Abstract
PURPOSE
Bahçeşehir Breast Cancer Screening Program is a population based organized screening program in Turkey, where asymptomatic women aged 40–69 years are screened biannually. In this prospective study, we aimed to determine the mammographic findings of screen-detected cancers and discuss the efficacy of breast cancer screening in a developing country.
METHODS
A total of 6912 women were screened in three rounds. The radiologic findings were grouped as mass, focal asymmetry, calcification, and architectural distortion. Masses were classified according to shape, border, and density. Calcifications were grouped according to morphology and distribution. Cancers were grouped according to the clinical stage.
RESULTS
Seventy cancers were detected with an incidence of 4.8/1000. Two cancers were detected in other centers and three were not visualized mammographically. Mammographic presentations of the remaining 65 cancers were mass (47.7%, n=31), calcification (30.8%, n=20), focal asymmetry (16.9%, n=11), architectural distortion (3.1%, n=2), and skin thickening (1.5%, n=1). The numbers of stage 0, 1, 2, 3, and 4 cancers were 13 (20.0%), 34 (52.3%), 14 (21.5%), 3 (4.6%), and 1 (1.5%), respectively. The numbers of interval and missed cancers were 5 (7.4%) and 7 (10.3%), respectively.
CONCLUSION
A high incidence of early breast cancer has been detected. The incidence of missed and interval cancers did not show major differences from western screening trials. We believe that this study will pioneer implementation of efficient population-based mammographic screenings in developing countries.
Breast cancer is the most common cancer affecting women worldwide, with about 1.4 million new cases diagnosed each year (1). The incidence of breast cancer is about four-fold higher in developed countries (2). However, it has been shown that in low and middle-income populations, the number of breast cancer cases is increasing at a faster rate compared with high-income countries (3). In Turkey, breast cancer incidence is 46.8/100,000 and has more than doubled in the last two decades due to a westernizing life style and aging (1, 4). The Bahçeşehir Breast Cancer Screening Program is a population-based organized screening program that began in 2008, in which asymptomatic women aged between 40–69 years are screened for 10 years biannually. In this prospective study, we aimed to determine whether the mammographic findings of screen-detected cancers correlated with histopathologic findings and discuss the efficacy of breast cancer screening in a developing country.
Methods
Study population
Screening mammography was performed in women aged 40–69 years who lived in Bahçeşehir and who accepted the screening invitation. Pregnant women, women with a previous diagnosis of breast cancer and women who had a mammography in the last two years were excluded. Screening was registered to the Bahçeşehir Breast Cancer Screening Center between January 2009 and October 2014 every two years in three screening rounds. An approval by Institutional Review Board of Bahçeşehir University was obtained. National Health Authorities were informed and approval was obtained. Each eligible woman signed a written informed consent form.
Screening procedure
A full-field digital mammography system was used (Selenia, Hologic). Bilateral mammograms were obtained including mediolateral oblique (MLO) and craniocaudal (CC) projections. All examinations were double read by two independent radiologists (A. K. and O. C.) with eight years of experience who were blinded to each other’s interpretations. Mammographic findings and breast parenchymal patterns were assessed in accordance with the Breast Imaging Reporting and Data System (BIRADS) of the American College of Radiology (ACR) (Reston, 2003). The final decision was made according to the highest BIRADS score. When there was a discrepancy between the readers as to whether to follow-up or perform a histopathologic confirmation, the final assessment was determined in consensus. Women with mammograms categorized as BIRADS 0 (incomplete, need additional imaging assessment) were recalled for additional work-up including spot compression and magnification mammogram, or ultrasonography (US). A follow-up US was performed to all women with type 3 and 4 breasts during a period not exceeding two weeks following the first round screening mammogram. The histopathologic confirmation for BIRADS scores of 4 and 5 lesions was made using a US-guided core (14-gauge) needle biopsy (n=20), vacuum assisted large core (11-gauge) stereotactic (VALCS) biopsy (n=11), wire-guided excisional breast biopsy (n=2), and excisional breast biopsy (n=37).
Outcome measurements
The women were grouped according to age as 40–49 and 50–69 years. For each breast, the localization of mammographically-detected abnormalities were grouped as upper-outer, upper-inner, lower-outer, and lower-inner quadrants, central, retroareolar, and axillary. The radiologic presentation of cancers were classified as mass, focal asymmetry, calcification, and architectural distortion.
