Abstract
Background
Colorectal cancer is a common and potentially deadly disease. While the U.S. has robust cancer data reporting, information from the Department of Veterans Affairs (VA) healthcare system is often underrepresented in national cancer data sources. In this article, we describe Veterans with incident colorectal cancer (CRC) in terms of their patient and tumor characteristics, as well as their mortality.
Patients and Methods
Patients diagnosed or treated with CRC at any VA institution from fiscal years 2009 to 2012 were identified using three data sources: 1) VA Central Cancer Registry (VACCR); 2) VA Corporate Data Warehouse (CDW); and 3) VA Reports and Measures Portal. CRC frequencies within the VA population and survival curves were examined descriptively and compared with national projections of SEER program data.
Results
There were 12,551 Veterans with CRC included in analysis. Median age at diagnosis was 65.5 years. Approximately 97% (n=12,229) of the CRC cases were diagnosed among men. Approximately 44% (n=5,517) of patients were diagnosed with localized disease. Three-year survival was associated with age (p<0.01) and stage (p<0.01) at diagnosis. We identified a possible decrease in VA CRC incidence over time.
Conclusion
While the VA CRC patient population is heavily skewed toward the male gender, patient and tumor characteristics are similar between incident CRC cases reported by VACCR and SEER. This suggests that research findings resulting from the VACCR might have applicability beyond the VA healthcare system setting.
Keywords: colorectal, neoplasms, United States Department of Veterans Affairs, incidence, mortality
INTRODUCTION
Colorectal cancer (CRC) is the third most commonly diagnosed and third leading cause of cancer-related death among men and women in the United States.1 The National Cancer Institute (NCI) recently issued a report with national projections for the new CRC cases and deaths using the population-based Surveillance, Epidemiology, and End Results (SEER) registry.2 While the SEER registry covers approximately 30% of the U.S. population, Veterans Affairs (VA) cancer registry data has historically been underreported to SEER.3 Although current VA policy enables data sharing with local state registries4, not all states have data sharing agreements. This may result in the omission of important cancer data because the VA is the largest integrated healthcare system providing cancer care in the U.S. and CRC is the second most commonly diagnosed cancer among veterans. The VA treats approximately 3% of all CRC in the U.S. each year, including approximately 6% of cases among men. Therefore, describing CRC among VA healthcare system users is important.5
Relative to the general U.S. population, Veterans receiving care in the VA healthcare system are, on average, older and often have a higher comorbidity burden.5,6 Veterans may also engage in different health behaviors that impact cancer risk. For example, prevalence of smoking is higher among Veterans.7,8 While Veterans and non-Veterans have similar rates of obesity, Veterans may be more likely to have a poor diet (low in fruits and vegetables).8,9 Whether these or other risk factors impact patterns of CRC diagnosis and disease characteristics is unknown. Additionally, the VA has a robust history of national CRC screening programs10 that might influence disease patterns, such as stage of diagnosis.5 In this article, we describe patient and tumor characteristics, as well as CRC incidence and mortality, for Veterans diagnosed with CRC between 2009 and 2012.
MATERIALS AND METHODS
Data Sources
This analysis used three data sources: 1) VA Central Cancer Registry (VACCR); 2) VA Corporate Data Warehouse (CDW); and 3) VA Reports and Measures Portal. CRC cases were identified in the VACCR. The VACCR has previously been described in detail.5 The VACCR receives data collected from local cancer registrars at VA Medical Centers across the country. Cancer registry data are aggregated and cleaned by the VACCR. The VACCR captures approximately 90% of cancer cases treated in VA healthcare system.11 Cases are captured in VACCR even when a patient is diagnosed outside of the VA healthcare system, but subsequently receives cancer care within VA. VACCR data are manually collected by field-based cancer registrars operating at VA Medical Centers nationwide. At routine intervals data are transmitted to the national cancer registry, located in Washington, D.C., where cases are aggregated and cleaned. The VACCR was the source of data for patient characteristics (e.g., age at diagnosis, sex, race) and disease characteristics (e.g., year of diagnosis, stage, tumor type and location). Data were obtained for incident CRC cases diagnosed in fiscal years 2009 through 2012.
