Abstract
PURPOSE
The purpose of this study was to evaluate the resistance to deformation under static overloading by measuring yield and fracture strength, and to analyze the failure characteristics of implant assemblies made of different titanium grades and connections.
MATERIALS AND METHODS
Six groups of implant assemblies were fabricated according to ISO 14801 (n=10). These consisted of the combinations of 3 platform connections (external, internal, and morse tapered) and 2 materials (titanium grade 2 and titanium grade 4). Yield strength and fracture strength were evaluated with a computer-controlled Universal Testing Machine, and failed implant assemblies were classified and analyzed by optical microscopy. The data were analyzed using the One-way analysis of variance (ANOVA) and Student's t-test with the level of significance at P=.05.
RESULTS
The group IT4S had the significantly highest values and group IT2 the lowest, for both yield strength and fracture strength. Groups IT4N and ET4 had similar yield and fracture strengths despite having different connection designs. Group MT2 and group IT2 had significant differences in yield and fracture strength although they were made by the same material as titanium grade 2. The implant system of the similar fixture-abutment interfaces and the same materials showed the similar characteristics of deformation.
CONCLUSION
A longer internal connection and titanium grade 4 of the implant system is advantageous for static overloading condition. However, it is not only the connection design that affects the stability. The strength of the titanium grade as material is also important since it affects the implant stability. When using the implant system made of titanium grade 2, a larger diameter fixture should be selected in order to provide enough strength to withstand overloading.
Keywords: Dental Implant-Abutment Connection, Titanium grade, Yield strength, Static loading, Implant failure
INTRODUCTION
Osseointegrated dental implants have become increasingly important in the field of oral rehabilitation1 with many studies reporting up to 99% the long-term success of dental implants.2,3,4 However, many reports assessing the prosthetic complications of implants showed that screw loosening, screw fracture, and implant mid-body fracture occur commonly, especially in single crowns which do not distribute the bite force to other implants.5,6,7,8
During the past years, manufacturers have developed different types of implant-abutment connections to achieve implant stability and strength. For a successful implantation, it is essential that the implant assembly has enough strength to resist the stress in the oral cavity and transmit forces to the bone; other requirements are biocompatibility of components, correct diagnosis, and appropriate surgical and prosthodontic procedures for implant placement. Thus, for an implant assembly to withstand the bite force in patients, the properties of the material and type of connection of the implant system should be considered. In addition, the stress exerted on the functional prosthesis should not exceed the fracture resistance of the implant assembly.9,10
Usually, mechanical failures of implant occur more from repeatable fatigue that lowers load than fracture strength of implant. However, static fracture of implants from overload also occurs frequently, due to factors such as clenching habit, hard food, and premature contact resulting from failure of occlusal adjustment.11,12 In addition, for the ethnic group which enjoys chewing hard or coarse food than tender vegetables or meats, the enough strength of the implant assemblies is important to prevent mechanical failure because the stress applied to implant prosthesis after intraoral insertion was influenced by dietary habits.
These days, the primary materials used for implant fixtures and abutments is commercially pure titanium, grade 2 and grade 4, the screw is usually made from a titanium alloy classified as titanium grade 5 (Ti-6Al-4V). Titanium grade 4 has the highest mechanical strength of all unalloyed Ti. Despite the relatively lower mechanical strength of titanium grade 2, the manufactures using this material have insisted that it is less brittle, and the elasticity and flexibility are beneficial in clinical situations. They have also suggested that implant of Ti grade 2 can be made resistant to local forces by using a greater amount of material to compensate for its lower mechanical strength.
The effects of differences in the design of the implant-abutment connection on the mechanical stability have been evaluated in various in vitro studies. However, few studies have considered the properties of the material used as well as the design of the implant connection. In addition, in studies comparing materials, zirconia and titanium have been compared as abutment materials13,14,15 rather than comparing different grades of titanium. Furthermore, manufacturers tend to claim that their own systems are superior to those of their competitors, but they do not provide specific data on the complications and types of failure of their systems.
The purpose of this study was to evaluate the stability of implant–abutment assemblies made of different titanium grades and using different connections by measuring the compressive load at yield corresponding to yield strength, and the fracture point, and to analyze the failure characteristics of different implant systems under static overloading in order to anticipate the failures that may occur in clinical situations.