Masses were classified according to their shape, border, and density. The shape of masses were grouped as round, oval, lobular, and irregular. The borders of masses were grouped as well-circumscribed, microlobular, obscured, irregular, and spiculated. The density of masses were classified as high, intermediate, low density, and fat-containing. Calcifications were grouped as heterogeneous, amorphous, pleomorphic, and fine linear according to their morphology. The distribution of calcifications were grouped as diffuse, regional, clustered, segmental, and linear. The presence or absence of axillary lymph nodes were noted. Mass was considered as the dominant finding in mammograms with a finding of mass associated with calcification. Cancers were also grouped according to the clinical stage to assess the distribution of early and invasive cancers as follows: stage 0 (in situ cancer), stage 1 and stage 2 (early invasive cancer), stage 3 (locally advanced cancer) and stage 4 (metastatic cancer).
The radiologic findings of interval cancers (cancer detected in women who were referred to the screening center with symptoms within one year of the last round with a negative mammogram) and missed cancers (cancer detected after a negative mammogram) were assessed.
Statistical analysis
The continuous distributions of variables were evaluated with Kolmogorov-Smirnov test. In addition, Spearman’s correlation analysis, chi-square test, Mann-Whitney U, and the Fisher-Freeman-Halton tests were performed. The statistical significance level was determined as P < 0.05. All analyses were performed using SPSS program version 11.0 (SPSS Inc.).
Results
A total of 6912 women were screened between January 2009 and October 2014, and 14485 bilateral mammographies were performed. A total of 70 cancers were detected, yielding an incidence of 4.8/1000. Two cancers were detected in other centers but the radiologic findings could not be obtained. Three cancers were solely detected under US and could not be visualized on mammography. Therefore, the statistical analysis was performed on a total of 65 cancers.
The number of cancers detected in the 40–49-year age group and the 50–69-year age group were 32 (45.7%) and 38 (54.3%), respectively. Of 68 cancers, 39 (57.3%) were located in the right breast and 29 (42.6%) were in the left breast. Cancers were located in the upper-outer quadrant (n=45, 66.2%), upper-inner quadrant (n=6, 8.8%), lower-inner quadrant (n=4, 5.9%), lower-outer quadrant (n=3, 4.4%), retroareolar (n=3, 4.4%), central (n=3, 4.4%), and axillary (n=4, 5.9%). Axillary lymphadenopathy was present in seven cases (10.2%) on mammogram.
In the first screening round, US was performed in women with type 3 and 4 breast parenchyma by the same radiologist who read the mammograms. All three cancers detected solely under US had type 3 breast parenchymal pattern, presenting a mass obscured by dense glandular parenchyma.
Of the 65 mammographically-detected cancers, the majority presented as a mass (n=31, 47.7%), followed by calcification (n=20, 30.8%), focal asymmetry (n=11, 16.9%), architectural distortion (n=2, 3.1%), and skin thickening (n=1, 1.5%) as shown in Table 1. Of the 32 cancers detected in women aged 40–49 years, three were not visible on mammogram and were detected solely under US. The mammographic presentation of the remaining 29 cancers were as follows: mass (n=3, 44.8%), calcification (n=10, 34.5%), focal asymmetry (n=5, 17.3%) and architectural distortion (n=1, 3.4%). In women aged 50–69 years, 38 cancers were detected of which, two were detected in external centers and radiologic findings could not be obtained. The mammographic findings of the remaining 36 cancers were as follows: mass (n=18, 50.0%), calcification (n=10, 27.8%), focal asymmetry (n=6, 16.6%), and architectural distortion (n=1, 2.8%). In one woman (2.8%), only skin thickening was detected (Table 1).
Table 1.
Distribution of radiologic findings of screen detected cancers according to age groups
| Radiologic presentation of cancers (n=65)* | 40–49 years n (%) |
50–69 years n (%) |
Total n (%) |
|---|---|---|---|
| Mass | 13 (44.8) | 18 (50.0) | 31 (47.7) |
| Calcifications | 10 (34.5) | 10 (27.8) | 20 (30.8) |
| Focal asymmetry | 5 (17.3) | 6 (16.6) | 11 (16.9) |
| Architectural distortion | 1 (3.4) | 1 (2.8) | 2 (3.1) |
| Skin thickening | 0 (0.0) | 1 (2.8) | 1 (1.5) |
| Total | 29 (100.0) | 36 (100.0) | 65 (100.0) |
No significant difference was found between the age groups (P = 0.984, Fisher-Freeman-Halton test).