Data were also obtained from the Corporate Data Warehouse (CDW) through the VA Informatics and Computing Infrastructure (VINCI). CDW is a national repository of VA clinical and administrative data. VINCI is a computing infrastructure containing multiple datasets originating from the VA’s nationwide electronic medical record and associated sources, including the CDW. Using CDW, VA electronic health record data were used to obtain clinical, demographic, and administrative information. We verified patients’ demographic characteristics (e.g., sex, race) and vital status. When there were discrepancies between data sources, a hierarchical approach was used to select the best available information from inpatient files, outpatient files, and the VACCR, respectively.
Additional data sources included the VA Reports and Measures Portal, which provided the distribution of VA healthcare system enrollees for corresponding years. Using these data, we made age and gender adjustments to incidence rates for the underlying VA patient population.
Eligibility Criteria and Variable Definitions
Eligible patients met the following criteria: diagnosed with incident colorectal cancer between October 1, 2009 through September 30, 2012; have stage I–IV disease; and have a clinical visit with a VA primary care provider and/or medical oncologist in the year prior to their cancer diagnosis (to include only patients who use the VA healthcare system for their care). Patients with missing data on sex or who were classified as transsexual were omitted from analysis.
CRC cases were categorized according to the International Classification of Diseases for Oncology as either colon (C18.0, C18.9, and C26.0) or rectum (C19.9 and C20.9).2,12 Cases were further classified by location as proximal (C18.0 and C18.2–C18.5), distal (C18.6–18.7), or other (C18.1, C18.8, C18.9, and C26.0). Stage was defined according to SEER Summary Stage13; categories for regional stages were collapsed (e.g., local, regional, distant, unknown). Sex was defined as male or female. Race was also included (e.g., white, black, other minority race, unknown).
Statistical Analysis
Frequency distributions of incident CRC diagnoses were evaluated by tumor site and location, sex, race, and stage. CRC frequencies within the VA population were examined descriptively and comparisons were made with national projections of SEER program data.2 Due to the categorical nature of these data, the characteristics of CRC cases were summarized using frequencies and proportions. We used a chi-square and chi-square row mean scores to test for differences in tumor location by gender categorical age, respectively. Incidence rates were age-standardized to the 2010 population of VA enrollees.14 Kaplan Meier survival curves are presented; because patients diagnosed later in the study time period did not have a full five years of observation, we estimated 3-year survival rates and censored those patients without sufficient follow-up time. Statistical analyses were performed using SAS 9.4 (Cary, NC).
RESULTS
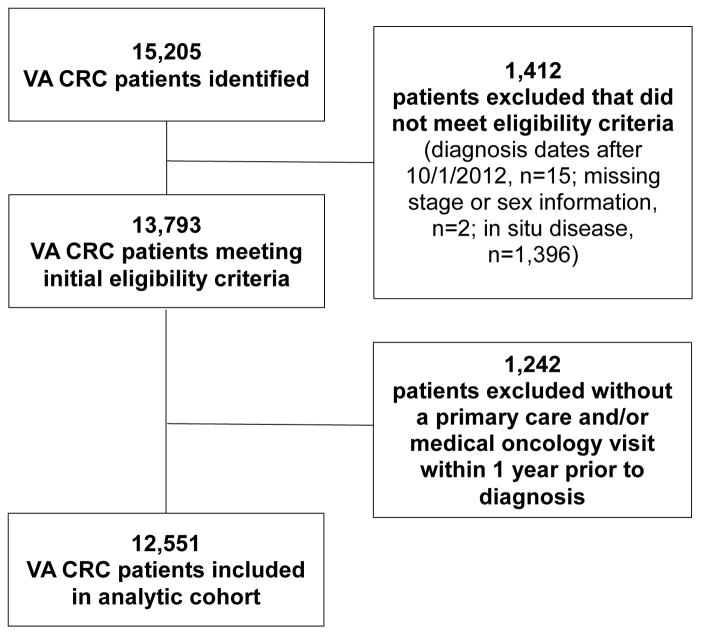
From fiscal year 2009 to 2012, the VACCR collected information for 15,205 VA patients diagnosed with CRC nationwide. After excluding patients not meeting eligibility criteria and/or with missing information on key variables, 12,551 patients remained in our analyses (Figure 1). Notably, the overall CRC incidence rate decreased from 0.22 to 0.16 cases per 1,000 veterans between fiscal years 2009 and 2012.
