Abstract
PURPOSE
American Indian/Alaska Native (AI/AN) people have the highest traumatic brain injury (TBI)-related mortality in the United States, but little is known about AI/AN children who survive traumatic brain injury (TBI). This study compares function and factors associated with discharge function between AI/AN and White children with TBI during inpatient rehabilitation.
METHODS
Retrospective national cohort study of 114 AI/AN and 7,267 White children aged 6 months-18 years who received inpatient TBI rehabilitation between 2002–2012 at facilities utilizing the Uniform Data System for Medical Rehabilitation®. The outcome measure was developmental functional quotients (DFQ is the FIM® or WeeFIM® score divided by age norms × 100) at discharge.
RESULTS
AI/AN race was not associated with motor (regression coefficient (β) 0.18, 95% confidence interval (CI) −2.39, 2.76) or cognitive (β −1.54, 95% CI −3.75, 0.67) function. Among a subgroup with loss of consciousness > 24 hours (AI/AN n = 13, White n = 643), AI/AN race was associated with lower motor DFQ (β −12.83, 95% CI −25.39, −0.34).
CONCLUSIONS
Overall, AI/AN race was not associated with inpatient rehabilitation function for children with TBI, but providers should not assume AI/ANs with more severe injuries have equitable outcomes.
Keywords: Traumatic brain injury, pediatric rehabilitation, American Indian, Alaska Native, Native Americans
1. Introduction
American Indian and Alaska Native (AI/AN) children have the highest mortality from unintentional injury in the Unites States [1,2]. Further, AI/AN people have the highest traumatic brain injury (TBI)-related mortality in the United States (27.3/100,000 for AI/AN versus 18.4/100,000 for the total population) [3]. Even with the reported disparities in injury and TBI mortality for AI/AN people, few studies have examined TBI treatment and outcomes in this population; moreover, studies among AI/AN children are non-existent.
While the literature is limited for AI/ANs, racial and ethnic disparities in functional outcomes after TBI have been demonstrated for non-AI/AN minority groups. Non-White adults with TBI had worse outcomes across a variety of long-term post-injury measures compared to non-Hispanic White (NHW) adults [4]. Hispanic children had higher levels of disability after TBI compared to NHW children three years after TBI [5]. There have been studies examining disparities during the inpatient rehabilitation period for adults with TBI [6,7], but AI/AN people were either excluded or grouped with other minorities in these studies meaning that the rehabilitation experience for AI/ANs with TBI is unknown.
A disability disparities model proposed by Dr. Allen Lewis identifies potential mechanisms contributing to disparities in rehabilitation outcomes for minority groups, including unequal service quality or quantity, differences in the treatment alliance between rehabilitation teams and families, cultural expectations regarding the value of treatments, and differences in a minority group’s worldview about the health condition causing functional impairment [8]. There is a small body of literature that shows differences between indigenous people of North America (including AI/ANs and indigenous groups in Canada) and the general population in the domains of the disability disparities model. Native North Americans at one Canadian inpatient rehabilitation facility had significantly fewer family conferences during inpatient rehabilitation, suggesting a difference in the service quality and quantity for Native North Americans [9]. Interviews with traditional healers identified culturally specific barriers and facilitators for treating AI/AN patients at a level I trauma center, suggesting a need for improved cultural competence among providers caring for AI/AN patients with traumatic injury [10]. A study of Canadian First Nations elders found differences between the Western and traditional approach to healing after TBI, and stressed the need for culturally safe and responsive occupational therapy services for First Nations individuals with TBI [11]. These studies suggest that the worldview of AI/AN people regarding TBI and cultural expectations for service differs from that of the majority population, which may affect rehabilitation outcomes for AI/AN children with TBI.
Using a national database, this study aims to compare motor and cognitive functional changes during inpatient rehabilitation between AI/AN and White children with TBI, with a hypothesis that AI/AN children will have less gain in function during inpatient rehabilitation. This study also aims to identify factors associated with functional status at discharge from inpatient rehabilitation for children with TBI, with a hypothesis that these factors differ between AI/AN and White children.
2. Methods
2.1. Patient population
This retrospective study of an administrative cohort included children 6 months to 18 years of age, who received initial inpatient TBI rehabilitation between January 1, 2002-December 31, 2012. This study utilized data from the Uniform Data System for Medical Rehabilitation (UDSMR®) which maintains data from over 800 inpatient rehabilitation facilities in the United States, representing approximately 70% of the rehabilitation facilities in the country [12]. Included in this study were children with race/ethnicity coded by rehabilitation unit staff as AI/AN or White in the UDSMR (UDSMR®) database. Other UDSMR race/ethnicity categories include the following: Black, Hispanic, Asian, Other, and Multiracial. In order to focus attention on AI/AN children, the analysis did not include other minority groups. The data provided by UDSMR was de-identified, so this study was exempt from IRB review.
Only children with UDSMR impairment codes corresponding to closed, open, or unspecified TBI and ICD-9 codes related to TBI or late effects of TBI (800.0–801.99, 803.0–804.99, 850.0–854.99, 905.0, 907.0, 959.01, 995.5) were included. TBI diagnostic codes were recorded from the primary rehabilitation diagnosis or one of 10 comorbidity fields. Children with impairment codes related to major multiple trauma, such as spinal cord injury, in addition to TBI were not included.
