Abstract
To advance the area of phenomenology of voices and their interrelatedness to forms of delusions this study investigated the prevalence and interrelatedness of co-occurring auditory verbal hallucinations (AVHs) and delusions. Additionally we explored the characterization of distinct sub-categories/clusters of AVHs and delusions. Ninety-two participants experiencing psychosis were administered standardized clinical measures. We found a significant diagnostic difference with increased prevalence of co-occurring AVHs and delusions within the schizophrenia group compared to the bipolar with psychosis group. Regardless of diagnosis, there was a significant positive correlation between AVHs and delusions of reference, persecution, control, thought insertion, thought withdrawal and thought broadcasting. However, no significant relationship was found between AVHs and grandiose, somatic, religious, guilty or jealousy-themed delusions. Cluster analysis yielded two distinct cluster groups. Cluster One: Voices and Thought Delusions, and Cluster Two: Voices and Thematic Delusions. Cluster One participants showed elevated disorganized, cognitive and depressive symptoms, but not negative symptoms or excitement. This study underscores the need for expanded clinical and phenomenological research into the intersection of AVHs and delusions, including work that seeks to deconstruct conventional divisions between ostensible symptoms of perception’ (hallucinations) and belief’ (delusions).
Keywords: Phenomenology, Auditory Verbal Hallucinations, Delusions, Psychosis
Introduction
Recent research suggests that psychotic experiences (PEs), including auditory verbal hallucinations (AVHs) and delusions, are more nuanced than conventionally believed. AVHs and delusions are both central and multi-dimensional symptoms found in schizophrenia spectrum disorders and other disorders with psychotic features (Lincoln, 2007; Jobe & Harrow, 2010; Rosen, Grossman, Harrow, Bonner-Jackson, & Faull, 2011). These experiences exist along a continuum spanning the general and clinical population (Johns & van Os, 2001; van Os, Hanssen, Bijl, & Vollebergh, 2001; van Os, 2014; Johns et al. 2014). A recent epidemiologic survey of the prevalence of PEs in the general population from 18 countries showed the mean lifetime prevalence of PEs was 5.8% with auditory or visual hallucinations (5.2%) more common than delusions (1.3%) (McGrath et al., 2015). Overall, 32.2% of the total population reported one lifetime PE and 31.8% reported 2 to 5 occurrences.
Traditionally, hallucinations have been understood as abnormalities of perception, and delusions as abnormalities of cognition (or belief) (Tuttle, 1902; Berrios & Markova, 2012). These types of PEs have been reinforced by recent research (Woods, Jones, Alderson-Day, Callard, & Fernyhough, 2015). Descriptive psychopathologists have long noted the presence of “silent” or thought-like AVHs, as well as AVHs with ambiguous perceptual and cognitive qualities. Some researchers have proposed that delusions of reference, control and communication may at times overlap with, or even prove to be indistinguishable from AVHs (Jones & Luhrmann, 2015 (In-Press)). Recent studies have also shown a strong association of content between AVHs and delusions in clinical population whereas the association is independent of content in the general population (de Leede-Smith & Barkus, 2013; Laroi, 2012).
Different causal pathways have been put forward to explain the relationship between AVHs and delusions. Phenomenological psychopathologists have conceptualized full-fledged/frank AVHs and delusions as downstream products of more fundamental disruptions in basic sense of self, believed to involve multiple systems (e.g. proprioception, sensation, perception) (Sass & Parnas, 2003, Nelson, Whitford, Lavoie, & Sass, 2014, Sass, 2014). Others have proposed that delusions often, arise as patients’ explanations and interpretations of bizarre or inexplicable sensory and/or perceptual anomalies (David, 2004; Maher, 2006; Hoffman, Varanko, Gilmore, & Mishara, 2008; Moritz & Laroi, 2008).
Historically, some forms of AVHs and delusions have been considered more pathognomonic of schizophrenia spectrum psychoses than others, including passivity symptoms (including thought insertion and thought withdrawal), ontologically bizarre delusions, and conversing AVHs or AVHs that provide running commentaries on a patient’s thoughts and/or actions (Liddle, 1987; Slade & Bentall, 1988; Peralta & Cuesta, 1999). Paranoid delusions are also often considered distinct from other defined beliefs. From an etiological perspective, childhood sexual trauma has been more specifically linked to AVHs, while childhood attachment problems have been more strongly linked to delusions (Bentall, Wickham, Shevlin, & Varese, 2012; van Nierop et al., 2014; Longden, Sampson, & Read, 2015). Prognostically, Van Os and colleagues (2014), suggest that outcomes are worst for those with co-occurring AVHs and delusions versus only AVHs or only delusions (van Os, 2014).
While recent efforts have certainly turned toward the investigation of the relationship between AVHs and delusions, additional research is needed which focusses on phenomenologically complex and nuanced interrelatedness. To advance the area of phenomenology of voices and their interrelatedness to forms of delusions in participants with psychosis, we investigated the following questions:
What is the prevalence of co-occurring AVHs and delusions in schizophrenia compared to bipolar disorder with psychosis?