Figure 1.
Cohort Assembly Diagram
Patient Characteristics
Median age at diagnosis was 65.5 years. Given that 91% of VA patients are males,15 it was not surprising that ~97% (n=12,229) of CRC cases identified in the VACCR were men (Table 1). The racial and ethnic composition of CRC cases in the VACCR was as follows: white (n=9,858, 78.5%), black (n=2,422, 19.3%), other minority (n=169, 1.4%), and unknown race/ethnicity (n=102, 0.8%).
Table 1.
Numbers of New VA Colorectal Cancer Cases and Deaths Among Males by Age, 2009 to 2012.
| Age, Years | New Cases | Deaths within 3 years of diagnosis | ||
|---|---|---|---|---|
| Male Count (%) | Female Count (%) | Male Count (%)* | Female Count (%) | |
| 00–49 | 343 (2.7%) | 39 (0.3%) | 102 (29.7%) | <10 (12.8%) |
| 50–64 | 5200 (41.4%) | 162 (1.3%) | 1703 (32.8%) | 36 (22.2%) |
| 65–79 | 4766 (38.0%) | 73 (0.6%) | 2046 (42.9%) | 25 (34.3%) |
| 80+ | 1920 (15.3%) | 48 (0.4%) | 1317 (68.6%) | 39 (81.3%) |
| All ages | 12,229 (97.4%) | 322 (2.6%) | 5168 (42.3%) | 105 (32.6%) |
Notes: Deaths include all-cause mortality.
Percent is percent of those diagnosed with gender in that age category that died within 3 years of diagnosis.
Tumor Characteristics
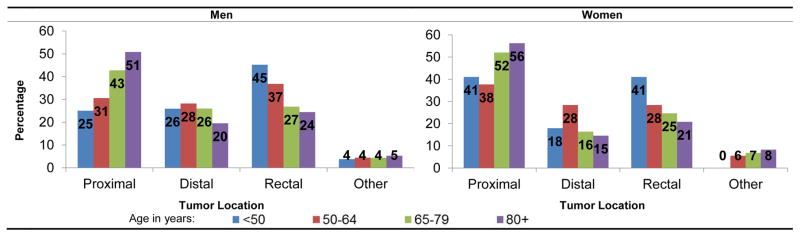
Approximately 68.9% of incident CRC cases were classified as colon cancer. The most common tumor locations (Table 2) were proximal colon (n=4,830, 38%), rectum (n=3,907, 31%), distal colon (n=3,240, 26%), and other colon (n=574, 5%). The distribution of tumor location was similar among men and women (p=0.11), but varied by age group (p<0.01, Figure 2). Regarding stage at diagnosis, ~44% (n=5,517) of patients were diagnosed with localized disease (e.g., local SEER summary stage): ~36% (n=4,488) were diagnosed with regional disease, 17% (n=2,091) with distant disease, and 4% (n=455) had unknown SEER summary stage (Table 3).
Table 2.
Colorectal Cancer Incidence Rates and Proportions by Tumor Subsite, 2009–2012.
| All Persons Rate (%) |
Male Rate (%) |
Female Rate (%) |
|
|---|---|---|---|
| Proximal colon | 0.47 | 0.43 | 0.52 |
| Distal colon | 0.25 | 0.31 | 0.19 |
| Rectum | 0.32 | 0.33 | 0.30 |
| Other | 0.05 | 0.05 | 0.09 |
| Total colorectum | 0.28 | 0.28 | 0.29 |
Notes: Adjustments were made based on information about the underlying VA patient population in 2010. Rates are averages over gender and age categories.
Figure 2.
Distribution of Colorectal Tumor Location by Age and Sex, 2009 to 2012.
Table 3.
Colorectal Cancer Stage Distribution, 2009 to 2012.
| Colorectum N (%) |
Colon N (%) |
Rectum N (%) |
|
|---|---|---|---|
| Localized | 5517 (44.0%) | 3778 (30.1%) | 1739 (13.9%) |
| Regional | 4488 (35.8%) | 3105 (24.7%) | 1383 (11.0%) |
| Distant | 2091 (16.7%) | 1484 (11.8%) | 607 (4.8%) |
| Unknown | 455 (3.6%) | 277 (2.2%) | 178 (1.4%) |
| All stages | 12551 (100%) | 8644 (68.9%) | 3907 (31.1%) |
Notes: Percentages are calculated based on the entire sample.
