiotensin II stimulates monocyte infiltration and proliferation and is a powerful activator of NADPH oxidase in the vessel wall. This enzyme system is a major contributor to the generation of ROS, which will oxidize LDL-C and degrade nitric oxide, reversing the vasodilatory effect of this endothelium-derived factor. Thus, inhibition of angiotensin synthesis (ACEIs) or action (ARBs) will be vasoprotective.
As this brief discussion suggests, there may be major cardiovascular benefits to exploring anti-inflammatory therapies for CVD treatment. It is also possible that these benefits may be greater if the anti-inflammatory therapies can be targeted toward the vessel wall to avoid systemic side effects.
Novel Targeting Strategies: The Beginning of a New Era
While there is an abundance of small drug molecules on the market that are effective for CVD treatment, the use of novel biological therapeutics (i.e., genetic materials, proteins, and peptides) remains challenging due to their poor stability upon systemic injection26 and the lack of efficient delivery methods. Efforts have been made to develop specialized carriers that facilitate delivery of biologics and identify the most effective molecular targets in desired tissues. As a result, several drug delivery platforms of varying size, shape, and material have been formulated. These platforms rely primarily on two fundamental aspects: (1) versatile formulation that permits the encapsulation of therapeutic agents, and (2) surface functionalization with targeting agents (i.e., antibodies, aptamers, and small molecules) to deliver therapeutics or diagnostics to pathological sites of inflammation within the endothelium.27
For most drug delivery platforms, the vascular system represents a natural route to reach diseased tissues.28 However, the vasculature can also be problematic29 since therapeutics cannot be delivered to a localized site when systemically administered.30 Recently, the endothelial layer has been identified as a potential target for pharmaceutical intervention due to its active involvement in the pathogenesis of CVD. Vascular inflammation and/or increased endothelial permeability are common mechanisms involved in atherosclerosis, heart failure, diabetic vascular disease, and ischemia-reperfusion injury (Figure 1).31 These endothelial alterations can facilitate delivery to the tissues subserved by these abnormal vessels. For example, nanostructured mesoporous silicon vectors (MSV) loaded with 10-nm polymeric micelles were used as a theranostic tool in chronic heart failure.31 The authors demonstrated that MSVs accumulated in failing myocardium after intravenous injection, suggesting a cardiac enhanced permeation and retention (CEPR) effect. Contrast agents, nanosensors, or therapeutics might thus be selectively delivered into failing myocardium for preventive, diagnostic, or therapeutic purposes.
Figure 1.
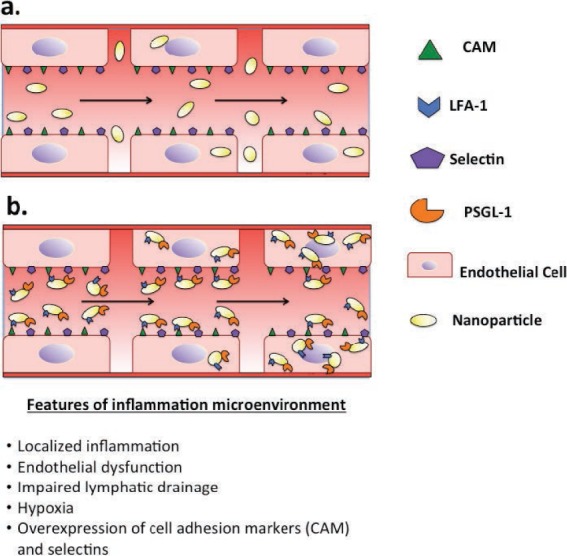
Schematic of (a) passive and (b) active targeting approaches.