Are there correlations between AVHs and forms of delusions?
Are there sub-categories/clusters of AVHs and forms of delusions that are distinct and identifiable and what is the symptom presentation of these sub-categories/clusters?
Methods
This study reports the analyses from a novel investigation into the intercept of AVHs and forms of delusions. The term “intrasubjectivity” used throughout this study is in reference to the intercept between voices and various types of delusions that are experienced within self. The sample was recruited from a large urban university medical center, private referrals, and community treatment facilities. The total sample were administered the Structured Clinical Interview for DMS Disorders (SCID-IVtr) and the Positive and Negative Syndrome Scale (PANSS) (Kay, Fiszbein, & Opler, 1987; First, Spitzer, Gibbon, & Williams, 2002).
Subjects
Ninety-two persons experiencing psychosis participated in the study. Inclusion criteria included participants between the ages of 21 – 60 who met criteria for schizophrenia or bipolar disorder/psychosis. Exclusion criteria included substance dependence, seizure disorders, and neurological conditions. Demographic characteristics and duration of untreated psychosis (DUP) were obtained at the study evaluation. DUP was defined as the number of months between onset of psychosis and initiation of antipsychotic medication. IQ was estimated using the 2-subtest version of the Wechsler Abbreviated Scale of Intelligence (WASI) (Wechsler, 1999). The study was approved by the University IRB, and signed consent was obtained prior to initiation of study procedures. Consensus diagnoses were determined by the clinical and research team using the SCID, and available collateral information. Of the 92 study-eligible participants, 59 (64%) were diagnosed with schizophrenia and 33 (36%) were diagnosed with bipolar disorder/psychosis.
Measures used to assess the phenomenology of voices and forms of delusions
Clinical measures for this study included the SCID and PANSS. The evaluation of AVHs and forms of delusions were based on the SCID and scored as absent (score of “1”), subthreshold (“2”) and threshold or present (“3”). The SCID includes an assessment of AVHs, including voices conversing, voices commenting, and forms of delusions such as referential, persecutory, grandiose, somatic, religious, guilt, jealous, erotomanic, control, thought insertion, thought withdrawal, and thought broadcasting.
PANSS was scored along a continuum of severity between one (asymptomatic) to seven (extreme symptom severity). Analysis was conducted via data reduction strategies guided by prior empirical studies of symptom domains assessed by the PANSS (Kay et al., 1987). Scores were calculated for five-factors: Positive symptoms (delusions, grandiosity, suspiciousness/persecution, unusual thought content), Negative symptoms (blunted affect, emotional withdrawal, poor rapport, passive/apathetic social withdrawal, lack of spontaneity and flow of conversation, and active social avoidance), Cognitive Disorganization (conceptual disorganization, difficulty in abstract thinking, mannerisms and posturing, disorientation, and poor attention), Depression (somatic concern, anxiety, guilt feelings, depression, and preoccupation) and Excitement (excitement, hostility, tension, and poor impulse control). Items were pooled in this way based on previous factor analytic findings (Lindenmayer, Bernstein-Hyman, & Grochowski, 1994; Lehoux, Gobeil, Lefebvre, Maziade, & Roy, 2009).
Data Analyses
Demographic data were analyzed using Fisher exact tests and analyses of variance (ANOVA). For ANOVAs that yielded significant results (alpha level <0.05), Newman-Keuls post hoc tests were used to identify significant pair-wise group differences. A diagnostic comparison of the prevelance of AVH and delusions were analyzed using 2×3 Chi Square test. Bivariate Spearman’s correlations were conducted to determine separate associations between voices and forms of delusions. Two-step cluster analyses using were conducted to identify distinct sub-categories of voices and forms of delusions followed by independent sample t-test to compare PANSS 5-factor scores between identified subgroup clusters. All analyses on symptoms utilized SCID data other than PANSS data that was utilized to compare symptoms between identified subcluster groups.
Results
Descriptive characteristics
Group comparisons of demographic characteristics show a significant sex difference between diagnostic groups, with the schizophrenia group including more male participants compared to the bipolar disorder group (p<0.05, Fisher’s exact test). There was no significant difference between diagnostic groups in race, current age, age of onset of psychosis, duration of untreated psychosis, IQ, or years of education.
