Abstract
Objective
The efficacy of low-level laser treatment (LLLT) for chronic back pain remains controversial due to insufficient trial data. We aimed to conduct an updated review to determine if LLLT (including laser acupuncture) has specific benefits in chronic non-specific low back pain (CNLBP).
Methods
Electronic databases were searched for randomised trials using sham controls and blinded assessment examining the intervention of LLLT in adults with CNLBP. Primary outcomes were pain and global assessment of improvement with up to short-term follow-up. Secondary outcomes were disability, range of back movement, and adverse effects. A random effects meta-analysis was conducted. Subgroup analyses were based on laser dose, duration of baseline pain, and whether or not laser therapy used an acupuncture approach.
Results
15 studies were selected involving 1039 participants. At immediate and short-term follow-up there was significant pain reduction of up to WMD (weighted mean difference) −1.40 cm (95% CI −1.91 to −0.88 cm) in favour of laser treatment, occurring in trials using at least 3 Joules (J) per point, with baseline pain <30 months and in non-acupuncture LLLT trials. Global assessment showed a risk ratio of 2.16 (95% CI 1.61 to 2.90) in favour of laser treatment in the same groups only at immediate follow-up.
Conclusions
We demonstrated moderate quality of evidence (GRADE) to support a clinically important benefit in LLLT for CNLBP in the short term, which was only seen following higher laser dose interventions and in participants with a shorter duration of back pain. Rigorously blinded trials using appropriate laser dosage would provide greater certainty around this conclusion.
Keywords: LASER THERAPY, LOW LEVEL; PAIN MANAGEMENT; SYSTEMATIC REVIEWS
Introduction
Chronic non-specific low back pain (CNLBP) not attributable to a recognisable, known specific pathology is common, with an estimated prevalence in developed countries of approximately 23%.1 CNLBP is a major cause of medical expenses, absenteeism, and disability. There are concerns regarding the benefits and potential harms of medication such as paracetamol, non-steroidal anti-inflammatory drugs (NSAIDs), and opioids2 3 for the treatment of chronic back pain, and non-drug treatments including exercise and multidisciplinary and behavioural treatment have been demonstrated to be of benefit.4
Low-level laser therapy (LLLT) is a light source treatment that may act via non-thermal or photochemical reactions in cells. It includes laser acupuncture (LA), which involves focused irradiation at specific points, most commonly traditional acupuncture points, with a low intensity laser.5 LLLT for pain relief in medicine remains controversial with claims that apparent efficacy is due to the placebo effect.
Multiple mechanisms for LLLT analgesia may exist. There is experimental evidence suggesting that laser irradiation induces peripheral neural blockade, suppresses central synaptic activity, modulates neurotransmitters, reduces muscle spasm and interstitial oedema, and exerts anti-inflammatory effects.6 The World Association of Laser Therapy (WALT) has published guidelines for LLLT dosage described in Joules (J) per point for arthritis and tendinopathy.7
A number of meta-analyses since 2003 have reported pain relief from LLLT in painful musculoskeletal conditions.8–10 In 2008, a Cochrane systematic review of laser therapy focusing on non-specific low back pain (LBP)11 included seven trials, considered both acute and chronic pain, did not restrict controls to sham laser, and excluded LA trials. At that point, there were insufficient data to draw firm conclusions on the effect of LLLT in LBP. Our objective was to conduct an updated systematic review of the efficacy of LLLT, including LA, for the treatment of CNLBP.
Methods
This meta-analysis was performed in accordance with the guidelines of the Cochrane Back Review Group (CBRG)12 and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).13 The study protocol is provided in online supplementary data file appendix A.
acupmed-2015-011036supp.pdf (961.5KB, pdf)
Eligibility criteria
Studies were randomised controlled trials (RCTs) with blinded assessment of the outcome. Participants were non-pregnant adults with CNLBP.1 The primary intervention studied was LLLT, including LA. For the purposes of this review, LA studies were defined as those in which low intensity laser was applied to classical acupuncture points, tender points and/or trigger points, and where acupuncture intent was explicitly stated in the report; other studies were classified as non-acupuncture laser therapy. The comparison intervention needed to be sham laser therapy with similar appearance to the active treatment but without laser irradiation. Studies including co-interventions were allowed if applied equally to both laser and control groups. Crossover studies were excluded.
Outcomes
Primary outcomes were: (1) LBP measured by visual analogue scale (VAS) or numerical pain rating scale (NPRS); and (2) ‘global assessment’, which represented dichotomous categorical outcomes of overall improvement or satisfaction with the received intervention. These were measured immediately (<1 week post-treatment) and at short-term (1–12 weeks) follow-up.
Secondary outcomes included disability, quantified using the Oswestry Disability Index (ODI)14 or the Roland-Morris Disability Questionnaire (RMQ),15 as well as adverse effects, range of movement (ROM) of the back, and pain or global assessment at intermediate (∼6 months) and long-term (∼1 year) follow-up.
Search methods for identification of studies
Electronic databases (MEDLINE, PubMed, EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Central Register of Controlled Trials (CENTRAL), Allied and Complementary Medicine Database (AMED), and Physiotherapy Evidence Database (PEDro)) were searched for RCTs of laser therapy or LA for the treatment of chronic LBP in which the control treatment used was sham laser. Publication reference lists were additionally examined to identify any missed studies. We used the Updated Search Strategies for CBRG,16 which included a generic search for RCTs and controlled clinical trials, combined with a specific search for ‘back’ conditions. We completed the search by adding terms related to the laser intervention, as detailed in the online supplementary data file appendix B.
Selection of studies, data extraction and management
Papers were initially screened at title and abstract level by one reviewer (GG) who removed duplicate reports and ineligible trials. There was no restriction of full text by language. Potentially eligible papers were reviewed by pairs of reviewers and data extracted independently. Authors were contacted if possible, to clarify further information. We used RevMan 5.3 (Cochrane Collaboration)17 for data management and statistical analysis.
Assessment of risk of bias in included studies
We adapted the Cochrane Collaboration tool12 for assessing risk of bias in 12 domains. Paired reviewers categorised domains as ‘high’, ‘low’ or ‘unclear’ risk of bias; disagreements were resolved by consensus. External reviewers assessed bias in one specific trial18 for which our reviewers were the authors. Trials were considered to be at ‘higher risk of bias’ if they contained more than six domains of ‘high’ and ‘uncertain’ risk.
Measures of treatment effect
For continuous data (pain intensity, disability, and ROM), treatment effects were expressed as a mean difference (MD) or standardised mean difference (SMD) together with 95% CIs. For global assessment we calculated the risk ratio (RR) and 95% CI. Meta-analysis was used to combine the results of trials using a random-effects model.