MATERIALS AND METHODS
The experimental models were prepared by combining different connections in macrogeometry (external hexagon, internal hexagon, morse tapered) and different materials (titanium grade 2 and 4), yielding six implant systems (Table 1). For internal connection types of titanium grade 4, group IT4S (Straumann Bone level, Institute Straumann AG, Waldenburg, Switzerland), group IT4D (Dentium Superline, Dentium, Co., Ltd., Korea), and group IT4N (Neobiotech CMI IS, Neobiotech, Co., Ltd., Korea) were used. Group IT2 (Dentsply Xive s, Dentsply Friadent, Mannheim, Germany) was used for an internal connection type of titanium grade 2. For the morse tapered connection of titanium grade 2 group MT2 (Ankylos C/X, Friadent GmbH, Mannheim, Germany) was used, and for the external connection type with titanium grade 4 group ET4 (Neobiotech CMI EB, Neobiotech, Co., Ltd., Korea) was used.
Table 1. Connection type and composition of the tested implant systems, and the torque required for screw tightening according to the manufacturers' instructions.
| Group | Connection type | Fixture | Abutment | Abutment screw | Manufacturer's recommended torque (N) | Clinical working vertical dimension (mm) | Implant | Abutment |
|---|---|---|---|---|---|---|---|---|
| IT4S | IH | Ti 4 | Ti 4 | TAN | 35 | 4.2 | Bone level implant Ø4.1 RC/12 mm |
RC cementable Ti abutment GH 2.0 mm |
| IT4D | IH | Ti 4 | Ti 4 | Ti 5 | 30 | 2.8 | Superline platform Ø4.0 body Ø3.8/12 mm |
dual abutment hex Ø4.5 |
| IT4N | IH | Ti 4 | Ti 5 | Ti 5 | 30 | 3.0 | CMI IS Ø4.0/13 mm |
Cementable hex Ø5.2/1.0/5.5 |
| IT2 | IH | Ti 2 | Ti 2 | Unknown Ti alloy | 24 | 2.8 | Xive s implant Ø3.8/13 mm |
FRIADENT EstheticBase straight Ø3.8/ GH2 |
| MT2 | MT | Ti 2 | Ti 2 | Unknown Ti alloy | 24 | 3.4 | Ankylos C/X Ø4.0/13 mm |
Regular/X abutment GH1.5/A0 |
| ET4 | ET | Ti 4 | Ti 5 | Ti 5 | 0030 | 0.7 | CMI EB Ø4.0/13 mm |
Cementable hex Ø5.2/1.0/6.0 |
IH: Internal Hex, MT: Morse Taper, Ti4: Commercially pure titanium grade 4, Ti2: Commercially pure titanium grade 2, Ti 5: Titanium grade 5 (Ti 6 Al 4 V), TAN: Ti 6Al 7Nb.
The components of each system were selected based on sizes as close to 4.0 mm for the fixture neck diameter, and 12 mm for the fixture length. Abutments were fixed to the fixtures by the corresponding screws, with the torque given by the manufacturer (Table 1), and retightened 10 minutes later with the same torque.16,17,18
Hemispherical crowns made of cobalt–chromium alloy were manufactured using computer-aided design/computer-assisted manufacturing (Etkon, Etkon AG, Gräfeling, Germany) and were seated onto the abutments with dual cure resin cement (Rely X Unicem, 3M ESPE, St. Paul, MN, USA).
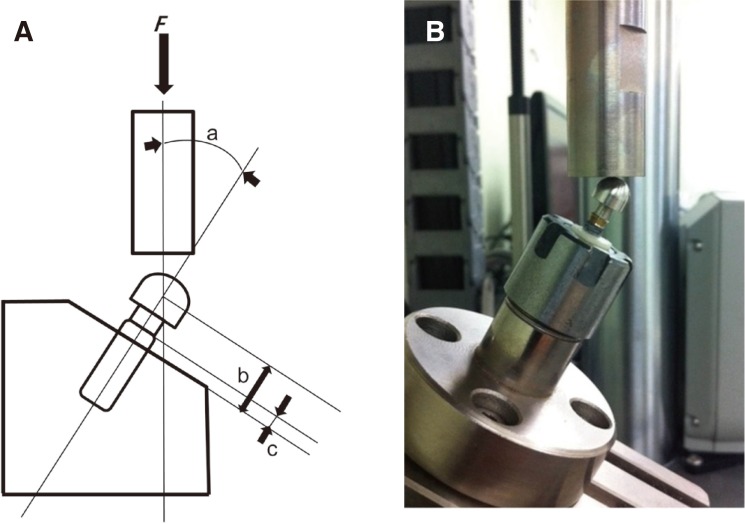
Ten implant fixtures of each group were embedded in acrylic resin (Unifast Trad, GC Corporation, Tokyo, Japan), which has an elastic modulus similar to bone, according to ISO 14801 (Dentistry-fatigue test for dental implants) (Fig. 1A). Following this norm, the vertical distance from the acrylic resin surface representing the bone level to implant shoulder was 3-mm for simulating bone resorption, and the distance to the center of the hemisphere was standardized at 11 mm. The fixtures were then clamped in a jig with a 30° angle between the implant axis and the force direction. The static load was applied using a universal testing machine (Electro Plus E3000, Instron, Norwood, MA, USA) with a crosshead speed of 1 mm/min (Fig. 1B). Load–displacement curves were recorded until visible fracture of the implant assembly was observed, or a decrease of 20% in the fracture strength in cases with no obvious fracture.14 Yield strength (offset 0.2%) and fracture strength were determined from the chart (Table 2), after the movements of the abutments were recorded (Table 3).
