Abstract
Introduction:
Hip fractures are common in the elderly patients with an incidence of 320 000 fractures/year in the United States, representing a health-care cost of US$9 to 20 billion. Hip fracture incidence is projected to increase dramatically. Hospitals must modify clinical models to accommodate this growing burden. Comanagement strategies are reported in the literature, but few have addressed orthopedic-hospitalist models. An orthopedic-hospitalist comanagement (OHC) service was established at our hospital to manage hip fracture patients. We sought to determine whether the OHC (1) improves the efficiency of hip fracture management as measured by inpatient length of stay (LOS) and time to surgery (TTS) and (2) whether our results are comparable to those reported in hip fracture comanagement literature.
Methods:
A comparative retrospective–prospective cohort study of patients older than 60 years with an admitting diagnosis of hip fracture was conducted to compare inpatient LOS and TTS for hip fracture patients admitted 10 months before (n = 45) and 10 months after implementation (n = 54) of the OHC at a single academic hospital. Secondary outcome measures included percentage of patients taken to surgery within 24 or 48 hours, 30-day readmission rates, and mortality. Outcomes were compared to comanagement study results published in MEDLINE-indexed journals.
Results:
Patient cohort demographics and comorbidities were similar. Inpatient LOS was reduced by 1.6 days after implementation of the OHC (P = .01) without an increase in 30-day readmission rates or mortality. Time to surgery was insignificantly reduced from 27.4 to 21.9 hours (P = .27) and surgery within 48 hours increased from 86% to 96% (P = .15).
Discussion:
The OHC has improved efficiency of hip fracture management as judged by significant reductions in LOS with a trend toward reduced TTS at our institution.
Conclusion:
Orthopedic-hospitalist comanagement may represent an effective strategy to improve hip fracture management in the setting of a rapidly expanding patient population.
Keywords: hip fracture, hospitalist, comanagement, length of stay
Introduction
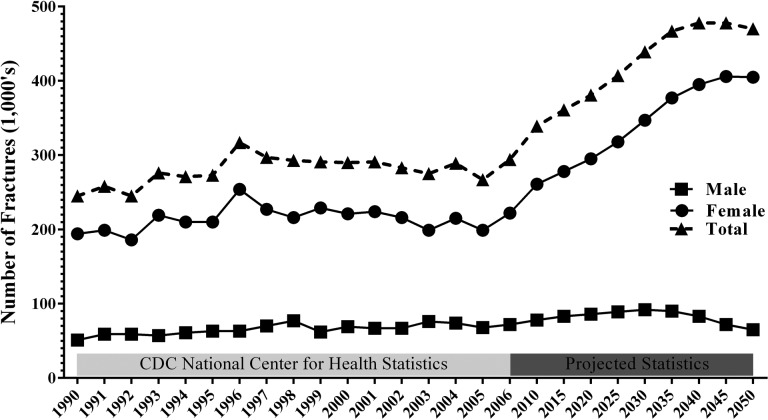
Hip fractures remain one of the most common injuries hospitalizing elderly patients and present significant morbidity and mortality in this age demographic. Worldwide, an estimated 1.6 million older adults sustain hip fractures each year, with 320 000 occurring in the United States alone.1 The annual cost of treating these injuries in the United States is an estimated US$9.2 billion in hospital costs, with overall costs in excess of US$20 billion.2-4 With an expanding geriatric population, overall costs may reach US$240 billion by the year 2040.5 Population growth models and analysis of past hip fracture trends6 predict hip fracture incidence to exceed 450 000 per year by 2040 (Figure 1). In order to accommodate this growing health-care burden, hospitals must modify clinical operations to minimize perioperative complications and improve efficiency of management.
Figure 1.