2.1.1. Functional outcome measures
All patients receiving inpatient rehabilitation at facilities that contribute data to UDSMR are assessed at rehabilitation admission and discharge by physical, occupational, and speech therapists certified in using the Functional Independence Measure (FIM® instrument) or Functional Independence Measure for Children (WeeFIM® instrument). Both instruments measure function in 3 subscales – mobility (5 items), self-care (8 items) and cognition (5 items) – with every item scored from 1 (dependent) to 7 (independent) and use similar scoring criteria. Previous studies have found that the items fall into two domains, cognitive and motor (a combination of the mobility and self-care subscales) [13,14].
Developmental functional quotients (DFQ) [15,16] for the motor and cognitive domains of the FIM (FIM®) and WeeFIM (WeeFIM®) assessments were used as the main outcome measures rather than the raw FIM or WeeFIM scores because of the known effect of age on functional ratings for children under age seven [17]. DFQs allow for comparisons across age groups by providing a quotient score based on age-normative values reported by the UDSMR, and derived from a sample of 414 children without known disability or developmental delay [18]. DFQs are provided by UDSMR for all patients assessed using the WeeFIM instrument. For patients for whom the FIM instrument was used, DFQs were calculated following the methodology of the WeeFIM instrument, where DFQ is calculated by taking the raw WeeFIM score divided by age norms multiplied by 100.
A higher DFQ indicates that a child functions closer to the level expected by age. At the age of 7, a typically developing child is expected to achieve independence on all items, such that the normative score for children 7 and older is 126, the highest possible FIM or WeeFIM score. For children under age seven, it is possible to have a DFQ above 100 if a child functions at a higher level than anticipated based on age. To control for outliers with DFQs that did not make sense clinically, cases with DFQ at admission or discharge above 150 were excluded.
2.2. Covariates
Other information in the UDSMR dataset included age, gender, race, discharge year, rehabilitation length of stay and primary payer for the rehabilitation admission. Primary payer is the only marker of socioeconomic status within the UDSMR dataset and was categorized as commercial insurance coverage, Medicaid/governmental insurance coverage, or other.
Based on clinical experience, AI/AN children may be admitted to inpatient rehabilitation with higher levels of function after less severe injury than the average patient with TBI because of limited access to outpatient rehabilitation services, making injury severity a covariate of interest. Injury severity predicts long term function [19–21], but unfortunately is not directly captured in the UDSMR database. Time from injury onset to rehabilitation admission is a proxy for injury severity [22,23], but this variable was only provided for children assessed with the FIM and not with the WeeFIM in this dataset. The UDSMR dataset contains International Classification of Disease (ICD-9) diagnostic codes for traumatic brain injury assigned by providers at the rehabilitation facility. The fifth digit of ICD-9 codes 800.00–801.99, 803.00–804.99, and 850.00–854.99 indicates the presence and duration of loss of consciousness (LOC) in the setting of TBI. Each subject was classified as having LOC less than or equal to 24 hours, LOC 24 hours or more, or an unknown length of LOC (ICD-9 fifth digit values of 0, 6, or 9, or with ICD-9 codes that do not indicate LOC). Length of LOC was used as a marker of injury severity in the subgroup of children with known length of LOC.
2.3. Data analysis
Differences between the AI/AN and White groups in demographic variables were examined with chi-square statistics and t-tests. To compare functional outcomes between AI/AN and White groups, t-tests were used for admission and discharge DFQs for the motor and cognitive domains. An exploratory subgroup analysis among AI/AN and White subjects with known length of LOC was performed using t-tests to compare admission and discharge DFQs for the motor and cognitive domains.
To determine the independent association of race with motor and cognitive discharge DFQ, and to assess if factors associated with discharge DFQ differed between the AI/AN and White groups, multiple linear regressions clustered by facility using robust standard errors were performed with the AI/AN and White cohorts together and separately. Exploratory regression analyses were performed for the subgroups with known length of LOC. All regression models used motor or cognitive discharge DFQ as the dependent variable. Independent variables were established on a priori hypotheses and included admission DFQ, age, gender, year of discharge from rehabilitation, length of stay, insurance, and race. There had been concern that admission DFQ would be collinear with length of stay; measures of collinearity showed that both admission DFQ and length of stay were not collinear and thus both were included in the regression model. Year of discharge from rehabilitation was included to account for potential changes in care over the 11 year study period.
Statistical significance was set at a p-value of 0.05 for all analyses. Stata® 13 (StataCorp, College Station, TX) was used for statistical analyses.