Three cancers could not be visualized on mammography, while two cancers were detected in other centers and the radiologic findings could not be obtained.
Two patients presented with focal asymmetry associated with calcifications; these patients were included in the calcification group because the calcifications were more remarkable. The characteristics of cancers presenting with a mass and calcifications are shown in Table 2. In one patient with a type 4 breast parenchyma, the only mammographic finding was skin thickening. Cancer was detected using US, which revealed a periareolar irregular solid mass.
Table 2.
Characteristics of screen-detected cancers that presented as mass and calcification
| Mass (n=31) | n (%) |
|---|---|
| Shape | |
| Irregular | 26 (83.9) |
| Round | 3 (9.7) |
| Oval | 2 (6.4) |
|
| |
| Margin | |
| Spiculated | 15 (48.4) |
| Irregular | 14 (45.2) |
| Well-defined | 2 (6.4) |
| Microlobular | 0 (0.0) |
| Obscured | 0 (0.0) |
|
| |
| Density | |
| Dense | 19 (61.3) |
| Intermediate density | 10 (32.3) |
| Low density | 2 (6.4) |
| Fat containing | 0 (0.0) |
|
| |
| Calcification (n=20) | |
|
| |
| Type | |
| Pleomorphic | 8 (40.0) |
| Heterogeneous | 6 (30.0) |
| Amorphous | 6 (30.0) |
| Fine linear | 0 (0.0) |
|
| |
| Distribution | |
| Segmental | 15 (75.0) |
| Regional | 5 (25.0) |
| Diffuse | 0 (0.0) |
| Clustered | 0 (0.0) |
| Linear | 0 (0.0) |
The distribution of histopathologic types of cancers are shown in Table 3. Cancers were staged as stage 0 (n=13, 20.0%), stage 1 (n=34, 52.3%), stage 2 (n=14, 21.5%), stage 3 (n=3, 4.6%), and stage 4 (n=1, 1.5%). Of the total stage 0 and 1 cancers, 15 (31.9%) presented as calcifications, whereas 22 (46.8%) presented as a mass.
Table 3.
Histopathologic types of screen-detected cancers
| Histopathologic type of cancers | n (%) |
|---|---|
| Invasive ductal | 41 (58.6) |
| DCIS | 12 (17.1) |
| DCIS intracystic papillary carcinoma | 1 (1.4) |
| Invasive lobular | 10 (14.3) |
| Mixed | 2 (2.9) |
| Tubular carcinoma | 3 (4.3) |
| Mucinous carcinoma | 1 (1.4) |
| Total | 70 (100) |
The radiologic and histopathologic correlation of tumor dimension was evaluated only for masses. The median diameter of 31 mammographically-detected masses was 16 mm (range, 6.0–47 mm), whereas the histopathologic median tumor diameter was 15 mm (range, 5.0–35 mm). Therefore, the radiologic assessments significantly correlated with the pathologic findings (r=0.675, P = 0.0001). The distribution of 6912 mammograms according to parenchymal pattern type 1, 2, 3, and 4 was 41.1%, 40.9%, 15.8%, and 2.2%, respectively. The breast parenchymal patterns of the 56 breast cancer patients that were detected in our center were as follows: type 1 (n=15, 26.8%), type 2 (n=36, 64.3%), type 3 (n=3, 5.4%), and type 4 (n=2, 3.6%). Cancers that presented as a mass were mostly seen in type 2 breast parenchymal pattern followed by types 1, 3, and 4, respectively. Calcifications were mostly seen in type 2 followed by type 1, type 4 and type 3, respectively. The distribution of radiologic findings according to breast parenchymal pattern is shown in Table 4. Of the 68 cancers, 56 (82.4%) were detected in routine screening rounds, five (7.4%) were interval cancers and seven (10.3%) were missed cancers.
Table 4.
