Abstract
Research on childhood mental illness traditionally examines risk factors most proximal to the child. However, current trends reflect growing interest in how broader contextual factors contribute to psychopathology risk. In this study, we examined neighborhood-level indicators as potential sources of chronic strain in a sample of 156 mother-child dyads. Children were 8–12 years old. For most neighborhood indicators, data were collected at the level of census tracts using publically available data sets. We hypothesized that these indicators would be associated with greater overall mental health symptoms, as well as specifically predictive of childhood symptoms of depression. We also examined potential mediators (maternal functioning and family cohesion), and moderators (maternal depression). Neighborhood indicators correlated with parents’ ratings of children’s overall mental health problems, but not children’s self-report of depression symptoms. Maternal functioning mediated neighborhood effects on children’s overall mental health problems. Implications and directions for future research are presented.
Keywords: neighborhoods, ecological models, child psychopathology, depression
Etiological research on psychopathology often examines the pathway from risk factors to outcomes at the individual level, with a focus on those risk factors most proximal to the individual. However, broader contextual factors may increase the risk of mental illness through direct and indirect mechanisms. Ecological models of development (EMDs) are designed to address this gap. These models take into account broader contextual factors and the ways in which these factors impact the onset and course of development generally and mental health outcomes specifically (Bronfenbrenner, 1977; 1994). Highlighting the interrelatedness between context and health, EMDs provide a more complete picture of the social determinants of health. Whether studying the impact of overt and subtle racism on African-American health (Williams, & Williams-Morris, 2000) or the lack of recreational facilities on obesity (Black et al., 2010), the importance of considering a wider array of influences on health is becoming clearer.
EMDs examine multiple contextual layers. The contexts under consideration vary in closeness to the developing individual, ranging from the most proximal contexts at the individual level (e.g., cognitive and biological factors) to those more distal to the person at the macro-level (e.g., societal characteristics) and serving as either risk or protective factors. Using an EMD to guide our examination of mental health outcomes broadly and depression in particular, may provide valuable information on the factors that influence mental health conditions in children.
In this study, we examined the relationship between one type of a macro-level factor, the neighborhood context, and symptoms of mental health problems. In addition to the broader domain of mental health overall, we also considered the impact of neighborhood-level factors on depression symptoms specifically. The population under examination was youth in late childhood and early adolescence. This particular developmental phase often coincides with a time when contact with extra-familial contexts (e.g., peer group, community, and school) increases (Boardman & Saint Onge, 2005; Steinberg & Morris, 2001). As such, the saliency of these contextual stressors as risk factors for mental health problems may rise.
Neighborhood context
Neighborhoods may be a source of chronic strain that is detrimental to individuals and families. Much of the current research on this connection finds its roots in William J. Wilson’s work examining neighborhood factors and their connection to and impact on residents’ behaviors and well-being (Wilson, 1987). Since then, researchers have mounted a strong case to suggest that aspects of the neighborhood environment are a type of chronic strain (Paczkowski & Galea, 2010) for individuals and families. As the link between stress and depression is well documented (Hammen, Hazel, Brennan, & Najman 2012, Tennant, 2002; Ensel & Lin, 1996), it is not surprising to find that stressful neighborhood characteristics are also associated with poorer mental health outcomes (Latkin & Curry, 2003; Picket & Pearl, 2001), including increases in depression symptomology (Mair, Diez-Roux, & Galea, 2008). Several neighborhood variables have been found to correlate with depression: residential instability, low socioeconomic status (SES), disadvantage, and social disorder (Aneshensel et al., 2007; Galea, Ahern, Rudenstine, Wallace, & Vlahov, 2005; Cutrona, Wallace & Wesner, 2006). Most of these data are based on adult studies; however, the more limited research on child and adolescent depression symptoms in relation to neighborhood-level characteristics shows similar trends. For adolescents, the research highlights correlations between depressive symptoms and perceptions of neighborhood strain, neighborhood poverty, and low sense of community (Aneshensel & Sucoff, 1996; Hadley-Ives, Stiffman, Elze, Johnson, & Dore, 2000; Caughy, O’Campo, & Muntaner, 2003). For children, correlational studies also demonstrate a link between neighborhood characteristics (e.g., neighborhood disorder and disadvantage) and broader mental health problems, as well as depression symptoms (Caughy, Nettles, & O’Campo, 2007; Xue, Leventhal, Brooks-Gunn, & Earls, 2005).
Research on neighborhood effects relies heavily on correlational data; however, a rare chance for an experimental design occurred with the Moving to Opportunity (MTO) housing program (Leventhal & Brooks-Gunn, 2003). Through a random housing lottery, families received vouchers to move to low-poverty areas or unrestricted vouchers. The control group did not receive any vouchers. Rates of parental depression within a one-year period were improved for those using low-poverty vouchers, which remained true at a 10–12 year follow-up (Ludwig et al., 2012). Children of the experimental group had fewer symptoms of anxiety and depression than either of the other two groups as assessed by subscales on the Behavior Problems Index (Leventhal & Brooks-Gunn, 2003; Katz, Kling, & Liebman, 2001). While the low poverty neighborhoods would not be expected to be devoid of any sources of strain, it is likely that the level of risk factors associated with high poverty neighborhoods was reduced. These findings provide further support for the idea that reductions in neighborhood strain may be associated with more positive psychological well-being for children.
Potential Mechanisms of Effects
Maternal functioning
Neighborhood strain can have direct and indirect effects on the developing child. Direct effects may include triggering the stress response system, and changes in cortisol in response to HPA axis activation (Dulin-Keita, Casazza, Fernandez, Goran, & Gower, 2010). Indirect effects on children may occur through the impact of chronic strain on overall maternal functioning, which in turn is likely to impact parenting practices and the parent-child relationship. Stress in general, and neighborhood-level stressors in particular, have been associated with decreased parental warmth, and increased harsh discipline practices (Tendulkar, Buka, Dunn, & Subramanian, 2010; Tompson, McKowen & Asarnow, 2009; Pinderhughes, Nix, Foster, & Jones, 2001). In light of these findings, we examined maternal functioning as a potential mechanism of the effect of neighborhood strain on children.