Three-Year Survival
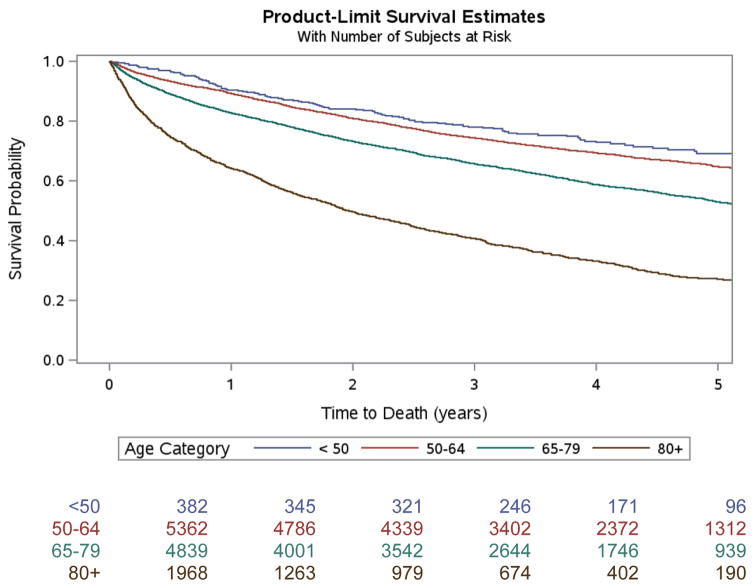
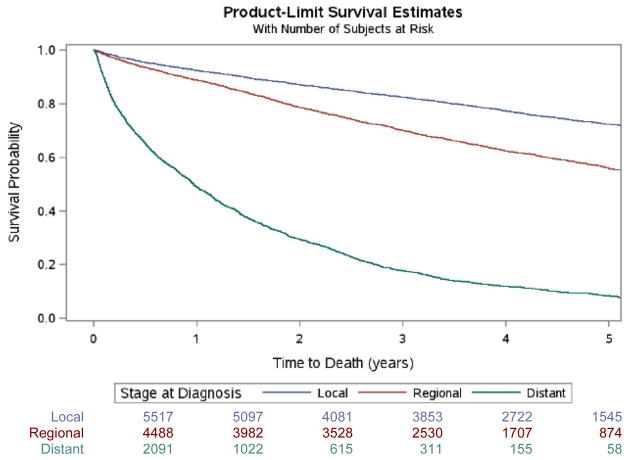
Overall, the estimated percent surviving three years was 65.9%. Three-year survival was associated with age at diagnosis (p<0.01), with patients diagnosed at 50 years or younger having a three-year survival rate of 78% (Figure 3). Among the 4,239 who died within three years of diagnosis, median age at death was 72 years. There was also a significant association between stage at diagnosis and survival (p<0.01; Figure 4). The product-limit estimated three-year survival rates for each stage were as follows: 82.4% for localized stage; 70.0% for regional stage; and 17.8% for distant stage).
Figure 3. Kaplan Meier Survival Curves by Age.
Note: Patients diagnosed later in the study time period did not have a full five years of observation. Thus, this figure depicts 3-year survival data and is censored for those patients without sufficient follow-up time.
Figure 4. Kaplan Meier Survival Curves by Stage.
Note: Patients diagnosed later in the study time period did not have a full five years of observation. Thus, this figure depicts 3-year survival data and is censored for those patients without sufficient follow-up time.
DISCUSSION
Among the nearly 13,000 Veterans who were diagnosed with CRC between 2009 and 2012, approximately 44% had localized disease. The two most common tumor locations were proximal colon and rectum. Their clinical characteristics are similar to CRC cases reported to SEER. Interestingly, despite the differences in the age distribution of the VA versus general US population, the average age of diagnosis was similar among users of the VA and CRC cases reported in SEER (mean of 67.5 years for VA CRC; median of 68 years for SEER).16 One major difference between the two data sources is that 97% of the incident CRC cases in the VACCR were male, reflecting the gender of Veterans receiving VA healthcare. Notably, the demographics are shifting and now women are the fastest growing group of VA healthcare system users.17 These women are, on average, younger than men, which reflects the gender composition of the U.S. military and their era of service.17 Thus, although CRC is common among both men and women2, evaluating gender differences in the VA context is limited.
