Abstract
Background
Parental perceptions about treatment influence their child’s engagement in and ongoing utilization of mental health services, but less is known about the association between caregiver expectancies and family outcomes. The literature is particularly lacking with families of color, who are at high risk for the onset and perpetuation of disruptive behaviors.
Methods
The purpose of this study was to examine caregiver treatment satisfaction amongst 320 youth of color aged 7 to 11 and their families who were assigned to either a Multiple Family Group intervention or services as usual condition. Caregiver stress was measured by the Parenting Stress Index Short-Form full scale and child oppositional defiant behaviors were measured using the Iowa Connors Rating Scale–Oppositional/Defiant subscale both at baseline and post-test. Satisfaction with treatment was measured using the Metropolitan Area Child Study process measures program satisfaction subscale at post-test.
Results
The two main effects models that focused on satisfaction with treatment was predictive of parental stress and child oppositional defiant behaviors independently. Satisfaction with treatment accounted for 31% of the variance in child oppositional behavior and 24% of parental stress improvements across time holding all covariates constant.
Conclusions
Our findings support previous research that shows parental expectancies, including treatment satisfaction, are powerful mechanisms of treatment outcomes for children with DBDs as well as parental emotional health. Further, parental expectancies may be enhanced by the involvement of families in the development of treatment approaches for children and a greater focus on caregiver emotional health for the benefit of the family as a whole.
Keywords: Parental expectancies, treatment satisfaction, family outcomes, child disruptive behavior disorders
Introduction
Parents are pivotal to their child’s engagement in mental health services and their therapeutic progress. In general, parents initiate their child’s initial and ongoing utilization of services (deHaan et al., 2013; Eapen & Ghubash, 2004; Nock & Kazdin, 2001; Thurston et al., 2015), are often actively involved in the therapeutic process (Acri & Hoagwood, 2015; Danko et al., 2015), and effect treatment outcomes via an array of parental factors including, but not limited to demographics characteristics (e.g., educational and socioeconomic status), their emotional health (e.g., depression and elevated stress), and their parenting style (Beauchaine et al., 2005; Foster et al., 2009; Hinshaw et al., 2000; Pilowsky et al., 2008; Reyno & McGrath, 2006).
Within this literature, a main area of examination involves the influence of caregiver perceptions, cognitions, and beliefs, or what Nock and Kazdin (2001) refer to as expectancies about treatment, upon their child’s experience with the mental health system. Negative perceptions of providers and treatment (e.g., mistrust of mental health professionals, concerns about violations in confidentiality) (Contractor et al., 2012; McKay & Bannon, 2004), the perceived relevance and helpfulness of therapeutic approaches (Eapen & Ghubash, 2004; Kazdin, et al, 1997; Morrisey-Kane & Prinz, 1999; Nock & Kazdin, 2001) and their acceptability (Choi & Kovshoff, 2013; Stevens et al., 2006), are powerful drivers of service utilization and underuse. Expectancies such as the perceived usefulness of treatment (Graf et al, 2014) and its acceptability (MacKenzie et al., 2004) are also associated with child treatment outcomes, including reductions in child problem behaviors, although this literature is considerably thinner than the association between these factors and engagement in care.
Among the various expectancies parents hold about their child’s mental health treatment, treatment satisfaction has emerged as a key domain of interest, particularly with insurance companies, agencies, and providers, as it is considered a metric for the quality of care received and the effectiveness of services (Bierling, 2010; Brestan et al., 2000; Edlund et al., 2003; Garland et al., 2008; Solberg et al., 2015). Defined as viewing the process and outcomes associated with treatment favorably (Brestan et al., 2000), treatment satisfaction has grown in importance due to increased emphasis on consumer choice and empowerment, and the impact of such preferences upon health outcomes (Day, Michelson, & Hassan, 2011; Rey et al., 1999; Solberg et al., 2015).
Among adults, treatment satisfaction is associated with increased treatment use, adherence, and positive patient outcomes (Barber et al., 2006; Tas et al., 2010). For children with mental health needs, results are uneven, with the research alternatingly finding either a positive association between parental satisfaction and improvement in symptom change (Rey et al., 1999) or no relationship between the two (Biering, 2010; Garland et al., 2008; Tas et al., 2010). Other issues that complicate parsing out the effect of satisfaction on therapeutic outcomes for children include a lack of standardization regarding the definition of treatment satisfaction, and that few instruments have been tested or have adequate psychometric properties (Day et al., 2011). Further, some critics argue that only those who receive treatment benefits will rate satisfaction highly (Bierling, 2010); however, recent studies show that there is in actuality a small association between outcomes and satisfaction (Solberg et al., 2015).
