Abstract
Objectives
Understand future home-based care needs/costs for disabled elders in China.
Method
Further develop/apply ProFamy extended cohort-component method.
Results
(1) Chinese disabled elders and percentage of national GDP devoted to home-based care costs for disabled elders will increase much quicker than growth of total elderly population; (2) Home-based care needs/costs for disabled oldest-old aged 80+ will increase much faster than that for disabled young-old aged 65–79 after 2030; (3) Disabled unmarried elders living alone and their home-based care costs increase substantially faster than disabled unmarried elders living with children; (4) Sensitivity analyses shown that possible changes in mortality and elderly disability status are the major factors affecting home-based care needs and costs; (5) Caregivers resources under two-child policy will be substantially better than under current fertility policy unchanged.
Discussion
Policy recommendations concerning reductions of prevalence of disability, gender equality, two-child policy, encouraging elder’s residential proximity to their adult children, etc.
Keywords: Household Projection, Elderly Living Arrangements, Disability, Population Aging, Home-based Care Costs
1. INTRODUCTION
With a continuing increase in life expectancy and decline of fertility rates, population and household aging has become a serious challenge in China. Projections under the medium fertility and mortality assumptions by the United Nations and other scholars inside and outside China confirm the likelihood of an extremely rapid increase in the number and proportion of older adults in China in the first half of the 21st century. Under the medium or low mortality assumptions, the total number of elderly aged 65+ in China is estimated to increase dramatically from 111 million in 2010 (8.2% of the total population) to 337 to 400 million in 2050 (23.9% to 26.9% of the total population); the number of oldest-old aged 80+ who most likely need daily life assistance were 19.3 million in 2010, but it will climb extraordinarily to about 107 to 150 million in 2050 (Zeng and George, 2010). Population aging will affect the old-age dependency ratio in China, which will climb from 0.11 to 0.24 and 0.42 in 2030 and 2050, respectively, 2.18 and 3.80 times the value in 2010 (U.N., 2011). Rapid population aging may bring about a heavy burden to the families of the elderly and the whole society, and may erode the foundation of needs and costs of home-based care, which has supported older adults for a few thousand years in China. For consistency of analysis of this subject, throughout this article the concept of “home-based care needs” refers to age-gender-marital status-rural/urban-living arrangement-specific distributions of disabled elders, and the concept of “home-based care costs” refers to the costs of home medical, home nursing or household paid-services and informal care (opportunity costs without cash payment) provided by family members or friends.
Rapid population aging in China will result in a declining labor supply and an increasingly higher proportion of GDP transferred into the long-term care for the elderly, which would negatively affect development at the macroeconomic level. At the microeconomic level, given that the current social endowment system for older adults in China is imperfect, population aging may lead to an increasingly heavy burden on home-based caregivers resulting in increased precautionary saving and reduced consumption (Li and Chen, 2006).
Older adults aged 65+ in China today have about 5–6 surviving children on average; Chinese baby boomers, who were born during 1950s and 1960s and will become elders after 2015, have fewer than 2 adult children on average due to a strict birth control policy and substantial changes in fertility attitudes along with rapid socioeconomic development (Zeng 2007). This greatly decreased availability of children plus an increased geographic/residential mobility of working age people associated with economic development will produce a rapid increase in empty-nest (without children living together) elderly households; many Chinese elders will face the problems of lack of daily caregiving, which may deteriorate the foundation of home-based care for the elderly population and aggravate the economic burden and opportunity costs to adult children.
A number of prior quantitative studies have projected home-based care needs and costs for disabled elderly in developed countries other than China (e.g., CMMS, 2004), but most prior studies in China were qualitative (e.g. Hu et al, 2003; Li, 1998; Jiang, 2008). Generally speaking, three types of care costs for older adults are described in quantitative studies: 1) home-based care, measured in cash expenditures; 2) non-cash home-based care time (opportunity costs) delivered by family members; and 3) inpatient and outpatient care, measured in cash expenditures. It is widely accepted that care needs and costs are closely related to the health status of older adults. Health survey data based on activities for daily living (ADL), including bathing, dressing, eating, indoor transferring, toileting, and continence, are available and have proven in many studies to be a significant predictor of health status, care needs and costs, and mortality among older adults. As a result, many scholars use ADL status to measure health care needs for older adults (e.g., Liang, 1999).
Projections of ADL status among older adults in developed countries have been relatively popular in recent decades and generally follow two methodologies. The simple proportional distribution projection method multiplies the age-sex-specific proportions of ADL statuses of older adults at baseline by projected age-sex-specific numbers of older adults in future years (Suthers et al, 2003). The multi-state transitions projection method estimates the age-sex-specific transition probabilities matrices of ADL statuses of older adults based on survey data and combines them with matrices of status-specific population forecasts (e.g., Lakdawalla, 2003). In general, most demographers calculate projections of elderly home-based care needs and costs by multiplying the ADL status-specific costs per person at baseline by the projected ADL status-specific population distribution in future years (Mayhew, 2000). A few scholars have projected care expenditures separately for surviving elders and for the deceased elderly in the last month or so before death (Serup-Hansen et al, 2002).
A series of studies indicated that the home-based care needs and costs are closely correlated with the age, gender, marital status, and family structure of older adults. For example, disabled elders who are unmarried or living alone have much higher care needs for paid services in the home than those who live with children and/or a spouse (Grundy, 2001). Older adults who co-reside with children tend to receive more informal, non-cash home-based care than those with an empty nest (Zhang, 2004). However, almost all previous projections of home-based care needs and costs did not consider simultaneously the different ADL statuses dynamic transitions, family structures, and living arrangements of older adults. The present study overcomes this limitation by introducing multistate projections of ADL status transition dynamics for older adults into the ProFamy extended cohort-component method for family household and living arrangement projection (Zeng, Vaupel and Wang, 1998; Zeng et al, 2006; 2013). The theoretical framework, method, and computer programs of the ProFamy multistate model are substantially extended in this article to project simultaneously the family structure, ADL status transitions, and home-based care needs and costs for the elderly population.
2. METHODS, DATA AND PROJECTION SCENARIOS
2.1. Methods
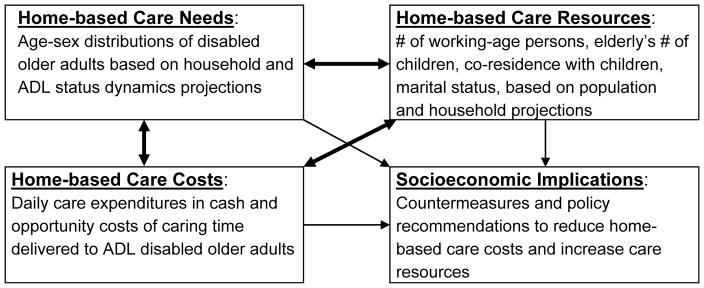
Figure 1 presents the theoretical and demographic framework of this study, highlighting interactions among home-based care needs, resources, and costs, as well as their socioeconomic implications. Based on this framework, we extend the ProFamy extended cohort-component method into a model for projecting home-based care needs and costs for older adults.
Figure 1.
Basic theoretical and demographic framework of this study
As noted above, almost all of the previously published projection models for the elderly disabled population and home-based care needs and costs ignored the family household structure and living arrangements of older adults; this was due to lack of reliable methods using available demographic data to project households and living arrangements. Currently, the classic headship-rate method is the most commonly used approach for household projections although it has been criticized widely by demographers for more than two decades (Mason and Racelis 1992; Spicer et al. 1992; Murphy 1991; Grundy 2013). The headship-rate method is limited because it is based on the vague and ill-defined concept of household heads (Murphy 1991; Mason and Racelis 1992), has no connection to demographic rates due to the nature of its cross-sectional extrapolations (Spicer et al. 1992), and lumps all household members other than heads into one category “non-head” with no projected information. This last limitation makes it impossible to study the household status and living arrangements of the elderly, adults, and children who are not heads of households (Burch 1999). Consequently, the headship-rate method is not appropriate for projections of home-based care needs and costs for disabled elderly, which are directly linked to all older adults in the population and their family household structure and living arrangements.
In contrast to the classic headship-rate method, the extended cohort-component model for projecting household types, sizes and living arrangements, known as ProFamy, projects all individuals in households (including older adults) grouped by cohorts and specified attributes (e.g., sex, age, rural/urban, marital/union status, co-residence status with children and parents), using demographic rates as input. The ProFamy model was initially developed in Zeng, Vaupel and Wang (1998) based on the pioneering innovation of the family status life table model by Bongaarts (1987), and further extended/justified in Zeng, Land, Wang and Gu (2006; 2013). The ProFamy method has been employed in various studies, for example, in Prskawetz et al. (2004), Smith et al. (2008), Dalton et al. (2008), Smith et al. (2012) and Feng et al. (2011).