Distribution of radiologic findings of screen detected cancers according to breast parenchymal pattern
| Radiologic findings (n=65) | Breast density n (%) | ||||
|---|---|---|---|---|---|
| Type 1 almost entirely fat | Type 2 scattered fibroglandular | Type 3 heterogeneously dense | Type 4 very dense | Total | |
| Mass | 9 (56.3) | 19 (48.7) | 2 (33.3) | 1 (25.0) | 31 (47.7) |
| Calcification | 4 (25.0) | 13 (33.3) | 1 (16.7) | 2 (50.0) | 20 (30.8) |
| Focal asymmetry | 3 (18.8) | 6 (15.4) | 1 (16.7) | 1 (25.0) | 11 (16.9) |
| Architectural distortion | 0 | 1 (2.6) | 1 (16.7) | 0 | 2 (3.1) |
| Skin thickening | 0 | 0 | 1 (16.7) | 0 | 1 (1.5) |
| Total | 16 (100) | 39 (100) | 6 (100) | 4 (100) | 65 (100) |
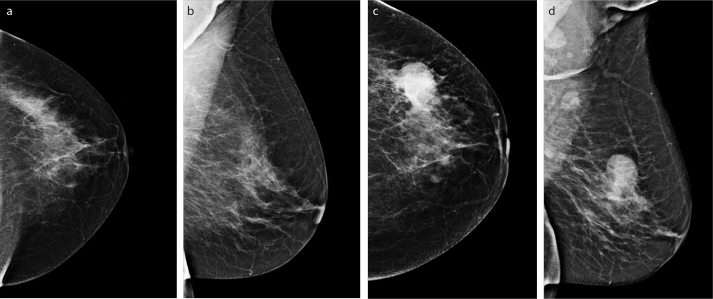
Of five patients with interval cancers, one patient (20%) with symptoms of breast pain was seen at our screening center four months before her routine screening round, and a focal asymmetry in a type 1 breast parenchymal pattern was detected on a follow-up mammogram. Two interval cancers (%40) were detected in type 2 breast parenchyma. Of those, one was detected in an external center one month before the third screening round, which presented as calcification. The second woman had a palpable breast mass one year following the screening before the round was completed, and a de novo mass was detected in the follow-up mammogram (Fig 1). One (20%) interval cancer, which was detected in a type 3 breast, presented as a palpable mass six months before the second round. Finally, one of the interval cancers was detected in a patient with a complaint of nipple discharge in a type 4 breast nine months after screening, and presented with retroareolar focal asymmetry.
Figure 1.
a–d. Left negative mammogram with a type 2 parenchymal pattern in an asymptomatic woman in 2011 (a, b). In 2012, a developing mass was detected in the upper-outer quadrant with an obscured inferior medial border (c, d).
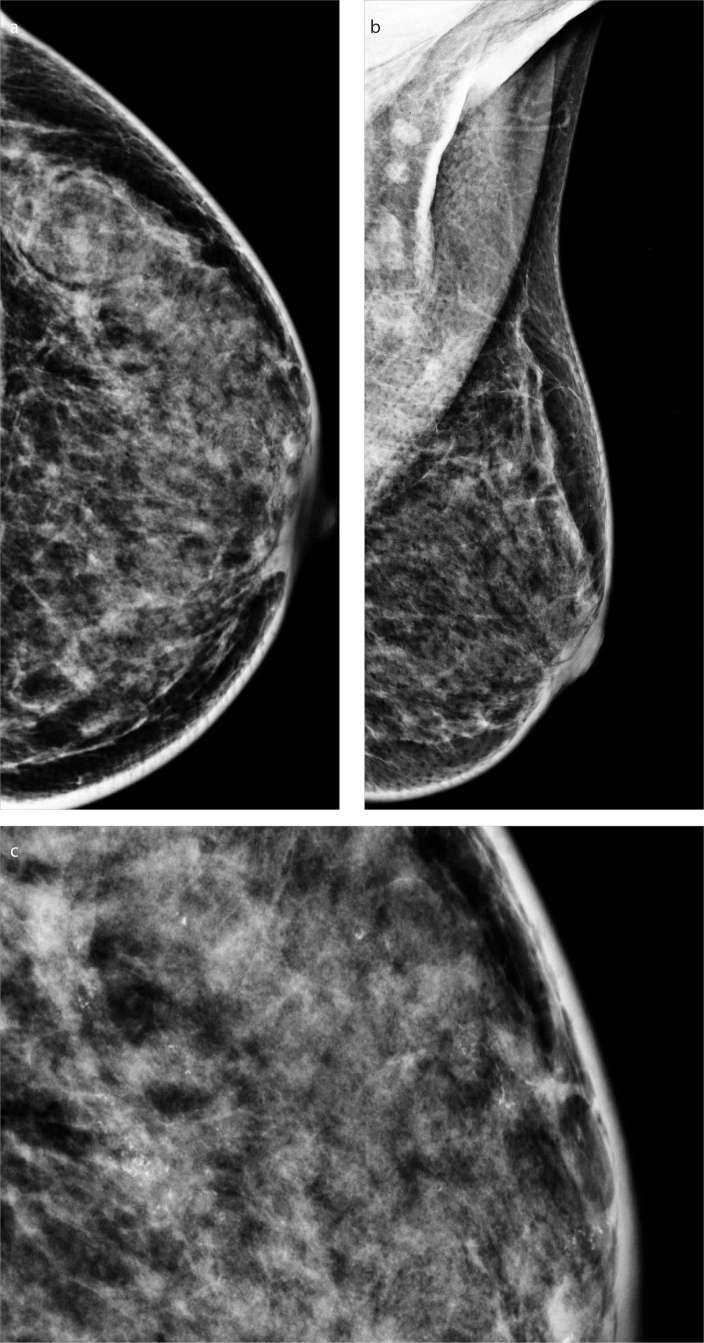
Of the seven missed cancers, one (14.3%) was detected in a type 1 breast parenchymal pattern that presented as focal asymmetry. It was misinterpreted as asymmetric glandular parenchyma following a spot compression mammogram. Three missed cancers (42.9%) were detected in type 2 breast parenchyma. Of these three, two presented as a mass and one presented as an architectural distortion. The remaining two (28.6%) were detected in type 3 and one (14.3%) in type 4 breasts, and all presented as calcification (Fig 2).
Figure 2.
a–c. Left craniocaudal and mediolateral oblique mammograms with a type 3 parenchymal pattern. The segmented pleomorphic microcalcifications in the upper-outer quadrant were missed by two readers (a, b). Panel (c) shows the retrospective digitally magnified view of the missed calcifications.
Discussion
