Abstract
The objective of this review was to assess the effectiveness of intrapartum ultrasonography in measuring cervical dilatation, head station and position. Electronic literature searches were carried out of MEDLINE, CINAHL, and Web of Knowledge, plus manual reference list checks of all relevant articles. All published prospective studies comparing intrapartum ultrasonography with digital VE in the determination of cervical dilatation, head station and position were then evaluated for the success rate and level of agreement between ultrasonography and digital VE. Ultrasonography had higher success rate than digital VE in the determination of fetal head position, with a statistically significant difference in the first stage of labour. Second, although the successful determination of cervical dilatation was in favour of digital VE, the difference was not statistically significant. In addition, there was high agreement between ultrasound and digital VE findings on cervical dilatation. Lastly, a significant but moderate correlation between digital VE and ultrasound methods was found in the assessment of fetal head station. However, no meta-analysis could be done for the fetal head station due to the methodological differences between ultrasound anatomical landmarks and that of digital VE. The findings suggest that ultrasonography is superior to digital VE in the assessment of fetal head position, but has moderate correlation with digital VE in the assessment of head station. It also showed high agreement with digital VE in the assessment of cervical dilatation with no statistically significant difference in terms of success rate.
Keywords: Intrapartum, ultrasonography, digital VE, cervical dilatation, head station, position
Introduction
Rationale
The role of digital vaginal examination (digital VE) in the assessment of labour progress includes measuring the cervical dilatation, head station and position. Not only is the procedure highly subjective,1 but it has also been described by mothers in labour as painful and posing risk of infection.2 It has been suggested that ultrasonography could become a useful and more objective imaging technique for monitoring labour in future,3 with the potential of minimising risk of infection and discomfort to the mother.
A systematic review was therefore conducted to evaluate published studies on the effectiveness of ultrasonography in assessing cervical dilatation, head station and position during labour.
Objective
The primary objective was to assess the success rate of ultrasonography in the determination of cervical dilatation and position in comparison to digital VE. The secondary objective was to evaluate the level of agreement or correlation between ultrasonography and digital VE in the measurement of cervical dilatation, head station and position.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) is the structure used for this systematic review.4
Protocol and registration
The general methods of the review and inclusion criteria were specified in advance. However, there was no registration of the review.
Eligibility criteria
Every type of primary study was eligible for inclusion, whether observational or randomised control trial. The selected study must have reported on the relationship between ultrasonography and digital VE in the measurement of either one or more of the following: cervical dilatation, head station or position. There were no language and date restrictions in the search process.
Information sources
Papers included in the review were obtained from electronic searches of the following databases: PubMed (MEDLINE), CINAHL and Web of Knowledge, all of which reference international journal citations for biomedical literature. It has been demonstrated that using two or more databases will identify a greater percentage of available citations;5,6 hence, the search was conducted in more than one database. In addition, there was a review of all reference lists of included studies for relevant papers that were not picked up through electronic search, as it was recognised that despite the advantages of electronic databases, they are not infallible.7
Search
The search strategy included the breaking down of the research question into component parts, for easy identification of the Population, Intervention, Comparator and Outcomes (PICO), as described by Sayers.8 Breaking down of the research question into a PICO framework was helpful in the choice of search-terms or key words for effective search. An electronic search of subject-specific databases was then used in identifying relevant articles in PubMed, Web of Knowledge and CINAHL.
The key search terms were reasonably combined in different sets of combinations, using Boolean operators ‘AND’ and ‘OR’, and truncations as appropriate. In total, nine steps of combined searches were made in PubMed, Web of Knowledge, and CINAHL on 4 and 5 November 2015. Table 1 shows the nine steps of the search conducted in PubMed.
Table 1.