The primary purpose of the current study is to contribute to the current literature of parental expectancies by examining the relationship between treatment satisfaction and child outcomes within data collected for the 4Rs and 2Ss Multiple Family Group (MFG) field-trial from 2006 to 2010 in New York City. This is a National Institute of Mental Health-funded study of a Multiple Family Group model. Briefly, this curriculum-based, time-limited (16 weeks) multiple family group model integrates common elements of evidence-informed treatments for conduct problems into a coordinated set of practices in order to decrease problem behaviors, strengthen families, and increase engagement in treatment. Examinations of outcomes of the MFG trial have demonstrated improvements in youth oppositional behavior and social competence over time for participants exposed to the intervention (MFG) as compared to the services as usual (SAU) condition (Chacko et al., 2015; Gopalan et al., 2014). See the Procedure section for a fuller description of the two conditions wtithin the MFG study.
While evidence-based interventions have been designed to treat DBDs (Eyberg, Nelson, & Boggs, 2008), notable challenges in implementing these interventions in publicly funded outpatient mental health settings have been recommended (Chacko et al., 2015). Thus, MFG was designed with a common elements approach (Chorpita & Daleiden, 2009; Garland et. al, 2008) utilizing and integrating core components of effective treatment for DBDs within the empirical literature (Chacko et al., 2015). Furthermore, evidence-based engagement techniques were embedded in the MFG model to specifically improve the mental health services retention of families within socioeconomically disadvantaged communities (Mckay & Bannon, 2004).
This study will extend upon the current knowledge base in two specific ways. First, it will focus on a relatively unstudied population at high risk of DBDs; children of color. As noted by Copeland et al. (2004), it isn’t entirely clear how children and families of color perceive treatment, and especially whether their satisfaction with services is related to treatment outcomes. A set of studies suggest that there are clear differences between caregivers of color and Caucasian parents with respect to knowledge about treatments for child mental health problems (Bussing, Schoenberg, & Perwien, 1998), and that African American parents view treatments differently and in some cases less favorably than other ethnic groups (Stevens et al., 2006). In light of these findings, more research is needed to distill the expectancies of families of color, and whether satisfaction in particular is associated with clinical improvement.
Second, this study will examine whether the impact of parent satisfaction extends beyond child outcomes. Few studies of child mental health services focus on parental outcomes independent of the child (e.g., examining parental depression as it impacts improvement in child behavior) (Acri & Hoagwood, 2015). However, parents of children with mental health problems are at high risk for increased stress due in large part to their caretaking role (McAdams et al., 2015; Shapiro et al., 2014; Theule et al., 2013). In addition to exacting a personal toll (e.g., increased risk of morbidity and mortality, high levels of parental stress erode the quality of the caretaker’s parenting, potentially resulting in an inconsistent and harsh parenting style (Coiro et al, 2012; Deater-Deckard, 2004), and increased risk of neglect (Friedman & Billick, 2015). Studying the relationship between satisfaction and parental emotional health may identify factors that enhance parent outcomes and benefit a large number of high-risk youth and families.
Methods
Overview of study methods and sites
This study analyzed data gathered from the Multiple Family Group (MFG) field-trial including 320 primary caregivers of children between seven and 11 years of age who were diagnosed with a Disruptive Behavior Disorder (DBD) as specified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000). Both groups of participants were enrolled from 13 New York State Office of Mental Health-licensed public child mental health outpatient clinics serving families. Each clinic provides an array of mental health services to youth and families from neighborhoods in the New York metropolitan area. New York University’s Institutional Review Board provided approval for this study.
Participants
The sample consisted of 320 primary caregivers of children between seven and 11 years of age diagnosed with a DBD seeking treatment at a public outpatient clinic. The majority of children identified as Latino (51%) or Black/African-American (31%) and male (70%). The majority of caregivers identified as Latino (53%) or Black/African American (30%), and over three-quarters (80%) reported a family income of below $30,000. Most families (67%) identified as having a single-parent household and 70% (n = 223) received publicly funded health insurance. Table 1 provides the sociodemographic characteristics of the sample by treatment condition.
Table 1.