Another approach is to design carriers functionalized with analogs of natural CAMs or selectin-ligands (i.e., anti-VCAM,32 anti-ICAM1, sialyl-Lewis X, PSGL-1)33 as well as lymphocyte function-associated antigen 1 (LFA-1) mimetics or antioxidized low-density lipoprotein receptor (LOX-1).34 This approach has prompted the development of bio-inspired carriers that target these moieties (Figure 1). In particular, CAMs are markers of inflammation, and their overexpression promotes the adhesion of immune cells. As leukocytes naturally target inflamed endothelium regardless of the injury, biomimetic carriers follow leukocyte tropism and selectively deliver cargo to the diseased tissue. Yanh et al. found that multifunctional core-shell VCAM-1-targeted Fe3O4SiO2 nanoparticles are preferentially internalized by inflamed endothelial cells compared to non-targeted nanoparticles.32 Liposomes targeting VCAM-1 were used in atherosclerotic mouse models and exhibited the ability to deliver a therapeutic effect.35
Nanoparticle-Based Imaging Strategies in Cardiovascular Disease
Biological targeting of inflamed endothelium has also been used to develop theranostic strategies that both image and treat the complex pathology of CVDs. For example, researchers have designed D-phe-pro-arg-chloromethyl ketone (PPACK) and micelle-based nanoparticles (NPs) with a high affinity for thrombi.36,37 The PPACK was conjugated with perfluorocarbon NPs while the micelle was loaded with an anticoagulant. Both of these approaches showed a significant antithrombotic effect when compared to anticoagulants delivered systemically without targeting vectors.38 Nanoparticles conjugated with Indium (111In) and surfaces functionalized with antibodies that bind to low-density LOX-1 receptors have been used to image atherosclerotic plaques in ApoE−/− knockout mice.34 Micelles loaded with gadolinium conjugated with anti-CD36 antibodies targeted the macrophages found in atherosclerotic human aortas. Through different imaging options, it is possible to follow NP biodistribution in the circulatory system, demonstrate extravasation, and track accumulation within the inflamed tissue and removal by the lymphatic system. Such studies provide information on biodistribution of NPs that complements studies of their therapeutic efficacy.
Biomimicry Inspires the Design of Drug Delivery Carriers
The decoration of carrier surfaces with moieties mimicking natural ligands can provide selective targeting and precise delivery of therapeutics to a diseased tissue. Even so, the sequestration of NPs by the mononuclear phagocyte system and the inability to adequately negotiate other biological barriers has hindered their clinical translation. New biomimetic developments are mainly based on two strategies: (1) top-down approaches, including the bioengineering of pathogens (bacteria and viruses) or cells (leukocytes, erythrocytes, platelets, and stem cells39), or (2) bottom-up approaches, such as conjugating NP surfaces with analogs of bioactive molecules that bind CAMs and selectins33,40 or coating synthetic particles with cell membranes as reported by Parodi et al.41 Additional approaches include poly(lactic-co-glycolic acid) (PLGA) NPs cloaked with platelet cell membrane that preferentially bind the denuded artery in a rat model of coronary restenosis.40
Other biomimetic NPs based on endogenous carriers such as LDL and HDL have been engineered to incorporate nucleic material and deliver therapeutic and diagnostic molecules.42 Low-density lipoproteins also have been used as imaging contrast agents in combination with gold NPs.43 The ability to modify these endogenous proteins to encapsulate and deliver lipophilic drugs continues to expand and indicates their potential effectiveness in selectively targeting drugs for CVD.44
In addition to the aforementioned platforms and strategies, Molinaro et al. recently published a novel method that combines the top-down and bottom-up approaches to assemble hybrid bio-mimetic nanovesicles.45 The platform is an evolution of the coating process previously employed for functionalization of lipid vesicles. In this iteration, membrane proteins are isolated from infiltrating immune cells and reconstituted with biocompatible choline-based phospholipids in a liposome-like nanovesicle called Leukosome.45 This method was derived from techniques commonly used to prepare liposomes. Leukocyte-like properties were conferred to Leukosomes by integrating more than 300 membrane proteins into their post-transcriptional status in the lipid bilayer. Among these properties, proteomic analysis revealed the presence of receptors that enabled adhesion of Leukosomes to activated vasculature and also revealed their self-tolerance and ability to evade immune clearance.45
Despite the authors' use of this biomimetic platform in a mouse model of localized inflammation, their description of the conservation of molecular pathways, the receptors involved, and the dynamic interactions between key cell types during the inflammatory process opens the possibility of employing Leukosomes in CVD, where inflammation plays a fundamental role in endothelial activation. Overall, these bio-inspired approaches represent the next generation of nanomedical therapeutics since they provide an alternative solution for evading the mononuclear phagocytic system and for transport across the endothelial vessel wall.
Table 1.
Summary of mechanisms of action for drugs treating/controlling cardiovascular disease.