The nine steps of the PubMed Search
| Search Number | Terms | Results |
|---|---|---|
| S1 | transperineal (ultraso* OR sonog*) AND clinical examination in labour | 32 |
| S2 | transperineal (ultraso* OR sonog*) AND digital examination in labour | 23 |
| S3 | transabdominal (ultraso* OR sonog*) AND clinical examination in labour | 38 |
| S4 | transabdominal (ultraso* OR sonog*) AND digital examination in labour | 24 |
| S5 | Intrapartum (ultraso* OR sonog*) AND rotation | 10 |
| S6 | Intrapartum (ultraso* OR sonog*) AND position | 48 |
| S7 | Intrapartum (ultraso* OR sonog*) AND station | 18 |
| S8 | Intrapartum (ultraso* OR sonog*) AND head descent | 11 |
| S9 | Intrapartum (ultraso* OR sonog*) AND cervical dilatation | 48 |
Study selection
Records identified through database searching were exported into the EndNote citation manager. After the removal of duplicates, articles were then screened by title and abstract to determine their relevance to the research question. The primary selection criteria for all papers were whether their results had reported on the relationship between ultrasonography and digital VE in measuring cervical dilatation, head station or position. The minimum patient selection criteria for all studies were pregnant women in labour with indication for digital VE for measuring either cervical dilatation, fetal head station or position. In some cases, all three parameters were assessed in one study. The full-text versions of all papers meeting the primary selection criteria were obtained for further evaluation.
Data collection process
Relevant data from all selected papers were entered into a data extraction sheet. The PRISMA diagram (Figure 1) explains the data collection process and the quantity of papers identified by the search.
Figure 1.
PRISMA flow diagram.
Data items
Information extracted from all studies included the following: author, year of publication, country of origin, clinical setting, sample size, study design, statistical method and results.
Risk of bias in individual studies
In determining the risk of bias, it was assessed whether there was blinding of the two examiners performing the ultrasound examination and the digital VE.
Data synthesis
Synthesis took a narrative approach using some of the techniques described by Popay et al.,9 including textual descriptions, tabulations and transformation of data into common rubric. Studies were classified and combined in the analysis in accordance with the type of outcome measured, which included the cervical dilatation group, head station group and head position group. Homogeneous groups of studies were entered into the RevMan 5.3 review manager, to construct forest plots for each classified group. Forest plots were analysed with the Mantel-Haenszel statistical method.
Risk of bias across studies
The model of analysis was performed using the random effect rather than fixed effect with the assumption that there were some degrees of difference even among homogeneous groups of studies. This was considered in order to minimise the impact of selection bias, sample size, detection bias and other potential sources of bias, as was evident of true effect between studies in performing the meta-analysis (P < 0.05).
Results
Study selection
A total of 657 articles were identified through database searching as described, including PubMed, Web of Knowledge and CINAHL. The 657 articles were exported into the citation manager (EndNote), and duplicates were manually removed. Two additional papers were identified by manual search of reference lists. The number of articles remaining for further screening by title and abstract was 215. The number of relevant articles for full text screening was 46, and 31 articles were found to be eligible for inclusion in the systematic review (see Figure 1).
Study characteristics
Table 2 shows study characteristics of articles included in the review. Thirty-one primary studies published between 2001 and 2015 met the eligibility criteria for inclusion in this review. Approximately 53% of these studies originated from Europe, 23% from Asia, 15% from North America, 6% from Africa, and 3% from Australia.
Table 2.