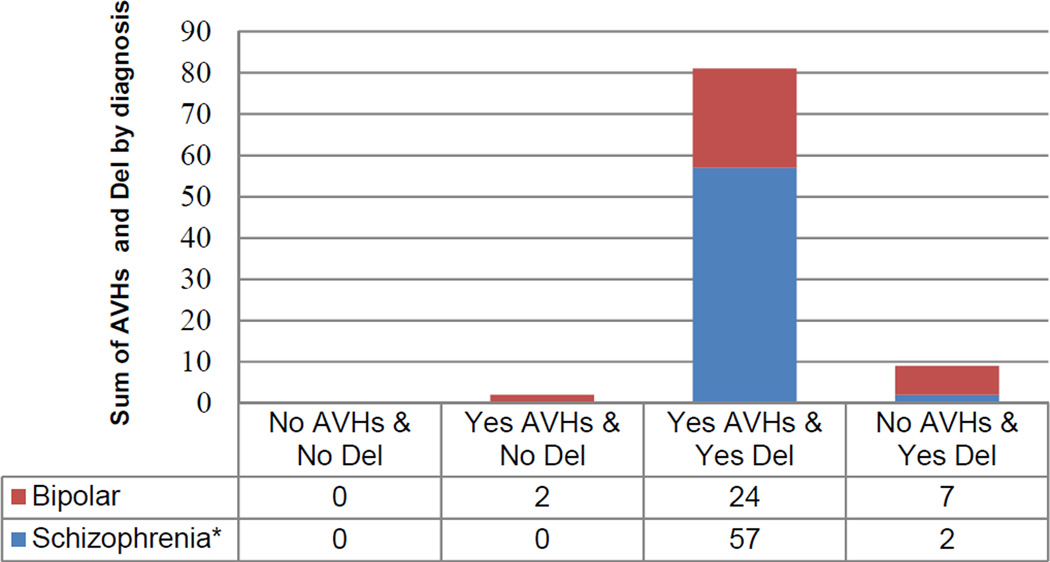
Figure one shows the prevalence of AVHs alone (n=2), co-occurring AVHs and delusions (n=81), and delusions alone (n=9) by diagnostic group. Group comparisons of prevalence of co-occurring AVHs and delusions show a significant diagnostic difference between groups, with increased prevalence of co-occuring AVH and delusions within the schizophrenia group (X2(1, N=92)=11.47, p<0.001).
Figure 1. Auditory Verbal Hallucinations & Delusions Interrelatedness.
The comparison of auditory verbal hallucinations and delusions in participants with schizophrenia in comparison to participants with bipolar with psychosis.
Phenomenological Characteristics of Voices and Delusions
To better understand the relationship between AVHs and forms of delusions in psychotic disorders we conducted a bivariate correlation. AVHs were strongly correlated with specific forms of delusions (Table 1). Regardless of diagnosis, there was a significant positive correlation between AVHs and delusions of reference, persecution, control, thought insertion, thought withdrawal and thought broadcasting. However, no significant relationship was found between AVHs and grandiose, somatic, religious, guilty or jealousy-themed delusions.
Table 1. Correlations between AVHs and forms of delusions.
Spearman Correlations between auditory verbal hallucinations and forms of delusions.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Voices | ~ | |||||||||||
| 2. | Delusions of reference |
0.50*** | ~ | ||||||||||
| 3. | Persecutory Delusions |
0.52*** | 0.33** | ~ | |||||||||
| 4. | Grandiose Delusions |
0.11 | 0.19 | 0.02 | ~ | ||||||||
| 5. | Somatic Delusions |
0.16 | 0.25* | 0.06 | 0.02 | ~ | |||||||
| 6. | Religious Delusions |
0.17 | 0.31** | 0.20 | 0.48*** | 0.01 | ~ | ||||||
| 7. | Delusions of Guilt |
0.14 | 0.14 | 0.13 | 0.15 | 0.19 | 0.20 | ~ | |||||
| 8. | Jealous Delusions |
0.15 | 0.16 | 0.07 | 0.06 | 0.14 | 0.09 | 0.63*** | ~ | ||||
| 9. | Erotomanic Delusions |
0.15 | 0.16 | 0.07 | 0.23* | 0.11 | 0.24* | 0.30** | 0.48*** | ~ | |||
| 10. | Delusions of being controlled |
0.35*** | 0.42*** | 0.22* | 0.22* | 0.21* | 0.37*** | 0.14 | 0.14 | −0.02 | ~ | ||
| 11. | Delusions of thought insertion |
0.29** | 0.38*** | 0.15 | 0.24* | 0.14 | 0.37*** | 0.19 | 0.20 | 0.05 | 0.85*** | ~ | |
| 12. | Delusions of thought withdrawal |
0.27** | 0.31** | 0.28** | 0.18 | 0.25* | 0.37*** | −0.07 | 0.02 | 0.02 | 0.62*** | 0.49*** | ~ |
| 13. | Delusions of thought broadcasting |
0.26** | 0.31** | 0.13 | 0.20 | 0.11 | 0.33*** | 0.05 | 0.01 | 0.08 | 0.53*** | 0.43*** | 0.28** |
p<0.05,
p<0.01,
p<0.001.