Empirical tests of ProFamy projections from 1990 to 2000 using observed U.S. and Chinese demographic rates before 1991 show that forecast errors, measured by discrepancies between the projected values and census observations in 2000, are reasonably small at the national level (Zeng et al., 2006; Zeng et al., 2008). Test comparisons of projections of household and living arrangements from 1990 to 2000 using the ProFamy method with census counts in 2000 for each of the 50 U.S. states and DC showed that 68.0, 17.0, 11.2, and 3.8 percent of the absolute percent errors are <3.0%, 3.0–4.99%, 5.0–9.99% and 10.0%, respectively (Zeng et al., 2013). Similar results have been found in comparisons of ProFamy projections from 2000 to 2010 and 2010 census-observed Chinese households and population by regions of Eastern, Middle and Western regions, Beijing and Hebei province, etc. (Zeng, Shen and Wang 2013). The various tests have confirmed that the ProFamy model for household and living arrangement projections is valid at both national and sub-national levels.
These prior studies have dealt solely with projections of household and living arrangements. By comparison, the analyses presented here project dynamic changes in disability status of older adults measured by ADLs (disability status may also be measured by other indicators) and their home-based care costs, classified by age, gender, rural/urban residence, marital status, and living arrangements. The key point of this analysis is to introduce and estimate changes in older adults’ disability status and the associated home-based care costs. In this analysis, disability statuses, marital statuses (i.e., unmarried, married, widowed, and divorced), number of co-residing children and co-residing parents, and living in private or institutional household are identified in the projection model.
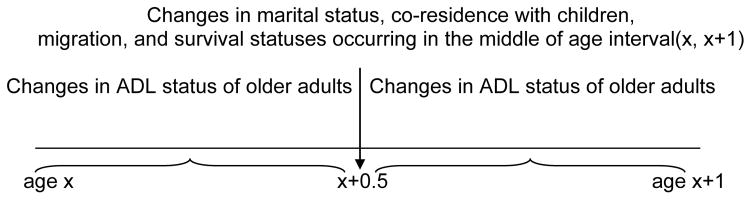
In these analyses, we distinguish 4 marital statuses (never-married, currently married, divorced and widowed), 2 ADL statuses (active and disabled), 6 parity statuses and 6 statuses of number of co-residing children (0, 1, 2, 3, 4, 5+), and 3 statuses of number of co-residing parents (0, 1, 2). If a conventional multistate computation strategy were adopted, we would accordingly have to estimate a cross-status transition probabilities matrix with 254,016 (=504×504; where , where the number of co-residing children is equal or less than parity p) elements for each sex at each age of the elderly population. This is certainly not practical, as it would be impossible to have a sufficiently large dataset with appropriate sizes of the sub-samples to reliably estimate so many elements of the cross-status transition probabilities matrix at each age and sex, although there are considerable numbers of structural zero elements such as transitions to lower parity. Thus, we circumvent this impossible data requirement by applying a computational strategy of calculating individual older adult groups’ changes of marital status, ADL status, co-residence (with parents/children), migration, and survival status, following continuously occurring periodic demographic accounting processes based on commonly available data. More specifically: (a) we calculate ADL status transitions throughout the first and second half of the single-year age intervals, and (b) we calculate marital/union status changes, children’s leaving parental home, migration, and deaths in the middle of the age intervals (see Figure 2). This computational strategy was originally proposed by Bongaarts (1987), further justified mathematically and numerically by Zeng (1991: 61–63 & 80–84), and adopted in the ProFamy extended cohort-component model for household and living arrangement projections (Zeng et al., 2006; Zeng et al. 2013). As stated above, the empirical tests of ProFamy projections from 1990 to 2000 (or from 2000 to 2010) show that forecast errors, measured by discrepancies between the projected values and census observations in 2000 (or 2010), are reasonably small at both the national and sub-national levels for each of the 50 states and DC in the U.S. and for each of the regions and provinces in China (Zeng et al., 2006; Zeng et al., 2008; Zeng et al. 2013; Zeng, Shen and Wang 2013). These empirical tests further verified the innovative computational strategy adopted here and depicted in Figure 2.
Figure 2.
Computational strategy to calculate changes in demographic, familial and ADL statuses of older adults by single year of age
In addition, the present analyses combine the projection of family structure, living arrangement, and ADL status for elders aged 65+ (depicted in Figure 2 of this article) with the projection of family structures and living arrangements of the younger population aged 0–64, including fertility, mortality, changes in marital status and co-residing status with children and parents, and migration (see Figure 2 in Zeng et al., 2013), in order to form a comprehensive dynamic projection model for all of the individuals in the population. That is, the extended model in the present article projects not only ADL statuses and home-based care needs and costs for older adults, but also numbers and age-sex-family household structures of the working-age population, i.e., the caregivers for the disabled elderly.
A basic projection module for institutional household arrangements for older adults is also included in the extended projection model. But the projection of institutional-based care costs for the elderly was not included in the present application to China because the sub-sample size for the institutionalized elderly in the Chinese survey was too small to estimate meaningful ADL status transition rates and care costs. Furthermore, projections for institutionalized elders and their costs are a complicated sub-field related to many other factors such as economic income, social facilities, and Chinese cultural attitude, which are out of the scope of the present study. Thus, we focus on home-based care needs/costs projections and analysis. Specifically, the present study focuses on the projection and analysis of how changes in households and living arrangements may affect home-based care expenditures in cash and care workdays devoted to caring for the disabled elders; inpatient or outpatient medical care expenditures are not included, as the needed nationwide data are not available for China and they are outside the scope of this paper.
2.2. Data sources and estimates
Population counts for China classified by rural/urban residence, single year of age, sex, marital status, number of co-residing children and parents, and whether living in private household or institution at the baseline of projection were extracted from the micro-data file of the 2000 census (the micro-data of the 2010 census are still not available for scholars and the public to use so far), and updated by the published rural/urban-single-year-age-sex-specific data from the 2010 census. Based on the micro-data file of the 2000 census and 2005 mini-census for one percent of the population, we estimated the distributions of rural/urban-single age-sex-specific occurrence/exposure (o/e) rates of first marriage and fertility by parity, and age-sex-specific net migration rates between rural and urban areas. The model standard schedules of age-sex-specific o/e rates of divorce and remarriages were estimated by the Chinese In-depth Fertility Survey data. We also estimated the rural/urban-specific general marriage rate and divorce rate based on age-sex-specific standard model schedules of marriage and divorce rates, 2000 census micro data, and published total numbers of marriage and divorce in 2000–2010 (see Zeng et al., 2008 for more details).
Estimates of transition probabilities for ADL statuses among older adults and average home-based care costs for ADL-disabled elders, which are the input of our projections, are based on the Chinese Longitudinal Healthy Longevity Survey (CLHLS). The CLHLS were conducted in a randomly selected half of the counties and cities of 22 provinces (out of a total of 31 provinces) in China since 1998, covering 85% of the total population. The CLHLS is a national representative survey on determinants of healthy longevity, which over-sampled the oldest-old aged 80+ especially males, plus comparative samples of the young-old aged 65–79. The target was to interview more or less equal numbers of males and females at each of the age groups of 65–79, 80–89 and 90–99. The CLHLS does not follow the proportionally sampling framework in order to avoid too small sub-sample size for the oldest-old especially males. Consequently, appropriate weights based on the census and the CLHLS data were used to calculate the average ADL status transition probabilities of the age groups in this study.
We used the older adult samples from the 2002 and 2005 CLHLS waves, which contain 15,983 and 16,566 elderly respondents aged 65+, respectively, as well as their follow-up ADL status and survival/death data collected in 2005 and 2008 waves, respectively. The data collected through in-home face-to-face interviews contain basic individual and household demographic characteristics, ADL status, socioeconomic background, health, psychological characteristics, cognitive function, lifestyle, eating habits, economic resources, daily caregiving, etc. Extensive evaluations of data quality, including assessments of non-response rate, sample attrition, proxy use, reliability and validity of major health measures, mortality rates and the proportions of logically inconsistent answers have produced generally satisfactory results, compared to other major aging studies (Gu, 2008; Shen, 2010, Chen, 2010). The CLHLS data have been widely used by demographers inside and outside of China and its reasonably good quality is widely recognized (e.g., Goodkind, 2009).