Unit of analysis issues
Different pain measurement scales (VAS and NPRS) were converted to a scale of 0–10 cm. In one trial18 that examined more than one laser dose, in order to avoid ‘double counts’, we split the sham laser control group into two equally sized groups to allow inclusion of two independent comparisons within the meta-analysis.19
Missing data, assessment of heterogeneity and publication bias
We used the RevMan calculator17 to derive unreported statistical data. Where laser parameters were unreported, the following physical formula was used to calculate the dose:
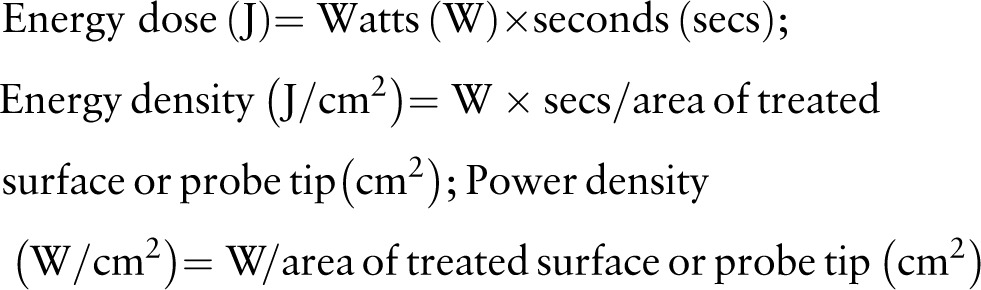 |
Heterogeneity was assessed and interpreted as described in the Cochrane Handbook.19 I2 values of 0–40%, 30–60%, and 50–90% were considered to represent ‘unimportant’, ‘moderate’, and ‘substantial’ heterogeneity, respectively. Publication bias was addressed by examination of funnel plots for primary outcomes.
Data synthesis
We conducted meta-analysis for outcomes at immediate and short-term follow-up except where outcomes were reported for two studies or less, in which case results were presented narratively, together with the longer term follow-up. Decisions for conducting subgroup analyses were made at protocol stage based on: (1) acupuncture/non-acupuncture laser therapy; and (2) laser dosage. A post-hoc decision regarding the cut-off value for laser dose and a subgroup analysis for baseline pain duration was guided by consideration of the review findings. A sensitivity analysis was performed excluding trials considered at ‘higher risk of bias’.
Grading the quality of evidence
We followed the CBRG12 recommendation to adapt the GRADE20 approach for back reviews with the quality of the evidence based on five domains (limitations of the study design, inconsistency, indirectness, imprecision, and publication bias).
Results
Search results
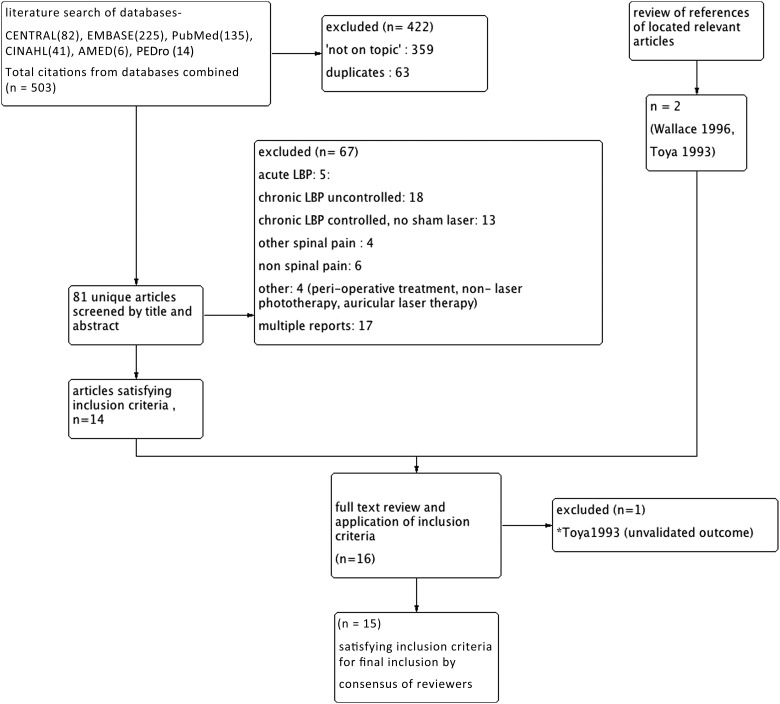
Electronic searches of databases from inception until August 2014, and screening reference lists, identified 15 studies that satisfied the inclusion criteria (figure 1). Three papers required translation into English from German21 and Japanese.22 23
Figure 1.
Flow chart: study selection. *Excluded study (Toya41). LBP, low back pain.
Characteristics of included studies
Participants
The selected trials18 21–34 included 1039 participants at randomisation (table 1). Participants were mostly recruited into trials from hospitals and rehabilitation clinics, except in the case of four trials18 21 28 34 that recruited via community newspapers. Some trials did not fully describe details of their inclusion criteria for chronicity22 23 or specificity.22 23 31 In trials where the mean baseline duration of pain was reported, this was categorised as ‘shorter’24 26 27 30 (average range 4.6–27 months) or ‘longer’18 21 25 28 29 34 (49 months to 13 years).
Table 1.