To identify specific sub-types we conducted two-step cluster analysis that consisted of preclustering and standard hierarchical clustering algorithm of SCID items pertaining to voices and delusions (Zhang, Ramakrishnon, & Livny, 1996; Chiu, Fang, Chen, Wang, & Jeris, 2001). The analysis yielded two distinct cluster groups. Cluster One: Voices and Thought Delusions, consisted of 54 individuals (59%) and Cluster Two: Voices and Thematic Delusions, consisted of 38 subjects (41%). Diagnostically, the Voices and Thought Delusions cluster consisted of 41 participants with schizophrenia and 13 participants with bipolar disorder/psychosis. Voices and Thematic Delusions consisted of 18 participants with schizophrenia and 20 participants with bipolar disorder/psychosis, which yielded a significant diagnostic difference between clusters (p<0.008, Fisher’s exact test); showing a higher percentage of participants with schizophrenia in the Voices and Thought Delusions cluster. There was no significant demographic difference between cluster groups in sex, race, DUP, age of onset of psychosis symptoms, current age, IQ, years of education. The primary cluster predictor algorithm show that delusions of control, thought insertion, thought withdrawal, and thought broadcasting are more discrete variables in identifying cluster subtypes and thematic type delusions, such as delusions of guilt, jealousy, and erotomania were least predictive.
An independent sample t-test was then conducted to compare PANSS 5-factor subscales with Voices and Thought Delusions to Voices and Thematic Delusions. There was a significant elevation in PANSS Positive factor scores in Voices and Thought Delusions compared to the Voices and Thematic Delusions cluster; t90=3.46, p=0.001. We also found significantly higher rates of PANSS Cognitive factor scores in Voices and Thought Delusions compared to Voices and Thematic Delusions clusters; t90=1.99, p=0.05. Additionally, there was a significant elevation in Voices and Thought Delusions compared to Voices and Thematic Delusions in PANSS 5-factor Depression scores; t90=2.48, p=0.015. There was no significant group difference in PANSS 5-factor Negative scores (t90=1.39, p=0.17) or PANSS 5-factor Excitement scores (t90=4.95, p=0.62). These results suggest that, participants in the Voices and Thought Delusions cluster experienced increased Positive, Cognitive, and Depressive factor scores but not Negative or Excitement factor scores.
Discussion
In this paper, we report novel findings that contribute to the understanding of the phenomenological intrasubjectivity of voices, and forms of delusions. AVHs are known to be transdiagnostic, and to exist along a continuum that are typically associated with delusions (Liddle, 1987; Allen et al., 2004; Jobe & Harrow, 2010). Building on findings that AVHs exist along a continuum, a recent study demonstrated that psychotic experiences, including hallucinations and delusions also exist as a continuum of variation in dimensions (McGrath et al., 2015). In fact, a recent re-examination of teachings by Kraepelin, Engstrom & Kendler, noted that Kraepelin underscored difficulties of clearly differentiating distinct diagnostic categories and suggested that dementia praecox and manic-depressive illness should be understood as a psychopathological continuum (Kraepelin, 1893; Engstrom & Kendler, 2015). In keeping with the continuum hypothesis, studies have also explored underlying neural correlates of inner speech and auditory hallucinations that suggest similar neural substrates are activated (Bentall, 2003; Jones & Fernyhough, 2006; Alderson-Day et al., 2015).
There are multiple hypotheses put forward regarding pathways of AVHs and delusions, though a full account for these experiences must involve an integration of social, psychological and biological factors as factors contributing to the pathogensis of psychosis. It has been hypothesized that AVHs and delusions may result from a core disturbance of basic self (Sass & Parnas, 2003; Parnas, Handest, Jansson, & Saebye, 2005; Nelson, Parnas, & Sass, 2014). The manisfestitation of self-disturbance consist of subclinical disturbances in thinking, perception, sensations, affect, and sense of control (Gross, Huber, Klosterkotter, & Linz, 1987; Gross, Huber, Klosterkotter, & Linz, 2008; Parnas et al., 2005). Self-disturbances can be further linked to biological changes in brain function (Badcock, 2015). In some case, the trajectory from core disturbances to AVH consists of a progression from perseveration on thoughts into audible thoughts that can then lead to the development of Schneiderian First Rank AVHs (Klosterkotter, 1992; Sass & Parnas, 2003; Laroi & Woodward, 2007). It has been hypothesized that the formulation of delusions may represent an extension of the individual’s process of attributing meaning to basic alterations and abnormalities of perceptual experience (Allen et al., 2004; Holt & Tickle, 2015; Bortolotti & Broome, 2008;; Handest, Klimpke, Raballo, & Laroi, 2015). These changes in perception and/or diminution of sense of boundary between self and others characterize a subset of Schneiderian FRS that share the experience of passivity in AVHs (voices conversing or voices commenting) and/or delusions (thought insertion, withdrawal or broadcast, and control) (Frith, Blakemore, & Wolpert, 2000; Waters, Badcock, Dragovic, & Jablensky, 2009). Our data cannot directly support a theory of ‘progressive symptom development’ which would require a measurement of a coordinated sequence of subjective experiences of the pathological sequela of temporal unity disturbance. Whereas, our data analyses with SCID items actually are (lifetime symptom presence without any temporal onset or simultaneous occurrence information). However, our analyses do support a non-temporal-specific disorder of self.