Family environment
Family environment refers to “the social environmental characteristics of the family” (Ogburn et al., 2010). The family environment might also contribute to the link between neighborhood strain and child outcomes. Neighborhood strain may have deleterious effects on the family environment, which may lead to more family conflict and less cohesion, negatively impacting child development (Kohen, Leventhal, Dahinten, & McIntosh, 2008). Family environment problems, such as negative emotional expressiveness, defined as the degree to which family members express negative emotions, have been linked to increased risk for depression and anxiety (Luebbe & Bell, 2014). Klebanov, Brooks-Gunn, Chase-Lansdale, & Gordon (1997) investigated the influence of neighborhood effects on child outcomes through its impact on family-level processes. Results were inconsistent for pre-school age cohorts, but evidence for mediation was greater for children closer to school age. More recent research by Yingling and Qian (2012) found that family functioning did mediate the relationship between neighborhood effects and parental reports of children’s overall health (which was broadly defined). For this study, we examined one component of the family environment, cohesion. Cohesion can be understood as the degree to which families are committed to and provide support for one another (Moos & Moos, 1994). Neighborhood strain may impact children through its effect on family cohesion (Plybon & Kliewer, 2001).
Maternal depression
There is some research supporting the potential mediating effect of maternal depression on the relationship between neighborhood stressors and child outcomes. In their research on young children (ages 4–5), Kohen et al. (2008) found that the impact of neighborhood strain on children’s overall behavior problems was mediated by maternal depressive symptoms. However, fewer researchers have examined maternal depression as a moderator of neighborhood effects. Given that maternal depression is a well-established risk factor for the development of depression in offspring (Beardslee, Versagem, & Gladstone, 1998; Weissman et al., 2005; Murray et al., 2011), it may be that children of mothers with a history of depression or with elevated depressive symptoms have a greater vulnerability to the effects of neighborhood stressors. This may be due to the aggregation of risk factors. Undoubtedly, the mechanisms of effects are likely quite broad and varied as neighborhood stressors interact with and influence a wide array of additional variables directly and indirectly (Kohen et al., 2008). In this study, we aimed to examine the potential moderating effect of maternal depression to provide further evidence to determine the mechanisms of effects of neighborhood strain.
Aims & Hypotheses
The primary purpose of this project was to examine the potential impact of neighborhood conditions on children’s self-reported depression symptoms and maternal reports of children’s overall symptoms of psychopathology, as well as the potential mechanisms of such effects. There were three aims: (1) Examine cross-sectional associations between neighborhood context and children’s overall mental health symptoms and depression symptoms at baseline. We hypothesized that levels of neighborhood strain would have a statistically significant correlation with broader symptoms of mental health problems and symptoms of childhood depression after controlling for child age, sex, and maternal age. (2) Examine two-year trends to see if greater neighborhood strain was predictive of higher levels of mental health problems and symptoms of depression over time. We hypothesized that children residing in neighborhoods with higher levels of strain would continue to exhibit more overall symptoms of mental health problems and depression symptoms over a two-year period. (3) Examine the potential mediating effect of maternal functioning and one aspect of the family environment, cohesion, as well as possible moderation by maternal depression (using both diagnostic history and present symptoms) at baseline. Our hypotheses were that the impact of neighborhood strain would be mediated by maternal functioning and family cohesion. Additionally, we expected that there would be an interaction effect between neighborhood context and maternal depression for both outcome variables, such that the effect of neighborhood strain would be stronger for children of mothers with a history of depression or greater present depression symptoms.
Methods
Study Sample
Data for this study were collected from a larger longitudinal study (n = 171) looking at child mental health outcomes for children of depressed and non-depressed mothers (see Tompson et al., 2010, for a detailed sample description). The study protocol was conducted in accord with appropriate ethical guidelines and under the approval of the Institutional Review Board at Boston University. This project analyzed data for the 156 dyads residing within Massachusetts. Approximately one third (33.3%) of the sample was non-white. Mean age of children and mothers was 10 (SD=1.4) and 42 (SD=5.9), respectively. Further sample characteristics can be found in Table 1. At the baseline assessment, 39.1% (N=61) of mothers had a depression diagnosis in the child’s lifetime. Diagnoses included major depressive disorder (MDD), dysthymic disorder (DD) and depressive disorder not otherwise specified (DD-NOS). After the initial baseline assessment, there were two follow-up assessments that occurred over a period of two years. Inclusion criteria included English-speaking, biological relationship between mother and child, and child residing with the mother for at least one year prior to study participation. Exclusion criteria included: a history of bipolar disorder, psychosis, brain injury, or pervasive developmental disorders.
Table 1.
Sample Characteristics
| (N=156) | |
|---|---|
| Child Age M (SD) | 10 (1.4) |
|
| |
| Gender N (%) | |
| Female | 64 (41.0) |
| Male | 92 (59.0) |
|
| |
| Child Racial/Ethnic Category N (%) | |
| European | 106 (67.9) |
| African-American | 22 (14.1) |
| Asian | 3 (1.9) |
| Hispanic | 10 (6.4) |
| Multiracial | 15 (9.6) |
|
| |
| Maternal Age M (SD) | 43 (5.8) |
Measures
Neighborhood indicators
The specific variables included: a) Criminal activity (as defined by regional violent and property crime rates per 100,000 persons); b) Poverty (as indicated by the percentage of residents at or below poverty level); and c) Residential instability (proportion of residents residing in a neighborhood for less than 5 years). Crime data were obtained based on participants’ neighborhood of residence. For the additional variables, U.S. Census tracts were identified for all subjects at baseline using the 2000 census tract classification, as that was the most recent full census prior to all participants’ enrollment. In total, there were 96 census tracts identified, out of which 79 (83%) represented areas in which 1 or 2 participants resided, 7 (16%) represented neighborhoods in which 3–4 participants resided, and 1 (1%) census tract included the residence of 5 participants.
Data were collected from publically available datasets (U.S. Census reports, 2000; Massachusetts Uniform Crime Reporting Database, 2005) according to the years that best fit the study period, which was 2004–2007. Research suggests that neighborhood conditions tend to be stable over as much as a 5-year period (Kunz, Page, & Solon 2003). Standardized z-scores were calculated for each neighborhood variable. Following previously established methods, these z-scores were summed to obtain an index of neighborhood strain (NSI), with higher values representing greater amounts of overall strain (Dulin-Keita et al., 2010). This aggregation method was used for several reasons. First, it is likely that a combination of stressors has a more deleterious impact on individuals than any one particular stressor (Evans, 2004), forming a larger stress context. Additionally, this aggregation method was supported by the fact that the indicators were so highly correlated and we had no particular hypotheses suggesting a differential impact of one indicator over any other.