Hip fracture incidence by year. Analysis of past hip fracture incidence combined with population growth models predict hip fracture incidence to reach 450 000 by the year 2040. Data adapted from Brown et al.6
There are already attempts in place to streamline care in this enlarging subgroup of patients in order to maximize efficiency without sacrificing quality of care.7 Comanagement strategies combining orthopedic and medicine subspecialty services have received increasing attention as a means to improve hip fracture treatment in elderly patients. Admitting these patients to a service comanaged by orthopedic surgeons and general medicine, hospitalists, or geriatricians may optimize perioperative treatment of comorbidities and reduce inpatient length of stay (LOS) as well as patient morbidity and mortality.8 Some data suggest these programs may decrease the length of hospital stay in the hip fracture patient population.9 However, literature on the efficacy of these comanagement strategies for hip fracture patients has reported mixed results.3,10-16
At our institution, patients presenting with isolated hip fractures have traditionally been admitted to the general medicine service with orthopedic consultation for definitive surgical management. Review of administrative data found inpatient LOS for these patients to be unacceptably high, and as a result, a combined orthopedic-hospitalist comanaged (OHC) hip fracture service was implemented to reduce LOS and improve patient-centric value. The current investigation’s aim was to (1) identify the effects of a combined orthopedic-hospitalist service on hip fracture management by assessing inpatient LOS and time to surgery (TTS) as primary outcomes before and after implementation of the OHC at a single academic hospital and also (2) to review the existing hip fracture comanagement clinical practice models described in the literature, with comparisons to our own experience. We hypothesized that the OHC would effectively reduce LOS and TTS measures and improve hip fracture management.
Methods
The OHC service was launched at our institution with the goal of improving the management of adult hip fractures. Previously, patients presenting to the emergency department with a hip fracture were admitted to the general medicine service unless: (1) preexisting comorbidities, such as heart failure, dialysis, or advanced dementia necessitated admission to a medical subspecialty service or (2) concurrent polytrauma or developing pathology required intensive care unit (ICU)-level care. In all cases, orthopedics was consulted for definitive surgical management of the hip fracture. After implementation of the OHC service, these patients previously admitted to general medicine were now admitted to orthopedics under the care of an orthopedic surgeon and a hospitalist physician who both round on these patients daily. All medical comorbidities, evolving medical pathology on the floor and preoperative medical clearance are evaluated and managed by the hospitalist. The orthopedic team is responsible for surgical management and disposition planning. Both the hospitalist and orthopedist round on the patient daily to determine medical clearance, optimal timing of surgery, anticipate potential complications in the perioperative period, and facilitate appropriate discharge planning postoperatively. Consensus decisions are made through regular communication between providers starting at the time of consultation in the emergency department. Once cleared for surgery, patients are posted for surgery via a preexisting hip fracture protocol when the case request is made before 7 am of the operative day. This ensures the case is prioritized and will not be delayed by other emergent trauma that may come in the day of surgery.
The section on hospital medicine consists of 40 internal medicine trained faculty, 15 of whom share OHC service responsibilities. Of these 15 providers, 4 are geriatricians. All are well versed on the philosophy, goals, and responsibilities of the orthopedic and hospitalist services, which are clearly outlined in a detailed protocol distributed to all providers, which has a strong emphasis on regular communication directly between providers at the start of each day. Hospitalists attend a monthly lecture series addressing perioperative management of orthopedic patients. Several iterations of the standardized OHC protocol have been published. Protocols are continually revised by the clinical director of orthopedics and the section head of hospital medicine after concerns or deficiencies are identified in the model. The most recent version details the agreed service exclusion criteria for admission, the specific order sets to be used, required preoperative laboratory tests, and the individual steps of how to engage both services and obtain medical clearance. Service responsibilities are subdivided to specify who manages pain, deep vein thrombosis prophylaxis, rehabilitation, surgical site care, and blood transfusions (orthopedics) versus who manages perioperative risk calculation, medical comorbidities, calling subspecialty consults, treatment dose anticoagulation, and ordering daily laboratory tests (hospitalist). Discharge summaries are shared between services with medicine and orthopedic subsections for ease of documentation.