Conclusion
Novel drug delivery platforms have the potential to encapsulate a plethora of molecules (both small drugs and biologics) and selectively deliver them to sites of endothelial inflammation. Altered endothelium can be targeted through classical approaches based on antibodies and other ligands or through a new generation of biomimetic delivery systems. These systems are based on the unique biology of certain cell phenotypes that have the ability to recognize inflammation and overcome the endothelial barrier. In particular, it is possible to engineer nanodelivery systems that maintain some of the properties of immune system cells such as macrophages, leukocytes, and T cells. By leveraging the exclusive ability of these cells to locate, recognize, and infiltrate sites of tissue inflammation, we and others have created alternative platforms that can selectively deliver therapeutic and diagnostic pay-loads to the areas of interest in a variety of pathological conditions associated with local vascular inflammation. Taken together, these discoveries illuminate three potential areas for further research: (1) understanding CVD pathophysiology as a result of inflammation pathways, (2) designing therapeutics that exploit inflamed endothelium in order to passively (CEPR effect) or actively (surface functionalized with targeting agents) target the diseased tissue, and (3) overcoming the current limitations of available therapies characterized by severe side effects and unwanted toxicity to healthy tissue. New developments in nanoparticle fabrication coupled with our understanding of endothelial-leukocyte interaction in CVD may soon allow the targeted delivery of novel cardiovascular therapies to sites of vascular inflammation, leading to greater efficacy and reduced systemic adverse effects.
Key Points
Local vascular inflammation plays a key role in the initiation and progression of atherosclerosis.
Systemic inflammation may heighten local vascular inflammation and accelerate the progression of atherosclerosis.
Agents that are effective at controlling local vascular inflammation may reduce cardiovascular morbidity and mortality.
Inflamed endothelium represents a viable target for targeted strategies due to the altered phenotype of adhesive surface markers and increased vascular permeability.
Novel nanotherapeutic approaches can exploit inflamed endothelium in order to passively (CEPR effect) or actively (surface functionalized with binding moieties) target diseased tissue.
Acknowledgments
The authors would like to thank Megan Livingston for editing this publication.
Footnotes
Conflict of Interest Disclosure: This research was funded by the National Institutes of Health (1R21CA173579-01A1, 1R21CA173579-Cornerstone, and 5U54CA143837 PSOC Pilot project), the U.S. Department of Defense (W81XWH-12-10414 BCRP Innovator Expansion), Brown Foundation-Bioma-terials Eng., William Randolph Hearst Foundation/Hearst Cardiovascular Regeneration, The Regenerative Medicine Program Cullen Trust for Health Care/Cullen Trust Fellowship, George J. and Angelina P. Kostas Charitable Foundation. This work also was supported in part by grants to Dr. Cooke from the National Institutes of Health (U01 HL100397) and the Cancer Prevention and Research Institute (RP150611).
References
- 1. Falk E. Pathogenesis of atherosclerosis. J Am Coll Cardiol. 2006. April; 47( 8s1): C7– C12. [DOI] [PubMed] [Google Scholar]
- 2. Mozaffarian D, Benjamin EJ, Go AS, . et al. Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016. January 26; 133( 4): e38– e360. [DOI] [PubMed] [Google Scholar]
- 3. Cooke JP. Flow, NO, and atherogenesis. Proc Natl Acad Sci U S A. 2003. February 4; 100( 3): 768– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Strong JP, Malcom GT, McMahan CA, . et al. Prevalence and extent of atherosclerosis in adolescents and young adults: implications for prevention from the Pathobiological Determinants of Atherosclerosis in Youth Study. JAMA. 1999. February 24; 281( 8): 727– 35. [DOI] [PubMed] [Google Scholar]
- 5. Cartier A, Lemieux I, Alméras N, Tremblay A, Bergeron J, Després JP.. Visceral obesity and plasma glucose-insulin homeostasis: contributions of interleukin-6 and tumor necrosis factor-alpha in men. J Clin Endocrinol Metab. 2008. May; 93( 5): 1931– 8. [DOI] [PubMed] [Google Scholar]