Accurate preoperative detection of tumor size plays a major role because the surgical approach depends on the relation between tumor size and breast size, particularly when planning breast conservation therapy or neoadjuvant chemotherapy (5). According to the guidelines, histologic examination is the gold standard for the accurate tumor dimension measurements. However, mammography and US examinations are taken into consideration in deciding the therapeutic approach and can be supported by magnetic resonance imaging in selected cases (6, 7). In our study, there was a significant correlation between mammographic and histologic tumor size in women aged 50–69 years. However, accurate measurement of the lesions was reported to be difficult in mammograms due to tissue superposition and the lesion masking effect of two-dimensional imaging (7). We believe that the decreased parenchymal density in this age group had an incremental role in accurate measurement of tumor size.
The correlation between the mammographic appearance of the tumors and prognosis has become especially important after settlement of organized screening programs that enable earlier detection of cancers. The characteristic mammographic presentations of breast cancer include mass, microcalcification, architectural distortion and focal asymmetry. Tumors with different clinical and pathologic characteristics have different mammographic manifestations that lead to variable prognoses. It has been stated that mammographic features can accurately be used as independent predictors for long-term outcome with a recommendation that the mammographic features of breast cancer should be taken into consideration during treatment planning especially for T1a and T1b tumors (8). Although the screening programs are successful in detecting small tumors leading to good prognosis, there is still a small number of women who die of early tumors. Tabar et al. (8) showed that women with casting microcalcifications had a poor prognosis and proposed that these women should undergo adjuvant chemotherapy. In our study, cancers that presented as calcifications were mostly pleomorphic with a segmental distribution. Additionally, the majority of tumors that presented as calcifications were Stage 0 and 1 tumors. However, tumors that presented with mass or focal asymmetry were mostly stage 1 cancers marking a little right shift. According to our data, in screen-detected cancers, the earliest tumors were those that are presented with calcifications. Screen-detected tumors presenting with calcifications may have a more favorable prognosis because calcification is thought to be one of the possible indicators of the presence of early breast carcinoma (9). We believe that this finding may be evaluated in more comprehensive screening series.
In our study, the screened women were grouped according to age distribution as 40–49 years and 50–69 years, and the distribution of mammographic features were delineated accordingly. The number of tumors that presented as a mass was slightly higher in women aged 50–69 years. The second most remarkable radiologic finding was calcification, which showed a higher proportion in women aged 40–49 years.