To identify changes in hip fracture management attributable to the OHC, a comparative cohort study of patients admitted before and after implementation of the OHC service was conducted using inpatient LOS as the primary outcome and TTS, 30-day readmission rates, and mortality as secondary outcomes. The retrospective arm of the study included hip fracture patients admitted to general medicine during the 10 months prior to OHC implementation, whereas the prospective arm of the study collected information on patients admitted to the OHC during the 10 months after service implementation. All patients admitted through the emergency department with a primary diagnosis of hip fracture were identified. To focus on the described geriatric hip fracture population, only patients 60 years and older were included in the study. High-energy trauma patients and patients requiring ICU level care for life-threatening conditions, dialysis, or subspecialty admission were also excluded from the study as these patients were never eligible for admission to a general medicine service or the OHC service. Patient cohort characteristics were compared by age, body mass index, gender, prior residence (home, assisted living facility, etc), The American Society of Anesthesiologists (ASA) classification, fracture type, operation type, anesthesia, and operative duration.
Time to surgery and LOS were calculated in hours measured from the time of arrival in the emergency department to the time of surgery and discharge, respectively. Measures were converted into whole days for comparison of LOS. For TTS and percentage of patients taken to surgery within 24 or 48 hours, metrics were maintained in hours. Medical record documentation of patient death was used to determine patient mortality as this is routinely updated in our medical record system based on patient attendance of postoperative visits, which are scheduled to 1 year postoperatively. Continuous variables are reported as the average ± standard error of the mean and were compared between groups using independent samples t test with an α = .05 to determine statistical significance. Categorical variables are reported as percentages and compared with Fisher exact tests. All study protocols and research methods were reviewed and approved by the institutional review board.
Results
During the 10 months prior to OHC implementation, 116 patients were admitted with a primary diagnosis of hip fracture. Of the 87 patients who met the inclusion criteria, 45 (52%) remained after applying exclusion criteria and were admitted to the general medicine service (mean age: 79.5 years; range: 60-102 years; 68% female). During the 10 months after OHC implementation, 172 patients were admitted with a primary diagnosis of hip fracture. Of the 116 patients who met the inclusion criteria, 54 (47%) remained after applying exclusion criteria and were admitted to the OHC service (mean age: 80.1 years; age range: 60-98 years; 71% female). Patients were most commonly excluded for high-energy trauma requiring admission to a trauma or ICU-level service and age <60 years. A number of patients met the inclusion criteria but were not admitted to the general medicine or OHC services. The most common reason for this was necessity of a medical subspecialty service. Patient with advanced dementia were commonly admitted to a specialized, closed geriatrics unit, and patients with renal failure, evolving sepsis, stroke, or cardiac pathology were admitted to their respective subspecialty services. Comparison of baseline demographics and comorbidities showed no difference between the retrospective general medicine group and the prospective OHC group (Table 1). Further analysis of operative parameters demonstrated no significant difference in ASA status, operative duration, estimated blood loss, fracture type, procedure type (arthroplasty or internal fixation), or anesthesia type (general or regional) between the general medicine group and the OHC group (Table 2).
Table 1.
Cohort Demographics and Comorbidities.
| General Medicine (n = 45) | Orthopedic-Hospitalist Comanagement (n = 54) | P Value | |
|---|---|---|---|
| Mean age (range) | 79.6 years (60-102) | 80.1 years (60-98) | .79 |
| Female | 68% | 71% | .82a |
| Body mass index | 24.37 ± 0.85 kg/m2 | 24.86 ± 0.80 kg/m2 | .68 |
| Race | .81a | ||
| White | 91% | 90% | |
| Black | 7% | 8% | |
| Hispanic | 2% | 0% | |
| Other | 0% | 2% | |
| Prior residence | .23a | ||
| Independent | 80% | 92% | |
| Assisted living | 4% | 2% | |
| Nursing facility | 16% | 6% | |
| Comorbidities | .43a | ||
| Coronary artery disease | 32% | 25% | |
| Diabetes | 20% | 25% | |
| Hypertension | 55% | 71% | |
| Hyperlipidemia | 25% | 14% | |
| COPD | 18% | 29% | |
| Atrial fibrillation | 16% | 20% | |
| Chronic kidney disease | 14% | 6% | |
| Congestive heart failure | 11% | 8% | |
| Osteoporosis (known) | 27% | 18% | |
| Hypothyroidism | 21% | 8% | |
Abbreviation: COPD, chronic obstructive pulmonary disease.
aFisher exact test.