Study characteristics
| Author | Country | Examination | Labour stage | Sample Size | Study design |
|---|---|---|---|---|---|
| Akmal et al.10 | UK | Position | Second | 64 | Observational |
| Akmal et al.11 | UK | Position | First | 496 | Observational |
| Barbera et al.12 | USA & Italy | Station | First | 88 | Observational |
| Benediktsdottir et al.13 | Sweden | Dilatation | First | 86 | Observational |
| Chan et al .14 | China | Station | First | 100 | Observational |
| Chou et al .15 | USA | Position | Second | 88 | Observational |
| Dietz et al.16 | Australia | Station | First | 139 | Observational |
| Dimmasi et al.17 | Tunisia | Station | First | 100 | Observational |
| Dupuis et al.18 | France | Position | Second | 110 | Observational |
| Eggebo et al.19 | UK & Norway | Position | First | 150 | Observational |
| Ghi et al.20 | Italy | Station | First | 60 | Observational |
| Gilboa et al.21 | Israel | Station | First | 65 | Observational |
| Hassan et al.22 | UK & Norway | Position, Station, Dilatation | First | 20 | Observational |
| Hassan et al.23 | UK & Norway | Dilatation | First | 21 | Observational |
| Hidar et al.24 | Tunisia | Position | First | 350 | Observational |
| Kawabata et al.25 | Japan | Position | First | 87 | Observational |
| Kreiser et al.26 | Israel | Position | Second | 44 | Observational |
| Maticot-Baptista et al.27 | France | Station | First | 45 | Observational |
| Molina et al.28 | UK | Station | First | 50 | Observational |
| Rivaux et al.29 | France | Station | First | 100 | Observational |
| Sherer et al (2002a)30 | USA | Position | First | 102 | Observational |
| Sherer et al (2002b)31 | USA | Position | Second | 112 | Observational |
| Sherer et al.32 | USA | Station | First | 222 | Observational |
| Shetty et al.33 | India | Position | First | 165 | Observational |
| Souka et al.34 | Greece | Position | Second | 148 | Observational |
| Tutschek et al.35 | Norway | Station | First | 106 | Observational |
| Tutschek et al.36 | Switzerland | Station | First | 50 | Observational |
| Youssef et al.37 | Italy | Station | First | 47 | Observational |
| Yuce et al.38 | Turkey | Position, Station, Dilatation | First | 43 | Observational |
| Zahalka et al.39 | Israel | Position | First | 60 | Observational |
| Zimerman et al.40 | Israel | Dilatation | First | 52 | Observational |
| Totals: 31 | 3370 |
The total sample population of birthing women who participated in these primary studies was 3370, with 47% of them from a European tertiary setting, about 18% of them in an Asian tertiary setting, 17% of them in the USA, 14% in a North African country and 4% in an Australian tertiary clinical setting.
The 31 studies were all observational with a wide range of sample sizes, the smallest sample size being 20 subjects, and the largest sample size being 496 subjects.
Risk of bias within studies
The various forest plots revealed a high percentage of heterogeneity amongst the classified group of studies. As a result, risk ratio was used for the forest plots rather than odd ratios.
Results of individual studies
Fetal head position
It was noted that in 13 out of the 15 studies (87%) that reported on fetal head position, accuracy of digital VE was defined within a range of ±45° agreement limit. Other studies in the minority have used different ranges of agreement limit (other than the 45°) with one study using 60°,39 and another using 180°.24 A zero degree agreement limit, for instance, is an absolute agreement with no provision for any margin of error. In one study, the range of agreement limit was unclear.17 Those isolated studies were therefore excluded from forest plots to minimise the impact of heterogeneity. As the ±45° range of agreement was the widely accepted one, only those studies using that range were included in the statistical analysis. Also, findings on the first stage of labour were analysed separately from the second stage of labour (see Tables 3 and 4).
Table 3.
Agreement between ultrasound and digital VE on head position at the first stage of labour
| Author | Statistical method | Ultrasound – Digital VE agreement |
|---|---|---|
| Hassan et al.22 | Simple percentage agreement plus average mean difference with Bland–Altman plots | 39%; MD: −3.9° |
| Sherer et al.30 | Cohen’s Kappa analysis | 47% |
| Akmal et al.11 | Simple percentage agreement | 49% |
| Souka et al.34 | Cohen’s Kappa analysis | 31% |
| Kawabata et al.25 | Simple percentage agreement | 40% |
| Shetty et al.33 | Cohen’s Kappa analysis | 32% |
| Eggebo et al.41 | Cohen’s Kappa analysis | 32% |
| Yuce et al.38 | Simple percentage agreement | 24% |
Table 4.