Child behavior problems
Children’s overall symptoms of psychopathology were assessed using the Child Behavior Checklist (CBCL; Achenbach, 1991), a 118-item parent-report measure that captures a wide range of symptoms. The CBCL yields a Total Problems T-score, used for this analysis, as well as broad Internalizing and Externalizing dimensions. The CBCL has very good inter-rater and test-retest reliability (McConaughy, 1993) and good discriminant validity. For the purpose of this project, behavior problems refer to the total symptoms of mental health problems reported across both dimensions.
Childhood depression symptoms
Depressive symptoms in children were assessed by the Child Depression Inventory (CDI). The CDI (Kovacs, 1981) is a 27-item self-report measure of present depressive symptoms in children ages 7–17. Items assess main symptoms of depression and correspond with DSM-IV criteria. Items are scored on a 0–2 scale. Total score ranges from 0–54 with higher numbers reflective of greater severity. Research on the CDI demonstrates acceptable internal consistency with Cronbach’s α ranging from 0.71 to 0.87 (Brooks & Kutcher, 2001; Kovaks, Feinberg, Crouse-Novak, Paulauskas, & Finkelstein, 1984). Internal consistency in the current study was within this range (α = 0.78). Test-retest reliability has also been demonstrated to be high (Sorenson, Frydenberg, Thastum, & Thomsen, 2005).
Maternal depression symptoms and diagnosis
Maternal symptoms of depression were assessed dimensionally using the Beck Depression Inventory (BDI). The BDI is a 21-item self-report measure of present depressive symptoms (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) that correspond with DSM criteria. Responses on this measure are on a 4-point scale (0–3) and total scores range from 0–63. The BDI has high internal reliability (Beck, Steer, & Garbin, 1988). Internal consistency in this sample was high (α = 0.89) and consistent with a meta-analysis of 25 studies that found mean Cronbach’s α values for nonpsychiatric and psychiatric samples were 0.81 and 0.86 respectively (Beck et al., 1988).
For a depression diagnosis, mothers were assessed using the Structured Clinical Interview for the DSM-IV (First & Gibbon, 2004). Inter-rater agreement for depression-spectrum disorder diagnoses in the full study was high (n = 40; kappa = 0.95, p < 0.001).
Maternal functioning
Maternal functioning was assessed using the Global Assessment of Functioning (GAF). The GAF is a clinician-rated scale used to determine overall psychosocial functioning across a variety of domains. It is based on the Global Assessment Scale (Endicott, Spitzer, Fleiss, & Cohen, 1976) and is included in the DSM-IV. Clinicians take into account the degree to which psychopathology, life stressors, and other factors hinder functioning in daily living. Clinicians consider questions of impairment across settings such as the home (activities of daily living), work (ability to function and complete tasks), and interpersonal relationships (presence of and ability to develop and maintain meaningful relationships). It is scored on a scale of 1 to 100 (with 1 representing extreme illness and impairment, and 100 representing optimal health and no impairment). Startup, Jackson and Bendix (2002) examined the concurrent validity of the GAF and found high correlations with symptoms of psychopathology and social behavior. Inter-rater reliability in the present study was determined to be strong (ICC2,1 = .88).
Family environment
The Family Environment Scale (FES; Moos & Moos, 1994) is a 90-item self-report measure that includes ten subscales. This study included data from the cohesion subscale. The cohesion subscale assesses family members’ commitment to and support of each other. Research demonstrates good internal consistency and test-retest reliability (Moos & Moos, 1994). Internal consistency of the family cohesion subscale in the current study was adequate (α = 0.75). Data were based on maternal report.
Data Analysis
All data analyses were conducted using SPSS (version 21). Prior to conducting analyses, variables of interest were examined for normality; BDI and CDI scores were positively skewed and were thus transformed using square root transformation such that the transformed scales met standard tests for normality. Pearson correlations were run to assess bivariate correlations of baseline characteristics. Correlations for the following baseline variables were examined: neighborhood strain (NSI), childhood depression symptoms (CDI), child behavior problems (CBCL-T Scores), maternal functioning (GAF), maternal symptoms of depression (BDI), and family cohesion (FCoh). Hierarchical linear regression analysis was used for cross-sectional hypotheses. Mixed models for repeated measures with Maximum Likelihood Estimation were used to examine longitudinal trends. Time, NSI and their interaction were included as fixed effects, and time was also entered as a random effect to determine if variation over time was significant. Time was coded 0, 1, and 2 for the baseline and the two follow-up assessments that occurred at intervals of approximately one year.
Results
Initial bivariate correlations of baseline variables are presented in Table 2. The particular variables examined include neighborhood strain, child symptoms of mental health problems, child symptoms of depression, maternal functioning, family cohesion, and maternal depression symptoms.
Table 2.
Bivariate Correlations Among Neighborhood Strain, Childhood Depression Symptoms, Child Behavior Problems, Maternal Functioning, Family Cohesion & Maternal Depression Symptoms
| Subscale | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. NSI | -- | ||||
| 2. CDI | .11 | -- | |||
| 3. CBCL | .18* | .35** | -- | ||
| 4. Maternal GAF | −.21** | −.24** | −.43** | -- | |
| 5. Family Cohesion | −.06 | −.07 | −.42** | .39** | -- |
| 6. Maternal BDI | .31** | .15 | .46** | −.63** | −.37** |
Note: NSI = Neighborhood Strain Index; CDI = Children’s Depression Inventory; CBCL = Child Behavior Checklist; GAF = Global assessment of functioning; BDI = Beck Depression Inventory.
Correlations marked with an asterisk (*) were significant at p < .05. Correlations marked with two asterisks (**) were significant at p < .01.