Table 2.
Cohort Operative Parameters Comparison.
| General Medicine (n = 45) | Orthopedic-Hospitalist Comanagement (n = 54) | P Value | |
|---|---|---|---|
| ASA status | .19a | ||
| 2 | 11% | 2% | |
| 3 | 64% | 73% | |
| 4 | 25% | 25% | |
| Operative duration | 112 ± 7 minutes | 112 ± 8 minutes | .97 |
| Estimated blood loss | 217.8 ± 24.5 mL | 212.5 ± 21.3 mL | .87 |
| Fracture type | .96a | ||
| Intertrochanteric | 54% | 57% | |
| Femoral neck | 39% | 36% | |
| Subtrochanteric | 7% | 6% | |
| Procedure type | .64a | ||
| Arthroplasty | 27% | 23% | |
| Internal fixation | 73% | 77% | |
| Anesthesia type | .15a | ||
| General | 41% | 56% | |
| Regional | 59% | 44% | |
aFisher exact test.
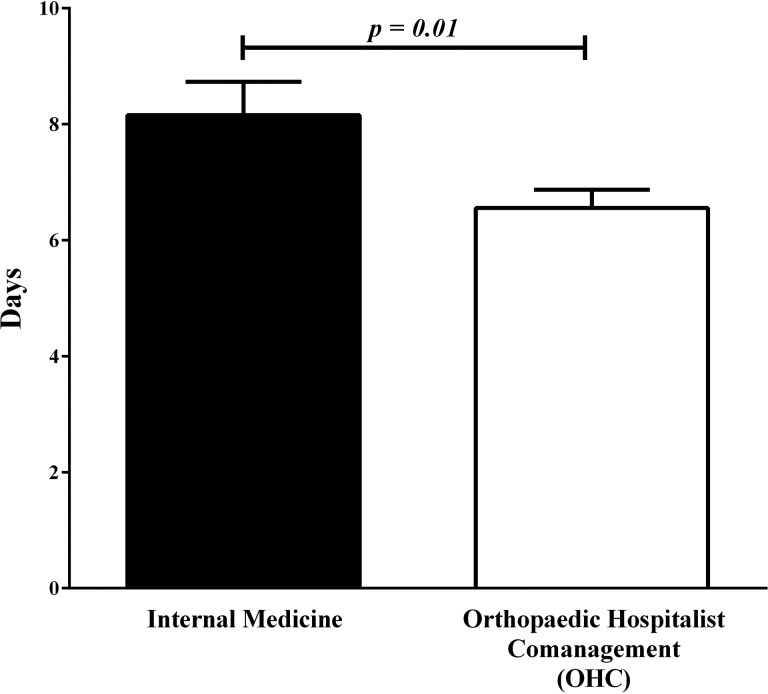
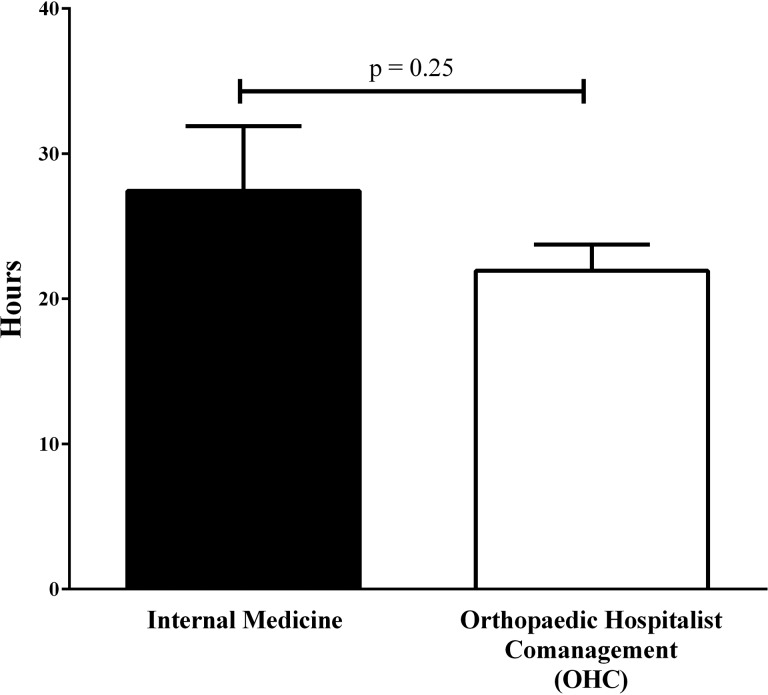
The average inpatient LOS on the general medicine service was 8.16 ± 0.56 days (range: 2.5-19.3 days), which decreased significantly to 6.56 ± 0.31 days (range: 2.7-11.9 days) after OHC implementation (P = .01; Figure 2). The average TTS for patients on the general medicine service was 27.43 ± 4.5 hours (range: 2.0-142.0 hours), which decreased to 21.94 ± 1.8 hours (range: 2.0-67.0 hours) after OHC implementation, but this difference was not significant (P = .25; Figure 3). Patients were taken to the operating room within 24 hours (P = 1.0) of presentation in similar number of cases between cohorts. More patients were taken to the operating room by 48 hours after OHC implementation, but this difference was also not significant (P = .15; Table 3). Thirty-day readmission rates (P = .72) and mortality rates (P = .80) did not differ when comparing patients admitted to general medicine against patients admitted to the OHC service (Table 3).
Figure 2.
Inpatient length of stay. Length of stay was measured in hours from the time of arrival to the emergency department until the time of discharge and converted to days. Values are reported as the mean ± standard error of the mean.
Figure 3.
Time to surgery. Time to surgery was measured in hours from the time of arrival to the emergency department until the time when surgery was started. Values are reported as the mean ± standard error of the mean.
Table 3.