3. Results
3.1. Demographics
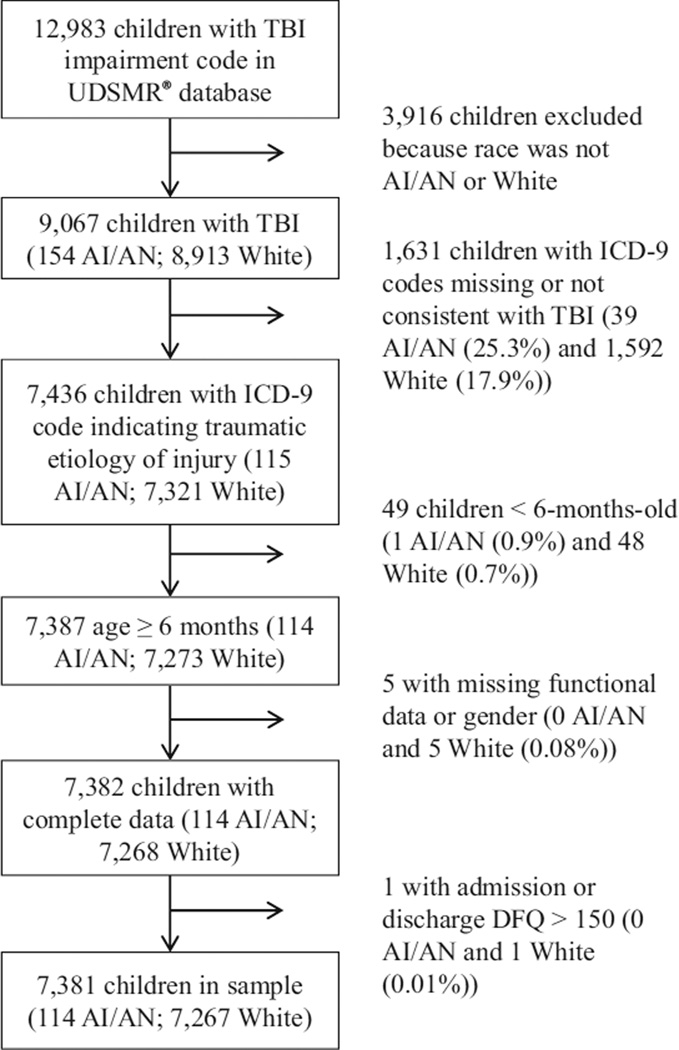
The sample consisted of 114 AI/AN and 7,267 White children (Fig. 1). As shown in Table 1, there was no significant difference between the AI/AN and White groups in gender, mean age or rehabilitation length of stay. A subgroup of 1,333 children (18%) had diagnostic codes indicative of length of loss of consciousness. There was no significant difference between the AI/AN and White groups in the distribution of patients with unknown length of LOC, LOC less than or equal to 24 hours, or LOC greater than 24 hours. AI/AN children were more likely to have non-commercial insurance (76% versus 31%, p < 0.001) and be evaluated with the FIM instrument (73% versus 55%, p < 0.001) compared to White children. The demographic trends were similar in the 1,333 children (24 AI/AN and 1,309 White) with known length of LOC, and there was no significant difference in mean age or length of rehabilitation stay between the AI/AN and White children when stratified by length of LOC.
Fig. 1.
Study population. Abbreviations: AI/AN (American Indian/Alaska Native), DFQ (Developmental Functional Quotients), ICD-9 (International Classification of Diseases, Ninth Revision), TBI (traumatic brain injury), UDSMR® (Uniform Data System for Medical Rehabilitation).
Table 1.
Patient characteristics by race and length of loss of consciousness, UDSMR® 2002–2012
| All TBI | LOC ≤ 24 hours | LOC > 24 hours | |||||||
|---|---|---|---|---|---|---|---|---|---|
| AI/AN (n = 114) |
White (n = 7,267) |
p | AI/AN (n = 11) |
White (n = 666) |
p | AI/AN (n = 13) |
White (n = 643) |
p | |
| Gender, % | 0.60 | 0.86 | 0.48 | ||||||
| Male | 69 | 67 | 73 | 70 | 54 | 63 | |||
| Female | 31 | 33 | 27 | 30 | 46 | 37 | |||
| Age, years; M (SD) | 14.2 (4.8) | 14.2 (4.6) | 0.93 | 13.5 (4.7) | 14.4 (4.2) | 0.46 | 13.3 (6.6) | 13.1 (4.9) | 0.46 |
| Insurance type, % | < 0.001 | < 0.001 | 0.002 | ||||||
| Commercial | 24 | 68 | 18 | 74 | 15 | 64 | |||
| Medicaid/Gov’t | 62 | 24 | 64 | 18 | 62 | 27 | |||
| Other | 14 | 8 | 18 | 8 | 23 | 9 | |||
| LOS, days; M (SD) | 19.4 (18.7) | 22.8 (27.7) | 0.19 | 8.9 (7.8) | 15.6 (22.7) | 0.33 | 29.2 (21.5) | 32.3 (30.4) | 0.71 |
| Data Source, % | < 0.001 | 0.22 | 0.006 | ||||||
| FIM® | 73 | 55 | 82 | 64 | 77 | 39 | |||
| WeeFIM® | 27 | 45 | 18 | 36 | 23 | 61 | |||
| Length of LOC | 0.61 | ||||||||
| LOC ≤ 24 hours | 10 | 9 | - | - | - | - | - | - | |
| LOC > 24 hours | 11 | 9 | - | - | - | - | - | - | |
| Unknown LOC | 79 | 82 | - | - | - | - | - | - | |
Abbreviations: AI/AN (American Indian/Alaska Native), FIM® (Functional Independence Measure), WeeFIM® (Functional Independence Measure for Children), Gov’t (governmental insurance), LOS (length of stay), LOC (loss of consciousness), M (mean), SD (standard deviation), TBI (traumatic brain injury), UDSMR® (Uniform Data System for Medical Rehabilitation).