Statistics & Data Analysis
Our first hypothesis that neighborhood strain would predict child psychopathology was upheld for overall mental health problems, but not depression symptoms. Hierarchical linear regression analyses were used to determine if NSI predicts child psychopathology, first examining CBCL total T scores while controlling for child age, child sex, and maternal age. The first regression equation including demographic variables only was not significant (R2 = .005, F (3,148) = .23, p = .87). The overall regression equation including NSI was a better predictor of CBCL total T scores but was not significant (R2 = .049, F (4,147) = 1.91, p = .11). However, NSI significantly correlated with CBCL total T scores when controlling for child age, sex and maternal age (see Table 3). It is interesting to note that although the correlations between neighborhood strain and overall CBCL total T scores were statistically significant, the correlations with the internalizing subscale and externalizing subscale trended towards, but did not reach, statistical significance.
Table 3.
Summary of Hierarchical Regression Analysis for Variables Predicting Child Behavior Problems
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Variable | B | SE B | β | B | SE B | β |
| Child Age | −.09 | .62 | −.01 | −.05 | .61 | −.01 |
| Child Gender | −.90 | 1.70 | −.04 | −.71 | 1.67 | −.04 |
| Maternal Age | .09 | .15 | .05 | .22 | .15 | .12 |
| Neighborhood Strain | .58 | .22 | .22** | |||
| R2 | .01 | .05 | ||||
| F for change in R2 | .23 | 6.92** | ||||
Correlations marked with an asterisk (*) were significant at p < .05. Correlations marked with two asterisks (**) were significant at p < .01.
A second hierarchical linear regression analysis was run to test whether NSI was a significant predictor of childhood depression symptoms after controlling for child and maternal demographic variable. The first step contained demographic variables only (child age, child sex, and maternal age). The model for this equation was not significant (R2 = .014, F (3,149) = .70, p = .56). Although the inclusion of NSI increased the model fit, the regression equation was still not significant (R2 = .032, F (4,148) = 1.21, p = .31). Examining the standardized coefficients demonstrated that none of the predictor variables significantly contributed to childhood depression symptoms (see Table 4).
Table 4.
Summary of Hierarchical Regression Analysis for Variables Predicting Childhood Depression Symptoms
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Variable | B | SE B | β | B | SE B | β |
| Child Age | −.07 | .06 | −.10 | −.07 | .06 | −.09 |
| Child Gender | −.07 | .17 | −.03 | −.05 | .17 | −.03 |
| Maternal Age | .01 | .01 | .07 | .02 | .02 | .12 |
| Neighborhood Strain | .04 | .02 | .14 | |||
| R2 | .01 | .03 | ||||
| F for change in R2 | .70 | 2.71 | ||||
Correlations marked with an asterisk (*) were significant at p < .05. Correlations marked with two asterisks (**) were significant at p < .01.
Our second hypothesis that NSI would predict child psychopathology from baseline to follow-up was not supported by the results. Since NSI was not significantly associated with childhood depression symptoms, childhood depression symptoms were not included in further analyses, with the exception of later moderation analyses. Mixed model analysis for repeated measures was used to examine the impact of NSI over time on CBCL total T scores. This method of analysis was used because of its robust ability to handle missing data and unbalanced groups. Results demonstrated that CBCL total T scores were 1.5 points lower at each follow-up, a slight, but significant decrease (SE = .949, t = 50.95, p < .001). However, there was no significant interaction effect between levels of NSI and time on CBCL total T scores, such that the rate of change of these scores from baseline through follow-ups 1 and 2 did not differ based on NSI levels (Table 5).
Table 5.
Summary of Mixed Model Analysis
| Estimate | SE | t | p | |
|---|---|---|---|---|
| Intercept | 48.33 | .95 | 50.95 | <.001 |
| Time | −1.50 | .32 | −4.62 | <.001 |
| Neighborhood Strain Index | .51 | .24 | 2.13 | .04 |
| Time X Neighborhood Strain Index | −.03 | .08 | −.30 | .76 |
Our third and fourth hypotheses looking at mediators and moderators of the relationship between NSI and childhood psychopathology were partially confirmed. Since NSI predicted overall symptoms of psychopathology based on CBCL total T scores, but did not predict child depression symptoms, mediational analysis was only conducted with CBCL total T scores as the dependent variable. First, we tested for maternal functioning as a possible mediator of the relationship between NSI and CBCL total T scores, and then family cohesion.
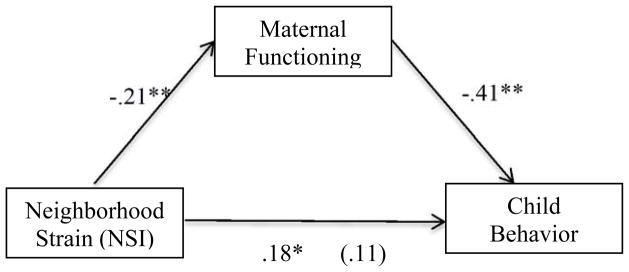
We ran a series of three regression equations, following standard methods of mediational analysis (Baron & Kenny, 1986). First, we regressed GAF onto NSI. The regression equation was significant, showing that NSI accounted for a portion of variance in GAF ratings, R2 = .04, F(1,151) = 6.86, p = .01. Next, we regressed CBCL total T scores onto NSI. The overall regression equation was significant, showing that NSI accounted for a portion of variance in CBCL total T scores, R2 = .03, F(1,153) = 5.32, p = .02. Examining the regression coefficients showed that NSI was a significant predictor of CBCL total T scores, β = −.18. With the first two mediation requirements satisfied, we conducted the final step, which was a multiple regression equation with GAF and NSI as the predictors. With GAF in the model, GAF significantly predicted CBCL total T scores, β = −.41, t(149) = −5.47, p < .001, and NSI was no longer a significant predictor of CBCL total T scores, β = .11, t(149) = 1.40, p = .16. These results demonstrate that the effect of NSI on CBCL is fully mediated by maternal GAF (figure 1).
Figure 1. Mediation analysis.
Standardized regression coefficients for the relationship between neighborhood strain (NSI) and child behavior problems (CBCL) as mediated by maternal functioning. Standardized regression coefficient between NSI and CBCL controlling for GAF is in parentheses. With GAF entered into the analysis as a mediator, the correlation between NSI and CBCL total T scores drops to .11, and is no longer statistically significant.
*p < .05, which represents the direct relationship without accounting for mediation.