Sociodemographic characteristics of participants by treatment condition
| Characteristic | Experimental Group (n= 225) | Control Group (n=95) | Significance1 | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Child age (M ± SD) | 209 | 8.88 ± 1.45 | 93 | 8.85 ± 1.34 | |
| Child race/ethnicity | |||||
| White/Caucasian | 16 | 7.11 | 9 | 9.47 | |
| Black/African American | 66 | 29.33 | 29 | 30.53 | |
| Hispanic/Latino | 112 | 49.78 | 44 | 46.32 | |
| Native American | 3 | 1.33 | 5 | 5.26 | |
| Asian/Pacific Islander | 0 | 0.00 | 1 | 1.05 | |
| Other | 15 | 6.67 | 6 | 6.32 | |
| Caregiver age (M ± SD) | 217 | 35.72 ± 8.39 | 93 | 38.18 ± 9.30 | * |
| Primary Caregiver | * | ||||
| Mother | 175 | 77.78 | 77 | 81.05 | |
| Father | 5 | 2.22 | 1 | 1.05 | |
| Grandparents | 6 | 2.67 | 8 | 8.42 | |
| Mother and father | 22 | 9.78 | 2 | 2.11 | |
| Other | 9 | 4.00 | 5 | 5.26 | |
| Caregiver marital status | ** | ||||
| Married | 139 | 61.78 | 44 | 46.32 | |
| Single | 86 | 38.22 | 51 | 53.68 | |
| Caregiver education | |||||
| Some high school | 60 | 26.67 | 31 | 32.63 | |
| Completed high school | 51 | 22.67 | 26 | 27.37 | |
| Some college | 49 | 21.78 | 21 | 22.11 | |
| Completed college | 16 | 7.11 | 5 | 5.26 | |
| Caregiver employment | |||||
| Employed full-time | 54 | 24.00 | 21 | 22.11 | |
| Employed part-time | 40 | 17.78 | 14 | 14.74 | |
| Unemployed | 71 | 31.56 | 33 | 34.74 | |
| Family income | |||||
| Less than $9,999 | 91 | 40.44 | 34 | 35.79 | |
| $10,000 to $19,999 | 55 | 24.44 | 26 | 27.37 | |
| $20,000 to $29,999 | 32 | 14.22 | 15 | 15.79 | |
| $30,000 to $39,999 | 15 | 6.67 | 8 | 8.42 | |
| $40,000 to $49,000 | 3 | 1.33 | 1 | 1.05 | |
| Over $50,000 | 14 | 6.22 | 4 | 4.21 | |
| Receipt of public health insurance | 150 | 72 | 73 | 77 | |
p<.05,
p<.01,
NS: not significant
T-tests and Chi-sq tests comparing differences between treatment condition
Note: Data are not available for the entire sample of 320 participants and their families; data are available for 217 participants in the experimental group and 93 in the control group.
Inclusion/exclusion criteria
Inclusion criteria included adults 18 years or older who spoke English or Spanish and were the primary caregiver of a child between seven and 11 years of age who met criteria for a DBD as measured by the Disruptive Behavior Disorders Rating Scale (Pelham et al, 1992). Caregivers were excluded if they manifested a significant cognitive impairment that would interfere with understanding the informed consent process, or if they had emergency psychiatric needs requiring services beyond those provided within an outpatient setting. Caregivers were also excluded if children resided in foster care or their legal guardian could not provide formal consent.
Procedure
After eligibility was confirmed, participants were assigned to the Multiple Family Group (MFG) experimental condition (n=225) or services as usual (SAU) control condition (n=95). Using a 2:1 allocation ratio block design, six to eight families were recruited to the experimental condition, while three to four families were assigned to the control condition. Because conditions can be populated quickly and efficiently, block comparison designs like the one utilized in this study are frequently employed for health services trials with logistical constraints (Goodwin et al., 2001). To reduce bias in assignment, decisions regarding condition assignment were managed by project coordinators who did not have contact with potential participants. Additionally, research staff and investigators were blind to youth and family profiles during allocation.
Description of the intervention and comparison condition
4Rs 2Ss Multiple Family Group
The 4Rs’ and 2Ss’ Multiple Family Group (MFG): MFG is a manualized, time-limited (16 weeks, 90–120 minutes per session) mental health service that targets school-age, urban children (seven to 11 years) meeting diagnostic criteria for ODD or CD and their families, including adult caregivers, and siblings over six years of age. MFG, led by licensed clinical social workers, typically involves six to eight families, and at least two generations of a family are present in each session. MFG integrates essential practices of behavioral parent training and family therapy as well as factors known to affect service utilization, translated into six core intervention components known as the 4Rs and 2Ss: Roles, Responsibilities, Relationships, Respectful communication, Social support, and Stress (see Chacko et al, 2015, Gopalan et al., 2014 for a full description of MFG services). Participants in the MFG condition were not restricted from also obtaining other services within the participating site (e.g., medication management). In addition, MFG attendance was relatively high despite the 16-week duration of the intervention and the risk factors for poor engagement in socioeconomically disadvantaged communities (Gopalan, Goldstein, Klingenstein, Sicher, & McKay, 2010. Specifically, 59% of participants in the MFG condition attended all sessions (SD = 7.55%).
Services -As-Usual (SAU)
In this treatment condition, participants only received any service typically provided by the participating site. This included medication management, case management, as well as individual/family/group therapy (see Chacko et al, 2015, Gopalan et al., 2014 for a full description of SAU services).
Measurement
Demographic characteristics were collected via a general sociodemographic questionnaire used in prior studies that assessed familial factors (e.g., child and caregiver age, gender, race/ethnicity, and family income). Family (parental stress) and child (oppositional defiant behavior) outcomes, along with satisfaction with treatment were evaluated in the current study.
Parenting stress in the parent-child system was assessed using the Parenting Stress Index-short form (PSI 3rd Ed.; Abidin, 1995). Parents with children 11 years old and younger completed a 36-item questionnaire with response options ranging from one (strongly disagree) to five (strongly agree). Possible scores on the PSI full scale (PSI) range from 36 to 180 with higher scores indicating increased levels of parent stress. Good internal consistency was found with all five subscales at baseline and post-test. Cronbach’s alphas at baseline and post-test were .91 and .94, respectively. In the current study, 69% of caregivers demonstrated clinically significant scores (≥90) on the PSI at baseline.