3.2. Developmental functional quotients
Table 2 shows the mean admission and discharge DFQs for the motor and cognitive domains of the FIM and WeeFIM instruments, with subgroups stratified by length of LOC. AI/AN children had higher motor DFQ at admission than White children (mean difference, 7.3, 95% confidence interval (CI) 3.3 to 11.3). Among children with LOC less than or equal to 24 hours, AI/AN children had higher admission motor DFQ than White children (mean difference 12.4, 95% CI 0.2 to 24.6). There were no statistically significant differences in discharge DFQ between the groups, though there was a trend toward a lower discharge motor DFQ (mean difference −12.2, 95% CI −25.3 to 0.9) for AI/AN compared to White children with LOC greater than 24 hours.
Table 2.
Unadjusted Developmental Functional Quotients by race and length of loss of consciousness
| All TBI | LOC ≤ 24 hours | LOC > 24 hours | ||||
|---|---|---|---|---|---|---|
| AI/AN (n = 114) |
White (n = 7,267) |
AI/AN (n = 11) |
White (n = 666) |
AI/AN (n = 13) |
White (n = 643) |
|
| Motor DFQ | ||||||
| Admission | 47 (43–51) | 40 (40–41) | 62 (51–74) | 50 (48–52) | 34 (22–47) | 32 (30–33) |
| Discharge | 76 (72–80) | 72 (72–73) | 83 (71–95) | 80 (78–81) | 56 (40–72) | 68 (66–70) |
| Cognitive DFQ | ||||||
| Admission | 45 (41–50) | 42 (42–43) | 60 (44–76) | 51 (49–53) | 34 (25–43) | 35 (33–36) |
| Discharge | 66 (62–70) | 66 (66–67) | 73 (60–86) | 73 (72–75) | 55 (42–67) | 63 (61–64) |
Note. Values presented are mean DFQ (95% confidence interval).
Abbreviations: DFQ (Developmental Functional Quotients), LOC (loss of consciousness), TBI (traumatic brain injury), AI/AN (American Indian/Alaska Native), FIM® (Functional Independence Measure), WeeFIM® (Functional Independence Measure for Children).
3.3. Regression analyses
In the primary multiple linear regression models, AI/AN race was not independently associated with discharge motor or cognitive DFQ. When adjusting for all covariates, discharge DFQ in the motor and cognitive domains was significantly associated with admission DFQ, patient age and insurance status. In the cognitive domain, female gender was significantly associated with a higher discharge DFQ (regression coefficient (β) 1.13, 95% CI 0.28 to 1.99). Younger patients and those with Medicaid/governmental insurance had lower discharge DFQ in both domains (p ≤ 0.002). A discharge year later in the study period was associated with a lower motor discharge DFQ (p = 0.04). (Table 3)
Table 3.
Results of multiple linear regressions examining the associations between demographic variables and discharge motor and cognitive Developmental Functional Quotient
| All (n =7,381) | AI/AN (n= 114) | White (n= 7,267) | ||||
|---|---|---|---|---|---|---|
| Motor | Cognitive | Motor | Cognitive | Motor | Cognitive | |
| Age, years | 0.97 | 0.38 | 1.08 | 0.46 | 0.97 | 0.38 |
| (0.82, 1.13) | (0.20, 0.57) | (0.41, 1.74) | (0.01, 0.92) | (0.81, 1.13) | (0.19, 0.57) | |
| Gender | ||||||
| Male (Ref) | - | - | - | - | - | - |
| Female | −0.49 | 1.13 | 1.08 | −0.96 | −0.50 | 1.18 |
| (−1.62, 0.63) | (0.28, 1.99) | (−7.76, 9.92) | (−7.39, 5.46) | (−1.64, 0.65) | (0.33, 2.03) | |
| Race | ||||||
| White (Ref) | - | - | - | - | - | - |
| AI/AN | 0.18 | −1.54 | ||||
| (−2.39, 2.76) | (−3.75, 0.67) | - | - | - | - | |
| Discharge year | −0.21 | 0.20 | −0.03 | 1.02 | −0.21 | 0.18 |
| (−0.40, −0.02) | (−0.04, 0.44) | (−1.04, 0.98) | (0.11, 1.93) | (−0.40, −0.02) | (−0.06, 0.43) | |
| Insurance | ||||||
| Commercial (Ref) | - | - | - | - | - | - |
| Medicaid/Gov’t. | −2.03 | −1.65 | −1.54 | −1.97 | −2.07 | −1.67 |
| (−3.10, −0.97) | (−2.67, −0.63) | (−8.55, 5.46) | (−8.30, 4.36) | (−3.15, −1.00) | (−2.70, −0.65) | |
| Other | −0.09 | −0.73 | −5.70 | −3.38 | 0.03 | −0.64 |
| (−2.13, 1.94) | (−2.29, 0.84) | (−14.85, 3.45) | (−12.00, 5.25) | (−2.10, 2.15) | (−2.27, 0.98) | |
NOTE: All regression models cluster by facility and adjust for admission developmental functional quotients and length of stay. Values are unstandardized regression coefficients (95% CI).