**p < .01
Next, we tested for mediation by family cohesion. Contrary to our hypothesis, cohesion did not mediate the relationship between NSI and overall CBCL T scores. To test for mediation by cohesion, we began by regressing cohesion onto NSI. Results showed that NSI did not make a statistically significant contribution to the variance in the cohesion variable. Examining the regression coefficients showed that NSI was not a significant predictor of cohesion, β = −.056, t(154) = −.70, p = .49. In light of these results, no further analyses were warranted.
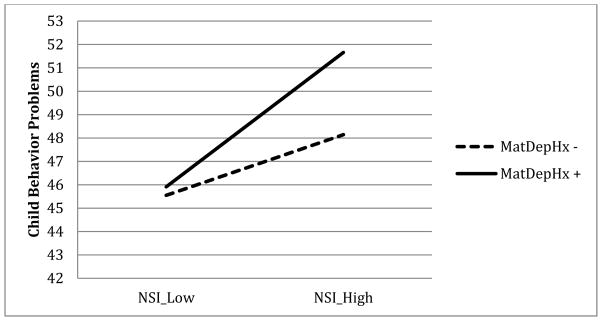
We next considered the possibility that children of mothers with higher depression symptoms or a past history of depression were more strongly impacted by the effects of neighborhood-level stressors. To address that question, we tested for potential moderation of the relationship between CBCL total T scores and NSI by maternal depression symptoms and past diagnostic history. An interaction term was created to be the product of the mean-centered NSI and maternal depression symptom scores, and a regression analysis was run with CBCL total T scores as the dependent variable and maternal depression symptoms, NSI and the interaction term entered as predictors. Results showed that the interaction between NSI and maternal symptoms of depression did not have a statistically significant contribution to the variance in CBCL total T scores, β = −.27, t(145) = −1.39, p = .17. A second moderation analysis was run to assess whether levels of NSI differentially predicted CBCL total T scores based on maternal depression history. The interaction effect trended towards significance, β =0.80, t(151)= 1.74, p= 0.08 (Figure 2; Table 6), such that for children whose mothers had a history of depression, NSI was predictive of higher CBCL total T scores as compared to children of mothers without a history of depression.
Figure 2. Maternal Depression History as Moderator.
Effect of neighborhood strain on child behavior problems (CBCL T scores) as moderated by maternal depression history. Low neighborhood strain is one standard deviation below the mean, high neighborhood strain is one standard deviation above the mean. Effect was not significant.
Table 6.
Summary of Moderation Analysis
| Coeff. | SE | t | p | ||
|---|---|---|---|---|---|
| Intercept | i1 | 46.81 | 0.81 | 58.01 | <.001 |
| Neighborhood Strain Index (X) | b1 | 0.41 | 0.23 | 1.82 | 0.07 |
| Maternal Depression Diagnostic History (M) | b2 | 2.23 | 1.71 | 1.3 | 0.19 |
| Neighborhood Strain Index X Maternal Depression Diagnostic History (XM) | b3 | 0.8 | 0.45 | 1.74 | 0.08 |
| R2 = .0697 | |||||
| F(3,151) = 3.30, p = .022 | |||||
Finally, we tested whether maternal depression moderated the impact of neighborhood strain on child depression symptoms. Neither present maternal symptoms of depression nor prior history of a depression diagnosis was found to be a statistically significant moderator.
Discussion
In this study, we examined the effect of neighborhood strain on children’s mental health outcomes using data from a longitudinal observational study of children of mothers with and without a history of depression. Four findings were particularly noteworthy. The first was that neighborhood strain was a significant predictor of child mental health problems more broadly, but not of childhood depression symptoms specifically. Second, neighborhood strain did not moderate the effect of time on child mental health problems, such that symptoms changed at similar rates regardless of the level of neighborhood-level strain. Third, maternal functioning fully mediated the relationship between NSI and child mental health problems, though family cohesion was not a mediator of this relationship. Finally, neither maternal history of depression diagnosis nor present symptoms of depression moderated the relationship between neighborhood strain and child mental health problems.
The significant effect of neighborhood strain on overall child mental health problems is in line with research that links neighborhood problems to childhood symptoms of psychopathology. Researchers have found that neighborhood conditions correlate with externalizing problems in children and adolescents (Plybon & Kliewer, 2001) as well as total problems overall (Caughy, Nettles, & O’Campo, 2008). In a study of adolescents, negative parental perceptions of neighborhood conditions were also associated with adolescent depressive symptoms in particular (Ford & Rechel, 2012). Our results did not show an effect of neighborhood strain on children’s depression symptoms. The lack of significant correlation in the present study may be a result of the lower base rate of childhood depression as compared to adolescent depression, which would require a larger sample to detect an actual effect should one exist. Alternatively, it may be that only some neighborhood factors are associated with depressive symptoms. The impact of neighborhood violence may not be as salient to child outcomes as other factors, such as poverty and other measures of neighborhood disorder (Plybon & Kliewer, 2001; Garbarino & Kostelny, 1996). Therefore, our aggregated variable of neighborhood strain may have masked links to specific ecological contributors of risk for child psychopathology. Neighborhood characteristics were also not significantly correlated with internalizing symptoms based on maternal report, which is consistent with the lack of correlation with depressive symptoms.
It is also noteworthy that neighborhood strain significantly correlated with overall child mental health problems, but not with either the internalizing or externalizing subscales, although the correlations trended towards significance. This raises the question of what was driving the statistically significant correlation between NSI and CBCL total T scores? The CBCL total T score is comprised of a much larger number of items, as it includes both the externalizing and internalizing subscales. It may be that the larger number of items allowed the statistically significant relationship to be captured.
Although much research has examined the effect of neighborhood strain on child mental health, there is less data on potential mechanisms of effects. In this study, we found that overall maternal functioning fully explained the relationship between neighborhood strain and overall child mental health symptoms. Maternal functioning is a global construct that captures how mothers function across a variety of domains. In particular, it serves as an indicator of the extent to which there is functional impairment in various areas of one’s life (e.g., interpersonal relationships, family, work, and activities of daily living). Neighborhood strain as a chronic stressor may impede maternal functioning across each of these areas. One possibility is that the stress increases cognitive load, depleting available resources needed for optimal functioning in each area. Decreased overall functioning could conceivably impact parental practices, which is commonly associated with both neighborhood strain and child outcomes (Pinderhughes et al., 2001). Finally, in a correlational analysis, one cannot determine the direction of effects. As such, it may be that mothers with poorer mental functioning tend to reside in neighborhoods with higher levels of chronic stress.