In this cohort, approximately 19% of Veterans diagnosed with CRC were black. Although this is a much higher proportion than that of VA healthcare system users18, the percentage of minorities in our analytic cohort is consistent with a prior analysis of VACCR data. A previous VACCR analysis reported that, across all cancer types, 19% of newly diagnosed Veterans receiving VA cancer care were black.5 The difference in racial composition between the general VA population and VA cancer population may be due to variation in underlying health status or healthcare utilization. Compared to white patients, minority users of the VA healthcare system report poorer self-reported health and use more clinical services.19–21 Our findings are consistent with previous research showing that there are more minorities are receiving cancer care within the VA than in the nationally.
VA patients may be diagnosed with CRC slightly earlier in the disease trajectory compared to SEER. As previously reported most patients were diagnosed with localized disease in both groups (44% in VA; 39% in SEER).16 Stage at diagnosis was similar for regional disease (35.8% in VA; 36% in SEER) and slightly fewer VA patients were diagnosed with distant disease (16.7% in VA; 20% in SEER).16 This could be a result of many national, robust CRC screening10 and quality improvement programs22 that have been conducted in the VA healthcare system. As an example, the VA has developed a nationwide CRC screening reminder which is integrated into the electronic health record. The goal of the reminder is to proactively identify individuals who are due for CRC screening.10,23 While screening rates vary by organization, national VA CRC screening rates are nearly 80%.24 These national VA screening and quality improvement programs may have led to earlier stage at detection and diagnosis.
Along with earlier diagnoses, we identified a decrease in CRC incidence over time. This slight decrease in incidence has also been noted among cases reported in SEER. The standard reporting delay for cancer registries is two years.25,26 It has been demonstrated that delays in reporting of incident cancer cases beyond a standard window may impact understanding of cancer incidence and trends.25,26 Because VACCR reporting delays are not systematically reported, it is unknown whether the decreasing CRC trend is actually due to fewer CRC diagnoses or a delay in reporting to the VACCR. This is a known limitation of many registries.
With regard to survival, the median age at death was 72 years among incident CRC cases from the VACCR and 73 years among those in SEER.16 Making direct comparisons between VA and SEER survival data is limited because we were only able to calculate 3-year survival for the entire sample rather than 5-year survival for SEER. However, the VA CRC patients had a 65.9% overall 3-year survival rate compared to 64.9% reported in SEER.16 Although data limitations do not permit direct comparisons, these data suggest that survival data are similar among cases reported in VACCR and SEER. We also noted that VA CRC cases are diagnosed at slightly earlier stages than cases reported in SEER. This earlier stage at diagnosis in the VA may also impact survival rates.
Limitations
This analysis had several limitations. First, although our analysis demonstrates that male patients in SEER and the VACCR have similar CRC tumor characteristics, the VA patient population is distinctive—predominately male, often older, with lower socioeconomic status, and higher comorbidity levels when compared to the general U.S. population.5,6,17 Second, we were only able to evaluate 3-year survival data (as opposed to 5-year or longer) due to the relatively recent dates of diagnosis. These mortality data include deaths from all-causes, not necessarily cancer-specific cause of death information. Third, we were unable to obtain data regarding the racial distribution of the underlying VA population, making it difficult to assess racial differences in diagnosis within the VA healthcare system. Similarly, we obtained information regarding enrollees in the VA healthcare system (e.g., for VA population adjustments). However, patients enrolled in the VA healthcare system may or may not be users of the VA healthcare system. This may cause underestimation of incidence. However, we expect that this limitation is minor because all patients included in the analysis had sufficient CRC care within the VA healthcare system to warrant their inclusion in the VACCR (e.g., meaning that they were either diagnosed or received all or part of their treatment within the VA).