Agreement between ultrasound and digital VE on head position at the second stage of labour
| Author | Statistical method | Ultrasound – Digital VE agreement |
|---|---|---|
| Kreiser et al.26 | Simple percentage agreement | 70% |
| Sherer et al.31 | Cohen’s Kappa analysis | 61% |
| Akmal et al.10 | Simple percentage agreement | 73% |
| Chou et al.15 | Simple percentage agreement | 72% |
| Souka et al.34 | Cohen’s Kappa analysis | 65% |
| Dupuis et al. 18 | Cohen’s Kappa analysis | 80% |
| Zahalka et al.39 | Simple percentage agreement | 79% |
Figure 2 shows the forest plot of eight studies on ultrasound versus digital VE in assessing fetal head position in the first stage of labour. For the second stage of labour, six studies qualified for inclusion in the meta-analysis as shown in the forest plot of Figure 3.
Figure 2.
Forest plot in favour of ultrasonography on the success rate of fetal head position determination in the first stage of labour.
Figure 3.
Forest plot in favour of ultrasonography on the success rate of fetal head position determination in the second stage of labour.
Cervical dilatation
The forest plot of Figure 4 shows statistically insignificant difference between the success rate of digital VE and that of ultrasound. Again, the high level of agreement reported by the five studies is presented in Table 5.
Figure 4.
Forest plot in favour of digital VE over ultrasonography on the success rate of the determination of cervical dilatation.
Table 5.
Results of individual studies on cervical dilatation
| Author | Statistical Method | Agreement between ultrasound and digital VE |
|---|---|---|
| Benediktsdottir et al.13 | linear regression | r2 = 0.72 |
| Hassan et al.22 | linear regression | r2 = 0.68 |
| Hassan et al.23 | Pearson correlation coefficient | r = 0.82 |
| Yuce et al.38 | Pearson correlation coefficient | r = 0.82 |
| Zimerman et al.40 | Simple linear regression | r2 = 0.61 |
Fetal head station
Of the 31 studies included in this review, 14 reported the relationship between ultrasonography and digital VE in assessing the station, with seven different ultrasound methods for measuring fetal head station described. However, forest plots could not be constructed because different landmarks and measurement methods were used for ultrasound and digital VE in determining fetal head station. These seven ultrasound methods demonstrated various levels of relationship with digital VE, which uses the ischial spines as the reference landmark. The ultrasound methods described by the 14 studies include:
Angle of Progression, which is also known as the Angle of Descent12,14,36
Head Symphysis Distance37
Ultrasound Fetal Head Engagement32 and
However, the widely used methods were the Angle of progression (AoP) and the Head perineum distance (HPD).
The angle of progression method
Results on the effectiveness of ultrasonography in relation to digital VE all showed moderate correlation with station.12,14,36 These studies had all included multiparous and nulliparous women at different stages of active labour in their study population.
Head perineum distance
Chan et al.,14 Hassan et al.22 and Yuce et al.38 have all reported moderate correlation between digital VE and the HPD. Also, Dimassi et al.,17 Maticot-Baptista et al.27 and Rivaux et al.29 all reported on the diagnostic value of the distance from the head to the perineum in diagnosing fetal head engagement using digital VE as the comparator. Dimassi et al.17 reported sensitivity and specificity of 86.7% and 94.1%, respectively, for diagnosing fetal head engagement, using a distance of 55 mm from the fetal head to the perineum as their predictive value.
Maticot-Baptista et al.27 also obtained a sensitivity of 97.8% in predicting fetal head engagement, using a distance of <60 mm from the fetal head to the perineum. Maticot-Baptista et al.27 added that whenever a distance of more than 60 mm was obtained, digital VE diagnosed fetal head as ‘non-engaged’ with a specificity of 89.0%. Likewise, Rivaux et al.29 reported that the fetal head was not engaged upon digital VE assessment whenever ultrasound recorded a mean distance of 66.4 mm (±7.53 mm) from the fetal head to the perineum.