We also examined the role of maternal depression as a potential moderator of the relationship between neighborhood strain and CBCL total T scores. Present depressive symptoms did not moderate this relationship. For children of mothers with a history of depression, greater levels of neighborhood strain did predict higher CBCL total T scores. Although the findings were not statistically significant, it is interesting to note that maternal history of depression seems to be more of a factor than present symptoms when considering the relationship between neighborhood strain and child mental health problems. One reason could be that a history of a depression diagnosis may be more indicative of a protracted course of depression than present symptoms. It may be that a chronic condition is more salient when examining interaction effects with a chronic source of strain such as neighborhood effects.
Another mechanism of effects hypothesized to influence the relationship between NSI and child outcomes was family cohesion. We expected that neighborhood strain would predict lower ratings of family cohesion and that family cohesion would mediate the relationship between neighborhood strain and child outcomes. However, our results did not support this hypothesis. Other researchers did find that greater neighborhood strain had a negative impact on the family environment (Kohen et al., 2008), which may be due to different methods of measuring family environment. Kohen and colleagues (2008) utilized a measure of “general family functioning,” which captured such components as communication and problem solving in situations such as “planning family activities” and “[making] decisions.” Although potentially related to cohesion, these constructs may be distinct. It may also be that different aspects of the neighborhood environment have an impact on family functioning. It may be that the particular groups of risk factors vary in their impact across different outcomes at the individual and family level. Future research might benefit from examining risk factors independently as well as in aggregation. However, it is still important to utilize aggregate means, as no one neighborhood-level risk factor operates in isolation (Plybon & Kliewer, 2001).
Strengths & Limitations
This study added to the research knowledge of the field by examining mechanisms of cross sectional effects in addition to whether levels of neighborhood strain related to child outcomes differently over three time-points. Few studies examine neighborhood effects in relation to children broadly, and middle-childhood in particular. In addition, this work addressed this question from a broader ecological approach to test the impact of neighborhood strain on the child. This type of work offers the possibility of providing a fuller picture of the etiological course of child psychopathology.
There were several study limitations. First, the actual number of residents from areas reflecting higher neighborhood strain may not have been large enough to detect a significant difference in all our variables of interest. However, the fact that we did find significant cross-sectional correlations in spite of this sampling challenge lends support to the likelihood that the findings may be an accurate reflection of the relationship. Second, crime data was collected at a higher level (town) than the other neighborhood strain factors (census tract). The impact on the data is that crime levels were more broadly generalized and may not be as reflective of the actual criminal activity within the census tracts in which an individual subject resided. The particular census tract may have had more or less crime, so it is difficult to say in which direction this measurement limitation may have biased the results, but it is likely to have the greatest impact for residents of large, diverse communities. Data for individuals from lower crime areas of a city could result in an overestimation in crime, and data for individuals from higher crime areas could result in an underestimation. This increases error in the neighborhood strain index. The likely result is a weakened ability to find statistical correlations and predictive relationships that actually may exist. Third, the inclusion of only objective measures of neighborhood strain may be seen as a limitation in this study, as it does not capture subjective experiences of the neighborhood environment. However, objective measures avoid potential informant bias, as reports of subjective experiences are influenced by mental health. Fourth, the particular community-level stressors chosen may not fully capture the effects of neighborhood strain. More research is needed to identify the particular factors at the community/neighborhood level that contribute to this constellation of risk.
Future Directions of Research
Collective efficacy
One more recent finding is that neighborhood stress erodes collective efficacy, or the sense that the neighborhood can work together for the good of the entire community (Odger, et al., 2009). This construct may serve as a proxy for social support. High collective efficacy seems to play a role in buffering effects of neighborhood strain on children and families, particularly in disadvantaged neighborhoods (Odger, et al., 2009). This factor could explain some of the inconsistent results for the effects of neighborhood stressors on youth. Research that does not assess this construct may suffer from unmeasured variable bias. When neighborhood factors do not have a statistically significant effect on outcomes in the face of high neighborhood strain, it may be that collective efficacy is also high. But if this is not assessed, researchers would not know whether the factors were truly unrelated, or if the presence of an unmeasured variable made it appear as such. This highlights the need to include measures of collective efficacy in future research on the effects of neighborhood strain.
Research on neighborhood-level risk factors, such as those examined in this study, has increased in the past few decades. However, the results of the association between neighborhood outcomes and child mental health are not always clear. Methodological inconsistencies may partly explain these divergent findings. More standardized practices and procedures could help answer key questions such as which factors are important to consider for which outcomes (e.g., poverty versus crime versus neighborhood instability). Efforts should be directed towards creating a standardized process of measuring and modeling the effects of neighborhood strain on child mental health. Additionally, it would be important to assess the impact of such variables across development, as the developmental stage of the child may buffer or increase the effect of neighborhood factors on child outcomes.
Research efforts also need to ensure that data on measures of neighborhood strain accurately reflect the environment in which the person resides. In areas as socioeconomically diverse as Massachusetts, this would likely require data at the census tract level or smaller. For more homogeneous regions, zip code level data may be sufficient. The geographic variability in demographic and socio-economic trends would help determine which level of data is most appropriate for consideration.
Future research would benefit from including multi-informant data on mental health outcomes of interest in children, collecting data on parenting practices and the parent-child relationship, and including both subjective and objective measures of chronic strain. In order to mitigate the effect of potential informant bias on subjective experiences of stressors, biological measures should be used (e.g., neuroendocrine functioning). These recommendations should allow the field to gain a better understanding of the extent to which neighborhoods matter in the risk, onset, and course of childhood psychopathology.
Acknowledgments
The current work was supported by the following grants from the National Institutes of Health, National Institute of Mental Health MH066077, MH082861, PI: Martha C. Tompson, Ph.D. and MH082861S1, PI: Gail N. Kemp, M.A., M.P.H.