In our study, 7.4% of the cancers were detected in the interval period between two consecutive screening rounds. The Malmö mammographic screening trial suggested that interval cancers are more aggressive and have a lower survival rate (10). However, no significant difference was found in other series (11, 12). The presence of interval cancers may be due to failure of mammographic detection because of their small dimension or obscured lesions that cannot be visualized in dense breasts. Interval cancers have been associated with factors such as younger age, dense breast parenchyma, premenopausal status, and hormone therapy (13–15). In our study interval cancer rate was not significantly different between the age groups. We also assessed the radiologic presentation of the interval cancers. Of the five interval cancers, two presented as focal asymmetry, two as mass and one as calcification. In a recent study, the most common finding of screened interval cancers at presentation was found to be a focal asymmetry (16). In the current study, a statistical comparison could not be made due to the low number of interval cancers.
The proportion of mammographically missed cancers ranges from 4% to 34% (17, 18). Failure to detect tumors in mammography is reportedly due to many factors, including increased parenchymal density, which obscures the subtle findings of malignancy (18, 19). Cancers are shown to be more frequently missed in dense breast parenchyma (20). Additionally, the relative low density of missed cancers compared with surrounding tissue was also attributed as a cause of missed cancers (17). In our study, 43% of the missed cancers were detected in type 2, and 43% in type 3 breast parenchyma, which is inconsistent with the literature. One cancer was detected in a type 4 breast. Cancers in type 2 breast may have been missed at a higher rate because of a false sense of overconfidence in mammographic sensitivity in less dense breasts, particularly in type 2 breast parenchyma. Considering that we saw the highest number of screen-detected, interval, and missed cancers in type 2 breast parenchyma, we believe that readers should be more cautious about missing a tumor focus especially in type 2 breasts.
In our series, the most common presentation of missed cancers was calcification, followed by mass. One missed cancer was retrospectively interpreted as a focal asymmetry and one as an architectural distortion. In the review of the United Kingdom Coordinating Committee on Cancer Research Frequency Trial, granular microcalcifications and deformity were two of the three most frequent presentations of missed cancers in screened women (21). In another study with a large number of screen-detected tumors in women aged 40–48 years, calcification and deformity were the most frequently detected signs (22). We retrospectively detected that calcifications were missed due to misinterpretation and the tendency of the readers to follow-up rather than take action for histopathologic confirmation. In accordance with the literature, the next most frequent presentation of missed cancers was a mass in our study. For mass lesions, an additional US was performed, and we think that, due to a similar reason as with calcifications the readers probably interpreted the masses as benign and a short-term follow-up was performed. We believe that our findings might be confirmed in the following rounds with higher numbers of screen-detected cancers.
Since sensitivity of mammography decreases in dense breasts, all women with type 3 and 4 parenchymal breast patterns underwent a follow-up US examination. A supplemental breast US in screened women increases the cancer detection rate by 2.391/1000 in women with dense breasts when compared with mammography alone (23, 24). We believe that US screening of dense breasts may have an incremental value for the detection of small and node-negative early cancers; a comprehensive series addressing the value of adding US in the survival of these women is required.
Delayed diagnosis of breast cancer is a crucial factor that increases mortality rates. Population-based organized screening studies have shown that the burden of breast cancer has decreased after the implementation of these screens in developing countries (25). With the introduction of mammographic screening, breast cancer is detected in earlier stages, with a tendency towards more favorable prognosis. This, in turn, will lead to a more gentle therapeutic approach, hence decreasing the use of chemotherapy. In the current study, most of the breast cancers were detected at earlier stages. We believe that this finding could be used as a basis to construct organized screening programs in developing countries.
The limitation of this study is that; not all types and distributions of calcifications were detected. There was no case ithaf clustered and fine-linear calcifications as well as diffuse distribution. We believe that this was due to the limited number of screen-detected cancers and this may be overcome in future comprehensive studies that have increased number of cancers with all types of calcifications.
In conclusion, this is the first organized breast screening study in Turkey. Our breast cancer incidence was similar to those obtained in western screening trials; there were no major differences in terms of missed and interval cancer rates. Screen-detected breast cancers had different characteristics in younger and older age groups. We believe that this study will pioneer implementation of efficient population-based mammographic screening in other developing countries.
Main points.
The purpose of this prospective study was to determine whether the mammographic findings of screen-detected cancers correlated with histopathologic findings. In addition, we aimed to discuss the efficacy of breast cancer screening in a developing country.