Child oppositional defiant behaviors were measured using the Iowa Connors Rating Scale–Oppositional/Defiant Subscale (IOWA CRS OD). The IOWA CRS OD subscale (Waschbusch & Willoughby, 2008) is completed by parents and is a widely used brief measure of oppositional defiant behavior in children. The IOWA CRS includes items evaluated using a 4-point Likert-type scale with the following rating categories: not at all (0), just a little (1), pretty much (2), and very much (3). Cronbach’s alphas at baseline and post-test were .80 and .86, respectively.
Satisfaction with treatment was measured using the Metropolitan Area Child Study (MACS) process measures program satisfaction subscale (Tolan et al., 2002). The MACS is a self-report measure of treatment process completed by parents rated on a scale from 1 to 4: not at all (1), just a little (2), somewhat (3), and very much (4). Fourteen items specifically ask about parents’ opinions about helpfulness of groups, the importance of therapy for families, and family improvements as a result of treatment. Scores for the program satisfaction subscale range from 14–56 with higher scores indicating greater treatment satisfaction. The Cronbach’s alpha at post-test was .92.
Data analysis
The data were analyzed using Structural Equation Modeling (SEM) with Mplus using a robust (Huber-White) maximum likelihood algorithm to deal with nonnormalty and variance heterogeneity. Missing data, though minimal, was present and was treated using Full Information Maximum Likelihood (FIML) methods. The fit of the SEM model was evaluated using both global (chi square, CFI, standardized RMR, RMSEA) and focused (standardized residuals and modification indices) fit indices. Endogenous variables independently included change scores of the PSI and IOWA CRS OD from baseline to post-test. The MACS satisfaction with treatment subscale at post-test served as the exogenous variable representing therapeutic process factors. The following were covariates: parent age, treatment condition (MFG vs. SAU), and baseline levels of parental stress (PSI) and child oppositional defiant behaviors (IOWA CRS OD) independently. In addition, potential interaction effects of treatment condition and parent age were modeled.
Preliminary analyses
Preliminary analyses examined differences in parent age, parent stress, and child oppositional defiant behaviors by treatment condition independently. Overall, MFG caregivers were significantly younger than SAU caregivers (t = −2.29, df = 308, p = .020). At baseline, there were no significant differences in levels of stress (PSI) or child oppositional defiant disorders (IOWA CRS OD) between treatment groups (MFG vs. SAU). At post-test, participants in the SAU condition reported marginally significantly higher levels of stress (M = 9.01, SD = 3.80) as compared to the MFG condition (M = 7.74, SD = 3.74; t = −1.78, df = 165, p = .07). In addition, SAU condition participants at post-test reported significantly greater levels of child oppositional defiant disorders (M = 94.46, SD = 21.55) as compared to MFG participants (M = 88.88, SD = 24.40; t = −2.47, df = 148, p = .014). Among the full sample (regardless of treatment condition), there were significant improvements in PSI (t = 4.51, df = 210, p = .000) and IOWA CRS OD (t = 3.69, df = 203, p = .000) scores from baseline to post-test. Thus, change scores from baseline to post-test were used as endogenous variables independently from baseline to post-test to represent improvements across time.
Results
Table 2 presents means and SDs for family and child outcomes at baseline and post-test. The mean change scores from baseline to post-test were 6.12 (SD= 19.70) for the parent stress (PSI) and .97 (SD= 4.02) for child oppositional defiant behaviors (IOWA CRS OD). Furthermore, change scores for the PSI (t = 2.93, df = 159, p = .004) and IOWA CRS OD (t = 2.76, df = 140, p = .007) among MFG participants were greater as compared to SAU. The mean score for the MACS satisfaction with treatment subscale at post-test was 34.84 (SD = 5.13). There were no significant differences in MACS satisfaction between treatment conditions (MFG vs. SAU).
Table 2.
Baseline and post-test means of outcome variables by treatment condition
| Outcome | Time Point | Experimental Group (n= 225) | Control Group (n=95) | ||
|---|---|---|---|---|---|
| n | M ± SD | N | M ± SD | ||
| PSI | Baseline | 191 | 100.05 ± 22.98 | 91 | 95.41 ± 21.42 |
| Post-Test | 160 | 88.87 ± 24.40 | 76 | 94.46 ± 21.55 | |
| IOWA CRS-OD | Baseline | 201 | 9.28 ± 3.37 | 87 | 9.04 ± 3.69 |
| Post-Test | 173 | 7.74 ± 7.74 | 79 | 9.01 ± 3.80 | |
The two main effects models that focused on satisfaction with treatment (MACS) was predictive of parental stress (PSI) and child oppositional defiant behaviors (IOWA CRS OD) independently. For the PSI change scores representing improvements in parent stress from baseline to post-test, the global fit indices all pointed towards good model fit (Chi square of 5.188 with df = 3 yielded p-value = 0.1585; CFI = 0.95, RMSEA = 0.055, p-value for close fit = 0.367, standardized RMR = 0.037). Examination of focused fit indices (standardized residuals and modification indices) revealed no theoretically meaningful points of stress on the model.