CONCLUSIONS
Accounting for differences in the underlying patient populations, VA CRC statistics are comparable to those reported and/or projected in SEER. This suggests that research findings resulting from the VACCR might have applicability beyond the VA healthcare system setting. Evaluating VA CRC statistics on a regular basis is important to inform our understanding of whether VA CRC screening initiatives and quality improvement programs are having an impact on earlier CRC detection at a population level. Additionally, this information can inform clinical CRC resource planning.
CLINICAL PRACTICE POINTS.
Colorectal cancer (CRC) is the third most commonly diagnosed cancer and third leading cause of cancer-related death among both men and women.
CRC characteristics among men, particularly stage and tumor location, are similar between patients in the VA Central Cancer Registry and the general U.S. population.
These data suggest that CRC-related findings in the VA healthcare system may have broader applicability.
Acknowledgments
Dr. Zullig is support by a Veterans Affairs Health Services Research & Development Career Development Award (CDA 13-025). Drs. Bosworth (RCS 08-027) and Weinberger (RCS 91-408) are supported by Senior Research Career Scientist awards from VA Health Services Research & Development. The views expressed in this article are those of the author(s) and do not necessarily represent the views of the Department of Veterans Affairs. We thank the VA cancer registrars for their data collection and related efforts.
ABBREVIATIONS
- CDW
Corporate Data Warehouse
- CRC
Colorectal cancer
- NCI
National Cancer Institute
- SEER
Surveillance, Epidemiology, and End Results
- US
United States
- VA
Veterans Affairs
- VACCR
Veterans Affairs Central Cancer Registry
- VINCI
VA Informatics and Computing Infrastructure
Footnotes
CONFLICTS OF INTEREST
The authors report no conflicts of interest in this work. Dr. Zullig is support by a Veterans Affairs Health Services Research & Development Career Development Award (CDA 13-025). Drs. Bosworth (RCS 08-027) and Weinberger (RCS 91-408) are supported by Senior Research Career Scientist awards from VA Health Services Research & Development. This content is solely the responsibility of the authors and does not reflect the position or policy of the U.S. Department of Veterans Affairs of the United States Government.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA: a cancer journal for clinicians. 2015;65(1):5–29. doi: 10.3322/caac.21254. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA: a cancer journal for clinicians. 2014;64(2):104–117. doi: 10.3322/caac.21220. [DOI] [PubMed] [Google Scholar]
- 3.Howlader N, Ries LA, Stinchcomb DG, Edwards BK. The impact of underreported Veterans Affairs data on national cancer statistics: analysis using population-based SEER registries. Journal of the National Cancer Institute. 2009;101(7):533–536. doi: 10.1093/jnci/djn517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. [Accessed December 20, 2015];Department of Veterans Affairs Veteras Health Administration Directive 1072: Release of VA Data to State Cancer Registries. 2014 Available from: http://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3028.
- 5.Zullig LL, Jackson GL, Dorn RA, et al. Cancer incidence among patients of the U.S. Veterans Affairs Health Care System. Military medicine. 2012;177(6):693–701. doi: 10.7205/milmed-d-11-00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha Z, Lofgren RP, VanRuiswyk JV, Layde PM. Are patients at Veterans Affairs medical centers sicker? A comparative analysis of health status and medical resource use. Archives of internal medicine. 2000;160(21):3252–3257. doi: 10.1001/archinte.160.21.3252. [DOI] [PubMed] [Google Scholar]
- 7.Brown DW. Smoking prevalence among US veterans. Journal of general internal medicine. 2010;25(2):147–149. doi: 10.1007/s11606-009-1160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park SY, Zhu K, Potter JF, Kolonel LN. Health-related characteristics and dietary intakes of male veterans and non-veterans in the Multiethnic Cohort Study (United States) Journal of military and veterans’ health. 2011;19(2):4–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Almond N, Kahwati L, Kinsinger L, Porterfield D. Prevalence of overweight and obesity among U.S. military veterans. Military medicine. 2008;173(6):544–549. doi: 10.7205/milmed.173.6.544. [DOI] [PubMed] [Google Scholar]