- 6. Abeywardena MY, Leifert WR, Warnes KE, Varghese JN, Head RJ.. Cardiovascular biology of interleukin-6. Curr Pharm Des. 2009; 15( 15): 1809– 21. [DOI] [PubMed] [Google Scholar]
- 7. Ridker PM. High-sensitivity C-reactive protein and cardiovascular risk: rationale for screening and primary prevention. Am J Cardiol. 2003. August 21; 92( 4B): 17K– 22K. [DOI] [PubMed] [Google Scholar]
- 8. Goldberg RB. Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab. 2009. September; 94( 9): 3171– 82. [DOI] [PubMed] [Google Scholar]
- 9. Libby P. Inflammation in atherosclerosis. Nature. 2002. December 19–26; 420( 6917): 868– 74. [DOI] [PubMed] [Google Scholar]
- 10. Roman MJ, Shanker BA, Davis A, . et al. Prevalence and correlates of accelerated atherosclerosis in systemic lupus erythematosus. N Engl J Med. 2003. December 18; 349( 25): 2399– 406. [DOI] [PubMed] [Google Scholar]
- 11. Anker SD, von Haehling S. Inflammatory mediators in chronic heart failure: an overview. Heart. 2004. April; 90( 4): 464– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vallance P, Collier J, Bhagat K.. Infection, inflammation, and infarction: does acute endothelial dysfunction provide a link? Lancet. 1997. May 10; 349( 9062): 1391– 2. [DOI] [PubMed] [Google Scholar]
- 13. Levi M, van der Poll T, Büller HR.. Bidirectional relation between inflammation and coagulation. Circulation. 2004. June 8; 109( 22): 2698– 704. [DOI] [PubMed] [Google Scholar]
- 14. Wagner DD, Burger PC. Platelets in inflammation and thrombosis. Arterioscler Thromb Vasc Biol. 2003. December; 23( 12): 2131– 7. [DOI] [PubMed] [Google Scholar]
- 15. Skålén K, Gustafsson M, Rydberg EK, . et al. Subendothelial retention of atherogenic lipoproteins in early atherosclerosis. Nature. 2002. June 13; 417( 6890): 750– 4. [DOI] [PubMed] [Google Scholar]
- 16. Kones R, Rumana U. Current treatment of dyslipidemia: evolving roles of non-statin and newer drugs. Drugs. 2015. July; 75( 11): 1201– 28. [DOI] [PubMed] [Google Scholar]
- 17. Ansell BJ, Watson KE, Fogelman AM, Navab M, Fonarow GC.. High-density lipoprotein function recent advances. J Am Coll Cardiol. 2005. November 15; 46( 10): 1792– 8. [DOI] [PubMed] [Google Scholar]
- 18. Esdaile JM, Abrahamowicz M, Grodzicky T, . et al. Traditional Framingham risk factors fail to fully account for accelerated atherosclerosis in systemic lupus erythematosus. Arthritis Rheum. 2001. October; 44( 10): 2331– 7. [DOI] [PubMed] [Google Scholar]
- 19. Krauss RM, Winston M, Fletcher BJ, Grundy SM.. Obesity: impact on cardiovascular disease. Circulation. 1998. October 6; 98( 14): 1472– 76. [PubMed] [Google Scholar]
- 20. Goldstein JL, Ho YK, Basu SK, Brown MS.. Binding site on macrophages that mediates uptake and degradation of acetylated low density lipoprotein, producing massive cholesterol deposition. Proc Natl Acad Sci U S A. 1979. January; 76( 1): 333– 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Libby P, Ridker PM, Hansson GK.. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011. May 19; 473( 7347): 317– 25. [DOI] [PubMed] [Google Scholar]
- 22. Jun M, Foote C, Lv J, . et al. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. 2010. May 29; 375( 9729): 1875– 84. [DOI] [PubMed] [Google Scholar]
- 23. Li S, Gokden N, Okusa MD, Bhatt R, Portilla D.. Anti-inflammatory effect of fibrate protects from cisplatin-induced ARF. Am J Physiol Renal Physiol. 2005. August; 289( 2): F469– 80. [DOI] [PubMed] [Google Scholar]
- 24. Husain S, Andrews NP, Mulcahy D, Panza JA, Quyyumi AA.. Aspirin improves endothelial dysfunction in atherosclerosis. Circulation. 1998. March 3; 97( 8): 716– 20. [DOI] [PubMed] [Google Scholar]
- 25. Münzel T, Keaney JF. Are ACE inhibitors a “magic bullet” against oxidative stress? Circulation. 2001. September 25; 104( 13): 1571– 4. [DOI] [PubMed] [Google Scholar]
- 26. Molinaro R, Wolfram J, Federico C, . et al. Polyethylenimine and chitosan carriers for the delivery of RNA interference effectors. Expert Opin Drug Deliv. 2013. December; 10( 12): 1653– 68. [DOI] [PubMed] [Google Scholar]