Activities of daily living (ADL) are measured by six separate questions on bathing, dressing, eating, indoor transferring, toileting, and continence; we classify a respondent as ADL disabled if he/she needs help in any one of the above six ADL items, following international standards. Because of too small sub-sample size for some sub-groups, it is unreliable to estimate age-sex-attribute-specific ADL status transition probabilities using the directly-computing approach. Instead, we applied a “two-step” approach which was successfully employed in the literature such as Land et al (1994) and Scafato et al (2008). More specifically, we first directly calculated baseline age-sex-specific ADL status transition probabilities with all of the other attributes combined. Second, we then estimated the age-sex-attribute-specific ADL status transition probabilities by multiplying the baseline age-sex-specific ADL status transition probabilities by the multivariate regression estimates of the corresponding odds ratios of ADL status transition probabilities with different attributes, as compared to the baseline. The reason why we adopted this two-step approach rather than a “one-step” approach of applying multivariate regression models to directly estimate the age-sex-attributes-specific ADL status transition is because the estimate of the age covariate coefficients in the one-step regression model produced results which are out of an empirically plausible range for some age groups. Even after correcting the logic errors by introducing some constraints to the regression, the estimates are still unreasonable.
If a CLHLS respondent reported needing help with an ADL, two further questions were asked: t “How much is the total direct cost in cash paid for caregiving last week?” and “How many hours (not-paid) in total did your spouse, children, grandchildren and their spouses, or others help you last week?”. Note that the reference period of the last week for care expenditures and time is intended to reduce recall errors of relatively long periods of time, which is a widely adopted international practice in the elderly population heath surveys. For respondents who were interviewed in a previous wave of the survey and died before the follow-up wave, one of his/her family members was interviewed to estimate home-based care expenditures in the last month before death. Home-based care and associated costs included nursing, door-to-door services, and items or goods for care provided in the home, but not inpatient and outpatient medical care and expenditures. We used the 2008 CLHLS data and multiple regression to estimate the average home-based care expenditures in cash (yuan) for ADL disabled survivors (per year) and decedents (in the last month before death), as well as the non-cash home-based care workdays (opportunity costs) delivered by family members for ADL disabled survivors per year.
To reflect the overall relative burdens in future years, we also projected the proportion of home-based elderly care cash costs among the national GDP, forecasted by the World Bank and the Development Research Center of State Council of China (2013).
2.3. Projection scenarios and parameters
Uncertainties in mortality rates, ADL status changes, and home-based care costs per disabled person should be considered in the design of the projection scenarios. The medium mortality scenario, which is widely used in population forecasts of China by scholars and agencies, assumes a life expectancy of about 79 years for both sexes combined in 2050. This is rather conservative, given that the average life expectancy in Shanghai in 2011 was already 82.5 years old (Health Bureau of Shanghai, 2012), 3.5 years higher than the projection for China in 2050. Some recent research indicates that there may be a significant improvement in mortality in the first half of this century because of biomedical breakthroughs and better personal health practices, such as healthy diets, smoking cessation, and exercise (see, e.g., Shekell, 2005). Therefore, we modelled another more optimistic low mortality scenario, namely, life expectancy for both sexes combined was assumed to approach 84.8 years in 2050, which is only 2.3 years higher than that in Shanghai in 2011. This optimistic mortality scenario is subject to uncertainty, but we believe that it is not impossible. The Chinese life expectancy at birth was 71.4 in 2000 and 73 years old in 2005. If the same annual rate of increase as in 2000–2005 were assumed in the future, the life expectancy at birth in China would be 87.4 years in 2050, which may not be feasible, as the rapid socioeconomic development accompanied with substantial reduction in mortality in 2000–2005 may not be sustained through the decades to come. Therefore, we assume a life expectancy at birth of 84.8 years in 2050 and 88 years in 2080 in China in the low mortality scenario, and we believe that such assumption involves a lot of uncertainty but may not be impossible. Despite the uncertainty, the medium and low mortality scenarios (see Table 1) bracket an informative range of possible average life expectancy at birth in China in the next decades.
Table 1.
Main demographic parameters used in the projections
| Rural | Urban | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Year | 2010 | 2015 | 2030 | 2035 | 2050 | 2010 | 2015 | 2030 | 2035 | 2050 |
| TFR-2-child policy | 2.01 | 2.09 | 2.09 | 2.27 | 2.27 | 1.24 | 1.67 | 1.67 | 1.80 | 1.80 |
| TFR-current fertility policy unchanged | 2.01 | 1.98 | 1.98 | 1.98 | 1.98 | 1.24 | 1.20 | 1.20 | 1.20 | 1.20 |
| Life expectancy at birth | ||||||||||
| Male: medium mortality | 69.38 | 70.03 | 72.20 | 72.90 | 75.00 | 73.24 | 73.91 | 75.90 | 76.60 | 78.60 |
| Male: low mortality | 69.38 | 70.69 | 74.84 | 75.98 | 79.40 | 73.24 | 75.16 | 80.91 | 87.84 | 81.9 |
| Female: medium mortality | 73.35 | 74.06 | 76.20 | 76.80 | 78.90 | 77.18 | 77.86 | 79.90 | 80.60 | 82.50 |
| Female: low mortality | 73.35 | 75.05 | 80.16 | 81.52 | 85.6 | 77.18 | 78.85 | 83.86 | 85.17 | 89.10 |
| General marriage rate | 0.0674 | 0.0674 | 0.0674 | 0.0674 | 0.0674 | 0.0601 | 0.0601 | 0.0601 | 0.0601 | 0.0601 |
| General divorce rate | 0.0022 | 0.0022 | 0.0022 | 0.0022 | 0.0022 | 0.0056 | 0.0056 | 0.0056 | 0.0056 | 0.0056 |
| Average age at birth | 25.20 | 25.20 | 26.50 | 26.50 | 26.50 | 26.00 | 26.00 | 27.30 | 27.30 | 27.30 |
| Urban population % | 49.7 | 52.3 | 60 | 64 | 75 | |||||
Demographers and health researchers have posited three different hypotheses about the future trends of disability in relation to increasing lifespan. The compression of morbidity theory assumes that morbidity will decline and become compressed into a shorter duration of disability before death with improvements in healthy life styles and increases in life expectancy (Fries, 1980). Conversely, the second theory argues that morbidity and disability will generally expand with the decline of mortality because it enhances the survival probabilities of unhealthy elderly groups (Olshansky et al., 1991). Manton (1982) proposed the “dynamic equilibrium model”, which is in the middle between the optimistic and pessimistic hypotheses. It is, however, not clear which theory is more applicable to changes of morbidity and disability among older adults in China. Gu and Zeng (2006) estimated that the prevalence of ADL disability among older adults in China had been declining 0.98% every year. On the other hand, Du and Wu (2006) declared that the proportion of disabled elderly population increased by 1% every year. Huang (2006) argued that it is most likely that the age-specific disability of the elderly remains unchanged across future years in China.
Based on this body of prior research, we designed the following four projection scenarios (low, medium, high(a), and high(b)) for combinations of mortality decline and ADL status changes among the Chinese elderly.
The low scenario assumes that there will be slow increases in life expectancy (medium morality) with a generally greater improvement in the prevalence of ADL disability among the elderly population (i.e., assuming compression of morbidity). Specifically, this scenario assumes that the age-sex-rural/urban residence-marital status-coresidence with children-specific probabilities of ADL status transition from “active” into “disabled” will decline by 1% annually in the projection period after 2010, while transitions from “disabled” into “active” will increase by 1% annually in the projection period after 2010.
The medium scenario assumes that there will be slow increases in life expectancy (medium morality) and the general health of the elderly population will remain stable (i.e., assuming dynamic equilibrium model). This scenario assumes that the age-sex-rural/urban residence-marital status-coresidence with children-specific ADL status transition probabilities remain unchanged.
The high(a) scenario assumes that there will be more rapid increases in life expectancy (low morality) and the general health of the elderly population will remain stable (dynamic equilibrium). This scenario specifies that the age-sex-rural/urban residence-marital status-coresidence with children-specific ADL status transition probabilities remain unchanged.
The high(b) scenario assumes that there will be more rapid increases in life expectancy (low morality) and the general health of the elderly population will deteriorate in the future (i.e., assuming expansion of morbidity). More specifically, the age-sex-rural/urban residence-marital status-coresidence with children-specific ADL status transition probabilities from “active” into “disabled” will increase by 1% annually, while the transition probabilities from “disabled” into “active” will decrease by 1% annually in the projection period after 2010.