References
- Achenbach TM, Howell CT, Quay HC, Conners CK. National survey of problems and competencies among four- to sixteen-year-olds: Parents’ reports for normative and clinical samples. Monographs of the Society for Research in Child Development. 1991;56(3):1–131. [PubMed] [Google Scholar]
- Aneshensel CS, Sucoff CA. The neighborhood context of adolescent mental health. Journal of Health and Social Behavior. 1996;37(4):293–310. [PubMed] [Google Scholar]
- Aneshensel CS, Wight RG, Miller-Martinez D, Botticello AL, Karlamangla AS, Seeman TE. Urban neighborhoods and depressive symptoms among older adults. Journals Of Gerontology: Series B: Psychological Sciences and Social Sciences. 2007;62B(1):S52–S59. doi: 10.1093/geronb/62.1.s52. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. Moderator-mediator variables distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TR. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock JE, Erbaugh JK. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Black JL, Macinko J, Dixon LB, Fryer GE. Neighborhoods and obesity in New York City. Health & Place. 2010;16:489–499. doi: 10.1016/j.healthplace.2009.12.007. [DOI] [PubMed] [Google Scholar]
- Boardman JD, Saint Onge JM. Neighborhoods and adolescent development. Child Youth Environment. 2005;15:138–164. [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U. Toward an experimental ecology of human development. American Psychology. 1977;32:513–531. [Google Scholar]
- Bronfenbrenner U. The International Encyclopedia of Education. 2. NY: Elsevier Science; 1994. Ecological models of human development. [Google Scholar]
- Brooks SJ, Kutcher S. Diagnosis and measurement of adolescent depression: a review of commonly utilized instruments. Journal of Child and Adolescent Psychopharmacology. 2001;11:341–376. doi: 10.1089/104454601317261546. [DOI] [PubMed] [Google Scholar]
- Caughy MO, Franzini L, Windle M, Dittus P, Cuccaro P, Elliott MN, Schuster MA. Social competence in late elementary school: Relationships to parenting and neighborhood context. Journal of Youth and Adolescence. 2012;41(12):1613–1627. doi: 10.1007/s10964-012-9779-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caughy MO, Nettles SM, O’Campo PJ. Community influences on adjustment in first grade: An examination of an integrated process model. Journal of Child and Family Studies. 2007;16(6):819–836. [Google Scholar]
- Caughy MO, Nettles SM, O’Campo PJ. The effect of residential neighbourhood on child behavior problems in first grade. American Journal of Community Psychology. 2008;42:39–50. doi: 10.1007/s10464-008-9185-9. [DOI] [PubMed] [Google Scholar]
- Caughy MO, O’Campo PJ, Muntaner C. When being alone might be better: neighborhood poverty, social capital, and child mental health. Social Science & Medicine. 2003;57:227–37. doi: 10.1016/s0277-9536(02)00342-8. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Wallace G, Wesner KA. Neighborhood characteristics and depression: An examination of stress processes. Current Directions in Psychological Science. 2006;15(4):188–192. doi: 10.1111/j.1467-8721.2006.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulin-Keita A, Casazza K, Fernandez JR, Goran MI, Gower B. Do neighborhoods matter? Neighborhood disorder and long-term trends in serum cortisol levels. Journal of Epidemiology & Community Health. 2010;66:24–29. doi: 10.1136/jech.2009.092676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: A procedure for measuring overall severity of psychiatric disturbance. Archives of General Psychiatry. 1976;33(6):766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Ensel WM, Lin N. Distal stressors and the life stress process. Journal of Community Psychology. 1996;24(1):66–82. [Google Scholar]
- Evans GW. The Environment of Childhood Poverty. American Psychologist. 2004;59(2):77–92. doi: 10.1037/0003-066X.59.2.77. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M. The structured clinical interview for DSM-IV axis I disorders (SCID-I) and the structured clinical interview for DSM-IV axis II disorders (SCID-II) In: Hilsenroth MJ, Segal DL, editors. Comprehensive handbook of psychological assessment, Vol. 2: Personality assessment. Hoboken, NJ: Wiley; 2004. pp. 134–143. [Google Scholar]
- Ford JL, Rechel M. Parental perceptions of the neighborhood context and adolescent depression. Public Health Nursing. 2012;29:390–402. doi: 10.1111/j.1525-1446.2012.01015.x. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Rudenstine S, Wallace Z, Vlahov D. Urban built environment and depression: A multilevel analysis. Journal of Epidemiology and Community Health. 2005;59(10):822–827. doi: 10.1136/jech.2005.033084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garbarino J, Kostelny K. The effects of political violence on Palestinian children’s behavior problems: A risk accumulation model. Child Development. 1996;67(1):33–45. [PubMed] [Google Scholar]
- Hadley-Ives E, Stiffman AR, Elze D, Johnson S, Dore P. Measuring neighborhood and school environments: Perceptual and aggregate approaches. Journal of Human Behavior in the Social Environment. 2000;3:1–28. [Google Scholar]
- Hammen C, Hazel NA, Brennan PA, Najman J. Intergenerational transmission and continuity of stress and depression: depressed women and their offspring in 20 years of follow-up. Psychological Medicine. 2012;42:931–42. doi: 10.1017/S0033291711001978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz LF, Kling JR, Liebman JB. Moving to opportunity in Boston: Early results of a randomized mobility experiment. The Quarterly Journal of Economics. 2001;116:607–54. [Google Scholar]
- Klebanov PK, Brooks-Gunn J, Chase-Lansdale PL, Gordon R. Are neighborhood effects on young children mediated by features of the home environment? In: Brooks-Gunn J, Duncan GJ, Aber JL, editors. Neighborhood poverty: Vol. 1. Context and consequences for children. New York: Russell Sage Foundation; 1997. pp. 119–145. [Google Scholar]
- Kohen DE, Leventhal T, Dahinten VS, McIntosh CN. Neighborhood disadvantage: pathways of effects for young children. Child Development. 2008;79:156–169. doi: 10.1111/j.1467-8624.2007.01117.x. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Paedopsychiatria. 1981;46(5–6):305–315. [PubMed] [Google Scholar]