Fig. 1. (A) Schematic illustration of the design of the testing apparatus following ISO 14801 (2007). The distance from the center of the hemisphere to the top face of the resin cylinder, representing the bone level, was standardized at 11 mm. The specimens were then clamped in a special jig (machine shop, Hannover Medical School, Hannover, Germany) while ensuring a 30° angle between the implant axis and the direction of force transfer. (B) The set up for mechanical testing, with crowns positioned in a 30° off-axis orientation.
Table 2. Yield strength and Fracture strength values for different types of implant.
| Various implant systems under static loading | |||||||
|---|---|---|---|---|---|---|---|
| IT4S | IT4D | IT4N | IT2 | MT2 | ET4 | P value1 | |
| n = 10 | n = 10 | n = 10 | n = 10 | n = 10 | n = 10 | ||
| Yield strength (N) | 550.44 ± 27.71 | 398.71 ± 46.01 | 367.85 ± 107.63 | 248.05 ± 15.45 | 437.94 ± 73.55 | 366.54 ± 69.08 | < .05 |
| T2 | a | b | b,c | c | a,b | b,c | |
| Fracture strength (N) | 1255.3 ± 145.98 | 1121.1 ± 125.89 | 810.75 ± 107.63 | 613.34 ± 70.86 | 917.07 78.29 | 798.89 ± 48.28 | |
| T2 | a | a | b | c | b | b, c | |
IT4S: Straumann Bone level, IT4D: Dentium superline, IT4N: Neobiotech CMI IS, IT2: Dentsply Xive s, MT2: Ankylos C/X, ET4:Neobiotech CMI EB
1 Statistical significances between groups were tested by one-way analysis of variance.
2 Same letters indicate non-significant differences between groups based on Tukey's multiple comparison test.
Table 3. Frequency distribution of failure types after the fracture strength test.
| Abutment screw | Abutment | Plastic deformation of fixture | Mobility of abutment | |||
|---|---|---|---|---|---|---|
| Bending | Fracture (whole/partially) | Bending | Fracture | |||
| IT4S | 10/10 | 0/10 | 10/10 | 0/10 | 0/10 | 0/10 |
| IT4D | 5/10 | 5 (partially)/10 | 0/10 | 0/10 | 0/10 | 0/10 |
| IT4N | 10/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 |
| IT2 | 10/10 | 0/10 | 0/10 | 0/10 | 10/10 | 9/10 |
| MT2 | 10/10 | 0/10 | 10/10 | 0/10 | 3/10 | 0/10 |
| ET4 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 | 0/10 |
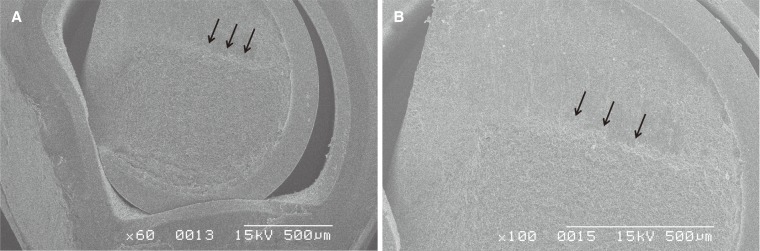
After the static load test, the failed samples were polished with #500 to #4000 grit SiC abrasive papers and aluminum oxide particles until the centers of the longitudinal sections were exposed. Images of these sections were taken with the digital microscope (Sometech, IMS-d-345, Korea). The longitudinal section of group IT4D that had a visible screw fracture in the digital microscopic view, and the cross-section of fractured screw in group IT2 that was loaded until the implant assembly completely fractured were observed with the scanning electron microscope (S-2300, Hitachi, Co., Ltd., Japan) to analyze the failure characteristics.