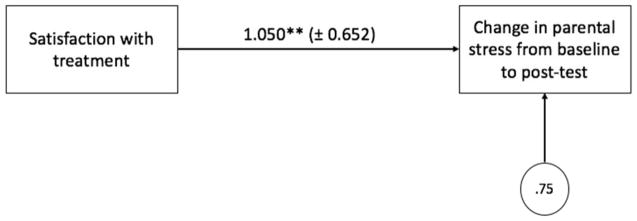
Figure 1 presents the unstandardized parameter estimates for the first main effects model, with margins of error in parentheses. The path coefficient for the MACS was statistically significant (p<.01). For every one-unit increase in parents’ report of satisfaction with treatment, parental stress change from baseline to post-test was found to increase on average by 1.05 units (p = 0.001) holding parent age, treatment condition, and baseline level of parent stress constant. Further, satisfaction with treatment accounted for 24% of the variance in parental stress improvements across time holding all covariates constant.
Figure 1.
Structural main effects model for parental stress
For the IOWA CRS OD change scores representing improvements in child oppositional defiant behaviors from baseline to post-test, the global fit indices all pointed towards good model fit (Chi square of 3.077 with df = 3 yielded p-value = 0.3799; CFI = 0.999, RMSEA = 0.010, p-value for close fit = 0.612, standardized RMR = 0.029). Examination of focused fit indices (standardized residuals and modification indices) revealed no theoretically meaningful points of stress on the model.
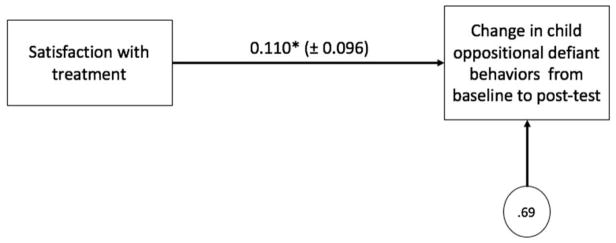
Figure 2 presents the unstandardized parameter estimates for the second main effects model, with margins of error in parentheses. The path coefficient for the MACS was statistically significant (p<.05). For every one-unit increase in parents’ report of satisfaction with treatment, child oppositional defiant behavior change from baseline to post-test was found to increase on average by .11 units (p = 0.023) holding parent age, treatment condition, and baseline level of child oppositional defiant behaviors constant. Further, satisfaction with treatment accounted for 31% of the variance in child oppositional behavior improvements across time holding all covariates constant.
Figure 2.
Structural main effects model for child oppositional defiant behaviors
Since all caregivers may not have entered the study with clinically pertinent needs, it was important to preform supplemental analyses to examine differences in child disruptive behaviors, satisfaction with treatment, and parental stress improvements (change score from baseline to post-test) by clinical significance status. There were no between group differences in child oppositional defiant behaviors among caregivers who had clinically or non-clinically significant PSI scores at baseline (t = −.901, df = 163, p = .369). Significant only at the .10 level, there was a trend in differences in satisfaction with treatment between caregivers who presented at baseline with clinically significant and non-clinically significant levels of stress (t = 1.69, df = 152, p = .093). Lastly, improvements in parental stress over time was significantly different for caregivers with clinically significant as compared to non-clinically significant PSI levels at baseline. As a result, the potential moderator of clinical significance status in the relationship between satisfaction and improvements in parental stress was tested using Marsh et al.’s (2004) strategy in SEM; however, there was no significant interaction effect.
Discussion
The purpose of this study was to examine the relationships between caregiver treatment satisfaction and child and parent-level outcomes amongst children and families of color who are at high risk for the onset and perpetuation of DBDs and parental stress. To our knowledge, this is the first study to both focus on ethnic minority families and independently examine the impact of treatment satisfaction upon parent emotional health.
Several findings warrant comment. First, we found that satisfaction with treatment was significantly associated with reductions in problematic child behaviors and parent stress, and that parent stress improved independent of child behavior. Despite finding no significant difference in MACS satisfaction between treatment groups at post-test, it was evident that significant differences were found in child oppositional defiant disorders at post-test and marginally significant differences for parental stress at post-test when comparing the two treatment groups independently. Moreover, families involved in the multiple family group intervention and those who received services as usual evidenced differing benefits in child behavior and parent stress.
These findings support previous research that shows parental expectancies are powerful mechanisms of treatment outcomes for children (e.g., Rey et al., 1999), and is concordant with a wide literature that documents the importance of parents in child mental health services, and specifically parental perceptions, beliefs, and attitudes about care. It also extends current knowledge in that satisfaction with the child’s treatment was associated with significant reductions in parental-level outcomes. These findings are particularly critical given there is a lack of knowledge regarding how treatment satisfaction impacts outcomes amongst ethnic minority families, and that children of color living in poverty-impacted communities demonstrate the highest need for mental health services, yet display the lowest rates of service use.