Participant data and outcomes
| Trial First author (year) (country) |
Total group size (n) | Mean age (years) | (1) Clinical inclusion criteria (2) Non-specific back pain |
Baseline mean pain duration | Baseline mean pain intensity: (0–10 cm) |
Baseline mean disability ODI (RMQ) |
Other baseline variables reported | Outcomes measure (follow-up period(s) post-treatment) |
|---|---|---|---|---|---|---|---|---|
| Alayat24 (2014) (Saudi Arabia) |
52 | 33 | (1) Male patients with history of LBP for at least 1 year (2) Yes |
13 months | 8.3 | 34 | Bodyweight | Pain, ODI, ROM (immediate, 12 weeks) |
| Ay25 (2010) (Turkey) |
40 | 53.5 | (1) LBP over 3 months duration due to lumbar disc herniation (2) Yes |
49 months | 6.3 | 24(15) | Education level | Pain, ODI, RMQ, ROM, GA (immediate) |
| Basford26 (1999) (USA) |
63 | 48 | (1) Non-radiating low back pain of >30 days duration (2) Yes |
10 months | 3.6 | 23 | Degeneration on lumbar X-ray, analgesic use, previous treatment |
Pain, ODI, ROM (immediate, 4 weeks) |
| Djavid27 (2007) (Iran) |
41 | 37 | (1) LBP minimum 12 weeks duration (2) Yes |
27 months | 6.2 | 33 | Education level, smoking status |
Pain, ODI, ROM (immediate, 6 weeks) |
| Glazov28 (2009) (Australia) |
100 | 51 | (1) LBP at least 3 months duration (2) Yes |
11 years | 5.7 | 30 | Multiple | Pain, ODI, GA (immediate, 6 weeks, 6 months) |
| Glazov18 (2014) (Australia) |
144 | 54 | (1) LBP at least 3 months duration (2) Yes |
13 years | 5.0 | 27 | Multiple | Pain, ODI, GA (immediate, 6 weeks, 6 months, 1 year) |
| Klein29 (1990) (USA) |
20 | 42 | (1) LBP at least 12 months duration (2) Yes |
8.5 years | 3.2 | (5.6) | Nil other | Pain, RMQ, ROM (1 month) |
| Konstantinovic30 (2011) (Serbia) |
56 | 69 | (1) Geriatric patients with chronic LBP caused by degenerative changes without red flag symptoms (2) NR |
4.6 months | 6.8 | 31 | Nil other | Pain, ODI, ROM (immediate) |
| Lin31 (2012) (Taiwan) |
28 | 64 | (1) LBP at least 3 months, recruited from a hospital. ‘Other complications like heart attack, kidney problem, pregnancy, excluded’ (2) NR |
NR | 5.2 | NR | BMI | Pain (immediate) |
| Okamoto22 (1989) (Japan) |
69 | 57 | (1) ‘Patients admitted to hospital with LBP,…pregnant, lactating, recent surgery, immune suppressants, difficult to treat excluded’ (2) NR |
NR | NR | NR | Nil other | GA (immediate) |
| Ruth21 (2010) (Germany) |
111 | 59 | (1) LBP over 6 months duration (2) Yes |
10 years | 6.3* | NR | Employment status |
GA (pain, disability)* (12 weeks) |
| Soriano32 (1998)(Argentina) | 85 | 64 | (1) LBP duration over 3 months (2) Yes |
NR | 8.0 | NR | Nil other | GA (immediate) |
| Umegaki23 (1989)(Japan) |
60 | 55 | Same as in Okamoto trial | NR | NR | NR | Nil other | GA (immediate) |
| Vallone33 (2014) (Italy) |
100 | 68 | (1) LBP duration over 6 months (2) Yes |
NR | 6.5 | NR | Nil other | Pain (immediate) |
| Wallace34 (1996) (Australia) |
41 | 50 | (1) LBP at least 3 months duration. (2) Yes |
6.5 years | 6.3 | 31 | Multiple | Pain, ODI (immediate) |
*von Korff scale.
BMI, body mass index; GA, global assessment; LBP, low back pain; NR, not reported; ODI, Oswestry Disability Index; RMQ, Roland Morris Questionnaire; ROM, range of back movement.
Interventions
Five trials were classified as LA studies18 21 28 31 34 (table 2). Three of these trials used smaller doses of 0.2–1.1 J/point.18 28 34 One trial21 used a ‘laser needle’ device to deliver 60–180 J/point irradiation, while another31 used 12 J/point.
Table 2.
Interventions
| Trial | Laser diode Pulse mode Wavelength (nm) | Dose/point (J) Spot size (cm2) |
Mean laser power (mW) (peak power) |
Energy density (J/cm2) J/cm2 |
Power density (W/cm2) | Sessions/weeks Points treated per session Time (s) |
Co-intervention | Details of sham control |
|---|---|---|---|---|---|---|---|---|
|
*Alayat24 (2014) |
Nd:YAG Pulsed 1064 |
25 0.2 |
1786 (3 kW) |
0.61 | 8.9 | 12/4 8 14 |
Exercise | No description of control device or if separate device used. Success of blinding not reported |
| Ay25 (2010) |
GaAlA Pulsed 805 |
2.8 0.07 |
12 (100 mW) |
40 | 1.4 | 15/3 2–4 240 |
Hot packs | Control used same machine without turning on device. Success of blinding not reported |
|
†Basford26 (1999) |
Nd:YAG Continuous 1060 |
239 4.9 |
2660 | 49 | 0.542 | 12/4 8 90 |
Nil | Control irradiated by the same but inactive probes. Not clear if separate machine used. Success of blinding not reported (there was a tendency for patients to experience ‘more warmth with active treatment’) |
|
‡Djavid27 (2007) |
GaAlAs Continuous 810 |
<7.5 0.22 |
50 | 27 | 8.2 | 12/6 8 <150 |
Exercise | Control was irradiated with inactive probes. Not clear if separate machines used. Procedure to ensure masking not described, and success of blinding not reported |
|
§Glazov28 (2009) |
GaAlAs Continuous 830 |
0.2 0.2 |
10 | 1 | 0.05 | 10/10 8 20 |
Exercise |
aDevice custom designed for this research. Success of blinding confirmed by statistical analysis |
|
§Glazov18 (2014) |
GaAlAs Continuous 830 |
0.2 0.2 |
20 | 1, 4 |
0.1 | 8/8 9 10, 40 |
Nil |
aDevice custom designed for this research. Success of blinding confirmed by statistical analysis |
|
¶Klein29 (1990) |
GaAs Pulsed 904 |
1.3 1.0 |
5.4 | 1.3 | 0.005 | 12/4 50 240 |
Exercise | Machine was modified by manufacturer with a toggle switch with two settings, only one of which activated the laser. Single device used. Success of blinding not reported |
| Konstant-inovic30 (2011) |
GaAs Pulsed 905 |
3 1.0 |
100 | 3 | 0.1 | 15/3 4 60 |
Exercise | Two machines were used labelled A or B; one with active laser, another deactivated. Patients and therapist treating the patients could not distinguish which was active or control. Success of blinding not reported |
|
**Lin31 (2012) |
NR Pulsed 808 |
12 0.8 |
20 (40 mW) |
15 | 0.025 | 5/1 4 600 |
Soft cupping | Control group had the same procedure as the laser group but without laser radiation. No other details given. Success of blinding not reported |
| Okomoto22 (1989) |
GaAlAs Continuous 830 |
18 0.126 |
30 | 143 | 0.24 | 10/3 1 600 |
Nil | Two machines of identical appearance used (A and B) corresponding to laser or placebo laser; each had decoy with light and sound. No other details given in paper. Success of blinding not reported |
|
††Ruth21 (2010) |
NR Continuous 680, 785 |
60–180 ? |
50–150 | ? | 1–5 | 10/5 8 1200 |
Nil | Toggle switch on same machine operated by independent person according to randomisation list. Goggles on participants, and controls on machine covered by opaque black tape. Success of blinding confirmed by statistical analysis |
|
‡‡Soriano32 (1998) |
GaAs Pulsed 904 |
4 ? 0.95 |
40 (20W) |
4.2 | 0.04 | 10/2 ? ? |
Nil | Used an activated laser and a deactivated laser but the electrical circuit, timer and alarm worked as usual. Not clear if separate devices used. Success of blinding not reported |
| Umegaki23 (1989) |
GaAlAs Continuous 830 |
18 0.126 |
30 | 143 | 0.24 | 10/3 2 600 |
Nil | Two machines of identical appearance used (A and B) corresponding to laser or placebo laser; each had decoy with light and sound. No other details given in paper. Success of blinding not reported |
|
§§Vallone33 (2014) |
GaAlAs Continuous 980 |
1200 32 |
20 000 | 37.5 | 0.625 | 9/3 6 60 |
Exercise | Dials showing the on/off power setting of machine were not within view of subjects. Success of blinding not reported |
|
¶¶Wallace34 (1996) |
GaAlAs Continuous 830 |
1.1 0.42 |
37 | 2.64 | 0.09 | 5/5 8 30 |
Nil | Independent assistant operated and covered the coded switch on laser machine determining if laser on or off. Appearance of machine the same regardless of laser output. Success of blinding not reported |
Entries in bold were not reported/unavailable and were calculated or assumed by reviewers.