Abbreviations: AI/AN (American Indian/Alaska Native), DFQ (Developmental Functional Quotient), Gov’t (Governmental), Ref (reference category).
Separate regression analyses for the AI/AN and White cohorts identified differences between the cohorts in the factors that were associated with discharge DFQ. Insurance status was associated with the motor and cognitive domains only for the White cohort (p ≤ 0.002) and not significantly associated with discharge function for the AI/AN cohort. Discharge year was more strongly associated with discharge cognitive DFQ for AI/AN children compared to White children (β 1.02, 95% CI 0.11 to 1.93 versus β 0.18, 95% CI −0.06 to 0.43). (Table 3)
In the exploratory subgroup analysis of those children with known LOC (n = 1,333, AI/AN= 24, White = 1,309), AI/AN race was independently associated with a lower motor discharge DFQ (β −7.56, 95% CI −14.84 to −0.28), after adjusting for the other covariates. For children with LOC lasting 24 hours or longer, AI/AN race was associated with a 12.86 point lower discharge motor DFQ (β −12.83, 95% CI −25.39 to −0.34) (Table 4).
Table 4.
Results of multiple linear regressions examining the associations between demographic variables and discharge motor and cognitive Developmental Functional Quotient in the subgroup with known length of loss of consciousness
| Known LOC (n = 1,333) | LOC ≤ 24 hours (n = 677) | LOC > 24 hours (n = 656) | ||||
|---|---|---|---|---|---|---|
| Motor | Cognitive | Motor | Cognitive | Motor | Cognitive | |
| Age, years | 0.98 | 0.36 | 1.03 | 0.21 | 1.01 | 0.50 |
| (0.76, 1.20) | (0.09, 0.63) | (0.77, 1.29) | (−0.30, 0.72) | (0.70, 1.32) | (0.22, 0.78) | |
| Gender | ||||||
| Male (Ref) | - | - | - | - | - | - |
| Female | −0.25 | 1.39 | 0.23 | 3.07 | −0.49 | 0.08 |
| (−2.10, 1.61) | (−0.65, 3.44) | (−2.01, 2.46) | (0.90, 5.24) | (−3.17, 2.20) | (−3.04, 3.20) | |
| Race | ||||||
| White (Ref) | - | - | - | - | - | - |
| AI/AN | −7.56 | −5.67 | −0.63 | −4.06 | −12.86 | −6.87 |
| (−14.84, −0.28) | (−12.12, 0.77) | (−5.93, 4.67) | (−11.42, 3.29) | (−25.39, −0.34) | (−17.45, 3.71) | |
| Insurance | ||||||
| Commercial (Ref) | - | - | - | - | - | - |
| Medicaid/Gov’t | −2.03 | −2.15 | −1.38 | −1.06 | −2.64 | −2.84 |
| (−4.06, −0.00) | (−4.56, 0.27) | (−3.72, 0.96) | (−3.77, 1.65) | (−6.01, 0.74) | (−7.18, 1.49) | |
| Other | −0.88 | −1.64 | −0.26 | −0.74 | −1.33 | −2.41 |
| (−4.88, 3.12) | (−5.03, 1.75) | (−3.79, 3.28) | (−4.22, 2.74) | (−7.38, 4.72) | (−8.25, 3.43) | |
NOTE: All regression models cluster by facility and adjust by admission developmental functional quotient, length of stay and discharge year. Values are unstandardized regression coefficients (95% CI).
Abbreviations: AI/AN (American Indian/Alaska Native), DFQ (Developmental Functional Quotients), Gov’t (Governmental), LOC (loss of consciousness), Ref (reference category), TBI (traumatic brain injury).
4. Discussion
This study of a national sample of AI/AN and White children with TBI undergoing inpatient rehabilitation found race was not significantly associated with discharge function. AI/AN children with TBI differed from White children in the variables that were associated with functional improvements during rehabilitation. A discharge year toward the end of the study period was associated with a higher cognitive discharge function for AI/AN children compared to White children. Female gender was associated with higher discharge cognitive function for White children but not AI/AN children.
In concordance with other studies [24,25], admission functional scores and age were associated with discharge functional scores for AI/AN and White children with TBI in this study. Similar to this study, a recent study found the effect of Hispanic and Non-Hispanic Black race/ethnicity on discharge function after inpatient rehabilitation for TBI was non-significant after adjustment for other variables including insurance status [26].
In an exploratory subgroup analyses among the children that had known length of LOC, AI/AN race was associated with a lower discharge functional score in the motor domain after adjusting for admission function, age, gender, discharge year and insurance. Given the limited number of AI/AN children in this dataset with known length of LOC, this finding would benefit from confirmation with a study designed specifically to compare rehabilitation outcomes among AI/AN and White children. Hypotheses for why AI/AN children with more severe injuries may have lower discharge motor DFQ need to be investigated, but could include AI/AN children having limited support due to the distance from child’s home to the rehabilitation facility (as seen in the authors’ clinical experience), treatment alliance mismatch related to cultural factors for AI/AN children and their families (as suggested by Dr. Lewis’s Disability Disparities Model [8]), or different family-team communication during the rehabilitation process for AI/AN children (similar to the differences seen in the Saskatchewan inpatient rehabilitation unit where indigenous patients had fewer family-team meetings [9]). These factors could be magnified with the longer length of stay needed for rehabilitation of a more severe injury.