Self, voices and thought/thematic delusion subtypes
The significant correlations we identified between voices and specific forms of delusions such as thought or thematic delusions supports claims of an intrasubjective relationship between voices, and delusions grounded in the merging or confusion of self/other and internal/external boundaries (Waters & Badcock, 2010; McCarthy-Jones, Krueger, Laroi, Broome, & Fernyhough, 2013; Humpston & Broome, 2015; Jones & Luhrmann, 2015 (In-Press); Rosen et al., 2015). While AVHs are conventionally understood as “hallucinatory” and delusions as “cognitive,” our analyses provisionally support a reframing of AVHs and thought delusions as endpoints on a shared continuum of attenuated sense of basic self (Schneider, 1959; Jaspers, 1963; Conrad, 1997; Sass & Parnas, 2003; Sass, 2010; Sass, 2014). Within this disturbance, aspects of agency, authorship, and mineness are experienced as foreign, not self-generated and with absence of intentionality (Laroi & Woodward, 2007; Vosgerau & Voss, 2014).
Our study also found two distinct clusters of AVHs and forms of delusions: AVHs paired with thought delusions (Cluster One) and AVHs paired with thematic delusions (Cluster Two). These clusters begin to disentangle the intrasubjectivity of voices and delusion by characterizing Cluster One: AVH and Thought Delusions as a structure that centers on alterations of self and internal/external boundaries, while Cluster Two: AVH and Thematic Delusions centers on exaggerated processes of social internalization (guilt) or externalization (jealousy/delusions of infidelity). Phenomenological psychopathologists have long contended, we found that participants with schizophrenia spectrum disorder were more likely to fall into Cluster One: AVH and Thought Delusions and those with bipolar psychosis into Cluster Two: AVH and Thematic Delusions. Nevertheless, neither group was diagnostically pathognomonic. Cluster One: AVH and Thought Delusions participants also showed elevated disorganized, cognitive and depressive symptoms, but not negative symptoms or excitement. Future research would be needed to further unpack whether these differences in severity are tied to diagnosis (schizophrenia versus bipolar) or more strongly to predominant pattern of delusions (Rosen et al., 2012; Wallwork, Fortgang, Hashimoto, Weinberger, & Dickinson, 2012; Rodriguez-Jimenez et al., 2013).
Intrasubjectivity and Clinical Implications
Clinically, study findings underscore the need for greater attention to the nuances of experiences conventionally divided up into AVHs and delusions, particularly when this distinction is framed as a difference between symptoms of perception versus belief. While our project did not explicitly query participants as to their perception of the validity of this distinction recent qualitative work (Jones & Luhrmann, 2015 (In-Press); Woods et al., 2015) suggests that, even at a conscious, subjective level, conventional divisions between AVHs and delusions may be perceived as misleading and/or inaccurate by patients. If the AVHs versus delusions distinction does not hold either conceptually or experientially—at least for some portion of patients--the psychotherapeutic implications are also significant given that tailored treatments (including specialized forms of CBTp) often target AVHs specifically or delusions. Potential problems with mono-symptom approaches are further highlighted by the high prevalence of co-occurring AVHs and delusions (Kingdon & Turkington, 1994; Chadwick, Birchwood, & Trower, 1996; McCarthy-Jones et al., 2014). Going one-step further, we might also conjecture that in cases where a common underlying alteration (such as attenuated ego boundaries) drives both AVHs and delusions, this underlying problem may represent a more valid clinical target. Thus, a detailed assessment of the phenomenology of self, voices, and thought or thematic delusions may help to provide information needed to develop a tailored, multipronged clinical intervention that addresses the complexities and interrelatedness.
Limitations
There are limits to the generalizability to these results in that the data are based largely on self-report. Additionally, although the primary focus of this study was not DUP, our finding of no diagnostic difference cannot be generalized. Our sample is unique in that it represents primarily an African American population; whereas many studies examining DUP typically represent Caucasian or heterogeneous populations and some studies do not report race.
Concluding Comments and Future Directions
In summary, this novel phenomenological study of self, voices and delusions suggests a significant relationship between voices and delusions of reference, persecution, control, thought insertion, thought withdrawal and thought broadcasting. The overwhelming majority of our participants reported both AVHs and delusions. We also provide preliminary support for differentiation of patients into subgroups characterized by the intersection of Voices and Thought Delusions versus Voices and Thematic Delusions. While both clusters implicate alternations of self-other experience, they do so in distinct ways: the former involving Schneiderian symptoms of passivity or confusion over ownership and internal versus external genesis of thoughts and the latter exaggerated projection and introjection. This study underscores the need for expanded clinical and phenomenological research into the intersection of AVHs and delusions, including work that seeks to deconstruct conventional divisions between ostensible symptoms of perception’ (hallucinations) and belief’ (delusions).
Acknowledgments
The authors would like to thank all subjects who participated in this study. This work was supported in part by PHS grant (NIH) R01MH094358 (R.P.S.)