*‘High intensity laser therapy’. Also included manual scanning of fields (2×1400 J). Total dose/session 3000 J.
†Laser device allowed simultaneous stimulation of two points.
‡Total treatment duration 20 mins including eight points and manual scanning of standardised field (time differential not reported but assume <150 s per discrete point). Total dose/session 60 J.
§aLaser/sham mode set by operating a number on dial. Probe had decoy light/sound device inbuilt. Individualised treatment (average 8–9 points/session) including local and distal GV, BL and GB points and ah shi points.
¶Multi-head device stimulating 10 points simultaneously.
**Multi-channel device. Simultaneous stimulation of four points (bilateral BL40 and two ah shi points in lumbar region).
††‘Laser needle’ fibre-optic cable device. Simultaneous stimulation of eight points (individualised treatment including BL23, BL40, BL60, KI3, GB and ah shi points). Same author previously described34 laser output tip diameters 2.0 and 0.8 mm (=power density 1 W/cm2 and 5 W/cm2, respectively.
‡‡‘2 cm grid in painful area’ (number of points and irradiation time per point unreported). Spot size given as 0.0015 cm2 but 1.1 cm2 with irradiation time 100 s according to Cochrane review.11
§§Unclear if manual scanning used.
¶¶Individualised treatment: local (BL26, ah shi points, GV2) and distal (GV14, BL11, LR3, BL60, LI4, ST36, SP6, PC6, HT7).
NR, not reported.
The remaining 10 trials were classified as non-acupuncture laser therapy studies. Two studies25 29 used ≤2.8 J/point, while much higher dosages were used in another two trials26 33 (239 and 1200 J/point, respectively). The remaining six trials used doses in the range of 3–25 J/point. Three trials24 27 33 used manual scanning to irradiate larger anatomically defined areas as well as irradiation of discrete points. Reporting of laser parameters was incomplete in certain trials and some values were calculated or assumed if authors could not be contacted.
Controls
A variety of methods to achieve sham laser controls were reported including use of the same machine with on/off switch, or use of a separate machine and/or probe. Blinding methods included the use of opaque goggles, as well as a specific laser machine35 capable of blinding both patient and operator to treatment allocation (table 2). In some trials the description of the masking procedure was unclear24 26 27 32 or completely absent.31 Only three studies18 21 28 statistically analysed the success of the blinding technique used.
Outcomes
Only four trials18 21 26 28 defined predetermined primary outcomes. The majority of studies reported pain using a VAS; two studies18 34 used an NPRS. Participant based ‘global assessment’ was reported as a dichotomised categorical variable including ‘condition improved’ versus ‘same or worse’18 28 and ‘good response’ versus ‘same or undecided’.22 23 Two trials only reported an arbitrary level of improvement on a pain scale (eg, >50% reduction of chronic pain on Von Korff Scale21 or ≥60% reduction pain on VAS scale32). These dichotomous outcomes were combined during meta-analysis to determine the RR of ‘global improvement’. The majority of studies that reported disability used ODI; one trial reported only RMQ.29 Range of back movement was measured as flexion in centimetres (Schober's test)25–27 30 or in degrees.24 29 Occurrence of adverse effects was briefly mentioned in five trials25 26 29 32 34 but quantitative comparisons were only undertaken in three.18 21 28 Most studies reported immediate and/or short-term outcomes; only three studies18 28 32 reported outcomes at longer-term follow-up.
Risk of bias in included studies
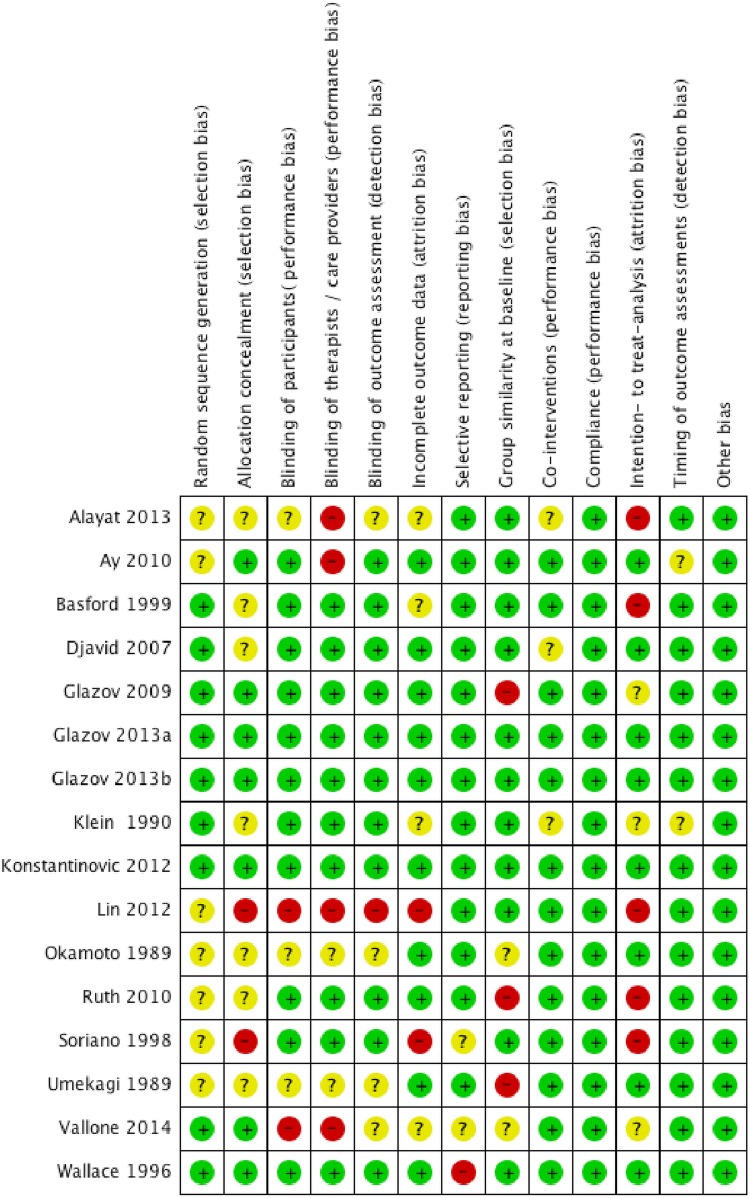
Figure 2 demonstrates the proportion of studies determined to be low risk for each domain. Under our criteria we found three trials24 31 33 that we considered to be at ‘higher risk of bias’.