The mean values of yield and fracture strength, and their standard deviations, are presented in Table 2. One-way analysis of variance (ANOVA) and Student's t-test with the level of significance at P = .05 (SPSS12.0, SPSS Software Corp., Chicago, IL, USA) were used.
RESULTS
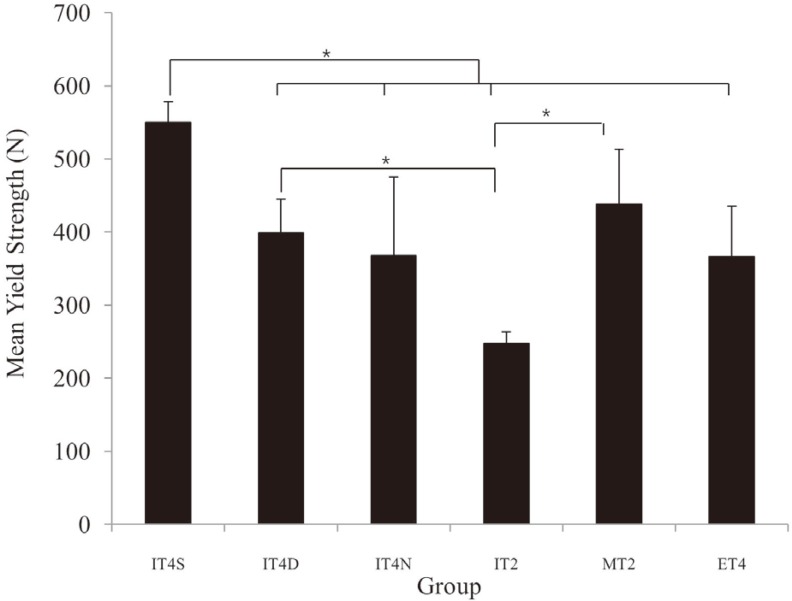
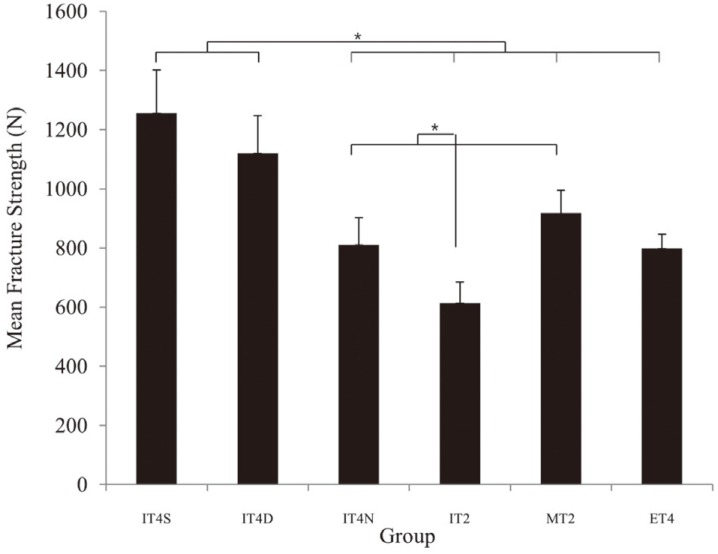
The mean values and standard deviations of yield and fracture strength for each system are presented in Table 2 and multiple comparisons are presented in Fig. 2 and Fig. 3. The specimens in group IT4S had the highest values for both yield strength and fracture strength, whereas those in group IT2 had the lowest values. There was no significant difference in the yield and fracture strength between the specimens in group IT4N and group ET4, which were made by the same manufacturer (Neobiotech, Co., Ltd., Korea) though they have different connection types. There was no significant difference in yield strength between group IT4D and group IT4N, which have similar internal connection designs and use Ti grade 4. Yield and fracture strength differed significantly between group MT2 and group IT2, although they used the same titanium grade 2 material.
Fig. 2. Multiple comparisons from the analysis of the mean yield strengths of different types of implants (oneway ANOVA, n = 10).
*Significant difference (P < .05).
IT4S: Straumann Bone level, IT4D: Dentium superline, IT4N: Neobiotech CMI IS, IT2: Dentsply Xive s, MT2: Ankylos C/X, ET4: Neobiotech CMI EB
Fig. 3. Multiple comparisons resulting from the analysis of the mean fracture strength of different types of implants (one-way ANOVA, n = 10).