We projected future home-based care costs for disabled older adults in cash in two different ways: (1) projecting the annual growth rate of the home-based care costs in cash based on time series data analysis and trend extrapolation; and (2) assuming that the annual growth rate of home-based care costs for the elderly would be the same as that for GDP during 2010–2050. We assume that in all of the scenarios, the average number of non-cash home-based care workdays provided by family members per disabled elder per year remains the same as that in the baseline 2010.
To analyze the impacts of different fertility policies on the elderly care providers’ resources, we designed the following two fertility level/policy scenarios:
A universal two-child with encouraging adequate spacing policy scenario, which assumes a smooth transition period to around 2015 when an average couple in urban and rural areas would have 1.8 and 2.27 children in their lifetime, respectively. We assume that the average age at first and second or higher order births will increase by 0.75 and 1.5 years in 2030 as compared to 2015, which constitutes an annual growth rate of about 0.05 and 0.1 years, respectively, during the years 2015–2030, due to delays of marriages and births under rapid socioeconomic development and the encouragement of governmental policies. This assumption is reasonable (or may be conservative), based on recent fertility timing data. As a result, the period TFRs of the first and second or higher order births would be 5% and 10% lower than the parity-specific lifetime cohort TFRs, respectively, based on the widely recognized Bongaarts and Feeney equations for translating changes in fertility timing into period TFRs (Bongaarts and Feeney, 1998). This would lead to the period TFRs in rural and urban areas being 2.09 and 1.67 during the period 2015–2030 (see Table 1).
The current fertility policy remains unchanged scenario, which assumes that the TFRs in rural and urban areas slightly grow to 1.98 and 1.20 in 2015, which is due to an increase in only-child couples who are allowed to have two children; and the TFRs after 2015 would remain unchanged (see Table 1).
3. RESULTS
We present in this section the results of our estimates, projections and analysis, with some explanations concerning the specific points. Discussions of the policy-related results will be presented in the next section.
3.1. Age-specific trajectories of ADL statuses transitions and home-based care costs
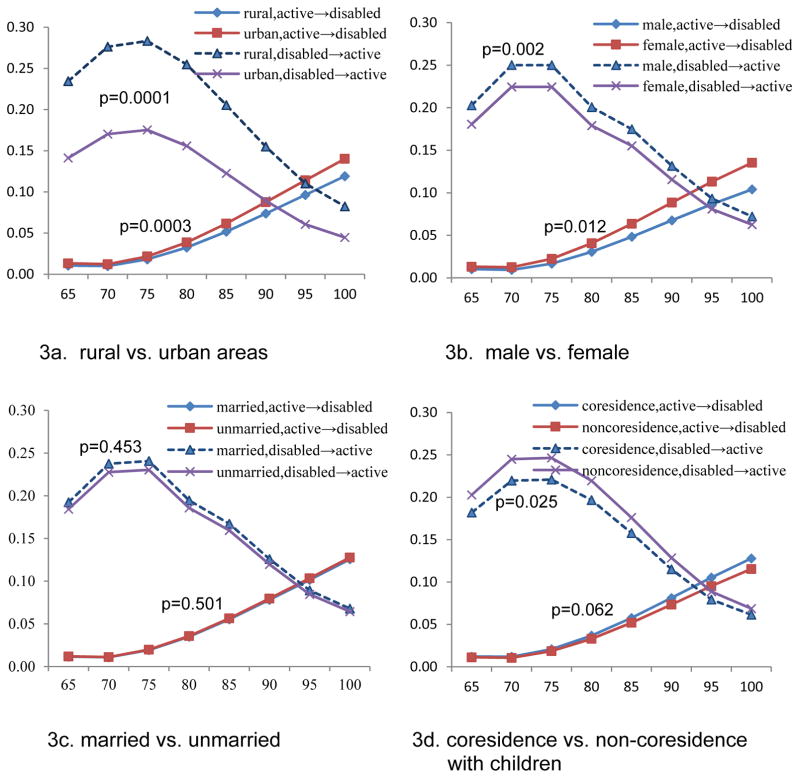
Figures 3a, 3b, 3c and 3d show comparisons of age-specific transition probabilities between ADL statuses for older adults in different groups classified by rural/urban residence, gender, marital status, and co-residence with children, which are inputs for our projections. The age-specific transition probabilities from “active” to “disabled” are relatively low for those elders aged 65–74, and grow quickly after age 75. Differences in transition probabilities from “active” to “disabled” between different groups of rural/urban residence, gender, and co-residence status with children are rather small before age 80, but become larger after age 80. The curves of ADL status transition probabilities from “disabled” to “active” in have an inverted J-type shape which reaches a peak at age 70–74 and then declines sharply with increase in ages.
Figure 3. Transition probabilities between ADL statuses for older adults, by rural/urban residence, gender, marital status, and coresidence with children.
Note: The p values indicate the levels of statistical significance of the overall difference between the two curves under comparison, adjusted for ages and all other variables included in this figure as covariates in the multivariate regressions.
Figure 3a indicate that, compared to those who are rural residents, the transition probabilities from “active” to “disabled” after age 80 are higher for urban residents (p = 0.0003). Elders living in rural areas have significant advantages in ADL status transition from “disable” to “active” over elders in urban areas at all old ages (p=0.0001). Poorer facilities may force rural old persons to perform daily activities by themselves and more frequent physical activity may enable them to better maintain or recover their capacities for daily living than their urban counterparts do. Furthermore, a harder life and higher mortality at younger ages in rural areas may have resulted in a population of old persons who are more selected than their counterparts in cities and towns are.
The results in Figure 3b shown that male elders have advantages over females in ADL status transition probabilities from “active” to “disabled” (p = 0.012), and from “disable” to “active” (p = 0.002). Such gender differentials of male advantages in ADL status transition found in this study is consistent with the existing literature (e.g. Manton and Land, 2000).
There are almost no differences in transition probabilities from “active” to “disabled” between the groups who are currently married and not currently married including never-married, divorced and widowed; married elders have some advantages over those unmarried elders in ADL transition probabilities from “disable” to “active”, but the differences are small and not significant (see Figure 3c).
The results in Figure 3d shown that the ADL status transition probabilities from “disabled” to “active” among elders not co-residing with children are significantly higher than those who live with children (p = 0.025); the ADL status transition probabilities from “active” to “disable” among elders who do not co-reside with children are lower than those living with children after age 80, but the estimates are only marginally significant (p = 0.062). Those who live alone may more likely have active ADL capacity; such selection may result in elders having disadvantages in ADL status transitions more likely to co-reside with children compared to those who have good ADL capacity.
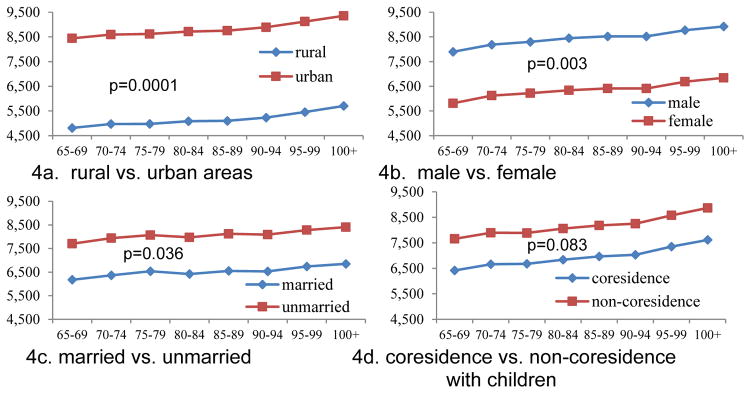
Figure 4 gives the average home-based care cash expenditures per disabled elder per year by rural/urban residence, gender, marital status, and co-residence with children, which are estimated based on the CLHLS 2008 survey data and used as input for projection in the present study. The results presented in Figures 4a, 4b, 4c show that home-based care expenditures in cash per disabled elder per year are substantially and significantly higher among those who are in urban areas (p = 0.0001), males (p = 0.003), and the unmarried (p = 0.036), compared to those who are in rural areas, females, and currently married, respectively. The home-based care cash costs for those who do not co-reside with children are sizably higher than those living together with children, but the estimates are only marginally significant (p = 0.083).
Figure 4. Annual home-based care costs in cash (yuan) per ADL disabled elder, by rural/urban residence, gender, marital status, and coresidence with children.
Note: The same as in Figure 3.
3.2. Trends under the medium scenario
Tables 2, 3 and 4 show the outcomes of the projections under the medium scenario, which is in general reasonable and helpful to understand the basic characteristics of future trends (Smith et al., 2001), while the high and low scenarios reflect uncertainties and they will be discussed in the next section. A few insights can be summarized based on the massive information of our projection results.