Figure 2.
Risk of bias summary: review authors’ judgements on risk of bias items for each included study. Proportion of low risk studies: Random sequence generation (53%), Allocation concealment (47%), Blinding participants (67%), Blinding therapists (60%), Blinding outcome assessors (67%), Incomplete outcome data (60%), Selective reporting (80%), Group baseline similarity (67%), Co-interventions (80%), Compliance (100%), Intention to treat (40%), Timing outcome assessment (87%). Note: Glazov 2013a and 2013b represent different groups of same study.
Primary outcomes
Pain
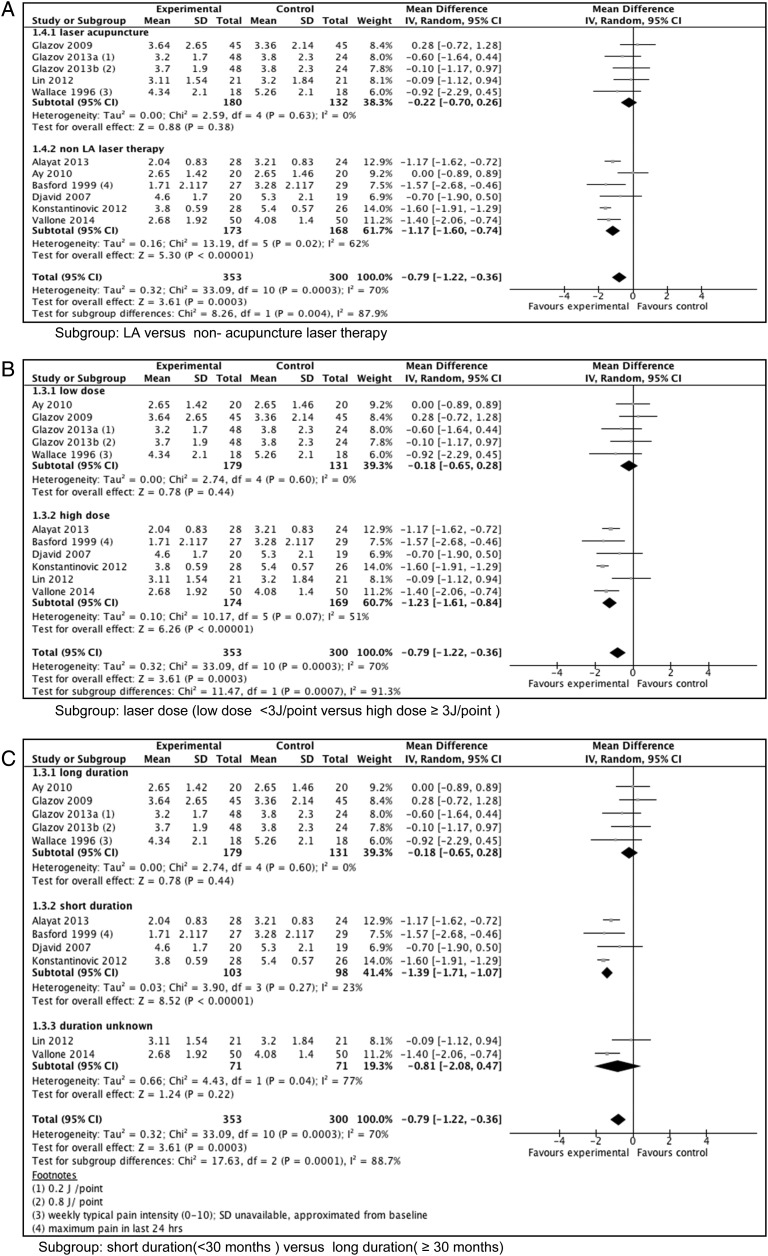
Meta-analysis of data from 653 participants across 10 trials at immediate follow-up indicated a statistically significant reduction in total pain scores in laser versus control groups (WMD (weighted mean difference) −0.79 cm, 95% CI −1.22 to −0.36 cm; I2=70%), albeit with substantial heterogeneity (figure 3). In our subgroup analyses, a significant reduction of pain (laser compared to control) was only seen for the trials in which participants had shorter mean baseline duration (<30 months) of LBP (WMD −1.39 cm, 95% CI −1.71 to −1.07 cm; I2=23%). Significant differences between laser and control were also seen in the higher dose trials (>3 J/point) (WMD −1.23 cm, 95% CI 11.61 to −0.84 cm; I2=51%) and non-acupuncture trials (WMD −1.17 cm, 95% CI −1.60 to 0.74 cm; I2=62%). At short-term follow-up, there were no significant differences and substantial heterogeneity in the total pain score was observed (see six trials, 391 participants; online supplementary data file appendix C). In subgroup analyses we observed a significant reduction of pain (for laser compared to control) with the largest effect seen in higher dose trials and in trials with shorter duration of back pain at baseline (WMD −1.40 cm, 95% CI −1.91 to −0.88 cm; I2=0%).
Figure 3.
Forest plots: subgroup analysis of pain at immediate follow-up. LA, laser acupuncture.