References
- Alderson-Day B, Weis S, McCarthy-Jones S, Moseley P, Smailes D, Fernyhough C. The brain's conversation with itself: Neural substrates of dialogic inner speech. Social Cognitive and Affective Neuroscience. 2015 doi: 10.1093/scan/nsv094. Pii:nsv094 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen PP, Johns LC, Fu CH, Broome MR, Vythelingum GN, McGuire PK. Misattribution of external speech in patients with hallucinations and delusions. Schizophrenia Research. 2004;69(2–3):277–287. doi: 10.1016/j.schres.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Badcock JC. A Neuropsychological approach to auditory verbal hallucinations and thought insertion-grounded in normal voice perception. Review of Philosophy and Psychology. 2015:1–22. doi: 10.1007/s13164-015-0270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentall RP. Madness explained: Psychosis and human nature. Penguin Global; 2003. New edition. [Google Scholar]
- Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the adult psychiatric morbidity survey. Schizophrenia Bulletin. 2012;38(4):734–740. doi: 10.1093/schbul/sbs049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berrios GE, Markova IS. Hallucinations: Research and practice. Springer; 2012. The construction of hallucination: Histiory and epistemology; pp. 55–71. [Google Scholar]
- Bortolotti L, Broome MR. Delusional beliefs and reason giving. Philosophical Psychology. 2008;21(6) [Google Scholar]
- Chadwick P, Birchwood M, Trower P. Cognitive therapy for voices, delusions and paranoia. Chichester: Wiley; 1996. [Google Scholar]
- Chiu T, Fang D, Chen J, Wang Y, Jeris C. Proceedings of the Seventh ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. San Francisco, CA: ACM; 2001. A robust and scalable clustering algorithm for mixed type attributes in large database environment. [Google Scholar]
- Conrad K. In: La esquizofrenia incipiente. Belda JM, Rabano A, editors. Madrid: Dundacion Archivos de Neurobiologia; 1997. [Google Scholar]
- David AS. The cognitive neuropsychiatry of auditory verbal hallucinations: An overview. Cognitive Neuropsychiatry. 2004;9(1–2):107–123. doi: 10.1080/13546800344000183. [DOI] [PubMed] [Google Scholar]
- de Leede-Smith S, Barkus E. A comprehensive review of auditory verbal hallucinations: Lifetime prevalence, correlates and mechanisms in healthy and clinical individuals. Frontiers in Human Neuroscience. 2013;7:367. doi: 10.3389/fnhum.2013.00367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engstrom EJ, Kendler KS. Emil kraepelin: Icon and reality. The American Journal of Psychiatry. 2015 doi: 10.1176/appi.ajp.2015.15050665. appiajp201515050665. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Frith CD, Blakemore SJ, Wolpert DM. Abnormalities in the awareness and control of action. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2000;355(1404):1771–1788. doi: 10.1098/rstb.2000.0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross G, Huber G, Klosterkotter J, Linz M. BSABS bonn scale for the assessment of basic symptoms. Germany: Shaker Verlag; 2008. (1st English Edition ed.) [Google Scholar]
- Gross G, Huber G, Klosterkotter J, Linz M. BSABS bonner skala fur die beurteilung von basissymptomen. manual, kommentar, dokumentationsbogen. Berlin: Springer; 1987. [Google Scholar]
- Handest P, Klimpke C, Raballo A, Laroi F. From thoughts to voices: Understanding the development of auditory hallucinations in schizophrenia. Rev. Phil. Psych. 2015;15:30011–30016. [Google Scholar]
- Hoffman RE, Varanko M, Gilmore J, Mishara AL. Experiential features used by patients with schizophrenia to differentiate 'voices' from ordinary verbal thought. Psychological Medicine. 2008;38(8):1167–1176. doi: 10.1017/S0033291707002395. [DOI] [PubMed] [Google Scholar]
- Holt L, Tickle A. "Opening the curtains": How do voice hearers make sense of their voices? Psychiatric Rehabilitation Journal. 2015;38(3):256–262. doi: 10.1037/prj0000123. [DOI] [PubMed] [Google Scholar]
- Humpston CS, Broome MR. The Review of Philosophy and Psychology. Springer; 2015. The spectra of soundless voices and audible thoughts: Towards an integrative model of auditory verbal hallucinations and thought insertion. [Google Scholar]
- Jaspers K. General psychopathology. Chicago, IL: JHU Press; 1963. [Google Scholar]
- Jobe T, Harrow M. Schizophrenia course, long-term outcome, recovery, and prognosis. Current Directions in Psychological Science. 2010;19 220-220-225. [Google Scholar]
- Johns LC, Kompus K, Connell M, Humpston C, Lincoln TM, Longden E, Fernyhough C. Auditory verbal hallucinations in persons with and without a need for care. Schizophrenia bulletin. 2014;40(Suppl 4):S255–S264. doi: 10.1093/schbul/sbu005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns LC, van Os J. The continuity of psychotic experiences in the general population. Clinical Psychology Review. 2001;21(8):1125–1141. doi: 10.1016/s0272-7358(01)00103-9. [DOI] [PubMed] [Google Scholar]