Cohort Secondary Outcome Measures.
| General Medicine (n = 45) | Orthopedic-Hospitalist Comanagement (n = 54) | Fisher Test | |
|---|---|---|---|
| Surgery within 24 hours | 66% | 68% | P = 1.00 |
| Surgery within 48 hours | 86% | 96% | P = .15 |
| Mortality | P = .80 | ||
| In-house | 0% | 0% | |
| 90-day | 5% | 6% | |
| 12-month | 9% | 12% | |
| 30-day readmission rate | 6.8% | 10% | P = .72 |
Discussion
Our investigation compared hip fracture management before and after implementation of a combined OHC service. Our experience showed that the OHC service significantly reduced inpatient LOS by 1.6 days without an increase in readmission rates and demonstrated an insignificant decrease in TTS.
A number of studies have examined multidisciplinary care in hip fracture management, but few have specifically addressed OHC. In these models, emphasis is placed on collaboration, improving communication between treatment teams, and a protocol-driven practice to improve care and efficient utilization of resources.17 Phy et al reported on their experience with an orthopedic-hospitalist model at the Mayo Clinic14 where patients were previously triaged to a teaching medicine or orthopedic service, representing 23 different services. Under their new model, hip fracture patients were admitted to the teaching orthopedic surgery service comanaged by hospitalists. The authors reported a significant reduction in LOS (10.6 to 8.4 days) and TTS (38 hours to 25 hours), with significantly more patients going to surgery within 24 hours of presentation (47.5%-72.6%). Readmission rates decreased significantly as well. The authors attributed these successes to improved coordination of patient care and decreased variability in admission. Roy et al also documented improvements in hip fracture management after introduction of hospitalist-coordinated care to a community-based academic medical center.18 Median LOS was reduced from 6 to 5 days, and the percentage of patients taken to surgery within 24 hours of presentation improved significantly (11% vs 32%). They attributed the improvements to the increased availability of hospitalists to discuss treatment plans with patients and families.