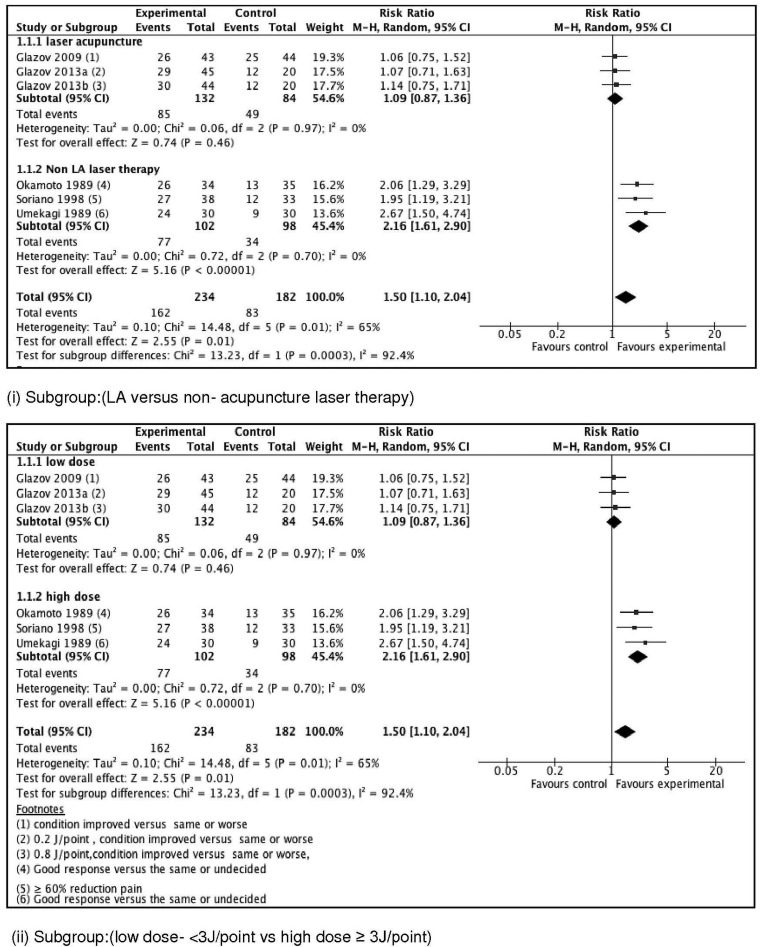
Global assessment
As illustrated in figure 4, pooling of categorical data at immediate follow-up from 416 subjects (five trials) showed a significant effect on global assessment (RR 1.5, 95% CI 1.10 to 2.04; I2=65%) in favour of laser treatment (substantial heterogeneity present) with a greater improvement in both non-acupuncture and higher dose subgroups (RR 2.16, 95% CI 1.61 to 2.90; I2=0%) with reduced heterogeneity. Pooled data for short-term follow-up showed no significant differences for three included LA trials, two of which used a ‘lower’ dose (see online supplementary data file appendix D).
Figure 4.
Forest plots: subgroup analysis of global assessment at immediate follow-up. LA, laser acupuncture.
Sensitivity analysis
Results were robust to exclusion of trials considered at ‘higher risk of bias’ with pain differences in favour of laser in the higher dose subgroup at immediate (WMD −1.5 cm, 95% CI −1.8 to −1.2 cm) and short-term (WMD −1.7cm, 95% CI −2.5 to −1.0 cm) follow-up (see online supplementary data file appendix E). Similar findings were shown in non-acupuncture and ‘short duration’ subgroups. There were no trials at ‘higher risk of bias’24 31 33 that reported global assessment outcomes.
Secondary outcomes
Intermediate and long-term pain and global assessment
Two trials (both low dose LA) reported outcomes at 6 months and at 12 months. They found no significant difference between groups for pain or global assessment at these time periods. One trial32 that reported less relapse of pain in the laser group at 6 months used an unvalidated outcome.
Disability
Analysis of data from 490 subjects (eight trials) at immediate follow-up found a small reduction in combined ODI score in laser versus control (WMD −2.5%, 95% CI −4.6% to −0.4%; I2=47%; see online supplementary data file appendix F). Subgroup analyses showed greater benefit of laser in non-acupuncture trials (WMD −3.5%, 95% CI −6.0% to −1.5%; I2=33%), and those applying higher dose treatment and/or including subjects with a shorter duration of back pain (WMD −3.6%, 95% CI −6.1% to −1.1%; I2=48%). Combined data from 383 subjects (six trials) at short-term follow-up found no significant difference, but subgroup analyses found greater benefit up to a WMD of −5.9% (95% CI −8.9% to −2.8%; I2=64%) in the same groups.
Range of back movement
ROM was measured only in the non-acupuncture trials.24–27 29 30 One trial24 found a significant difference of 4° flexion in favour of laser in the short-term.
Adverse effects
Brief reference to the absence of adverse effects was made in six trials.25 26 29 32–34 Quantitative comparison (including flares of pain and other minor adverse effects) was undertaken in three studies18 21 28 showed no significant difference between laser and control.
Risk of publication bias
We plotted the effect sizes from trials that reported pain at immediate or short-term follow-up against the inverse of their standard error (see online supplementary data file appendix G). Visual inspection of the funnel plot did not show asymmetry suggestive of ‘small study bias’.
Quality of evidence
We reached the conclusion that there was moderate quality evidence (GRADE profile20) that laser therapy reduces pain in the immediate and short term in subjects with CNLBP if pain has been present for <30 months or if a laser dose of at least 3 J/point is used (see online supplementary data file appendix H). The overall quality of evidence for this outcome was reduced due to limitations in the domain involving risk of bias. For the outcome of global assessment at immediate follow-up, the evidence of benefit of laser therapy was further reduced to low quality due to uncertainty in details of duration and specificity of LBP in trials22 23 and laser intervention parameters in a trial32 reporting this outcome.
Discussion
This meta-analysis summarised RCTs that compared the effect of low-level laser with sham controls for the treatment of CNLBP. While combining data from all clinically heterogeneous studies demonstrated a small benefit, subgroup analyses showed larger positive effects of laser on pain, global assessment and disability present up to 12 weeks after treatment, particularly in trials with higher laser dose interventions. The effect size of the pain reduction (over sham) of 1.4 cm in these subgroups approached the minimally important change (MIC) for pain proposed by Ostelo36 of 1.5 cm. Disability (ODI) reduction was significant in the short term but less than the MIC of 10%.36 In this review, the mean pain reduction in the placebo laser groups averaged approximately 2.0 cm. The total average pain reduction between baseline and short-term follow-up, representing both non-specific and specific effects of the laser intervention, was about 60%.
Our results are consistent with previous findings8–10 suggesting benefits of low-level laser in a range of painful musculoskeletal conditions including chronic neck pain. In the trials we examined there appeared to be a dose threshold of 3 J/point for benefit of laser. This is higher than the minimal dose suggested by reviews by Baxter37 (0.5 J/point for myofascial pain) and Chow38 (0.8 J/point for chronic neck pain), but closer to the dose recommended by WALT7 (4 J/point for lumbar spine arthritis). This could be explained by the deeper location of structures in the low back area, requiring a higher laser irradiation dose for penetration. There was no upper dose at which laser appeared not to be effective or caused adverse effects.