A second finding of note is that approximately 70% of the sample evidenced clinically significant levels of stress at baseline. This finding is not surprising considering caregivers living in poverty experience enormous stressors that affect their emotional health, including chaotic communities, substance abuse, criminal activity and violence, and scarce resources (McKay & Bannon, 2004) not to mention the demands of caring for a child with mental health needs. The finding that almost three-quarters of the sample evidenced high stress levels speaks to the need to attend to the emotional health of caregivers within the context of the child’s treatment, and echoes calls to integrate child and parent mental health services (Acri & Hoagwood, 2015). At a minimum, detection for caregiver emotional health risks such as depression and stress should be standardized whenever a child presents for mental health services; optimally, co-locating child and adult mental health services would be one of the more effective ways to address unmet parental mental health needs, particularly given passive referrals to services are largely ineffective (Acri & Hoagwood, 2015). Although considerable barriers to linking child and parent mental health services have been cited, such as separate funding streams and treatment systems, (Blanch, Nicholson, & Purcell, 1994; Mason & Subedi, 2006). Not addressing the emotional health of parents has potentially serious, deleterious implications for families. While not every parent will be in need of mental health care, this study shows that families of color living in low-income communities are at particularly high risk of unmet need, and thus parental health should be part of the assessment and treatment plan for children with behavior problems.
Limitations
In light of these findings, the study has several limitations suggesting the need for replication. Although attention was placed on reducing selection bias, the assignment to treatment condition was not randomized. Importantly, however, there were no differences between the two treatment conditions in treatment satisfaction at post-test or parental stress and child disruptive behavior disorders at baseline and post-test. As for demographic characteristics at baseline, significantly more caregivers in the experimental group (MFG) were mothers, married, and younger as compared to the control group (SAU). While there were no clinical differences related to the study outcomes, it is important to consider the few demographic differences between groups when interpreting findings.
In addition, treatment satisfaction was only collected from caregivers who completed treatment, which may suggest that those dissatisfied with services dropped out from treatment. Future research is needed in which satisfaction is assessed from families that do not complete treatment in order to discern whether it is dissatisfaction or other factors that were responsible for dropout.
Lastly, we did not assess for child satisfaction with services. Future research could benefit from assessing satisfaction from both the child and parents, to determine if child expectancies have a similar effect upon treatment outcomes. Additionally, future research should investigate the potential prediction of caregiver stress and child disruptive behaviors from treatment satisfaction.
In close, this study is a promising first step for understanding the relationship between parent satisfaction with their child’s treatment, child outcomes, and caregiver emotional health among high-risk families of color. The implications of this study suggest that caregiver expectancies are important to the treatment process and may be enhanced through collaborative research methodologies that involve families in the development of treatment approaches for children, and that these treatments should optimally assess and address caregiver emotional health for the benefit of the entire family.
Key Practitioner Message.
Parental expectancies, including treatment satisfaction, are shown to positively impact their child’s treatment engagement and lead to more positive child outcomes.
Our research addresses a gap in the literature on treatment satisfaction among poverty impacted families of color and looks at both child and parent outcomes
Out findings show that parental expectancies, including treatment satisfaction, are powerful mechanisms of treatment outcomes for children with DBDs as well as parental emotional health.
Clinical practice and future research should aim to maximize acceptability, relevance and quality of services for poverty impacted children and families of color.
Acknowledgments
Funding for this study was obtained through R01 MH072649 (M.M.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the National Institutes of Health.
Footnotes
The authors declare they have no competing or potential conflicts of interest.
References
- Abidin RR. Parenting Stress Index, Third Edition: Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc; 1995. [Google Scholar]
- Acri MC, Hoagwood KE. Addressing parental mental health within interventions for children A review. Research on Social Work Practice. 2015;25(5):578–586. doi: 10.1177/1049731514546027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber AJ, Tischler VA, Healy E. Consumer satisfaction and child behaviour problems in child and adolescent mental health services. Journal of Child Health Care. 2006;10(1):9–21. doi: 10.1177/1367493506060200. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: A latent growth curve analysis. Journal of Consulting and Clinical Psychology. 2005;73:371–388. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- Biering P. Child and adolescent experience of and satisfaction with psychiatric care: A critical review of the research literature. Journal of Psychiatric and Mental Health Nursing. 2010;17(1):65–72. doi: 10.1111/j.1365-2850.2009.01505.x. [DOI] [PubMed] [Google Scholar]