Discussion
The general results of this systematic review suggest that ultrasonography could be as effective as the conventional digital VE for assessing cervical dilatation, head station and position. However, its applicability in the wider non-tertiary settings and the general population remain unclear, as studies have largely been limited to tertiary settings. It will therefore be worth investigating its applicability in the general non-tertiary clinical settings, including developing country settings.
In assessing fetal head position in labour, findings indicate that in comparison to ultrasound, digital VE is less successful in the first stage than the second stage. The level of agreement with ultrasound doubles in the second stage from approximately 35% in the first stage to 70% in the second stage. This suggests that ultrasonography is a better option than digital VE for assessing fetal head position, using the transabdominal scanning approach. It is also worth noting that the average accuracy level was slightly higher for digital VE in studies that use simple percentage agreement statistics rather than kappa, which does not account for agreement by chance.42 Given that slightly lower agreement values were obtained by digital VE in studies analysed with kappa, it can be assumed that the accuracy level of ultrasound in the second stage of labour may also be slightly lower than the over 90% reported by Chou et al.14 and Kreiser et al.,25since these were analysed with simple percentage agreement rather than by kappa statistics.
In the ultrasound measurement of cervical dilatation, there was consensus among studies on the use of the transperineal scanning approach rather than the transvaginal, with measurements obtainable in both transverse and vertical planes (see the transverse and anterior-posterior measurement options demonstrated in Figure 5).This may give ultrasound an edge over digital VE if its effectiveness is explored further, since that may provide mothers with a non-invasive option for measuring cervical dilatation, especially in cases where the risk of infection transfer is a major concern.
Figure 5.
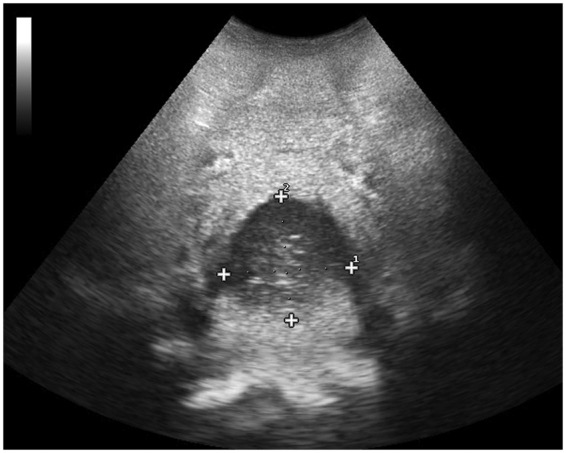
Cervical dilatation measurement.
However, some of the included studies had very low sample sizes, and the effect of labour characteristics on the success rate is generally unclear. For example, the extent to which success rate is affected by ruptured or unruptured membrane, latent versus active phase, could not be assessed extensively because of low sample size.
Lastly, although several methods for assessing the fetal head station have been found, the widely reported methods are the AoP and the HPD. The AoP is described as an angle formed by a line drawn through the long axis of the pubic symphysis and another tangential line drawn from the leading edge of the fetal head cranium (see Figure 6). The HPD also refers to the shortest obtainable distance from the leading edge of the fetal head cranium to the skin surface of the perineum (see Figure 7). Their level of correlation with digital VE on station was reported by the individual studies as moderate but statistically significant. Given that the digital VE itself is known to be subjective, the possible advantage ultrasound may have is that, since it has more than one measurement method, a high level of agreement amongst the ultrasound methods may indicate reliability for users. Future studies could therefore concentrate on exploring the level of agreement between these ultrasound methods.
Figure 6.
The angle of progression measurement.
Figure 7.
Head perineum distance measurement.
Conclusion
Findings suggest that ultrasonography is superior to digital VE in the assessment of fetal head position with a statistically significant difference in success rate in favour of ultrasound in the first stage of labour.