Table 2.
Projected numbers of ADL disabled elders (in thousands), by age, marital status, and living arrangement with children, under the Medium scenario, 2010–2050
| Disabled young elders aged 65–79 | Disabled oldest-old aged 80+ | Total disabled elders | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| married | unmarried | total | married | unmarried | total | married | unmarried | total | |||||||
| year | living with child | Not with child | living with child | living alone | living with child | Not with child | living with child | living alone | living with child | Not with child | living with child | living alone | |||
| 2010 | 1,688 | 1,178 | 1,367 | 476 | 4,709 | 461 | 347 | 2,266 | 595 | 3,670 | 2,149 | 1,526 | 3,634 | 1,071 | 8,380 |
| 2020 | 2,714 | 1,882 | 1,812 | 644 | 7,052 | 752 | 531 | 3,327 | 1,012 | 5,622 | 3,466 | 2,413 | 5,138 | 1,657 | 12,674 |
| 2030 | 3,983 | 2,802 | 2,692 | 977 | 10,454 | 1,296 | 891 | 4,821 | 1,519 | 8,526 | 5,278 | 3,693 | 7,512 | 2,496 | 18,980 |
| 2040 | 5,423 | 3,823 | 3,634 | 1,489 | 14,369 | 2,177 | 1,525 | 7,837 | 2,539 | 14,078 | 7,601 | 5,347 | 11,471 | 4,028 | 28,447 |
| 2050 | 4,895 | 3,539 | 3,154 | 1,845 | 13,432 | 4,096 | 2,899 | 12,578 | 4,291 | 23,864 | 8,991 | 6,438 | 15,732 | 6,135 | 37,296 |
| 2010–30 annual growth rate % | 4.4 | 4.4 | 3.4 | 3.7 | 4.1 | 5.3 | 4.8 | 3.8 | 4.8 | 4.3 | 4.6 | 4.5 | 3.7 | 4.3 | 4.2 |
| 2030–50 annual growth rate % | 1.0 | 1.2 | 0.8 | 3.2 | 1.3 | 5.9 | 6.1 | 4.9 | 5.3 | 5.3 | 2.7 | 2.8 | 3.8 | 4.6 | 3.4 |
| 2010–50 annual growth rate% | 2.7 | 2.8 | 2.1 | 3.4 | 2.7 | 5.6 | 5.5 | 4.4 | 5.1 | 4.8 | 3.6 | 3.7 | 3.7 | 4.5 | 3.8 |
| Ratio of # in 2030 to 2010 | 2.4 | 2.4 | 2.0 | 2.1 | 2.2 | 2.8 | 2.6 | 2.1 | 2.6 | 2.3 | 2.5 | 2.4 | 2.1 | 2.3 | 2.3 |
| Ratio of # in 2050 to 2010 | 2.9 | 3.0 | 2.3 | 3.9 | 2.9 | 8.9 | 8.4 | 5.6 | 7.2 | 6.5 | 4.2 | 4.2 | 4.3 | 5.7 | 4.5 |
Table 3.
Projected home-based care costs (in cash) for ADL disabled elders, and home-based care workdays delivered by family members for disabled elders, under the Medium scenario, 2010–2050
| % of total home-based care costs (in cash) for disabled elders among national GDP | Home-based care workdays for disabled elders delivered by family members (in millions) | ||||
|---|---|---|---|---|---|
| year | Home-based care costs grow at the same rate of GDP growth | Home-based care costs growth rates estimated by time series analysis | Aged 65–79 | Aged 80+ | subtotal |
| 2010 | 0.24 | 0.24 | 1,210 | 1,128 | 2,338 |
| 2020 | 0.37 | 0.45 | 1,795 | 1,740 | 3,535 |
| 2030 | 0.57 | 0.75 | 2,694 | 2,646 | 5,340 |
| 2040 | 0.88 | 1.16 | 3,747 | 4,413 | 8,160 |
| 2050 | 1.18 | 1.58 | 3,505 | 7,494 | 11,000 |
| 2010–30 annual growth rate % | 4.4 | 5.9 | 4.1 | 4.4 | 4.2 |
| 2030–50 annual growth rate % | 3.7 | 3.8 | 1.3 | 5.3 | 3.7 |
| 2010–50 annual growth rate % | 4.0 | 4.8 | 2.7 | 4.9 | 4.0 |
| Ratio of # in 2030 to 2010 | 2.4 | 3.1 | 2.2 | 2.3 | 2.3 |
| Ratio of # in 2050 to 2010 | 4.9 | 6.5 | 2.9 | 6.6 | 4.7 |
Table 4.
Projected rural/urban distributions of young-old and oldest-old ADL disabled elders (in thousands), under the Medium scenario, 2010–2050
| Disabled young-old aged 65–79 | Disabled oldest-old aged 80+ | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| urban | rural | Total | urban | rural | Total | |||||||
| year | # | % | # | % | # | % | # | % | # | % | # | % |
| 2010 | 2,356 | 50.0 | 2,354 | 50.0 | 4,709 | 100 | 1,677 | 45.7 | 1,993 | 54.3 | 3,670 | 100 |
| 2020 | 3,785 | 53.7 | 3,266 | 46.3 | 7,052 | 100 | 2,870 | 51.0 | 2,752 | 49.0 | 5,622 | 100 |
| 2030 | 6,358 | 60.8 | 4,096 | 39.2 | 10,454 | 100 | 4,682 | 54.9 | 3,844 | 45.1 | 8,526 | 100 |
| 2040 | 9,598 | 66.8 | 4,771 | 33.2 | 14,369 | 100 | 8,518 | 60.5 | 5,560 | 39.5 | 14,078 | 100 |
| 2050 | 10,320 | 76.8 | 3,112 | 23.2 | 13,432 | 100 | 15,841 | 66.4 | 8,023 | 33.6 | 23,864 | 100 |
Disabled elders will increase substantially faster than the total elderly population. Numerical results in Table 2 show that, during the period 2010–2050, the annual growth rate of the number of disabled elders (3.8%) is substantially higher than that of the total elderly population (data not shown in the Tables) by more than one third. The number of disabled elders in 2050 will be 4.5 times as many as that in 2010, while the total number of old-age adults in 2050 will be 3.0 times as large as that in 2010. The dramatically rapid increase of the Chinese oldest-old aged 80+ compared to the young-old aged 65–79 in the next a few decades (as reviewed in the introduction section) may partially explain why the average annual growth rate of disabled elders is substantially higher than the annual growth rate of total elderly population during 2010–2050, because oldest-old have substantially higher likelihood of being ADL disabled as compared to young-old. Another explanation may be the rapid increase of proportion of urban population, while the urban elders have higher rates of ADL disability (see Figure 3a as discussed earlier).
Home-based care needs and costs for disabled oldest-old will increase much faster than that for disabled young-old after 2030. In general, the annual growth rate of disabled oldest-old in 2010–2050 is 4.8%, which is 1.8 times as high as that of the annual growth rate of disabled young-old (2.7%). The number of disabled oldest-old in 2050 will be 6.5 times as many as that in 2010, in contrast to the corresponding figures of 2.9 times for disabled young-old (see Table 2). The results in Tables 2 and 3 show that, during the period 2010–2030, the average annual growth rate of disabled oldest-old and the home-based care workdays devoted to them (4.3%–4.4%) is slightly higher than that of disabled young-old (4.1%). However, during the period 2030–2050, the average annual growth rate of disabled oldest-old and the home-based care workdays devoted to them (5.3%) is 4.2 times as high as that of disabled young-old (1.3%). These numerical results indicate that the speed of increase in home-based care needs and costs for disabled oldest-old will be accelerated and much faster than that for disabled young-old after 2030, which is due to that the baby boomer cohorts born in 1950s–1960s will enter oldest-old ages after 2030.
Disabled unmarried elders living alone increase substantially faster than those disabled unmarried elders living with children. The annual growth rates for disabled young-old and oldest-old who are un-married and living alone are 3.4 and 5.1 percent on average, respectively, which are much higher than those who are un-married and living together with children (2.1% and 4.4%) during the period 2010–2050 (see Table 2). The number of disabled young-old and oldest-old who are un-married and live alone in 2050 will be 3.8 times and 7.2 times as large as that in 2010, while the corresponding figures for those who are unmarried but co-reside with children will be 2.8 times and 5.0 times.