- Jones N, Luhrmann T. Beyond the sensory: Findings from an in-depth analysis of the phenomenology of ' auditory hallucinations' in schizophrenia. Psychosis. 2015 (In-Press) [Google Scholar]
- Jones SR, Fernyhough C. The roles of thought suppression and metacognitive beliefs in proneness to auditory verbal hallucinations in a non-clinical sample. 2006;41(8) 1421-1421-1432. [Google Scholar]
- Kay SR, Fiszbein A, Opler L. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2) doi: 10.1093/schbul/13.2.261. 261-261-276. [DOI] [PubMed] [Google Scholar]
- Kingdon DG, Turkington D. Cognitive behavioural therapy of schizophrenia. New Yorjk: Guilford; 1994. [DOI] [PubMed] [Google Scholar]
- Klosterkotter J. The meaning of basic symptoms for the development of schizophrenic psychoses. Neurology Psychiatry and Brain Research. 1992;1 30-30-41. [Google Scholar]
- Kraepelin E. Psychiatrie: Ein kurzes lehrbuch fur studirende und aerzte. 1893 [Google Scholar]
- Laroi F. How do auditory verbal hallucinations in patients differ from those in non-patients? Frontiers in Human Neuroscience. 2012;6:25. doi: 10.3389/fnhum.2012.00025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laroi F, Woodward TS. Hallucinations from a cognitive perspective. Harvard Review of Psychiatry. 2007;15(3):109–117. doi: 10.1080/10673220701401993. [DOI] [PubMed] [Google Scholar]
- Lehoux C, Gobeil MH, Lefebvre AA, Maziade M, Roy MA. The five-factor structure of the PANSS: A critical review of its consistency acorss studies. Clin Schizophre Relat Psychoses. 2009;3(2) 103-103-110. [Google Scholar]
- Liddle PF. The symptoms of chronic schizophrenia. A re-examination of the positive-negative dichotomy. The British Journal of Psychiatry : The Journal of Mental Science. 1987;151:145–151. doi: 10.1192/bjp.151.2.145. [DOI] [PubMed] [Google Scholar]
- Lincoln TM. Relevant dimensions of delusions: Continuing the continuum versus category debate. Schizophrenia Research. 2007;93(1–3):211–220. doi: 10.1016/j.schres.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Lindenmayer JP, Bernstein-Hyman R, Grochowski S. Five-factor model of schizophrenia. initial validation. The Journal of Nervous and Mental Disease. 1994;182(11):631–638. doi: 10.1097/00005053-199411000-00006. [DOI] [PubMed] [Google Scholar]
- Longden E, Sampson M, Read J. Childhood adversity and psychosis: Generalised or specific effects? Epidemiology and Psychiatric Sciences. 2015;9:1–11. doi: 10.1017/S204579601500044X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher BA. The relationship between delusions and hallucinations. Current Psychiatry Reports. 2006;8(3):179–183. doi: 10.1007/s11920-006-0021-3. [DOI] [PubMed] [Google Scholar]
- McCarthy-Jones S, Krueger J, Laroi F, Broome M, Fernyhough C. Stop, look, listen: The need for philosophical phenomenological perspectives on auditory verbal hallucinations. Frontiers in Human Neuroscience. 2013;7:127. doi: 10.3389/fnhum.2013.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy-Jones S, Trauer T, Mackinnon A, Sims E, Thomas N, Copolov DL. A new phenomenological survey of auditory hallucinations: Evidence for subtypes and implications for theory and practice. Schizophr Bull. 2014;40(1):231–235. doi: 10.1093/schbul/sbs156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: A cross-national analysis based on 31261 respondents from 18 countries. JAMA Psychiatry. 2015;72(7):697–705. doi: 10.1001/jamapsychiatry.2015.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moritz S, Laroi F. Differences and similarities in the sensory and cognitive signatures of voice-hearing, intrusions and thoughts. Schizophrenia Research. 2008;102(1–3) doi: 10.1016/j.schres.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Nelson B, Parnas J, Sass LA. Disturbance of minimal self (ipseity) in schizophrenia: Clarification and current status. Schizophrenia Bulletin. 2014;40(3):479–482. doi: 10.1093/schbul/sbu034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson B, Whitford TJ, Lavoie S, Sass LA. What are the neurocognitive correlates of basic self-disturbance in schizophrenia?: Integrating phenomenology and neurocognition. part 1 (source monitoring deficits) Schizophrenia Research. 2014;152(1):12–19. doi: 10.1016/j.schres.2013.06.022. [DOI] [PubMed] [Google Scholar]
- Parnas J, Handest P, Jansson L, Saebye D. Anomalous subjective experience among first-admitted schizophrenia spectrum patients: Empirical investigation. Psychopathology. 2005;38(5):259–267. doi: 10.1159/000088442. [DOI] [PubMed] [Google Scholar]
- Parnas J, Moller P, Kircher T, Thalbitzer J, Jansson L, Handest P, Zahavi D. EASE: Examination of anomalous self-experience. Psychopathology. 2005;38(5):236–258. doi: 10.1159/000088441. [DOI] [PubMed] [Google Scholar]