Population-based organized screening studies have shown that the burden of breast cancer decreases after the implementation of screening in developing countries. With the introduction of mammographic screening, breast cancer is detected in earlier stages, and there is a tendency towards more favorable prognosis.
We believe that this study will pioneer implementation of efficient population-based mammographic screening in other countries.
Acknowledgements
The authors would like to thank Mr. David Chapman for the medical writing and editing assistance in the preparation of this article.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: Globocan 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. http://dx.doi.org/10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.Igene H. Global health inequalities and breast cancer: an impending public health problem for developing countries. Breast J. 2008;14:428–434. doi: 10.1111/j.1524-4741.2008.00618.x. http://dx.doi.org/10.1111/j.1524-4741.2008.00618.x. [DOI] [PubMed] [Google Scholar]
- 3.Porter P. “Westernizing” women’s risks? Breast cancer in lower-income countries. N Engl J Med. 2008;358:213–216. doi: 10.1056/NEJMp0708307. http://dx.doi.org/10.1056/NEJMp0708307. [DOI] [PubMed] [Google Scholar]
- 4.TC. Halk Sağlığı Kurumu Türkiye Kanser İstatistikleri, Ankara. 2015. [Accessed 2015]. p. 20. Available at: http:/kanser.gov.tr/Dosya/ca_istatistik/ANA_rapor_2012v02.pdf.
- 5.Association of Breast Surgery at Baso. Surgical guidelines for the management of breast cancer. Eur J Surg Oncol. 2009;35:1–22. doi: 10.1016/j.ejso.2009.01.008. http://dx.doi.org/10.1016/j.ejso.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Betts GL, Kessels AG, Rupa JD, Bosch AM, Koster D. Preoperative estimation of the pathological breast tumour size by physical examination, mammography and ultrasound: a prospective study on 105 invasive tumours. Eur J Radiol. 2003;48:285–292. doi: 10.1016/s0720-048x(03)00081-0. http://dx.doi.org/10.1016/S0720-048X(03)00081-0. [DOI] [PubMed] [Google Scholar]
- 7.Dummin LJ, Cox M, Plant L. Prediction of breast tumor size by mammography and sonography - A breast screen experience. Breast. 2007;16:38–46. doi: 10.1016/j.breast.2006.04.003. http://dx.doi.org/10.1016/j.breast.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Tabar L, Tony Chen HH, Amy Yen MF, et al. Mammographic tumor features can predict long-term outcomes reliably in women with 1-14-mm invasive breast carcinoma. Cancer. 2004;101:1745–1759. doi: 10.1002/cncr.20582. http://dx.doi.org/10.1002/cncr.20582. [DOI] [PubMed] [Google Scholar]
- 9.Tabar L, Dean PB. Teaching atlas of mammography. 3rd edition. Thieme; Stuttgart: Germany: 2001. [Google Scholar]
- 10.Ikeda BM, Andersson I, Wattsgård C, Janzon L, Linell F. Interval carcinomas in the Malmö mammographic screening trial: radiographic appearance and prognostic considerations. AJR Am J Roentgenol. 1992;159:287–294. doi: 10.2214/ajr.159.2.1632342. http://dx.doi.org/10.2214/ajr.159.2.1632342. [DOI] [PubMed] [Google Scholar]
- 11.Frisell J, Avon Rosen, Wiege M, Nilsson B, Goldman S. Interval cancer and survival in a randomized breast cancer screening trial in Stockholm. Breast Cancer Treat Res. 1992;24:11–16. doi: 10.1007/BF01832353. http://dx.doi.org/10.1007/BF01832353. [DOI] [PubMed] [Google Scholar]
- 12.Burrell HC, Sibbering DM, Wilson AR, et al. Screening interval cancers: mammographic features and prognostic factors. Radiology. 1996;199:811–817. doi: 10.1148/radiology.199.3.8638010. http://dx.doi.org/10.1148/radiology.199.3.8638010. [DOI] [PubMed] [Google Scholar]