The year of discharge from rehabilitation was more strongly associated with cognitive outcomes among AI/AN children than among White children in this study. An AI/AN child discharged from a rehabilitation facility in 2012 was predicted to have a cognitive discharge score 11 points higher compared to a AI/AN child discharged in 2002; for White children, discharge year was not significantly associated with cognitive function at discharge. A hypothesized mechanism for this improvement over time is that infrastructure upgrades allowed AI/AN communities improved access to internet and cellular phone services, which may have made it easier for AI/AN children to communicate with their extended families and meaningfully use the skills being measured in the cognitive domain of the FIM and WeeFIM instruments. In 1995, 20% of AI/AN households had a personal computer and less than 5% of AI/AN households had a computer with internet access; in 2012 68% of AI/AN household had a computer and 58% have internet access at home [27]. Further investigation into the rehabilitation experience of AI/AN children may elucidate potential mechanisms that could be utilized to further improve functional outcomes for this population.
4.1. Study limitations
This retrospective study has several limitations. The number of AI/AN included in the database is small. Previous studies have shown it was far more likely for an AI/AN person to be ascribed a different race/ethnicity rather than a non-AI/AN person being identified as AI/AN [28,29]. It is likely that not all AI/AN children with TBI treated at UDSMR-subscribing facilities were correctly classified by race, lowering the AI/AN sample size and power of the study.
There were no direct indicators of injury severity in the UDSMR database. Time from injury to rehabilitation admission was non-randomly missing for 45% of the sample. Admission functional score and change in functional score during rehabilitation have been shown to be inversely related to length of time from injury to rehabilitation admission [24]. Without being able to control length of time from injury to rehabilitation admission, functional score at admission was thought to be an insufficient proxy measure of injury severity. Length of LOC was only specified in 18% of the total sample, and will vary by the facility processes of recording diagnostic codes, but was the best available surrogate measure of injury severity in this dataset. Comparing several variables by length of LOC indicated that grouping by length of LOC differentiated subgroups that were functionally different and with different rehabilitation length of stay. However, it is unclear how representative the subgroup with length of LOC recorded in the diagnostic code is of the study population who did not have detailed diagnostic codes.
A national database linking injury markers and acute care outcomes with the functional outcomes found in the UDSMR datasets for children with TBI would eliminate the need for proxy measurement of injury severity. The TBI Model Systems serve this need for adults and older teens, but only for those seen at Model System centers, which are not currently located in areas with large AI/AN populations.
The only available marker of socioeconomic status in the dataset was insurance type. The dataset does not accurately capture poverty – which is more highly concentrated in in the Southeast and on AI/AN tribal land [30]. Parents of families living in poverty may need to continue working to meet their family’s financial needs and thus they may not attend their child’s inpatient rehabilitation therapy sessions and learn how to promote their child’s progress. This is hypothesized to influence the child’s ability to practice functional skills with their family outside of formal therapy sessions and the child’s overall functional improvement. While the WeeFIM instrument contains a variable indicating household structure, the FIM instrument does not. American Indian and Alaska Native children are more likely to live in single-parent households [31,32], which may affect parental presence during rehabilitation. Research on the association of family presence throughout rehabilitation and functional outcome may reveal mechanisms through which disparities in functional outcomes develop.
5. Conclusions
Representing a small percentage of the overall population, AI/AN children bear a disproportionate burden of traumatic injury. This study indicates that overall, AI/AN race is not associated with functional outcomes during inpatient rehabilitation for children with TBI, but rehabilitation providers should not assume AI/AN with more severe injuries have the same rehabilitation experience as the general population. The importance of culturally-sensitive care in achieving optimal rehabilitation outcomes is increasingly acknowledged [33]. Rehabilitation physicians who scored higher on a test of implicit racial bias had patients with more limitations in social integration, higher levels of depression and lower life satisfaction than physicians who demonstrated less implicit bias [34]. The link between cultural sensitivity and patient outcomes is corroborated outside of rehabilitation. Minority patients with HIV whose providers have higher self-rating of cultural competenence are more likely to be on appropriate treatments and report higher self-efficacy than patients whose providers reported lower self-rated cultural competence [35]. Further research is needed to understand the AI/AN experience of injury and rehabilitation in order to support the development or adaptation of culturally-sensitive interventions to improve the rehabilitation experience and outcomes for AI/AN children.
Acknowledgments
Molly Fuentes receives support from the National Institute of Child Health and Human Development (5T32HD057822-05, PI: Frederick P. Rivara). Nathalia Jimenez receives support from the National Institute for Child Health and Human Development (1K23H DO7843-01).
Footnotes
Conflict of interest
The authors have no conflict of interest to declare.