Our review also found a relationship between duration of pain and laser effectiveness. This finding is plausible but needs to be explored in further research. Two previous studies examining physical treatment for back pain39 and acupuncture for chronic pain conditions40 showed a generally worse outcome for subjects with longer pain duration, but no interaction effect with type of treatment. Acute pain is more likely to resolve spontaneously than chronic pain and, once central sensitisation occurs, a condition may become unresponsive to LLLT.
Most (eight out of 10) non-acupuncture laser therapy trials were positive, that is, they showed a difference between laser and sham groups in primary outcomes; negative trials in this group25 29 treated participants with a longer duration of pain with a lower dose. Most non-acupuncture laser trials in this review treated relatively few points in the area of pain, although some also irradiated wider areas using a manual scanning technique. Skin surface application of laser results in photon scattering in the underlying volume of tissue,38 resulting in more widespread biological effects regardless of the intent of the therapist to stimulate acupuncture points, ah shi points or local anatomical structures. Acupuncturists and other laser therapists both irradiate tender points in the region of pain; the absence of positive acupuncture trials in this review could be related to small laser dosage and other factors unrelated to the approach to treatment. We were not able to determine why two higher dose LA trials21 31 were negative in this review.
Heterogeneity of studies and insufficient data were quoted as reasons for the previous inability to establish firm conclusions on the effect of LLLT for LBP.11 A strength of our review was the larger number of trials and inclusion of more recent eligible publications since the last such review, as well as exclusion of acute back pain and trials without sham laser controls, thus reducing heterogeneity and allowing the study of specific laser effects. Subgroup analysis was important in explaining the heterogeneity.
A major limitation of this review was related to bias from possible unmasking. Low risk of bias in all blinding domains according to the Cochrane tool was present in only about 60% of trials. In positive trials, the success of blinding was not tested and there were other possible deficiencies in blinding. Subject awareness of thermal sensation in trials with higher power devices is possible, which may potentially have unmasked the patients to treatment allocation. These issues arguably reduce the ability of this review to draw firm conclusions. Inadequate reporting of the characteristics of participants and laser parameters also produced uncertainty.
It is critical that rigorous blinding35 is instituted in any further clinical trials investigating laser therapy for the treatment of pain. The appropriate laser dose range for specific body regions (as recommended by WALT) should be followed, and full and explicit description of the laser parameters,5 treatment regimen, and baseline characteristics of the participants is important. Future studies may also establish the role of other components of the intervention such as the number and/or location of points, frequency/duration of treatment, and the effect of longer-term follow-up on outcomes.
Our meta-analysis suggests that LLLT, when used by itself or in combination with other modalities, may achieve a useful reduction in pain for up to 3 months in CNLBP with few adverse effects. However, we would recommend a degree of caution before widespread implementation, until our results can be confirmed by further rigorously blinded trials using adequate laser doses.
Summary points.
This updated systematic review examined the effectiveness of low-level laser therapy compared to sham laser in the treatment of chronic non-specific low back pain.
There was substantial clinical heterogeneity present between the 15 included trials, related to differences in both participant characteristics and laser interventions.
Meta-analysis showed a clinically important pain reduction in laser versus sham lasting up to 12 weeks post-completion of treatment (WMD −1.40 cm, 95% CI −1.91 to −0.88 cm).
Pain reduction occurred in subgroups with non-acupuncture laser interventions, laser dosage ≥3 J per point, and in participants with a shorter duration of baseline pain (30 months).
Further trials using strict masking and adequate laser doses are needed to ensure that the apparent benefits of laser are not due to bias related to unblinding of participants.
Acknowledgments
The authors would like to thank external reviewers Roberta Chow and Philip Gabel for assessing our own trial, and Yoshi Inoue for helping with the Japanese translation.
Footnotes
Contributors: GG was the doctoral candidate and lead author and was responsible for the conceptualisation of the protocol and conduct of the review. MY and JE made substantial contributions to the design of the work, drafted and critically revised the manuscript for important intellectual content, and agree to be accountable for the content of the work. All authors approved the final version of the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data sharing on this research article is available on request from the corresponding author.
References
- 1.Airaksinen O, Hildebrandt J, Mannion A, et al. European guidelines for the management of chronic non specific low back pain (Amended version June 14th 2005) 2004. http://www.backpaineurope.org/web/files/WG2_Guidelines.pdf (accessed 5 Apr 2015).
- 2.Machado GC, Maher CG, Ferreira PH, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ 2015;359:h1225 10.1136/bmj.h1225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deyo RA, Von Korff M, Duhrkoop D. Opioids for low back pain. BMJ 2015;350:g6380 . 10.1136/bmj.g6380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Middelkoop M, Rubinstein SM, Kuijpers T, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 2011;20:19–39. 10.1007/s00586-010-1518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baxter G, Diamantopoulos C. Therapeutic lasers: theory and practice. London: Churchill Livingstone, 1994. [Google Scholar]
- 6.Hamblin M, Huang YY. Handbook of photomedicine. Taylor & Francis, 2013. Chapter 51, Low-level laser therapy in treatment of pain, 591–601. [Google Scholar]
- 7.World Association of Laser Therapy. Dosage Recommendations 2010. http://waltza.co.za/documentation-links/recommendations/dosage-recommendations/ (accessed 4 Apr 2015).
- 8.Bjordal J, Couppé C, Chow RT, et al. A systematic review of low level laser therapy with location-specific doses for pain from joint disorders. Aust J Physiother 2003;49:107–16. 10.1016/S0004-9514(14)60127-6 [DOI] [PubMed] [Google Scholar]
- 9.Fulop AM, Dhimmer S, Deluca JR, et al. A meta-analysis of the efficacy of laser phototherapy on pain relief. Clin J Pain 2010;26:729–36. 10.1097/AJP.0b013e3181f09713 [DOI] [PubMed] [Google Scholar]
- 10.Law D, McDonough S, Bleakley C, et al. Laser acupuncture for treating musculoskeletal pain: a systematic review with meta-analysis. J Acupunct Meridian Stud 2015;8:2–16. 10.1016/j.jams.2014.06.015 [DOI] [PubMed] [Google Scholar]
- 11.Yousefi-Nooraie R, Schonstein E, Heidari K, et al. Low level laser therapy for nonspecific low-back pain. Cochrane Database Syst Rev 2008;(2):CD005107 10.1002/14651858.CD005107.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Furlan AD, Pennick V, Bombardier C, et al. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34:1929–41. 10.1097/BRS.0b013e3181b1c99f [DOI] [PubMed] [Google Scholar]
- 13.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med 2009;151:W65–94. 10.7326/0003-4819-151-4-200908180-00136 [DOI] [PubMed] [Google Scholar]
- 14.Fairbank J, Pynsent P. The Oswestry disability index. Spine 2000;25:2940–53. 10.1097/00007632-200011150-00017 [DOI] [PubMed] [Google Scholar]
- 15.Roland M, Morris R. A study of the natural history of back pain. Part 1: development of a reliable and sensitive measure of disability in low back pain. Spine (Phila Pa 1976) 1983;8:141–4. [DOI] [PubMed] [Google Scholar]
- 16.2013. Updated Search Strategies for CBG Jan 2013. http://back.cochrane.org/sites/back.cochrane.org/files/uploads/PDF/CBRG Search Strategies Jan 2013.pdf.