- Kovacs M, Feinberg TL, Crouse-Novak MA, Paulauskas SL, Finkelstein R. Depressive disorders in childhood. I. A longitudinal prospective study of characteristics and recovery. Archives of General Psychiatry. 1984;41:229–237. doi: 10.1001/archpsyc.1984.01790140019002. [DOI] [PubMed] [Google Scholar]
- Kunz J, Page ME, Solon G. Are point-in-time measures of neighborhood characteristics useful proxies for children’s long-run neighborhood environment? Economic Letters. 2003;79:231–237. [Google Scholar]
- Latkin CA, Curry AD. Stressful neighborhoods and depression: A prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior. 2003;44:34–44. [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. Moving to opportunity: An experimental study of neighborhood effects on mental health. American Journal of Public Health. 2003;93:1576–1582. doi: 10.2105/ajph.93.9.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ludwig J, Duncan GJ, Gennetian LA, Katz LF, Kessler RC, Kling JR, Sanbonmatsu L. Neighborhood effects on the long-term well-being of low-income adults. Science. 2012;337(6101):1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luebbe AM, Bell DJ. Positive and negative family emotional climate differentially predict youth anxiety and depression via distinct affective pathways. Journal of Abnormal Child Psychology. 2014;42(6):897–911. doi: 10.1007/s10802-013-9838-5. [DOI] [PubMed] [Google Scholar]
- Mair CF, Diez-Roux AV, Galea S. Are neighborhood characteristics associated with depressive symptoms? A critical review. Journal of Epidemiological & Community Health. 2008;62:940–946. doi: 10.1136/jech.2007.066605. [DOI] [PubMed] [Google Scholar]
- McConaughy SH. Advances in empirically based assessment of children’s behavioral and emotional problems. School Psychology Review. 1993;22(2):285–307. [Google Scholar]
- Moos R, Moos B. Family Environment Scale manual: Development, applications, research - Third Edition. Palo Alto, CA: Consulting Psychologist Press; 1994. [Google Scholar]
- Murray L, Arteche A, Fearan P, Halligan S, Goodyer I, Cooper P. Maternal postnatal depression and the development of depression in offspring up to 16 years of age. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:460–470. doi: 10.1016/j.jaac.2011.02.001. [DOI] [PubMed] [Google Scholar]
- Odger CL, Moffitt TE, Tach LM, Sampson RJ, Taylor A, Matthews CL, Caspi A. The protective effects of neighborhood collective efficacy on British children growing up in deprivation: A developmental analysis. Developmental Psychology. 2009;45:942–957. doi: 10.1037/a0016162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogburn KM, Sanches M, Williamson DE, Caetano SC, Olvera RL, Pliszka S, … Soares JC. Family environment and pediatric major depressive disorder. Psychopathology. 2010;43(5):312–318. doi: 10.1159/000319400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paczkowski MM, Galea S. Sociodemographic characteristics of the neighborhood and depressive symptoms. Current Opinion in Psychiatry. 2010;23(4):337–341. doi: 10.1097/YCO.0b013e32833ad70b. [DOI] [PubMed] [Google Scholar]
- Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. Journal of Epidemiological & Community Health. 2001;55:111–22. doi: 10.1136/jech.55.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinderhughes EE, Nix R, Foster EM, Jones D. Parenting in context: Impact of neighborhood poverty, residential stability, public services, social networks, and danger on parental behaviors. Journal of Marriage and Family. 2001;63(4):941–953. doi: 10.1111/j.1741-3737.2001.00941.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plybon LE, Kliewer W. Neighborhood types and externalizing behavior in urban school-age children: Tests of direct, mediated, and moderated effects. Journal of Child and Family Studies. 2001;10(4):419–437. [Google Scholar]
- Sorensen MJ, Frydenberg M, Thastum M, Thomsen PH. The Children’s Depression Inventory and classification of major depressive disorder: validity and reliability of the Danish version. European Child & Adolescent Psychiatry. 2005;14:328–334. doi: 10.1007/s00787-005-0479-2. [DOI] [PubMed] [Google Scholar]
- Startup M, Jackson MC, Bendix S. The concurrent validity of the Global Assessment of Functioning (GAF) British Journal of Clinical Psychology. 2002;41(4):417–422. doi: 10.1348/014466502760387533. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Morris AS. Adolescent development. Annual Review of Psychology. 2001;52:83–110. doi: 10.1146/annurev.psych.52.1.83. [DOI] [PubMed] [Google Scholar]
- Tendulkar SA, Buka S, Dunn EC, Subramanian SV. A multilevel investigation of neighborhood effects on parental warmth. Journal of Community Psychology. 2010;38:557–573. [Google Scholar]
- Tennant C. Life events, stress and depression: a review of recent findings. Australian and New Zealand Journal of Psychiatry. 2002;36:173–182. doi: 10.1046/j.1440-1614.2002.01007.x. [DOI] [PubMed] [Google Scholar]
- Tompson MC, Pierre CB, Dingman Boger K, McKowen JW, Chan PT, Freed RD. Maternal depression, maternal expressed emotion, and youth psychopathology. Journal of Abnormal Child Psychology. 2010;38:105–117. doi: 10.1007/s10802-009-9349-6. [DOI] [PubMed] [Google Scholar]
- Tompson MC, McKowen JW, Asarnow JR. Adolescent mood disorders and familial processes. In: Allen NB, Sheeber L, editors. Adolescent Emotional Development and the Emergence of Depressive Disorders. Chapter 15. London, UK: Cambridge University Press; 2009. pp. 280–298. [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Verdeli H, Pilowsky DJ, Grillon C, Bruder G. Families at high and low risk for depression: a 3-generational study. Archives of General Psychiatry. 2005;51:734–744. doi: 10.1001/archpsyc.62.1.29. [DOI] [PubMed] [Google Scholar]
- Williams DR, Williams-Morris R. Racism and mental health: The African American experience. Ethnicity & Health. 2000;5:243–268. doi: 10.1080/713667453. [DOI] [PubMed] [Google Scholar]
- Wilson WJ. The truly disadvantaged. Chicago: University of Chicago Press; 1987. [Google Scholar]
- Xue Y, Leventhal T, Brooks-Gunn J, Earls FJ. Neighborhood residence and mental health problems of 5- to 11-year-olds. Archives of General Psychiatry. 2005;62:554–563. doi: 10.1001/archpsyc.62.5.554. [DOI] [PubMed] [Google Scholar]
- Yingling F, Qian C. Family functioning as a mediator between neighborhood conditions and children’s health: Evidence from a national survey in the United States. Social Science & Medicine. 2012;74(12):1939–1947. doi: 10.1016/j.socscimed.2012.01.039. [DOI] [PubMed] [Google Scholar]