*Significant difference (P < .05)
IT4S: Straumann Bone level, IT4D: Dentium superline, IT4N: Neobiotech CMI IS, IT2: Dentsply Xive s, MT2: Ankylos C/X, ET4: Neobiotech CMI EB
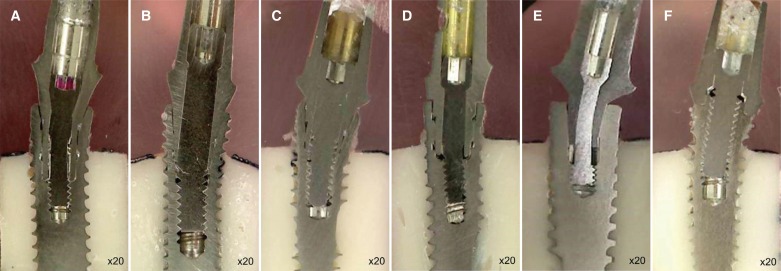
The types of failure observed are described in Table 3. Permanent deformation of the fixtures occurred in all specimens except for those in group MT2, and was mostly observed around the neck of the fixtures (Fig. 4). Specifically in specimens of group ET4, deformation occurred in the middle of the fixture. Specimens in group IT4S had a longer joint depth and an apparently more stable implant-abutment connection than the specimens in the other groups. Implant fixtures, abutments, and screws were bent in the area of decreased abutment wall thickness at its center. In specimens of group IT4D, we observed no deformation of the abutments and only partial fractures of the screws. The fracture zone was observed at the junctions of the unthreaded and threaded parts of the abutment screws after fixture deformation. In specimens of group IT4N, we observed screw bending with deformation of the fixture at the end of the union of abutment and screw on the fixture inner surface. Unlike the specimens in the other groups, the fixtures of the specimens in group MT2 had few variations. Deformation in the abutment structure usually occurred at the area with the smallest diameter. In specimens of group IT2, there was a distinct vertical gap between the fixture and abutment, suggesting abutment mobility. The movement of failed abutments was not observed after the static load test in any groups except group IT2. Interestingly, in specimens of group ET4, deformation of the fixtures was observed below the bone level, whereas the deformation of fixtures in specimens of other groups was mostly seen above the bone level or at the bone level. In the cross sectional view of the fractured screw in group IT2, typical marks indicating the direction of crack propagation were evident (Fig. 5).
Fig. 4. Longitudinal section images of failed systems taken with a digital microscope (×20). (A) IT4S (Straumann Bone level), (B) IT4D (Dentium superline), (C) IT4N (Neobiotech CMI IS), (D) IT2 (Dentsply Xive s), (E) MT2 (Ankylos C/X) (F) ET4 (Neobiotech CMI EB).
Fig. 5. (A) Bottom view of a failed screw and fixture in group IT2 (×60). Dimples, which are characteristic of ductile failure, can be seen on the surface of the fractured screw. (B) Bottom view of a failed screw and fixture in group IT2 (×60). The black arrow indicates a compression curl, which defines the fracture origin on the opposing tensile side (×100).
DISCUSSION
The average physiological bite force is in a range of 50 N to almost 400 N in natural dentition19, but it was reported that some patients had very high magnitude bite force from 1200 N to 2000 N.19,20,21 So the strength and load bearing capacity of implant is an important property for successful implant restoration, especially to the patient with ability to produce high magnitude bite force. Static fracture occurs when the applied load exceeds the fracture strength, and this type of fracture is closely related to overload. Strong bite force, premature contact, the habit of teeth clenching, eating coarse and hard food, etc. are recognized risk factors for clinical conditions that cause implant failure.11,12
This study was not a test of materials, but an investigation of implant components functioning together as a whole system.9 Therefore, the strength was expressed in Newtons, not in MPa as is usual in testing of materials. In the load-displacement curve obtained using this study, yield strength is represented by the point when irreversible plastic deformation of the implant assembly was initiated. The peak value of the curve represents the fracture strength, the ability to withstand the overload until the implant system is destroyed by external force.22 It is also known as flexural strength or bending strength,13,23 beyond this point, permanent implant failure occurs.
There were significant differences in the yield and fracture strength against static load among each groups of the implant system in this study (Fig. 2, Fig. 3). It was observed that the yield strength of specimens in five groups except for those in group IT2 was acceptable in a clinical situation because they had a higher or similar value of yield strength compared to average maximum bite force. Exceptionally, the yield strength of group IT2 was much lower than average maximum bite force. Although the fixture of group IT2 has an approximately 0.2 mm smaller diameter than any of the other groups (Table 1), this group should be carefully selected when it was placed in patient who is expected to have high bite force and recommended using the fixture with larger diameter.