Increase of percentage of home--based care costs in cash for disabled elders as a fraction of total GDP is much faster than growth of elderly population. The annual growth rate in percentage of home-based care costs in cash for disabled elders as a fraction of total GDP in the 1st half of this century will be about 4.0%–4.8%, which is about 1.5–2.0 times as high as the annual growth rate of the elderly population (see Table 3). Such a trend may be mainly due to, compared to the total elderly population, increases in the proportions of disabled older adults is faster in general, and especially much faster increase in disabled oldest-old and those disabled elders living alone in urban areas, whose home-based care costs per person are substantially higher.
Percent of rural disabled oldest-old will be substantially higher than percent of rural population after 2030. Data in Table 4 show that the rural- urban distributions of disabled young-old is generally consistent with the proportion of rural and urban residents of the total population. However, the percentage of disabled oldest-old in rural areas among the total number of disabled oldest-old of rural-urban combined in 2030 and 2050 is 45.1% and 33.6% (see Table 4), which is 5.1 and 8.6 percentage points higher than that of the projected proportion of rural residents among total population (see Table 1). The main reason is that most rural peasants, who were middle-aged in the 1980s and 1990s and will become oldest-old after 2030, may stay in their villages, while the large-scale population migration from rural to urban areas may continue to occur among younger people.
3.3. Possible ranges of the trends
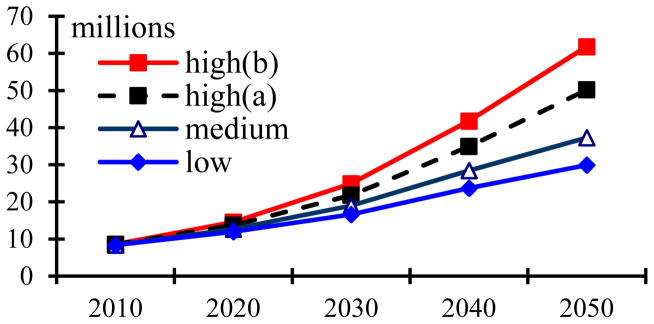
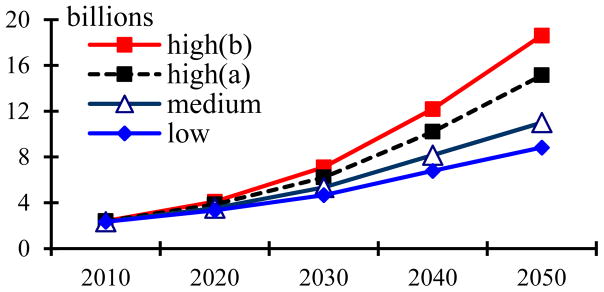
The projection results under the low, medium, high(a), and high(b) scenarios presented in Figure 5 show that the total number of disabled elders in China will rapidly climb from 8.4 million in 2010 to 12.7–14.6, 19.0–24.9, and 37.3–61.8 million in 2020, 2030, and 2050, respectively. Figure 6 shows that the non-cash workdays of care provided by family members will increase rapidly from 2.3 billion workdays in 2010 to 3.5–4.1, 5.3–7.1, and 11.0–18.6 billion workdays in 2020, 2030, and 2050, respectively. Figure 7b shows that the percentage of home-based care expenditures in cash for disabled elderly among total GDP in China will grow from 0.24% in 2010 to 0.35–0.41%, 0.49–0.71%, and 0.85–1.66% in 2020, 2030, and 2050, respectively, assuming that the annual growth rates of home-based care costs for disabled elderly are the same as the annual growth rates of GDP. The percentage of total amount of home-based care expenditures in cash for disabled elders as a fraction of the total GDP in 2020, 2030, and 2050 will increase to 0.41–0.49%, 0.63–0.92% and 1.14–2.21%, if we assume estimate the annual growth rate of home-based care expenditures per disabled elder in 2010–2030 based on time series data analysis and trend extrapolation, and the care costs and GDP grow at the same speed after 2030 (see Figure 7a). Note that the gap between the high (b) and low scenarios will increasingly enlarge as the projection period is prolonged, which is similar to the results in other demographers’ high, medium and low projections (Lee and Tuljapurkar, 2001, p.22).
Figure 5.
Projected numbers of ADL disabled elders under different scenarios (in millions)
Figure 6.
Projected numbers of home-based care work days for disabled elders delivered by family members under different scenarios (in billions)
Figure 7.
Figure 7a. Projected percentages of total home-based care costs in cash for disabled elders among national GDP, service wages follow trend extrapolation
Figure 7b. Projected percentages of total home-based care costs in cash for disabled elders among national GDP, service wages grow at same rate of GDP
3.4. Resources of care providers under different fertility policy scenarios
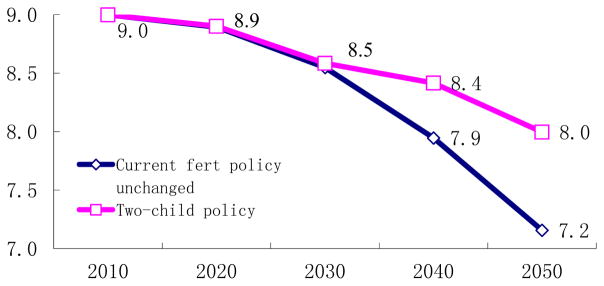
Under the current fertility policy unchanged, the caregivers who are of working ages 18–64 will quickly shrink from 910 million in 2030 to 730 million in 2050. After 2030 to 2080, the number of caregivers will be reduced by about 90 million every 10 years. As compared to 2030, the number of caregivers in 2050 will decline by 20 percent. The number of caregivers aged 18–64 per elderly aged 65+ will dramatically decrease from 8.0 in 2010 to 3.5, and 2.0 in 3030 and 2050, respectively; the elderly dependent burden in 2030 and 2050 will be 2.3 and 4.1 times as high as that in 2010 (see Figure 8). The number of caregivers under the two-child policy will be 47 million and 84 million more than that under the current fertility policy unchanged in 2040 and 2050. As clearly shown in Figure 8, the resources of caregivers and old-age support burden under the two-child policy will be substantially better than that under the current policy unchanged.
Figure 8.
Projected numbers of caregivers aged 18–64 under different fertility policies (unit: 100 millions)
3.5. Sensitivity analysis
The sensitivity analysis presented in Table 5 shows that, as compared to the scenario which assumes constant ADL status transition rates, improved or deteriorated ADL status transition rates would cause care needs and costs of disabled elders in 2030 to be reduced by 10.9–12.6% (low versus medium scenarios) or increased by 12.6–14.2% (high(b) versus high(a) scenarios); the corresponding change in 2050 would be a reduction of 17.8–19.8% or increase of 30–32%. As compared to the medium mortality scenario, the more remarkable decline in mortality rates in the high(b) scenario would increase the home-based care needs and costs for disabled elderly by 11.9–25.2% and 29.6–37.7% in 2030 and 2050, respectively.
Table 5.
Sensitivity analysis of the impacts of future changes in the mortality rate and prevalence of ADL disability on home-based care needs/costs for the elderly
| year | High(a) vs. medium scenarios: impact of mortality rates declining more rapidly | High(b) vs. high(a) scenarios: Impact of ADL disability deteriorating | Low vs. medium scenarios: Impact of ADL disability improving | ||||||
|---|---|---|---|---|---|---|---|---|---|
| # of disabled elders | Care costs in cash | Opportunity costs | # of disabled elders | Care costs in cash | Opportunity costs | # of disabled elders | Care costs in cash | Opportunity costs | |
| 2020 | +8.36% | +6.17% | +9.24% | +6.09% | +5.23% | +6.08% | −5.75% | −4.84% | −5.75% |
| 2030 | +14.97% | +11.88% | +16.56% | +14.23% | +12.57% | +14.20% | −12.54% | −10.85% | −12.60% |
| 2040 | +22.94% | +18.87% | +25.19% | +19.52% | +17.68% | +19.40% | −16.74% | −14.81% | −16.78% |
| 2050 | +34.56% | +29.61% | +37.69% | +23.18% | +21.40% | +22.92% | −19.74% | −17.83% | −19.75% |
4. DISCUSSIONS AND POLICY CONSIDERATIONS
This study shows that declines in mortality rates and changes in older adults’ ADL status are the two most important determinants of home-based care needs and costs for disabled elders in the 1st half of this century in China. Our analysis also shows that, regardless of whether ADL status change rates are assumed to improve or deteriorate over time, and whether mortality rates decrease moderately or remarkably, the home-based care needs and costs for older adults in China will increase substantially due to the inevitable trends of population aging and extremely fast increases of the oldest-old. Consequently, relevant reforms of policies and socioeconomic planning should be taken to respond to the serious challenges of large and rapid increases in home-based care needs and costs.