- 17.Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014 (accessed Jul 2014).
- 18.Glazov G, Yelland M, Emery J. Low-dose laser acupuncture for non-specific chronic low back pain: a double blind randomised controlled trial. Acupunct Med 2014;32:116–23. 10.1136/acupmed-2013-010456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org [Google Scholar]
- 20.Atkins D, Best D, Briss P, et al. , GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ruth M, Weber M, Zenz M. Laser acupuncture for chronic back pain: a double-blind clinical study. Schmerz 2010;24:485–93. 10.1007/s00482-010-0966-3 [DOI] [PubMed] [Google Scholar]
- 22.Okamoto H. Therapeutic effect of semiconductor laser irradiation on low-back pain. J Jpn A Phys Med Balneology Climatology 1989;52:131–45. [Google Scholar]
- 23.Umegaki S. Effectiveness of low-power laser therapy on low-back pain: double blind comparative study to evaluate the analgesic effect of low-power laser therapy. Kiso to Rinsho (The Clinical Report) 1989;23:2839–46. [Google Scholar]
- 24.Alayat MS, Atya AM, Ali MM, et al. Long-term effect of high-intensity laser therapy in the treatment of patients with chronic low back pain: a randomized blinded placebo-controlled trial. Lasers Med Sci 2014;29: 1065–73. 10.1007/s10103-013-1472-5 [DOI] [PubMed] [Google Scholar]
- 25.Ay S, Doğan S, Evcik D. Is low-level laser therapy effective in acute or chronic low back pain? Clin Rheumatol 2010;29:905–10. 10.1007/s10067-010-1460-0 [DOI] [PubMed] [Google Scholar]
- 26.Basford J, Sheffield C, Harmsen B. Laser therapy: a randomized controlled trial of effects of low intensity Nd:YAG laser irradiation on musculoskeletal back pain. Arch Phys Med Rehabil 1999;80:647–52. 10.1016/S0003-9993(99)90167-3 [DOI] [PubMed] [Google Scholar]
- 27.Djavid GE, Mehrdad R, Ghasemi M, et al. In chronic low back pain, low level laser therapy combined with exercise is more beneficial than exercise alone in the long term: a randomised trial. Aust J Physiother 2007;53:155–60. [DOI] [PubMed] [Google Scholar]
- 28.Glazov G, Schattner P, Lopez D, et al. Laser acupuncture for chronic non-specific low back pain: a controlled clinical trial. Acupunct Med 2009;27:94–100. 10.1136/aim.2009.000521 [DOI] [PubMed] [Google Scholar]
- 29.Klein RG, Eek BC. Low-energy laser treatment and exercise for chronic low back pain: double-blind controlled trial. Arch Phys Med Rehabil 1990;71:34–7. [PubMed] [Google Scholar]
- 30.Konstantinovic L, Lazovic M, Milovanovic N, et al. Low level laser therapy in geriatric patients with low back pain. Eur J Pain Suppl (Poster Sessions) 2011;5:61 10.1016/S1754-3207(11)70205-X [DOI] [Google Scholar]
- 31.Lin ML, Wu HC, Hsieh YH, et al. Evaluation of the effect of laser acupuncture and cupping with ryodoraku and visual analog scale on low back pain. Evid Based Complementary Altern Med 2012;2012:521612 10.1155/2012/521612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soriano F, Rios R. Gallium arsenide laser treatment of chronic low back pain: a prospective, randomized and double blind study. Laser Ther 1998;10:175–80. 10.5978/islsm.10.175 [DOI] [Google Scholar]
- 33.Vallone F, Benedicenti S, Sorrenti E, et al. Effect of diode laser in the treatment of patients with nonspecific chronic low back pain: a randomized controlled trial. Photomed Laser Surg 2014;32:490–4. 10.1089/pho.2014.3715 [DOI] [PubMed] [Google Scholar]
- 34.Wallace G. The effects of laser acupuncture on chronic low back pain [Thesis]. Melbourne Monash University, 1996. [Google Scholar]
- 35.Relf I, Chow R, Pirotta M. Blinding techniques in randomized controlled trials of laser therapy: an overview and possible solution. Evid Based Complement Alternat Med 2008;5: 383–9. 10.1093/ecam/nem085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ostelo RW, Deyo RA, Stratford P, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine 2008;33:90–4. 10.1097/BRS.0b013e31815e3a10 [DOI] [PubMed] [Google Scholar]
- 37.Baxter GD, Bleakley C, McDonough S. Clinical effectiveness of laser acupuncture: a systematic review. J Acupunct Meridian Stud 2008;1:65–82. 10.1016/S2005-2901(09)60026-1 [DOI] [PubMed] [Google Scholar]
- 38.Chow R, Johnson M, Lopes-Martins R, et al. Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials. The Lancet 2009;374:1897–908. 10.1016/S0140-6736(09)61522-1 [DOI] [PubMed] [Google Scholar]
- 39.Underwood M, Morton V, Farrin A. Do baseline characteristics predict response to treatment for low back pain? Secondary analysis of the BEAM dataset [ISRCTN32683578]. Rheumatology 2007;46:1297–302. [DOI] [PubMed] [Google Scholar]
- 40.Witt CM, Schützler L, Lüdtke R, et al. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain? Clin J Pain 2011;27:550–5. 10.1097/AJP.0b013e31820dfbf5 [DOI] [PubMed] [Google Scholar]
- 41.Toya S, Inomata K, Macda T. Report on a computer randomized double blind trial to determine the effectiveness of the GaAlAs(830 nm)diode laser for pain attenuation in selected pain groups. Laser Ther 1994;6:143–48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
acupmed-2015-011036supp.pdf (961.5KB, pdf)