- 27. Chacko AM, Hood ED, Zern BJ, Muzykantov VR.. Targeted nano-carriers for imaging and therapy of vascular inflammation. Curr Opin Colloid Interface Sci. 2011. June; 16( 3): 215– 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Muzykantov VR. Targeted therapeutics and nanodevices for vascular drug delivery: quo vadis? IUBMB Life. 2011. August; 63( 8): 583– 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Howard M, Zern BJ, Anselmo AC, Shuvaev VV, Mitragotri S, Muzykantov V.. Vascular Targeting of Nanocarriers: Perplexing Aspects of the Seemingly Straightforward Paradigm. ACS Nano. 2014. May 27; 8( 5): 4100– 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wagner DD, Frenette PS. The vessel wall and its interactions. Blood. 2008. June 1; 111( 11): 5271– 81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ruiz-Esparza GU, Segura-Ibarra V, Cordero-Reyes AM, . et al. A specifically designed nanoconstruct associates, internalizes, traffics in cardiovascular cells, and accumulates in failing myocardium: a new strategy for heart failure diagnostics and therapeutics. Eur J Heart Fail. 2016. February; 18( 2): 169– 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Yang H, Zhao F, Li Y, . et al. VCAM-1-targeted core/shell nanoparticles for selective adhesion and delivery to endothelial cells with lipopolysaccharide-induced inflammation under shear flow and cellular magnetic resonance imaging in vitro. Int J Nanomedicine. 2013; 8: 1897– 906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Robbins GP, Saunders RL, Haun JB, Rawson J, Therien MJ, Hammer DA.. Tunable leuko-polymersomes that adhere specifically to inflammatory markers. Langmuir. 2010. September 7; 26( 17): 14089– 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li D, Patel AR, Klibanov AL, . et al. Molecular imaging of athero-sclerotic plaques targeted to oxidized LDL receptor LOX-1 by SPECT/CT and magnetic resonance. Circ Cardiovasc Imaging. 2010. July; 3( 4): 464– 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Homem de Bittencourt PI Jr, Lagranha DJ, Maslinkiewicz A, . et al. LipoCardium: endothelium-directed cyclopentenone prostaglan-din-based liposome formulation that completely reverses atherosclerotic lesions. Atherosclerosis. 2007. August; 193( 2): 245– 58. [DOI] [PubMed] [Google Scholar]
- 36. Cyrus T, Zhang H, Allen JS, . et al. Intramural delivery of rapamycin with alphavbeta3-targeted paramagnetic nanoparticles inhibits stenosis after balloon injury. Arterioscler Thromb Vasc Biol. 2008. May; 28( 5): 820– 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chorny M, Fishbein I, Yellen BB, . et al. Targeting stents with local delivery of paclitaxel-loaded magnetic nanoparticles using uniform fields. Proc Natl Acad Sci U S A. 2010. May 4; 107( 18): 8346– 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Myerson J, He L, Lanza G, Tollefsen D, Wickline S.. Thrombin-inhibiting perfluorocarbon nanoparticles provide a novel strategy for the treatment and magnetic resonance imaging of acute thrombosis. J Thromb Haemost. 2011. July; 9( 7): 1292– 300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yoo JW, Irvine DJ, Discher DE, Mitragotri S.. Bio-inspired, bio-engineered and biomimetic drug delivery carriers. Nat Rev Drug Discov. 2011. July 1; 10( 7): 521– 35. [DOI] [PubMed] [Google Scholar]
- 40. Hu CM, Fang RH, Wang KC, . et al. Nanoparticle biointerfacing by platelet membrane cloaking. Nature. 2015. October 1; 526( 7571): 118– 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Parodi A, Quattrocchi N, van de Ven AL, . et al. Synthetic nanoparticles functionalized with biomimetic leukocyte membranes possess cell-like functions. Nat Nanotechnol. 2013. January; 8( 1): 61– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. McMahon KM, Mutharasan RK, Tripathy S, . et al. Biomimetic high density lipoprotein nanoparticles for nucleic acid delivery. Nano Lett. 2011. March 9; 11( 3): 1208– 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Allijn IE, Leong W, Tang J, . et al. Gold nanocrystal labeling allows low-density lipoprotein imaging from the subcellular to macroscopic level. ACS Nano. 2013. November 26; 7( 11): 9761– 70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zhang W, He H, Liu J, . et al. Pharmacokinetics and atherosclerotic lesions targeting effects of tanshinone IIA discoidal and spherical biomimetic high density lipoproteins. Biomaterials. 2013. January; 34( 1): 306– 19. [DOI] [PubMed] [Google Scholar]
- 45. Molinaro R, Corbo C, Martinez JO, . et al. Biomimetic proteolipid vesicles for targeting inflamed tissues. Nat Mater. 2016; doi: 10.1038/NMAT4644. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Jain MK, Ridker PM. Anti-inflammatory effects of statins: clinical evidence and basic mechanisms. Nat Rev Drug Discov. 2005. December; 4( 12): 977– 87. [DOI] [PubMed] [Google Scholar]