The majority of recent hip fracture comanagement literature has been conducted under an orthopedic-geriatric model, and published results have shown mixed effects. Khan et al, Wagner et al, and Dy et al found no difference in LOS or TTS with orthogeriatric comanaged care.10,16,19 In Australia, Fisher et al followed one of the largest cohorts of hip fracture patients admitted to orthopedic-geriatric cocare and also reported no improvement to inpatient LOS in comparison to orthopedic-only care.11 However, they did find significant improvements in mortality, 6-month readmissions, and postoperative medical complications. They concluded that LOS does not accurately reflect quality of overall care and supported use of combined orthopedic-geriatric management. Most investigations however have found positive results with combined care. Earlier cohorts reported by Koval et al,20 Khasraghi et al,21 Vidan et al15 as well as more recent cohorts reported by Della Rocca et al3 and Leung et al all found improvements in inpatient LOS, TTS, and mortality with geriatric comanagement.
The University of Rochester has a well-documented longitudinal experience with orthopedic-geriatric care.12,22-24 Implementation of the Geriatric Fracture Center (GFC) in 2004 significantly reduced inpatient LOS, TTS, and medical complications, including infection.12 Recent study of their 758 patient GFC cohort reported a 4.3-day LOS, a 10.8% 30-day readmission rate, and a 24.1-hour average TTS.23 Success of the GFC is largely attributed to its founding principles, which focus on prioritizing early surgery, improving communication with comanagement partners, standardizing protocols, and early discharge planning.
Since introduction of our OHC model, an encouraging data point, although insignificant, is the reduced TTS and improvement in the proportion of patients taken to the operating room within 24 to 48 hours of presentation. A number of studies have identified early surgical intervention as a significant prognostic factor in outcomes for patients presenting with hip fractures.25-27 It was not feasible to accurately measure time to medical clearance in this investigation, but we believe that preoperative medical optimization has improved with the OHC, allowing us to expedite operative intervention. Having the patients admitted to the orthopedic floor provides access to physical therapists who routinely work exclusively with orthopedic patients and accelerate discharge planning. Our 30-day readmission rates remained stable and do not suggest that the reduction in LOS resulted from premature patient discharge. Previous reports estimate that hospital care represents 44% of the direct costs associated with hip fractures,22 with average inpatient hospitalization costs an estimated US$699/day.28 It is reasonable to assume that by reducing inpatient LOS by 1.6 days, we have significantly reduced inpatient cost of hip fracture care at our hospital. Admitting patients to a primary orthopedic service has also streamlined postoperative referrals to our outpatient fracture liaison service for management of bone health and prevention of fragility fractures.29 Although the downstream financial savings associated with early initiation of osteoporosis treatment is unclear, it is reasonable to assume that we can help prevent additional fragility fractures with early intervention.28
Our average inpatient LOS of 6.56 days remains above averages reported in a number of studies. One study reported the national average LOS at 6.2 days,5 whereas another study examining average inpatient LOS from the state of New York database Statewide Planning and Research Cooperative System (SPARCS) reported that LOS for hip fractures over an 11-year period dropped from 12.9 days in 2000 to 5.6 days by the end of 2011.30 We have noticed that one of the greatest barriers to expedite patient discharge at our facility has been arranging appropriate placement for patients requiring long-term advanced care with home health nursing or inpatient nursing facilities. Insurance processing and approval often may delay discharge by 2 to 3 days.