- 10.Chao HH, Schwartz AR, Hersh J, et al. Improving colorectal cancer screening and care in the Veterans Affairs Healthcare system. Clinical colorectal cancer. 2009;8(1):22–28. doi: 10.3816/CCC.2009.n.004. [DOI] [PubMed] [Google Scholar]
- 11.Jackson GL, Melton LD, Abbott DH, et al. Quality of nonmetastatic colorectal cancer care in the Department of Veterans Affairs. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2010;28(19):3176–3181. doi: 10.1200/JCO.2009.26.7948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Medical Association. AMA Physician ICD-9-CM, Volumes 1 And 2: International Classification of Diseases, 9th Revision Clinical Modification. American Medical Association Press; 2005. [PubMed] [Google Scholar]
- 13.Ries LAG, Fritz AG, Hurlbut A. SEER summary staging manual-2000: codes and coding instructions. National Cancer Institute, SEER Program, NIH Pub; 2007. pp. 62–84. [Google Scholar]
- 14.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected US population. 2001:1–10. [PubMed] [Google Scholar]
- 15.Department of Veterans Affairs Statistics At A Glance. National Center for Veterans Analysis and Statistics; 2015. [Accessed November 12, 2015]. Available from: http://www.va.gov/vetdata/docs/quickfacts/stats_at_a_glance_08_27_15.pdf. [Google Scholar]
- 16.NCI Surveillance, Epidemiology, and End Results Program. [Accessed November 23, 2015];SEER Stat Fact Sheets: Colon and Rectum Cancer. Available from: http://seer.cancer.gov/statfacts/html/colorect.html.
- 17.Frayne S, Phibbs C, Saechao F, et al. Sociodemographics, Utilization, Costs of Care, and Health Profile. Vol. 3. Women’s Health Services, Veterans Health Administration, Department of Veterans Affairs; 2014. Sourcebook: Women Veterans in the Veterans Health Administration. [Google Scholar]
- 18.Department of Veterans Affairs Unique Veteran Users Report FY 2014. National Center for Veterans Analysis and Statistics; 2016. [Accessed March 28, 2016]. Available from: http://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Unique_Veteran_Users_2014.pdf. [Google Scholar]
- 19.Liu CF, Chapko M, Bryson CL, et al. Use of outpatient care in Veterans Health Administration and Medicare among veterans receiving primary care in community-based and hospital outpatient clinics. Health services research. 2010;45(5 Pt 1):1268–1286. doi: 10.1111/j.1475-6773.2010.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheehan CM, Hummer RA, Moore BL, Huyser KR, Butler JS. Duty, Honor, Country, Disparity: Race/Ethnic Differences in Health and Disability among Male Veterans. Population research and policy review. 2015;34(6):785–804. doi: 10.1007/s11113-015-9358-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Washington DL, Harada ND, Villa VM, et al. Racial variations in Department of Veterans Affairs ambulatory care use and unmet health care needs. Military medicine. 2002;167(3):235–241. [PubMed] [Google Scholar]
- 22.Jackson GL, Powell AA, Ordin DL, et al. Developing and sustaining quality improvement partnerships in the VA: the Colorectal Cancer Care Collaborative. Journal of general internal medicine. 2010;25(Suppl 1):38–43. doi: 10.1007/s11606-009-1155-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarfaty M, Wender R. How to increase colorectal cancer screening rates in practice. CA: a cancer journal for clinicians. 2007;57(6):354–366. doi: 10.3322/CA.57.6.354. [DOI] [PubMed] [Google Scholar]
- 24.Chou AF, Rose DE, Farmer M, Canelo I, Yano EM. Organizational Factors Affecting the Likelihood of Cancer Screening Among VA Patients. Medical care. 2015;53(12):1040–1049. doi: 10.1097/MLR.0000000000000449. [DOI] [PubMed] [Google Scholar]
- 25.Clegg LX, Feuer EJ, Midthune DN, Fay MP, Hankey BF. Impact of reporting delay and reporting error on cancer incidence rates and trends. Journal of the National Cancer Institute. 2002;94(20):1537–1545. doi: 10.1093/jnci/94.20.1537. [DOI] [PubMed] [Google Scholar]
- 26.Huang L, Midthune D, Krapcho M, Zou Z, Horner MJ, Feuer EJ. Adjusting for reporting delay in cancer incidence when combining different sets of cancer registries. Biometrical journal Biometrische Zeitschrift. 2013;55(5):755–770. doi: 10.1002/bimj.201100191. [DOI] [PubMed] [Google Scholar]