Our projections found that if ADL status change rates substantially improve (under the low scenario) or substantially deteriorate (under the high(b) scenario), the care needs and costs for disabled elders would remarkably decrease or increase accordingly. Note that the most effective way to improve elderly ADL statuses is not only to cure disease, but also to effectively prevent illnesses. The latter may be more important since elders who are cured of one illness are likely to suffer another illness and long-term ADL disability if there is no improvement in their abilities to prevent disease. Therefore, studies of why some elders remain happy and healthy up to the oldest-old ages, and how to reach such pathways of healthy aging should be further strengthened.
Our analyses shows that female elders have significant disadvantages in ADL status transitions compared with male counterparts (see Figure 3b). However, the home-based care expenditures for female disabled elders are much lower than those for male disabled elders (see Figure 4b); this is an important problem that should receive much more attention from the Chinese government and society. The government and society should try their best to guarantee that both male and female older adults enjoy equal benefits. The finding that home-based care expenditures for disabled elders without a spouse are much higher than expenditures for married disabled elders (see Figure 4c) indicates that, in order to reduce home-based care costs for the elderly, remarriage for widows and widowers should be strongly encouraged and a series of measures should be taken to remove obstacles to remarriage, especially in rural areas, in terms of laws, regulations, and social attitudes.
This study shows that if the current fertility policy remains unchanged, the burden of home-based care for disabled older adults per caregivers of working ages will be increasingly aggravated and much more serious than that under the two-child policy. The projection results demonstrate the lagging effect of fertility policy transition due to the fact that it takes about 20 years for the new births to join the labor force, but this substantially alleviates the serious challenge of population aging and caregiving in China. If China adopts the two-child policy as soon as possible, the home-based care burden for disabled elderly per caregiver of working ages will be significantly reduced after 2030 compared to the current fertility policy unchanged scenario. If the fertility policy transition is delayed 5–10 years, the newly born babies will still be children or adolescents who need to be supported for a rather long period after 2030; this need will combine with the sharp increase in the elderly population and rapid decline of care givers resources then, and thus overload the working-age population and bring the social security system of China to the verge of collapse. Furthermore, the results of other studies show that there are many other serious problems if the present fertility policy in China remains unchanged (Zeng, 2006, 2009a; 2009b; 2009c). Thus, we suggest that the two-child policy should be launched as soon as possible.
Our projection results also show that, even under the two-child policy, home-based care needs and costs for disabled elders per working-age person will increase remarkably; disabled unmarried elders living alone increase substantially faster than those disabled unmarried elders living with children; percent of rural disabled oldest-old will be substantially higher than percent of rural population after 2030. Besides the adjustment of current fertility policy, other socioeconomic countermeasures should also be taken. For example, including elderly parents (especially oldest-old) in rural-to-urban family migration; adult children may be encouraged to live together with or near to their old-age parents especially those unmarried old parents, which will help elders to obtain home-based care from children whenever need. Co-residence with or close proximity to children will decrease cash home-based care expenditures for disabled older adults; living in close proximity would overcome intergenerational conflicts between elders and their co-residing children/grandchildren concerning eating and entertainment, etc., which will increase the happiness of elderly parents.
5. CONCLUDING REMARKS
In sum, this article further develops and empirically applies the ProFamy extended cohort-component model to project future home-based care needs and costs for disabled older adults, by an integration of multistate projections of elderly disability status transitions with those of household structures and living arrangements, based on the commonly available demographic data. This integrated multistate model projects the dynamics of ADL statuses and yearly workdays and payments for disabled elders, providing relatively more realistic and detailed information of future trends than previous similar studies which excluded elderly living arrangements, which is a crucially important determinant of home-based care needs and costs. To our knowledge, this is the first successful attempt to integrate multistate dynamic projections of elderly activity of daily living statuses transitions, household structure, living arrangements, home-based care needs and costs for disabled elders, as well as the working-age care providers simultaneously in one model. The detailed projections we have presented could prove useful for governmental policy analysis and strategic plans of future public services and for private sector market potentials research.
There are, however, some important limitations of the projections presented in this study that should be investigated in future research. First, due to space limitations, we have presented here only the general trends and patterns of both-genders-combined numbers of disabled elders aged 65+ and disabled oldest-old aged 80+, and the yearly workdays and payments of home-based care for them by rural/urban residence and living arrangement. These results are extracted from more detailed projection outcomes of the numbers of disabled elders, the yearly workdays and payments of home-based care by gender, rural/urban residence, five-year age groups, marital status and living arrangements, based on our multistate model and the available CLHLS datasets.
Second, in this article, we mainly follow the expert opinion approach for projecting future demographic summary measures, disability trends and per-disabled-elder home-based care hours and payments. This serves reasonably well for the purpose of demographic and policy research simulations in a relatively longer time horizon of 40 years from 2010 to 2050. Within the multistate model framework, future summary measures can also be forecasted using methods of time series analysis and regression models with a focus on shorter forecasting time horizons. Furthermore, these parameters may be forecasted by regressions including time series data of other related socioeconomic covariates. It should always be noted, however, that the accuracy of the forecasts relies heavily on the validity of assumptions regarding future time paths of the various covariates included in the forecasting model. Erroneous assumptions about too many covariates and parameters included in the model can quickly lead to forecasts that are far off the mark (e.g. Lee and Tuljapurkar 2001).
Finally, we emphasize that projections for time horizons of less than 20 years may be used as forecasting for business and governmental planning, but any results beyond that should be considered to be simulations only, due to large uncertainties after more than 20 years. Thus, the projection results of the middle years of this century presented in this article should be mainly regarded as simulations. Such simulations are useful for the academic and policy analysis to answer the “what, if” questions about effects of changes in demographics and disability status transition rates on the future general trends and patterns of elderly disability, home-based care needs and costs for disabled elders in China, but they cannot be considered to be accurate forecasts.
Footnotes
This study is funded by the research grants of the major project of Humanity and Social Science Key Research Centers Foundation of Ministry of Education of China (2009JJD790001) (YZ), National Natural Science Foundation of China (71110107025) (YZ), Humanity and Social Science Youth Foundation of Ministry of Education of China (10YJC790021) (HC).
References
- Bongaarts J. The projection of family composition over the life course with family status life tables. In: Bongaarts J, Burch T, Wachter KW, editors. Family demography: Methods and applications. Oxford, UK: Clarendon Press; 1987. pp. 189–212. [Google Scholar]
- Bongaarts J, Feeney G. On the Quantum and Tempo of Fertility. Population and Development Review. 1998;24(2):271–291. [Google Scholar]
- Burch TK. Comment on a comparison between headship-rate approach and the ProFamy method. Personal email communication. 1999.
- Chen H. Assessment of the quality of the cross-sectional data collected in the 2008 wave of Chinese Longitudinal Healthy Longevity Survey. In: Zeng Yi., editor. Research on Elderly Population, Family, Health and Care Needs/Costs (in Chinese) Beijing: Science Press; 2010. pp. 350–352. [Google Scholar]
- CMMS: Center for Medicare and Medicaid Services. Projections of National Health Expenditures: Methodology and Model Specification. Baltimore: the Centers for Medicare & Medicaid Services; 2004. http://www.cms.hhs.gov/statistics/nhe/projections-methodology/ [Google Scholar]
- Dalton M, O’Neill B, Prskawetz A, Jiang L, Pitkin J. Population aging and future carbon emissions in the United States. Energy Economics. 2008;30:642–675. [Google Scholar]
- Du P, Wu C. Ability of Daily Life of the Chinese Elderly: Status and Change. Population Research. 2006;30(1):50–56. [Google Scholar]
- Feng Q, Wang Z, Gu D, Zeng Y. Household Vehicle Consumption Forecasts in the United States, 2000 to 2025. International Journal of Market Research. 2011;53(5):593–618. [Google Scholar]
- Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- Goodkind D. Review on the book Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Population Studies. 2009;63(3):1–7. [Google Scholar]
- Grundy E. United Nations Population Bulletin. 2001. Living arrangements and the health of older persons in developed countries. Special Issue Nos. 42/43. [Google Scholar]
- Grundy E. Opening keynote speech at the “Households and Living Arrangement Projections: New Method, Software and Applications”, held at the 27th General Conference of International Union for Scientific Population Studied (IUSSP), August 30 (the entire conference was held in August 26–31); 2013; Busan, Korea. 2013. [Google Scholar]
- Gu D. General data quality assessment of the CLHLS. In: Zeng Yi, Poston Dudley, Vlosky Denese Ashbaugh, Gu Danan., editors. Healthy Longevity in China: Demographic, Socioeconomic, and Psychological Dimensions. Dordrecht: Springer Publisher; 2008. pp. 39–60. [Google Scholar]
- Gu D, Zeng Y. Changes of Disability in Activities of Daily Living among the Chinese Elderly from 1992 to 2002. Population & Economics. 2006;4:9–13. [Google Scholar]
- Heath Bureau of Shanghai. [accessed April 27, 2013];Health Status in Shanghai, 2011. 2012 http://www.chinanews.com/df/2012/02-20/3682967.shtml.