In this study, we suggested that the reason for obtaining the highest yield and fracture strength in specimens of group IT4S was the relatively long internal connection of about 4.2 mm joint depth with strong material property of Ti grade 4 (Table 1). Many studies reported that longer joint length of abutment-fixture connection were advantageous with respect to longevity and fracture strength.24,25,26,27,28
Fracture strength differed significantly between the specimens in group IT4D and group IT4N despite a similar connection interface. This may have been affected by differences of microstructure of components and the technology of material manufacture.
Generally, implant fixture-abutment connections are divided into external and internal, although they can be further classified based on the tapered degree or the locking index. Many studies performed with fatigue stress25,26,29,30,31 have reported that an internal connection has a superior yield strength and stability to those of an external connection. They claimed that the lateral forces are better distributed to conical interface of internal connection whereas the short height of the hexagon in external connection could not provide enough resistance for lateral force and the bending moments were transmitted to the fastening screw. However, this study, performed without fatigue stress, did not present the lowest mean values of yield and fracture strength in group ET4, which have a short external-hex with a butt joint connection. In addition, specimens in group IT4N (internal hex connection) and group ET4 (external hex connection), produced by the same manufacturer but had different connections, did not differ significantly in yield and fracture strength. We could presume that the reason of this is the implant assemblies used in this study kept holding the initial settling force between the thread parts without preload loss because it didn't receive extrinsic stress, thus the strength of systems themselves had been measured.
Specimens in group MT2 (Morse tapered connection) and group IT2 (internal connection), which were both made with Ti grade 2, differed in both yield and fracture strength. It could be suggested that the thick wall of the fixture based on the 'platform switching concept' in group MT2 resulted in significantly higher values and led to fewer instances of fixture deformation.32
The deformation of the implant assembly (Fig. 4) in the internal connection groups was generally observed above or at the bone level near the fixture neck. Specimens in groups IT4D and IT4N which have similar connection interfaces displayed similar types of deformation. Specimens in group ET4 as external connection, the abutment-fixturescrew assembly was firmly combined one unit, and deformation had occurred in the middle of the fixture at the end of the inserted screw. Only in group IT4D, partial fracture of the screw occurred at the junction between the unthreaded and threaded portions of the screw (Fig. 4). This was in contrast to previous studies33,34 reporting that screw failure occurred below the screw head or the threaded part of the screw. We could suggest that this different result may be due to difference in the amount of preload loss by external forces in threaded part when screw failure occurred. The groups made with Ti grade 2 (groups IT2 and MT2) showed more bending rather than fractures in failure characteristics as the manufacturer clamed in this study.
In SEM fractography of cross sections of the fractured screws in group IT2 (Fig. 5), we observed compression curl,35 indicating that the fracture originated on the tensile side, and a strong flexure phenomenon occurred prior to complete failure as a characteristic of Ti grade 2. The feature of curved lip marks in a compression curl results from a travelling crack that changes direction when it enters into a compression field.35 Figure 5 illustrates both a rough surface and a smooth surface, characteristics of ductile failure and brittle failure.36 However, we may suppose that brittle failure occurred without significant plastic deformation because the smooth surface occupied more than half of the area.
This study involved a small number of specimens and did not completely reproduce the intraoral condition. Future studies might include representing complex masticatory movements within a wet environment to obtain realistic intraoral conditions. Additionally, further study is required using more specimens and types of implant systems.
CONCLUSION
The result of this study did not suggest that one implant system is superior to another, but it provides an advisable knowledge for patients who are exposed to the overload. The internal connection design is not the only factor which provides enough resistance to static overloading. The property of titanium grades as material of the implant assembly is also important and has to be considered to avoid mechanical failure of an implant by overloading. A larger diameter implant should be selected when using a system made of Ti grade 2 for preventing implant failure.
Footnotes
This work was supported by the Basic Science Research Program of the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2013R1A1A1061129).
None of the authors have conflicts of interest related to this study.