- Blanch AK, Nicholson J, Purcell J. Parents with severe mental illness and their children: The need for human services integration. The Journal of Mental Health Administration. 1994;21(4):388–396. doi: 10.1007/BF02521357. [DOI] [PubMed] [Google Scholar]
- Brestan EV, Jacobs JR, Rayfield AD, Eyberg SM. A consumer satisfaction measure for parent-child treatments and its relation to measures of child behavior change. Behavior Therapy. 2000;30(1):17–30. [Google Scholar]
- Bussing R, Schoenberg NE, Perwien AR. Knowledge and information about ADHD: Evidence of cultural differences among African-American and White parents. Social Science and Medcine. 1998;46(7):919–928. doi: 10.1016/s0277-9536(97)00219-0. [DOI] [PubMed] [Google Scholar]
- Chacko A, Gopalan G, Franco L, Dean-Assael K, Jackson J, Marcus S, … McKay M. Multiple Family Group Service Model for Children With Disruptive Behavior Disorders Child Outcomes at Post-Treatment. Journal of Emotional and Behavioral Disorders. 2015;23(2):67–77. doi: 10.1177/1063426614532690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KY, Kovshoff H. Do maternal attributions play a role in the acceptability of behavioural interventions for problem behaviour in children with autism spectrum disorders? Research in Autism Spectrum Disorders. 2013;7(8):984–996. [Google Scholar]
- Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: Application of the distillation and matching model to 615 treatments from 322 randomized trials. Journal of Consulting and Clinical Psychology. 2009;77(3):566. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Coiro MJ, Riley A, Broitman M, Miranda J. Effects on children of treating their mothers’ depression: Results of a 12- month follow-up. Psychiatric Services. 2012;63:357–363. doi: 10.1176/appi.ps.201100126. [DOI] [PubMed] [Google Scholar]
- Contractor LF, Celedonia KL, Cruz M, Douaihy A, Kogan JN, Marin R, Stein BD. Mental health services for children of substance abusing parents: voices from the community. Community Mental Health Journal. 2012;48(1):22–28. doi: 10.1007/s10597-010-9357-6. [DOI] [PubMed] [Google Scholar]
- Copeland VC, Koeske G, Greeno CG. Child and mother client satisfaction questionnaire scores regarding mental health services: Race, age, and gender correlates. Research on Social Work Practice. 2004;14(6):434–442. [Google Scholar]
- Danko CM, Brown T, Van Schoick L, Budd KS. Child & Youth Care Forum. Springer; US: 2015. Predictors and Correlates of Homework Completion and Treatment Outcomes in Parent–Child Interaction Therapy; pp. 1–19. [Google Scholar]
- Day C, Michelson D, Hassan I. Child and adolescent service experience (ChASE): Measuring service quality and therapeutic process. British Journal of Clinical Psychology. 2011;50(4):452–464. doi: 10.1111/j.2044-8260.2011.02008.x. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice. 2004;5:314–332. [Google Scholar]
- DeHann A, Boon A, de Jong J, Hoeve M, Vermeiren R. A meta-analytic review on treatment dropout in child and adolescent outpatient mental health care. Clinical Psychology Review. 2013;33(5):698–711. doi: 10.1016/j.cpr.2013.04.005. [DOI] [PubMed] [Google Scholar]
- Eapen V, Ghubash R. Help-seeking for mental health problems or children; Preference’s and attitudes in the United Arab Emirates. Psychological Reports. 2004;94:663–667. doi: 10.2466/pr0.94.2.663-667. [DOI] [PubMed] [Google Scholar]
- Edlund MJ, Young AS, Kung FY, Sherbourne CD, Wells KB. Does satisfaction reflect the technical quality of mental health care? Health Services Research. 2003;38(2):631–645. doi: 10.1111/1475-6773.00137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyberg S, Nelson M, Boggs S. Evidence-based psychological treatments for children and adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Foster CW, Webster MC, Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, et al. Remission of maternal depression: Relations to family functioning and Youth internalizing and externalizing symptoms. Journal of Clinical Child and Adolescent Psychology. 2009;37(4):714–724. doi: 10.1080/15374410802359726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman E, Billick SB. Unintentional child neglect: literature review and observational study. Psychiatric Quarterly. 2015;86(2):253–259. doi: 10.1007/s11126-014-9328-0. [DOI] [PubMed] [Google Scholar]
- Garland AF, Hawley KM, Brookman-Frazee L, Hurlburt MS. Identifying common elements of evidence-based psychosocial treatments for children’s disruptive behavior problems. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(5):505–514. doi: 10.1097/CHI.0b013e31816765c2. [DOI] [PubMed] [Google Scholar]
- Goodwin PJ, Leszcz M, Ennis M, Koopmans J, Vincent L, Guther H, Hunter J. The effect of group psycho- social support on survival in metastatic breast cancer. New England Journal of Medicine. 2001;345(24):1719–1726. doi: 10.1056/NEJMoa011871. [DOI] [PubMed] [Google Scholar]