References
- 1.Centers for Disease Control and Prevention. Vital signs: Unintentional injury deaths among persons aged 0–19 years – United States, 2000–2009. MMWR Morb Mortal Wkly Rep. 2012;61:270–276. [PubMed] [Google Scholar]
- 2.Wong CA, Gachupin FC, Holman RC, MacDorman MF, Cheek JE, Holve S, et al. American Indian and Alaska Native Infant and Pediatric Mortality, United States, 1999–2009. American Journal of Public Health. 2014;104(S3):S320–S328. doi: 10.2105/AJPH.2013.301598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, Faul MD, et al. Surveillance for traumatic brain injury-related deaths-United States, 1997–2007. MMWR Surveill Summ. 2011;60(5):1–32. [PubMed] [Google Scholar]
- 4.Arango-Lasprilla JC, Kreutzer JS. Racial and ethnic disparities in functional, psychosocial, and neurobehavioral outcomes after brain injury. J Head Trauma Rehabil. 2010;25(2):128–136. doi: 10.1097/HTR.0b013e3181d36ca3. [DOI] [PubMed] [Google Scholar]
- 5.Jimenez N, Ebel BE, Wang J, Koepsell TD, Jaffe KM, Dorsch A, et al. Disparities in disability after traumatic brain injury among Hispanic children and adolescents. Pediatrics. 2013;131(6):e1850–e1856. doi: 10.1542/peds.2012-3354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rosenthal M, Dljkers M, Harrison-Felix C, Nabors N, Witol AD, Young ME, et al. Impact of Minority Status on Functional Outcome and Community Integration Following Traumatic Brain Injury. J Head Trauma Rehabil. 1996;11(5):40–57. [Google Scholar]
- 7.Burnett DM, Kolakowsky-Hayner SA, Slater D, Stringer A, Bushnik T, Zafonte R, et al. Ethnographic analysis of traumatic brain injury patients in the national Model Systems database. Arch Phys Med Rehabil. 2003;84(2):263–267. doi: 10.1053/apmr.2003.50091. [DOI] [PubMed] [Google Scholar]
- 8.Lewis A. Disability disparities: a beginning model. Disabil Rehabil. 2009;31(14):1136–1143. doi: 10.1080/09638280902773737. [DOI] [PubMed] [Google Scholar]
- 9.Blackmer J, Marshall SC. A comparison of traumatic brain injury in the Saskatchewan native North American and non-native North American populations. Brain Inj. 1999;13(8):627–635. doi: 10.1080/026990599121359. [DOI] [PubMed] [Google Scholar]
- 10.Bassett D, Tsosie U, Nannauck S. “Our culture is medicine”: perspectives of Native healers on posttrauma recovery among American Indian and Alaska Native patients. Perm J. 2012;16(1):19–27. doi: 10.7812/tpp/11-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keightley ML, King GE, Jang SH, White RJ, Colantonio A, Minore JB, et al. Brain injury from a first nations’ perspective: teachings from elders and traditional healers. Can J Occup Ther. 2011;78(4):237–245. doi: 10.2182/cjot.2011.78.4.5. [DOI] [PubMed] [Google Scholar]
- 12.Buffalo: UB Foundation Activities; 2014. [[cited 2014 Oct 1]]. Uniform Data System for Medical Rehabilitation: The Functional Assessment Specialists [Internet] Available from: http://www.udsmr.org/WebModules/Pro/Pro_About.aspx. [Google Scholar]
- 13.Chen CC, Bode RK, Granger CV, Heinemann AW. Psychometric properties and developmental differences in children’s ADL item hierarchy: a study of the WeeFIM instrument. Am J Phys Med Rehabil. 2005;84(9):671–679. doi: 10.1097/01.phm.0000176439.32318.36. [DOI] [PubMed] [Google Scholar]
- 14.Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Measurement characteristics of the Functional Independence Measure. Top Stroke Rehabil. 1994;1(3):1–15. doi: 10.1080/10749357.1994.11754030. [DOI] [PubMed] [Google Scholar]
- 15.Msall ME, Tremont MR. Measuring functional status in children with genetic impairments. Am J Med Genet. 1999;89(2):62–74. doi: 10.1002/(sici)1096-8628(19990625)89:2<62::aid-ajmg3>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 16.Suskauer SJ, Slomine BS, Inscore AB, Lewelt AJ, Kirk JW, Salorio CF. Injury severity variables as predictors of WeeFIM scores in pediatric TBI: Time to follow commands is best. J Pediatr Rehabil Med. 2009;2(4):297–307. [PMC free article] [PubMed] [Google Scholar]
- 17.Msall ME, DiGaudio K, Rogers BT, LaForest S, Catanzaro NL, Campbell J, et al. The Functional Independence Measure for Children (WeeFIM). Conceptual basis and pilot use in children with developmental disabilities. Clin Pediatr (Phila) 1994;33(7):421–430. doi: 10.1177/000992289403300708. [DOI] [PubMed] [Google Scholar]
- 18.Uniform Data System for Medical R. The WeeFIM II® Clinical Guide, Version 6.0. Buffalo, NY: Author; 2006. [Google Scholar]
- 19.Catroppa C, Godfrey C, Rosenfeld JV, Hearps SS, Anderson VA. Functional recovery ten years after pediatric traumatic brain injury: outcomes and predictors. J Neurotrauma. 2012;29(16):2539–2547. doi: 10.1089/neu.2012.2403. [DOI] [PubMed] [Google Scholar]