Second, there is no statistically significant difference between the success rate of ultrasound and digital VE in the determination of cervical dilatation. And again, there is high level of agreement on cervical dilatation between the two methods.
Lastly, whilst primary studies were in agreement on a significant but moderate correlation between ultrasound and digital VE in the assessment of fetal head station, a comparison of their success rate could not be determined.
Recommendations
Future studies could extend to non-tertiary settings in a much more representative general population of women in labour, including developing country settings.
Although findings suggest no statistically significant difference in success rate between ultrasound and Digital VE on cervical dilatation, future studies should target larger sample sizes to enable detailed evaluation of possible influencing factors of success rate.
Again, assessing the specificity and sensitivity of ultrasonography in diagnosing active labour would add in-depth knowledge on its effectiveness. This could be defined by using a ≥4 cm threshold of cervical dilatation determined by digital VE.
Lastly, although ultrasound is highly recommended over digital VE in the assessment of fetal head position, future studies could evaluate the effectiveness further, using a much more robust statistical method.
Acknowledgements
The authors are grateful to Ms Ann C. Polin MSc, RDMS, RDCS, RVT who helped with getting the full articles of some of the papers in the review.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: This article forms part of the systematic review chapter submitted by the first author for his PhD thesis at the University of Derby.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval
Not applicable
Guarantor
BW
Contributorship
YAW researched literature and conceived the study. YAW, BW, HV designed the search strategy. YAW, BW did the data analysis. YAW wrote the first draft of the manuscript. BW, HV reviewed the first draft. EKN reviewed and validated the meta-analysis. YAW wrote the final version of the manuscript. All authors reviewed and approved the final version of the manuscript.
References
- 1.Buchmann E, Libhaber E. Interobserver agreement in intrapartum estimation of fetal head station. Int J Gynaecol Obstet 2008; 101: 285–289. [DOI] [PubMed] [Google Scholar]
- 2.Dixon L and Foureur M. The vaginal examination during labour. Is it of benefit or harm? In 11th International Conference on Control, Automation, Robotics and Visions. New Zealand College of Midwives (ICARCV) 2010.
- 3.Eggebo TM. Ultrasound is the future diagnostic tool in active labor. Ultrasound Obstet Gynecol 2013; 41: 361–363. [DOI] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151: 264–269. [DOI] [PubMed] [Google Scholar]
- 5.Wilkins T, Gillies RA, Davies K. EMBASE versus MEDLINE for family medicine searches: can MEDLINE searches find the forest or a tree? Can Fam Phys 2005; 51: 848–849. [PMC free article] [PubMed] [Google Scholar]
- 6.Lawrence DW. What is lost when searching only one literature database for articles relevant to injury prevention and safety promotion? Injury Prevent 2008; 14: 401–404. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong R, Jackson N, Doyle J, et al. It’s in your hands: the value of handsearching in conducting systematic reviews of public health interventions. J Public Health 2005; 27: 388–391. [DOI] [PubMed] [Google Scholar]
- 8.Sayers A. Tips and tricks in performing a systematic review. Br J Gen Pract 2008; 58: 136–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme. Version 1, https://www.researchgate.net/publication/233866356 (2006, accessed 07 September 2016).