- Gopalan G, Chacko A, Franco L, Dean-Assael KM, Rotko LE, Marcus SM, … McKay MM. Multiple Family Groups for Children with Disruptive Behavior Disorders: Child Outcomes at 6-Month Follow-Up. Journal of Child and Family Studies. 2014:1–13. doi: 10.1007/s10826-014-0074-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Wells KC, Kraemer HC, Abikoff HB, Arnold LE, … Hoza B. Family processes and treatment outcome in the MTA: Negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology. 2000;28(6):555–568. doi: 10.1023/a:1005183115230. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Holland L, Crowley &, Breton S. Barriers to treatment participation scale: Evaluation and validation in the context of child outpatient treatment. Journal of Child Psychology and Psychiatry. 1997;38(8):1051–1062. doi: 10.1111/j.1469-7610.1997.tb01621.x. [DOI] [PubMed] [Google Scholar]
- MacKenzie EP, Fite PJ, Bates JE. Predicting outcome in behavioral parent training: Expected and unexpected results. Child & Family Behavior Therapy. 2004;26:37–53. doi: 10.1300/J019v26n02_03. [DOI] [Google Scholar]
- Marsh HW, Wen Z, Hau K. Structural equation models of latent interactions: Evauation of alternative estimation strategies and indicator construction. Psychological Methods. 2004;9(3):275–300. doi: 10.1037/1082-989X.9.3.275. [DOI] [PubMed] [Google Scholar]
- Mason C, Subedi S. Helping parents with mental illnesses and their children: a call for family-focused mental health care. Journal of Psychosocial Nursing and Mental Health Services. 2006;44(7):36–41. doi: 10.3928/02793695-20060701-06. [DOI] [PubMed] [Google Scholar]
- McAdams TA, Rijsdijk FV, Neiderhiser JM, Narusyte J, Shaw DS, Natsuaki MN, … Lichtenstein P. The relationship between parental depressive symptoms and offspring psychopathology: evidence from a children-of-twins study and an adoption study. Psychological Medicine. 2015:1–12. doi: 10.1017/S0033291715000501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay MM, Bannon WM. Engaging families in child mental health services. Child and Adolescent Psychiatric Clinics of North America. 2004;13(4):905–921. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Morrissey-Kane E, Prinz RJ. Engagement in child and adolescent treatment: The role of parental cognitions and attributions. Clinical Child and Family Psychology review. 1999;2(3):183–198. doi: 10.1023/a:1021807106455. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE. Parent expectancies for child therapy: Assessment and relation to participation in treatment. Journal of Child and Family Studies. 2001;10:155–180. [Google Scholar]
- Pelham WE, Gnagy EM, Greenslade KE, Milich R. Teacher ratings of DSM- III-R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31(2):210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Wickramaratne P, Talati A, Tang M, Hughes CW, Garber J, … Alpert JE. Children of depressed mothers 1 year after the initiation of maternal treatment: findings from the STAR* D-Child Study. American Journal of Psychiatry. 2008;165(9):1136–47. doi: 10.1176/appi.ajp.2008.07081286. [DOI] [PubMed] [Google Scholar]
- Rey JM, Plapp JM, Simpson PL. Parental satisfaction and outcome: a 4-year study in a child and adolescent mental health service. Australian and New Zealand Journal of Psychiatry. 1999;33(1):22–28. doi: 10.1046/j.1440-1614.1999.00516.x. [DOI] [PubMed] [Google Scholar]
- Reyno SM, McGrath PJ. Predictors of parent training efficacy for child externalizing behavior problems–a meta_analytic review. Journal of Child Psychology and Psychiatry. 2006;47(1):99–111. doi: 10.1111/j.1469-7610.2005.01544.x. [DOI] [PubMed] [Google Scholar]
- Shapiro CJ, Kilburn J, Hardin JW. Prevention of behavior problems in a selected population: Stepping Stones Triple P for parents of young children with disabilities. Research in Developmental Disabilities. 2014;35(11):2958–2975. doi: 10.1016/j.ridd.2014.07.036. [DOI] [PubMed] [Google Scholar]
- Solberg C, Larsson B, Jozefiak T. Consumer satisfaction with the Child and Adolescent Mental Health Service and its association with treatment outcome: A 3–4- year follow-up study. Nordic Journal of Psychiatry. 2015;69(3):224–232. doi: 10.3109/08039488.2014.971869. [DOI] [PubMed] [Google Scholar]
- Stevens J, Kelleher KJ, Ward-Estes J, Hayes J. Perceived barriers to treatment and psychotherapy attendance in child community mental health centers. Community Mental Health Journal. 2006;42(5):449–458. doi: 10.1007/s10597-006-9048-5. [DOI] [PubMed] [Google Scholar]
- Tas FV, Guvenir T, Cevrim E. Patients’ and their parents’ satisfaction levels about the treatment in a child and adolescent mental health inpatient unit. Journal of Psychiatric and Mental Health Nursing. 2010;17(9):769–774. doi: 10.1111/j.1365-2850.2010.01612.x. [DOI] [PubMed] [Google Scholar]
- Thurston I, Phares V, Coates E, Bogart L. Child problem recognition and help-seeking intentions among black and white parents. Journal of Child and Adolescent Psychology. 2015;44(4):604–615. doi: 10.1080/15374416.2014.883929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theule J, Wiener J, Tannock R, Jenkins JM. Parenting Stress in Families of Children With ADHD A Meta-Analysis. Journal of Emotional and Behavioral Disorders. 2013;21(1):3–17. [Google Scholar]
- Tolan PH, Hanish L, McKay MM, Dickey MH. Evaluating process in child and family interventions: Aggression prevention as an example. Journal of Family Psychology. 2002;16(2):220–236. doi: 10.1037//0893-3200.16.2.220. [DOI] [PubMed] [Google Scholar]
- Waschbusch DA, Willoughby MT. Parent and teacher ratings on the IOWA Conners Rating Scale. Journal of Psychopathology and Behavioral Assessment. 2008;30:180–192. [Google Scholar]