- 20.Anderson V, Godfrey C, Rosenfeld JV, Catroppa C. Predictors of cognitive function and recovery 10 years after traumatic brain injury in young children. Pediatrics. 2012;129(2):e254–e261. doi: 10.1542/peds.2011-0311. [DOI] [PubMed] [Google Scholar]
- 21.Rassovsky Y, Levi Y, Agranov E, Sela-Kaufman M, Sverdlik A, Vakil E. Predicting long-term outcome following traumatic brain injury (TBI) J Clin Exp Neuropsychol. 2015:1–13. doi: 10.1080/13803395.2015.1015498. [DOI] [PubMed] [Google Scholar]
- 22.Ryser DK, Egger MJ, Horn SD, Handrahan D, Gandhi P, Bigler ED. Measuring medical complexity during inpatient rehabilitation after traumatic brain injury. Arch Phys Med Rehabil. 2005;86(6):1108–1117. doi: 10.1016/j.apmr.2004.11.041. [DOI] [PubMed] [Google Scholar]
- 23.Whyte J, Katz D, Long D, DiPasquale MC, Polansky M, Kalmar K, et al. Predictors of outcome in prolonged posttraumatic disorders of consciousness and assessment of medication effects: A multicenter study. Arch Phys Med Rehabil. 2005;86(3):453–462. doi: 10.1016/j.apmr.2004.05.016. [DOI] [PubMed] [Google Scholar]
- 24.Rice SA, Blackman JA, Braun S, Linn RT, Granger CV, Wagner DP. Rehabilitation of children with traumatic brain injury: descriptive analysis of a nationwide sample using the WeeFIM. Arch Phys Med Rehabil. 2005;86(4):834–836. doi: 10.1016/j.apmr.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 25.Niedzwecki CM, Marwitz JH, Ketchum JM, Cifu DX, Dillard CM, Monasterio EA. Traumatic brain injury: a comparison of inpatient functional outcomes between children and adults. J Head Trauma Rehabil. 2008;23(4):209–219. doi: 10.1097/01.HTR.0000327253.61751.29. [DOI] [PubMed] [Google Scholar]
- 26.Jimenez N, Osorio M, Ramos JL, Apkon S, Ebel BE, Rivara FP. Functional Independence after Inpatient Rehabilitation for Traumatic Brain Injury among Minority Children and Adolescents. Arch Phys Med Rehabil. 2015;96(7):1255–1261. doi: 10.1016/j.apmr.2015.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Parkhurst ND, Morris T, Tahy E, Mossberger K. The digital reality: e-government and access to technology and internet for American Indian and Alaska Native populations. Proceedings of the 16th Annual International Conference on Digital Government Research; 2015 May 27; ACM; [Google Scholar]
- 28.Jim MA, Arias E, Seneca DS, Hoopes MJ, Jim CC, Johnson NJ, et al. Racial Misclassification of American Indians and Alaska Natives by Indian Health Service Contract Health Service Delivery Area. Am J Public Health. 2014;104(S3):S295–S302. doi: 10.2105/AJPH.2014.301933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith N, Iyer RL, Langer-Gould A, Getahun DT, Strickland D, Jacobsen SJ, et al. Health plan administrative records versus birth certificate records: quality of race and ethnicity information in children. BMC Health Serv Res. 2010;10:316. doi: 10.1186/1472-6963-10-316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Farrigan T. Washington, DC: United States Department of Agriculture; 2014. [[updated 2015 December 17, cited 2015 Apr 08]]. Geography of Poverty [Internet] Available from: http://www .ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/geography-of-poverty.aspx. [Google Scholar]
- 31.Ness M, Barradas DT, Irving J, Manning SE. Correlates of overweight and obesity among American Indian/Alaska Native and Non-Hispanic White children and adolescents: National Survey of Children’s Health, 2007. Matern Child Health J. 2012;16(Suppl 2):268–277. doi: 10.1007/s10995-012-1191-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The Annie E. Casey Foundation. The 2014 KIDS COUNT Data Book. Baltimore, MD: The Annie E. Casey Foundation; 2014. [Google Scholar]
- 33.Lequerica A, Krch D. Issues of cultural diversity in acquired brain injury (ABI) rehabilitation. NeuroRehabilitation. 2014;34(4):645–653. doi: 10.3233/NRE-141079. [DOI] [PubMed] [Google Scholar]
- 34.Hausmann LR, Myaskovsky L, Niyonkuru C, Oyster ML, Switzer GE, Burkitt KH, et al. Examining implicit bias of physicians who care for individuals with spinal cord injury: A pilot study and future directions. J Spinal Cord Med. 2015;38(1):102–110. doi: 10.1179/2045772313Y.0000000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saha S, Korthuis PT, Cohn JA, Sharp VL, Moore RD, Beach MC. Primary care provider cultural competence and racial disparities in HIV care and outcomes. J Gen Intern Med. 2013;28(5):622–629. doi: 10.1007/s11606-012-2298-8. [DOI] [PMC free article] [PubMed] [Google Scholar]