Several limitations exist in our study. We described our initial experience with hospitalist comanagement over a relatively short period of time with small sample sizes. Further study over a longer period of time will be necessary to fully investigate the effects of our OHC model. However, shorter study period may help minimize the effects of changes in faculty structure. Our faculty remained stable throughout the 20 months of our study. Studies conducted over longer periods cannot exclude effects of hiring more orthopedic trauma faculty on TTS and LOS. Our study design is somewhat limited by the large number of hip fractures that were excluded from the study. As a level 1 trauma center, a number of patient were excluded for polytrauma and life-threatening conditions present in addition to a hip fracture. These exclusions were necessary in order to focus on the geriatric population with fragility fractures, which still represent the majority of hip fractures we manage at our institution. A number of patients meeting initial inclusion criteria were ultimately excluded from the study because they required admission to medical subspecialty services. These patients would not have been eligible for OHC admission and in most cases had significantly longer LOS. This would have biased results and made comparison against the OHC cohort inappropriate. Finally, our study is constrained by the inherent limitations of retrospective study design with respect to the pre-OHC group.
Conclusion
Since the introduction of an OHC, we have significantly reduced hip fracture inpatient LOS by 1.6 days and seen more patients reaching the operating room within 24 to 48 hours of presentation. An OHC service may represent an effective health-care model to improve the efficiency of hip fracture treatment. Reducing LOS and TTS reduces inpatient costs, liberates resources to accommodate larger patient volumes, and may improve outcomes and patient satisfaction scores.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hung WW, Egol KA, Zuckerman JD, Siu AL. Hip fracture management: tailoring care for the older patient. JAMA. 2012;307(20):2185–2194. [DOI] [PubMed] [Google Scholar]
- 2. Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465–475. [DOI] [PubMed] [Google Scholar]
- 3. Della Rocca GJ, Moylan KC, Crist BD, Volgas DA, Stannard JP, Mehr DR. Comanagement of geriatric patients with hip fractures: a retrospective, controlled, cohort study. Geriatr Orthop Surg Rehabil. 2013;4(1):10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chuang CH, Pinkowsky GJ, Hollenbeak CS, Armstrong AD. Medicine versus orthopaedic service for hospital management of hip fractures. Clin Orthop Relat Res. 2010;468(8):2218–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kates SL, Blake D, Bingham KW, Kates OS, Mendelson DA, Friedman SM. Comparison of an organized geriatric fracture program to United States government data. Geriatr Orthop Surg Rehabil. 2010;1(1):15–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Brown CA, Starr AZ, Nunley JA. Analysis of past secular trends of hip fractures and predicted number in the future 2010-2050. J Orthop Trauma. 2012;26(2):117–122. [DOI] [PubMed] [Google Scholar]
- 7. Egol KA, Marcano AI, Lewis L, Tejwani NC, McLaurin TM, Davidovitch RI. Can the use of an evidence-based algorithm for the treatment of intertrochanteric fractures of the hip maintain quality at a reduced cost? Bone Joint J. 2014;96-B(9):1192–1197. [DOI] [PubMed] [Google Scholar]
- 8. Della Rocca GJ, Crist BD. Hip fracture protocols: what have we changed? Orthop Clin North Am. 2013;44(2):163–182. [DOI] [PubMed] [Google Scholar]
- 9. Suhm N, Kaelin R, Studer P, et al. Orthogeriatric care pathway: a prospective survey of impact on length of stay, mortality and institutionalisation. Arch Orthop Trauma Surg. 2014;134(9):1261–1269. [DOI] [PubMed] [Google Scholar]
- 10. Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM. Does a multidisciplinary team decrease complications in male patients with hip fractures? Clin Orthop Relat Res. 2011;469(7):1919–1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fisher AA, Davis MW, Rubenach SE, Sivakumaran S, Smith PN, Budge MM. Outcomes for older patients with hip fractures: the impact of orthopedic and geriatric medicine cocare. J Orthop Trauma. 2006;20(3):172–178; discussion 179-180. [DOI] [PubMed] [Google Scholar]