- 10.Akmal S, Kametas N, Tsoi E, et al. Comparison of transvaginal digital examination with intrapartum sonography to determine fetal head position before instrumental delivery. Ultrasound Obstet Gynecol 2003; 21: 437–440. [DOI] [PubMed] [Google Scholar]
- 11.Akmal S, Tsoi E, Kametas N, et al. Intrapartum sonography to determine fetal head position. J Matern Fetal Neonatal Med 2002; 12: 172–177. [DOI] [PubMed] [Google Scholar]
- 12.Barbera AF, Pombar X, Perugino G, et al. A new method to assess fetal head descent in labor with transperineal ultrasound. Ultrasound Obstet Gynecol 2009; 33: 313–319. [DOI] [PubMed] [Google Scholar]
- 13.Benediktsdottir S, Eggebø TM, Salvesen KÅ. Agreement between transperineal ultrasound measurements and digital examinations of cervical dilatation during labor. BMC Preg Childbirth 2015; 15: 273–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chan YT, Ng VK, Yung WK, et al. Relationship between intrapartum transperineal ultrasound measurement of angle of progression and head-perineum distance with correlation to conventional clinical parameters of labor progress and time to delivery. J Matern Fetal Neonatal Med 2015; 28: 1476–1481. [DOI] [PubMed] [Google Scholar]
- 15.Chou MR, Kreiser D, Taslimi MM, et al. Vaginal versus ultrasound examination of fetal occiput position during the second stage of labor. Am J Obstet Gynecol 2004; 191: 521–524. [DOI] [PubMed] [Google Scholar]
- 16.Dietz HP, Lanzarone V. Measuring engagement of the fetal head: validity and reproducibility of a new ultrasound technique. Ultrasound Obstet Gynecol 2005; 25: 165–168. [DOI] [PubMed] [Google Scholar]
- 17.Dimassi K, Ben Amor A, Belghith C, et al. Ultrasound diagnosis of fetal head engagement. Int J Gynecol Obstet 2014; 127: 6–9. [DOI] [PubMed] [Google Scholar]
- 18.Dupuis O, Ruimark S, Corinne D, et al. Fetal head position during the second stage of labor: comparison of digital vaginal examination and transabdominal ultrasonographic examination. Eur J Obstet Gynecol Reprod Biol 2005; 123: 193–197. [DOI] [PubMed] [Google Scholar]
- 19.Eggebo TM, Hassan WA, Salvesen KA, et al. Sonographic prediction of vaginal delivery in prolonged labor: a two-center study. Ultrasound Obstet Gynecol 2014; 43: 195–201. [DOI] [PubMed] [Google Scholar]
- 20.Ghi T, Farina A, Pedrazzi A, et al. Diagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasound. Ultrasound Obstet Gynecol 2009; 33: 331–336. [DOI] [PubMed] [Google Scholar]
- 21.Gilboa Y, Kivilevitch Z, Spira M, et al. Head progression distance in prolonged second stage of labor: relationship with mode of delivery and fetal head station. Ultrasound Obstet Gynecol 2013; 41: 436–441. [DOI] [PubMed] [Google Scholar]
- 22.Hassan WA, Eggebo T, Ferguson M, et al. The sonopartogram: a novel method for recording progress of labor by ultrasound. Ultrasound Obstet Gynecol 2014; 43: 189–194. [DOI] [PubMed] [Google Scholar]
- 23.Hassan WA, Eggebo TM, Ferguson M, et al. Simple two-dimensional ultrasound technique to assess intrapartum cervical dilatation: a pilot study. Ultrasound Obstet Gynecol 2013; 41: 413–418. [DOI] [PubMed] [Google Scholar]
- 24.Hidar S, Choukou A, Jerbi M, et al. Clinical and sonographic diagnosis of occiput posterior position: a prospective study of 350 deliveries. Gynecol Obstet Fertil 2006; 34: 484–488. [DOI] [PubMed] [Google Scholar]
- 25.Kawabata I, Nagase A, Oya A, et al. Factors influencing the accuracy of digital examination for determining fetal head position during the first stage of labor. J Nippon Med School 2010; 77: 290–295. [DOI] [PubMed] [Google Scholar]
- 26.Kreiser D, Schiff E, Lipitz S, et al. Determination of fetal occiput position by ultrasound during the second stage of labor. J Matern Fetal Med 2001; 10: 283–286. [DOI] [PubMed] [Google Scholar]