- 13.Kavanagh AM, Mitchell H, Giles GG. Hormone replacement therapy and accuracy of mammographic screening. Lancet. 2000;355:270–274. doi: 10.1016/S0140-6736(99)07319-5. http://dx.doi.org/10.1016/S0140-6736(99)07319-5. [DOI] [PubMed] [Google Scholar]
- 14.Sala E, Warren R, McCann J, Duffy S, Day N, Luben R. Mammographic parenchymal patterns and mode of detection: implications for the breast screening programme. J Med Screen. 1998;5:207–212. doi: 10.1136/jms.5.4.207. http://dx.doi.org/10.1136/jms.5.4.207. [DOI] [PubMed] [Google Scholar]
- 15.Carney PA, Miglioretti DL, Yankaskas BC, et al. Individual and combined effects of age, breast density, and hormone replacement therapy use on the accuracy of screening mammography. Ann Intern Med. 2003;138:168–175. doi: 10.7326/0003-4819-138-3-200302040-00008. http://dx.doi.org/10.7326/0003-4819-138-3-200302040-00008. [DOI] [PubMed] [Google Scholar]
- 16.Knox M, O’Brien A, Szabó E, et al. Impact of full field digital mammography on the classification and mammographic characteristics of interval breast cancers. Eur J Radiol. 2015;84:1056–1061. doi: 10.1016/j.ejrad.2015.03.007. http://dx.doi.org/10.1016/j.ejrad.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 17.Goergen SK, Evans J, Cohen GPB, MacMillan JH. Characteristics of breast carcinomas missed by screening radiologists. Radiology. 1997;204:131–135. doi: 10.1148/radiology.204.1.9205234. http://dx.doi.org/10.1148/radiology.204.1.9205234. [DOI] [PubMed] [Google Scholar]
- 18.Majid AS, de Paredes ES, Doherty RD, Sharma NR, Salvador X. Missed breast carcinoma: pitfalls and pearls. Radiographics. 2003;23:881–895. doi: 10.1148/rg.234025083. http://dx.doi.org/10.1148/rg.234025083. [DOI] [PubMed] [Google Scholar]
- 19.Huynh PT, Jarolimek AM, Daye S. The false-negative mammogram. Radiographics. 1998;18:1137–1154. doi: 10.1148/radiographics.18.5.9747612. http://dx.doi.org/10.1148/radiographics.18.5.9747612. [DOI] [PubMed] [Google Scholar]
- 20.Bird RE, Wallace TW, Yankaskas BC. Analysis of cancers missed at screening mammography. Radiology. 1992;184:613–617. doi: 10.1148/radiology.184.3.1509041. http://dx.doi.org/10.1148/radiology.184.3.1509041. [DOI] [PubMed] [Google Scholar]
- 21.Warren RML, Young JR, McLean L, et al. Radiology review of the UKCCCR breast screening frequency trial: potential improvements in sensitivity and lead time of radiological signs. Clin Radiol. 2003;58:128–132. doi: 10.1053/crad.2002.1132. http://dx.doi.org/10.1053/crad.2002.1132. [DOI] [PubMed] [Google Scholar]
- 22.Evans AJ, Kutt E, Record C, Waller M, Moss S. Radiological findings of screen-detected cancers in a multi-centre randomized, controlled trial of mammographic screening in women from age 40 to 48 years. Clin Radiol. 2006;61:784–788. doi: 10.1016/j.crad.2006.04.013. http://dx.doi.org/10.1016/j.crad.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 23.Chae EY, Kim HH, Cha JH, Shin HJ, Kim H. Evaluation of screening whole-breast sonography as a supplemental tool in conjuction with mammography in women with dense breasts. J Ultrasound Med. 2013;32:1573–1578. doi: 10.7863/ultra.32.9.1573. http://dx.doi.org/10.7863/ultra.32.9.1573. [DOI] [PubMed] [Google Scholar]
- 24.Korpraphong P, Limsuwarn P, Tangcharoensathien W, Ansusingha T, Thephamongkhol K, Chuthapisith S. Improving breast cancer detection using ultrasonography in asymptomatic women with non-fatty breast density. Acta Radiol. 2014;55:903–908. doi: 10.1177/0284185113507711. http://dx.doi.org/10.1177/0284185113507711. [DOI] [PubMed] [Google Scholar]
- 25.Christensen LH, Engholm G, Cortes R, et al. Reduced mortality for women with mammography-detected breast cancer in east Denmark and south Sweden. Eur J Cancer. 2006;42:2773–2780. doi: 10.1016/j.ejca.2006.03.036. http://dx.doi.org/10.1016/j.ejca.2006.03.036. [DOI] [PubMed] [Google Scholar]