- Huang C. Elderly health and family care burden in China. Chinese Health Resources. 2006;9(5) [Google Scholar]
- Hu A, Tang W, Wang H, Mo Z, Wang B, Chen Z. Reasonably Distribute the Eldercare Health Service. Population and Economics. 2003;138(3):13–18. [Google Scholar]
- Jiang C. PhD thesis. Beijing: Peking University, China Center for Economic Research; 2008. The Analysis and Prediction on the ADL Care Cost for the Chinese Elderly. [Google Scholar]
- Lakdawalla D, Goldman DP, Bhattacharya J, Hurd MD, Joyce GF, Panis CWA. Forecasting the nursing home population. Medical Care. 2003;41(1):8–20. doi: 10.1097/00005650-200301000-00003. [DOI] [PubMed] [Google Scholar]
- Land KC, Guralnik JM, Blazer DG. Estimating Increment-Decrement Life Tables with Multiple Covariates from Panel Data: The Case of Active Life Expectancy. Demography. 1994;31(2):297–319. [PubMed] [Google Scholar]
- Lee RD, Tuljapurkar S. Population Forecasting for Fiscal Planning: Issues and Innovation. In: Auerbach AJ, Lee RD, editors. Demographic Changes and Fiscal Policy. Cambridge: Cambridge University Press; 2001. [Google Scholar]
- Li J. Economic Analysis of Burdens for Elderly Population in China. Population Research. 1998;22(6):5–10. [Google Scholar]
- Li L, Chen Q. Impacts of Population Changes on the National Medical and Health Care System. In: Zeng Y, Li L, Gu B, et al., editors. 21st Century Population and Economic Development in China. Social Sciences Academic Press of China; Beijing: 2006. pp. 221–235. [Google Scholar]
- Liang H. Studies on Self-supporting Abilities of Rural Elderly in China. Population and Economics. 1999;115(4):21–25. [Google Scholar]
- Manton KG. Changing concepts of morbidity and mortality in the elderly population. Milbank Q/Health Society. 1982;60:183–244. [PubMed] [Google Scholar]
- Manton KG, Land KC. Active life expectancy estimates for the U.S. elderly population: A multidimensional continuous mixture model of functional change applied to complete cohorts, 1982–1996. Demography. 2000;37(3):253–265. [PubMed] [Google Scholar]
- Mason A, Racelis R. A comparison of four methods for projecting house- holds. International Journal of Forecasting. 1992;8:509–527. doi: 10.1016/0169-2070(92)90061-d. [DOI] [PubMed] [Google Scholar]
- Mayhew L. Health and elderly care expenditure in an aging world. IIASA; Laxenburg, Austria: 2000. [Google Scholar]
- Murphy M. Modeling households: A synthesis. In: Murphy MJ, Hobcraft J, editors. Population research in Britain, A supplement to population studies. Vol. 45. London, UK: Population Investigation Committee, London School of Economics; 1991. pp. 157–176. [Google Scholar]
- Olshansky SJ, Rudberg MA, Carnes BA, Cassel CK, Brody JA. Trading off longer life for worsening health: the expansion of morbidity hypothesis. J Aging Health. 1991;3:194–216. [Google Scholar]
- Prskawetz A, Jiang L, O’Neill B. Vienna yearbook of population research. Vienna, Austria: Austrian Academy of Sciences Press; 2004. Demographic composition and projections of car use in Austria; pp. 274–326. [Google Scholar]
- Scafato E, Galluzzo L, Gandin C, et al. Marital and cohabitation status as predictors of mortality: A 10-year follow-up of an Italian elderly cohort. Social Science & Medicine. 2008;67:1456–1464. doi: 10.1016/j.socscimed.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Serup-Hansen N, Wickstrøm J, Kristiansen IS. Future health care costs-do health care costs during the last year of life matter? Health Policy. 2002;62:161–172. doi: 10.1016/s0168-8510(02)00015-5. [DOI] [PubMed] [Google Scholar]
- Shekelle PG, Ortiz E, Newberry SJ, Rich MW, Rhodes SL, Brook RH, Goldman DP. Identifying potential health care innovations for the future elderly. Health Affairs. 2005:W5-R67–R76. doi: 10.1377/hlthaff.w5.r67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen K. Assessment of the quality of the follow-up mortality data collected in the 2008 wave of Chinese Longitudinal Healthy Longevity Survey. In: Zeng Yi., editor. Research on Elderly Population, Family, Health and Care Needs/Costs (in Chinese) Beijing: Science Press; 2010. pp. 352–354. [Google Scholar]
- Smith SK, Rayer S, Smith EA. Aging and Disability: Implications for the Housing Industry and Housing Policy in the United States. Journal of the American Planning Association. 2008;74(3):289–306. [Google Scholar]
- Smith SK, Tayman J, Swanson DA. State and local population projections: Methodology and analysis. New York: Kluwer Academic/Plenum Publishers; 2001. [Google Scholar]
- Smith SK, Rayer S, Smith E, Wang Z, Zeng Y. Population Aging, Disability and Housing Accessibility: Implications for Sub-national Areas in the United States. Housing Studies. 2012;27(2):252–266. [Google Scholar]
- Spicer K, Diamond I, Bhrolcham MN. Into the twenty-first century with British households. International Journal of Forecasting. 1992;8:529–539. doi: 10.1016/0169-2070(92)90062-e. [DOI] [PubMed] [Google Scholar]
- Suthers K, Kim JK, Crimmins E. Life expectancy with cognitive impairment in the older population of the United States. Journal of Gerontology: Social Sciences. 2003;58B(3):S179–S186. doi: 10.1093/geronb/58.3.s179. [DOI] [PubMed] [Google Scholar]
- UN(Population Division, United Nations) World Population Prospects: The 2005 Revision Volume II: Sex and Age. New York: United Nations; 2011. [Google Scholar]
- World Bank and the Development Research Center of State Council of China. China 2030: Building a Modern, Harmonious, and Creative Society. Washington: The World Bank; 2013. [Google Scholar]
- Zeng Y. Family Dynamics in China: A Life Table Analysis. Wisconsin: The University of Wisconsin Press; 1991. [Google Scholar]
- Zeng Y, Vaupel JW, Wang Z. Household Projection Using Conventional Demographic Data. Population and Development Review, Supplementary Issue: Frontiers of Population Forecasting. 1998;24:59–87. [Google Scholar]
- Zeng Y, Land KC, Wang Z, Gu D. U.S. Family Household Momentum and Dynamics -- Extension of ProFamy Method and Application. Population Research and Policy Review. 2006;25(1):1–41. [Google Scholar]
- Zeng Yi. Options of Fertility Policy Transition in China. Population and Development Review. 2007;33(2):215–246. (Heading article) [Google Scholar]
- Zeng Y, Wang Z, Jiang L, Gu D. Future trend of family households and elderly living arrangement in China. GENUS - An International Journal of Demography. 2008;LXIV(1–2):9–36. [Google Scholar]
- Zeng Y, George LK. Population Aging and Old-Age Care in China. In: Dannefer D, Phillipson C, editors. Sage Handbook of Social Gerontology, Thousand. Oaks/CA/USA: Sage Publications; 2010. [Google Scholar]
- Zeng Y, Land KC, Wang Z, Gu D. Household and Living Arrangements Projections At The Sub-National Level: An Extended Cohort-Component Approach. Forthcoming in. Demography. 2013;50:827–852. doi: 10.1007/s13524-012-0171-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng Y, Shen K, Wang Z. Multistate Projections and Policy Analysis of Population and Household Aging in Eastern, Middle, and Western Regions of China in the 1st Half of the 21st Century. 2013 Manuscript submitted to a peer-reviewed journal for consideration of publication. [Google Scholar]
- Zhang Z. PhD thesis. Beijing: Peking University; 2004. Impact of intergenerational support on healthy longevity. [Google Scholar]