References
- 1.Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, Peters F, Simpson JP. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13:144–153. doi: 10.1034/j.1600-0501.2002.130204.x. [DOI] [PubMed] [Google Scholar]
- 2.Nelson K, Semper W, Hildebrand D, Ozyuvaci H. A retrospective analysis of sandblasted, acid-etched implants with reduced healing times with an observation period of up to 5 years. Int J Oral Maxillofac Implants. 2008;23:726–732. [PubMed] [Google Scholar]
- 3.Sullivan D, Vincenzi G, Feldman S. Early loading of Osseotite implants 2 months after placement in the maxilla and mandible: a 5-year report. Int J Oral Maxillofac Implants. 2005;20:905–912. [PubMed] [Google Scholar]
- 4.Zarb GA, Zarb FL. Tissue integrated dental prostheses. Quintessence Int. 1985;16:39–42. [PubMed] [Google Scholar]
- 5.Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10:387–416. doi: 10.1016/s0300-9785(81)80077-4. [DOI] [PubMed] [Google Scholar]
- 6.Jemt T, Lekholm U, Gröndahl K. 3-year followup study of early single implant restorations ad modum Brånemark. Int J Periodontics Restorative Dent. 1990;10:340–349. [PubMed] [Google Scholar]
- 7.Scheller H, Urgell JP, Kultje C, Klineberg I, Goldberg PV, Stevenson-Moore P, Alonso JM, Schaller M, Corria RM, Engquist B, Toreskog S, Kastenbaum F, Smith CR. A 5-year multicenter study on implant-supported single crown restorations. Int J Oral Maxillofac Implants. 1998;13:212–218. [PubMed] [Google Scholar]
- 8.Jemt T, Pettersson P. A 3-year follow-up study on single implant treatment. J Dent. 1993;21:203–208. doi: 10.1016/0300-5712(93)90127-c. [DOI] [PubMed] [Google Scholar]
- 9.Strub JR, Gerds T. Fracture strength and failure mode of five different single-tooth implant-abutment combinations. Int J Prosthodont. 2003;16:167–171. [PubMed] [Google Scholar]
- 10.Brunski JB. Biomaterials and biomechanics in dental implant design. Int J Oral Maxillofac Implants. 1988;3:85–97. [PubMed] [Google Scholar]
- 11.Tagger Green N, Machtei EE, Horwitz J, Peled M. Fracture of dental implants: literature review and report of a case. Implant Dent. 2002;11:137–143. doi: 10.1097/00008505-200204000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Binon PP, McHugh MJ. The effect of eliminating implant/abutment rotational misfit on screw joint stability. Int J Prosthodont. 1996;9:511–519. [PubMed] [Google Scholar]
- 13.Truninger TC, Stawarczyk B, Leutert CR, Sailer TR, Hämmerle CH, Sailer I. Bending moments of zirconia and titanium abutments with internal and external implant-abutment connections after aging and chewing simulation. Clin Oral Implants Res. 2012;23:12–18. doi: 10.1111/j.1600-0501.2010.02141.x. [DOI] [PubMed] [Google Scholar]
- 14.Sailer I, Sailer T, Stawarczyk B, Jung RE, Hämmerle CH. In vitro study of the influence of the type of connection on the fracture load of zirconia abutments with internal and external implant-abutment connections. Int J Oral Maxillofac Implants. 2009;24:850–858. [PubMed] [Google Scholar]
- 15.Mitsias ME, Silva NR, Pines M, Stappert C, Thompson VP. Reliability and fatigue damage modes of zirconia and titanium abutments. Int J Prosthodont. 2010;23:56–59. [PubMed] [Google Scholar]
- 16.Dixon DL, Breeding LC, Sadler JP, McKay ML. Comparison of screw loosening, rotation, and deflection among three implant designs. J Prosthet Dent. 1995;74:270–278. doi: 10.1016/s0022-3913(05)80134-9. [DOI] [PubMed] [Google Scholar]
- 17.Breeding LC, Dixon DL, Nelson EW, Tietge JD. Torque required to loosen single-tooth implant abutment screws before and after simulated function. Int J Prosthodont. 1993;6:435–439. [PubMed] [Google Scholar]
- 18.Standlee JP, Caputo AA. Accuracy of an electric torque-limiting device for implants. Int J Oral Maxillofac Implants. 1999;14:278–281. [PubMed] [Google Scholar]
- 19.Flanagan D. Diet and implant complications. J Oral Implantol. 2016;42:305–310. doi: 10.1563/aaid-joi-D-15-00127. [DOI] [PubMed] [Google Scholar]