- 27.Maticot-Baptista D, Ramanah R, Collin A, et al. Ultrasound in the diagnosis of fetal head engagement. A preliminary French prospective study. J Gynecol Obstet Biolog Reprod 2009; 38: 474–480. [DOI] [PubMed] [Google Scholar]
- 28.Molina FS, Terra R, Carrillo MP, et al. What is the most reliable ultrasound parameter for assessment of fetal head descent? Ultrasound Obstet Gynecol 2010; 36: 493–499. [DOI] [PubMed] [Google Scholar]
- 29.Rivaux G, Dedet B, Delarue E, et al. The diagnosis of fetal head engagement: Transperineal ultrasound, a new useful tool? Gynecologie Obstetrique Fertilite 2012; 40: 148–152. [DOI] [PubMed] [Google Scholar]
- 30.Sherer DM, Miodovnik M, Bradley KS, et al. Intrapartum fetal head position I: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the active stage of labor. Ultrasound Obstet Gynecol 2002; 19: 258–263. [DOI] [PubMed] [Google Scholar]
- 31.Sherer DM, Miodovnik M, Bradley KS, et al. Intrapartum fetal head position II: comparison between transvaginal digital examination and transabdominal ultrasound assessment during the second stage of labor. Ultrasound Obstet Gynecol 2002; 19: 264–268. [DOI] [PubMed] [Google Scholar]
- 32.Sherer DM, Abulafia O. Intrapartum assessment of fetal head engagement: comparison between transvaginal digital and transabdominal ultrasound determinations. Ultrasound Obstet Gynecol 2003; 21: 430–436. [DOI] [PubMed] [Google Scholar]
- 33.Shetty J, Aahir V, Pandey D, et al. Fetal head position during the first stage of labor: comparison between vaginal examination and transabdominal ultrasound. ISRN Obstet Gynecol 2014; 2014: 314617–314617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Souka AP, Haritos T, Basayiannis K, et al. Intrapartum ultrasound for the examination of the fetal head position in normal and obstructed labor. J Matern Fetal Neonatal Med 2003; 13: 59–63. [DOI] [PubMed] [Google Scholar]
- 35.Tutschek B, Torkildsen EA, Eggebo TM. Comparison between ultrasound parameters and clinical examination to assess fetal head station in labor. Ultrasound Obstet Gynecol 2013; 41: 425–429. [DOI] [PubMed] [Google Scholar]
- 36.Tutschek B, Braun T, Chantraine F, et al. A study of progress of labour using intrapartum translabial ultrasound, assessing head station, direction, and angle of descent. BJOG 2011; 118: 62–69. [DOI] [PubMed] [Google Scholar]
- 37.Youssef A, Maroni E, Ragusa A, et al. Fetal head-symphysis distance: a simple and reliable ultrasound index of fetal head station in labor. Ultrasound Obstet Gynecol 2013; 41: 419–424. [DOI] [PubMed] [Google Scholar]
- 38.Yuce T, Kalafat E, Koc A. Transperineal ultrasonography for labor management: accuracy and reliability. Acta obstetricia et gynecologica Scandinavica 2015; 94: 760–765. [DOI] [PubMed] [Google Scholar]
- 39.Zahalka N, Sadan O, Malinger G, et al. Comparison of transvaginal sonography with digital examination and transabdominal sonography for the determination of fetal head position in the second stage of labor. Am J Obstet Gynecol 2005; 193: 381–386. [DOI] [PubMed] [Google Scholar]
- 40.Zimerman AL, Smolin A, Maymon R, et al. Intrapartum measurement of cervical dilatation using translabial 3-dimensional ultrasonography correlation with digital examination and interobserver and intraobserver agreement assessment. J Ultrasound Med 2009; 28: 1289–1296. [DOI] [PubMed] [Google Scholar]
- 41.Eggebo TM, Hassan WA, Salvesen KA, et al. Prediction of delivery mode with ultrasound assessed fetal position in nulliparous women with prolonged first stage of labor. Ultrasound Obstet Gynecol 2015; 46: 606–610. [DOI] [PubMed] [Google Scholar]
- 42.Carletta J. Assessing agreement on classification tasks: the kappa statistic. Computat Linguist 1996; 22: 249–254. [Google Scholar]