- 12. Friedman SM, Mendelson DA, Bingham KW, Kates SL. Impact of a comanaged Geriatric Fracture Center on short-term hip fracture outcomes. Arch Intern Med. 2009;169(18):1712–1717. [DOI] [PubMed] [Google Scholar]
- 13. Leung AH, Lam TP, Cheung WH, et al. An orthogeriatric collaborative intervention program for fragility fractures: a retrospective cohort study. J Trauma. 2011;71(5):1390–1394. [DOI] [PubMed] [Google Scholar]
- 14. Phy MP, Vanness DJ, Melton LJ, III, et al. Effects of a hospitalist model on elderly patients with hip fracture. Arch Intern Med. 2005;165(7):796–801. [DOI] [PubMed] [Google Scholar]
- 15. Vidan M, Serra JA, Moreno C, Riquelme G, Ortiz J. Efficacy of a comprehensive geriatric intervention in older patients hospitalized for hip fracture: a randomized, controlled trial. J Am Geriatr Soc. 2005;53(9):1476–1482. [DOI] [PubMed] [Google Scholar]
- 16. Wagner P, Fuentes P, Diaz A, et al. Comparison of complications and length of hospital stay between orthopedic and orthogeriatric treatment in elderly patients with a hip fracture. Geriatr Orthop Surg Rehabil. 2012;3(2):55–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mendelson DA, Friedman SM. Principles of comanagement and the geriatric fracture center. Clin Geriatr Med. 2014;30(2):183–189. [DOI] [PubMed] [Google Scholar]
- 18. Roy A, Heckman MG, Roy V. Associations between the hospitalist model of care and quality-of-care-related outcomes in patients undergoing hip fracture surgery. Mayo Clin Proc. 2006;81(1):28–31. [DOI] [PubMed] [Google Scholar]
- 19. Khan R, Fernandez C, Kashifl F, Shedden R, Diggory P. Combined orthogeriatric care in the management of hip fractures: a prospective study. Ann R Coll Surg Engl. 2002;84(2):122–124. [PMC free article] [PubMed] [Google Scholar]
- 20. Koval KJ, Chen AL, Aharonoff GB, Egol KA, Zuckerman JD. Clinical pathway for hip fractures in the elderly: the Hospital for Joint Diseases experience. Clin Orthop Relat Res. 2004(425):72–81. [DOI] [PubMed] [Google Scholar]
- 21. Khasraghi FA, Christmas C, Lee EJ, Mears SC, Wenz JF., Sr Effectiveness of a multidisciplinary team approach to hip fracture management. J Surg Orthop Adv. 2005;14(1):27–31. [PubMed] [Google Scholar]
- 22. Friedman SM, Mendelson DA, Kates SL, McCann RM. Geriatric co-management of proximal femur fractures: total quality management and protocol-driven care result in better outcomes for a frail patient population. J Am Geriatr Soc. 2008;56(7):1349–1356. [DOI] [PubMed] [Google Scholar]
- 23. Kates SL, Mendelson DA, Friedman SM. Co-managed care for fragility hip fractures (Rochester model). Osteoporos Int. 2010;21(suppl 4):S621–S625. [DOI] [PubMed] [Google Scholar]
- 24. Kates SL, Mendelson DA, Friedman SM. The value of an organized fracture program for the elderly: early results. J Orthop Trauma. 2011;25(4):233–237. [DOI] [PubMed] [Google Scholar]
- 25. Gdalevich M, Cohen D, Yosef D, Tauber C. Morbidity and mortality after hip fracture: the impact of operative delay. Arch Orthop Trauma Surg. 2004;124(5):334–340. [DOI] [PubMed] [Google Scholar]
- 26. Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738–1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7(10):e46175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Swart E, Vasudeva E, Makhni EC, Macaulay W, Bozic KJ. Dedicated perioperative hip fracture comanagement programs are cost-effective in high-volume centers: an economic analysis. Clin Orthop Relat Res. 2016;474(1):222–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Miller AN, Lake AF, Emory CL. Establishing a fracture liaison service: an orthopaedic approach. J Bone Joint Surg. 2015;97(8):675–681. [DOI] [PubMed] [Google Scholar]
- 30. Nikkel LE, Kates SL, Schreck M, Maceroli M, Mahmood B, Elfar JC. Length of hospital stay after hip fracture and risk of early mortality after discharge in New York state: retrospective cohort study. BMJ. 2015;351:h6246. [DOI] [PMC free article] [PubMed] [Google Scholar]