- 20.Helkimo E, Carlsson GE, Helkimo M. Bite force and state of dentition. Acta Odontol Scand. 1977;35:297–303. doi: 10.3109/00016357709064128. [DOI] [PubMed] [Google Scholar]
- 21.Hagberg C. Assessment of bite force: a review. J Craniomandib Disord. 1987;1:162–169. [PubMed] [Google Scholar]
- 22.Dittmer MP, Dittmer S, Borchers L, Kohorst P, Stiesch M. Influence of the interface design on the yield force of the implant-abutment complex before and after cyclic mechanical loading. J Prosthodont Res. 2012;56:19–24. doi: 10.1016/j.jpor.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 23.Khraisat A. Stability of implant-abutment interface with a hexagon-mediated butt joint: failure mode and bending resistance. Clin Implant Dent Relat Res. 2005;7:221–228. doi: 10.1111/j.1708-8208.2005.tb00067.x. [DOI] [PubMed] [Google Scholar]
- 24.English CE. Externally hexed implants, abutments, and transfer devices: a comprehensive overview. Implant Dent. 1992;1:273–282. doi: 10.1097/00008505-199200140-00009. [DOI] [PubMed] [Google Scholar]
- 25.Semper W, Kraft S, Krüger T, Nelson K. Theoretical considerations: implant positional index design. J Dent Res. 2009;88:725–730. doi: 10.1177/0022034509341172. [DOI] [PubMed] [Google Scholar]
- 26.Semper W, Kraft S, Krüger T, Nelson K. Theoretical optimum of implant positional index design. J Dent Res. 2009;88:731–735. doi: 10.1177/0022034509341243. [DOI] [PubMed] [Google Scholar]
- 27.Möllersten L, Lockowandt P, Lindén LA. Comparison of strength and failure mode of seven implant systems: an in vitro test. J Prosthet Dent. 1997;78:582–591. doi: 10.1016/s0022-3913(97)70009-x. [DOI] [PubMed] [Google Scholar]
- 28.McGlumphy EA, Robinson DM, Mendel DA. Implant superstructures: a comparison of ultimate failure force. Int J Oral Maxillofac Implants. 1992;7:35–39. [PubMed] [Google Scholar]
- 29.Merz BR, Hunenbart S, Belser UC. Mechanics of the implant-abutment connection: an 8-degree taper compared to a butt joint connection. Int J Oral Maxillofac Implants. 2000;15:519–526. [PubMed] [Google Scholar]
- 30.Steinebrunner L, Wolfart S, Ludwig K, Kern M. Implant-abutment interface design affects fatigue and fracture strength of implants. Clin Oral Implants Res. 2008;19:1276–1284. doi: 10.1111/j.1600-0501.2008.01581.x. [DOI] [PubMed] [Google Scholar]
- 31.Levine RA, Clem D, Beagle J, Ganeles J, Johnson P, Solnit G, Keller GW. Multicenter retrospective analysis of the solid-screw ITI implant for posterior single-tooth replacements. Int J Oral Maxillofac Implants. 2002;17:550–556. [PubMed] [Google Scholar]
- 32.Lazzara RJ, Porter SS. Platform switching: a new concept in implant dentistry for controlling postrestorative crestal bone levels. Int J Periodontics Restorative Dent. 2006;26:9–17. [PubMed] [Google Scholar]
- 33.Semper-Hogg W, Kraft S, Stiller S, Mehrhof J, Nelson K. Analytical and experimental position stability of the abutment in different dental implant systems with a conical implant-abutment connection. Clin Oral Investig. 2013;17:1017–1023. doi: 10.1007/s00784-012-0786-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freitas Júnior AC, Bonfante EA, Silva NR, Marotta L, Coelho PG. Effect of implant-abutment connection design on reliability of crowns: regular vs. horizontal mismatched platform. Clin Oral Implants Res. 2012;23:1123–1126. doi: 10.1111/j.1600-0501.2011.02257.x. [DOI] [PubMed] [Google Scholar]
- 35.Freitas-Júnior AC, Almeida EO, Bonfante EA, Silva NR, Coelho PG. Reliability and failure modes of internal conical dental implant connections. Clin Oral Implants Res. 2013;24:197–202. doi: 10.1111/j.1600-0501.2012.02443.x. [DOI] [PubMed] [Google Scholar]
- 36.Apicella D, Veltri M, Balleri P, Apicella A, Ferrari M. Influence of abutment material on the fracture strength and failure modes of abutment-fixture assemblies when loaded in a bio-faithful simulation. Clin Oral Implants Res. 2011;22:182–188. doi: 10.1111/j.1600-0501.2010.01979.x. [DOI] [PubMed] [Google Scholar]