- Peralta V, Cuesta MJ. Diagnostic significance of schneider's first-rank symptoms in schizophrenia. comparative study between schizophrenic and non-schizophrenic psychotic disorders. The British Journal of Psychiatry : The Journal of Mental Science. 1999;174:243–248. doi: 10.1192/bjp.174.3.243. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Jimenez R, Bagney A, Mezquita L, Martinez-Gras I, Sanchez-Morla EM, Mesa N, et al. Cognition and the five-factor model of the positive and negative syndrome scale in schizophrenia. Schizophrenia Research. 2013;143(1):77–83. doi: 10.1016/j.schres.2012.10.020. [DOI] [PubMed] [Google Scholar]
- Rosen C, Jones N, Chase KA, Grossman LS, Gin H, Sharma RP. Self, voices and embodiment: A phenomenological analysis. Journal of Schizophrenia Research. 2015;2(1) [PMC free article] [PubMed] [Google Scholar]
- Rosen C, Grossman LS, Harrow M, Bonner-Jackson A, Faull R. Diagnostic and prognostic significance of schneiderian first-rank symptoms: A 20-year longitudinal study of schizophrenia and bipolar disorder. Comprehensive Psychiatry. 2011;52(2):126–131. doi: 10.1016/j.comppsych.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen C, Marvin R, Reilly JL, Deleon O, Harris MS, Keedy SK, et al. Phenomenology of first-episode psychosis in schizophrenia, bipolar disorder, and unipolar depression: A comparative analysis. Clinical Schizophrenia & Related Psychoses. 2012;6(3):145–151. doi: 10.3371/CSRP.6.3.6. [DOI] [PubMed] [Google Scholar]
- Sass LA. Phenomenology as description and as explanation: The case of schizophrenia. Netherlands: Springer; 2010. [Google Scholar]
- Sass LA, Parnas J. Schizophrenia, consciousness, and the self. Schizophrenia Bulletin. 2003;29(3):427–444. doi: 10.1093/oxfordjournals.schbul.a007017. [DOI] [PubMed] [Google Scholar]
- Sass LA. Self-disturbance and schizophrenia: Structure, specificity, pathogenesis (current issues, new directions) Schizophrenia Research. 2014;152(1):5–11. doi: 10.1016/j.schres.2013.05.017. [DOI] [PubMed] [Google Scholar]
- Sass LA, Parnas J. Schizophrenia, consciousness, and the self. Schizophrenia Bulletin. 2003;29(3):427–444. doi: 10.1093/oxfordjournals.schbul.a007017. [DOI] [PubMed] [Google Scholar]
- Schneider K. Clinical psychopathology. Indiana University: Grune & Stratton; 1959. [Google Scholar]
- Slade PD, Bentall RP. Sensory deception: A scientific analysis of hallucination. the johns hopkins series in contemporary medicine and public health. Johns Hopkins University Press; 1988. [Google Scholar]
- Tuttle TG. Hallucinations and illusions. American Journal of Psychiatry. 1902;58 443-443-467. [Google Scholar]
- van Nierop M, Lataster T, Smeets F, Gunther N, van Zelst C, de Graaf R, et al. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: Analysis of a large, representative population-based sample. Schizophrenia Bulletin. 2014;40(Suppl 2):S123–S130. doi: 10.1093/schbul/sbt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Os J. The many continua of psychosis. JAMA Psychiatry. 2014;71(9):985–986. doi: 10.1001/jamapsychiatry.2014.1068. [DOI] [PubMed] [Google Scholar]
- van Os J, Hanssen M, Bijl RV, Vollebergh W. Prevalence of psychotic disorder and community level of psychotic symptoms: An urban-rural comparison. Archives of General Psychiatry. 2001;58(7):663–668. doi: 10.1001/archpsyc.58.7.663. [DOI] [PubMed] [Google Scholar]
- Vosgerau G, Voss M. Authorship and control over thoughts. Mind & Language. 2014;29(5) 534-534-565. [Google Scholar]
- Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D. Searching for a consensus five-factor model of the positive and negative syndrome scale for schizophrenia. Schizophrenia Research. 2012;137(1–3):246–250. doi: 10.1016/j.schres.2012.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters FA, Badcock JC. First-rank symptoms in schizophrenia: Reexamining mechanisms of self-recognition. Schizophrenia Bulletin. 2010;36(3):510–517. doi: 10.1093/schbul/sbn112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters FA, Badcock JC, Dragovic M, Jablensky A. Neuropsychological functioning in schizophrenia patients with first-rank (passivity) symptoms. Psychopathology. 2009;42(1):47–58. doi: 10.1159/000187634. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler abbreviated scale of intelligence. Psychological Corporation; 1999. [Google Scholar]
- Woods A, Jones N, Alderson-Day B, Callard F, Fernyhough C. Experiences of hearing voices: Analysis of a novel phenomenological survey. Lancet Psychiatry. 2015;2(4):323–331. doi: 10.1016/S2215-0366(15)00006-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang T, Ramakrishnon R, Livny M. BIRCH: An efficient data clustering method for very large databases. Proceedings of the ACM SIGMOD Conference on Management of Data. 1996;25(2):103–114. [Google Scholar]